Abstract
Ramp injury, that is, injury to the peripheral attachment of the posterior horn of the medial meniscus, often requires additional surgery during anterior cruciate ligament (ACL) reconstruction. Diagnosis and treatment of ramp lesions are important because unrepaired ramp lesions could cause risk to the reconstructed ACL because of anteroposterior and external rotation laxity, whereas acute rupture or chronic deficiency of the ACL could also cause ramp lesions because of instability. Ramp lesions are difficult to diagnose and treat from the anterior compartment during arthroscopy. Typically, this repair requires technically demanding skills and is performed from the posterior portal using a suture hook under visualization with the arthroscope through the intercondylar notch. Inexperienced surgeons often struggle with using the posterior portal and the suture hook. Our all-inside repair technique using the FasT-Fix system (Smith & Nephew, Andover, MA) under direct visualization from the anterior compartment accompanied by a medial collateral ligament pie-crusting technique facilitates repair of ramp lesions without causing medial instability.
Technique Video
A patient who visited the outpatient clinic for left knee pain after a fall from a height while climbing showed a complete anterior cruciate ligament (ACL) tear and complex meniscal tear on magnetic resonance imaging (MRI). With the patient lying in the semi-lithotomy position under general anesthesia, routine arthroscopic examination is performed using the anteromedial, anterolateral, and superomedial portals. To confirmatively show the ramp lesion, an additional posteromedial portal is made, which is not necessary in our technique. The suspected ramp lesion can also be examined with posteromedial visualization by diving the arthroscope deep through the intercondylar notch between the posterior cruciate ligament (PCL) and the medial femoral condyle. Typically, through standard anterior portals, the ramp lesion is not fully exposed because it is covered by the medial femoral condyle and the sufficient space necessary for the repair technique is not secured. In this case, an additional longitudinal meniscal tear is observed on the posterior and inferior side of the meniscal body. The probe from the anteromedial portal can examine the ramp lesion by pulling, but the medial femoral condyle blocks fine manipulation. Medial-compartment release is performed with multiple applications of the pie-crusting technique to the medial collateral ligament (MCL) in the valgus position at 15° of flexion with manual assistance. After assessment of the surface anatomy, multiple applications of pie crusting on the superficial MCL are performed with a spinal needle. In the process of puncturing, the surgeon can monitor whether the needle tip penetrates into the capsule. The surgeon should take care not to injure the meniscocapsular junction and saphenous nerve and vein. Moreover, under the surveillance of the scope, a sufficient medial-compartment release can be confirmed and, at the same time, excessive widening can be avoided. As a result, the ramp lesion can be fully visualized from the anterolateral portal and a probe or Fast-Fix needle from the anteromedial portal can approach the posteromedial meniscocapsular junction without any other help. All repair procedures are performed with the Fast-Fix 360 Meniscal Repair system. This system is introduced through the anteromedial portal over a slotted cannula to avoid lodging of soft tissues. The first needle is fired at the posterior capsule, and the second needle is fired on the meniscal body. The suture is then tightened, and the surgeon can observe that the gap made by the ramp lesion is approximated. The stability of the repaired lesion and the necessity for additional suture are evaluated. In this case, additional suturing is performed for more desirable sutures with about a 7-mm interval from the previous suture. The repaired lesion is examined again and confirmed to be stable with proper tension. Thereafter, suturing for the longitudinal meniscal tear is also performed with Fast-Fix suture device. Finally, the stability of the sutured meniscus is checked with a probe. To show the repaired state, the arthroscope is advanced through the posteromedial portal and the well-reduced ramp lesion is confirmed. ACL reconstruction is then performed. At 3 months postoperatively, no valgus instability is observed on the valgus stress radiograph compared with the preoperative radiograph.
Ramp lesions, which were first reported in 1988 by Strobel, are characterized by injury to the peripheral attachment of the posterior horn of the medial meniscus.1 These lesions are found in approximately 9.3% to 17% of anterior cruciate ligament (ACL) injury cases.2,3 Diagnosis and treatment of ramp lesions are important because, if neglected, they can cause anteroposterior instability or injury to the body of the medial meniscus, resulting in early failure of the reconstructed ACL or early osteoarthritis of the knee joint.4,5 Ramp lesions are difficult to diagnose and treat arthroscopically from the anterior compartment.6 A technique using a suture hook through the high posteromedial portal is commonly used for ramp lesion repair.7 However, it is challenging and requires more surgical skill because there is some risk of damage to the posterior neurovascular structures and articular cartilage.7 Under these circumstances, Mostafa Zaky Abdelrazek et al.8 introduced a technique to repair ramp lesions using standard anterior portals. This technique provides convenient and reliable repair of ramp lesions through standard anterior portals using the FasT-Fix 360 Meniscal Repair system (Smith & Nephew, Andover, MA). However, this technique requires visualization of the ramp lesion with a light source through the intercondylar notch, which can be challenging for inexperienced surgeons, especially in tight knees.8 We thus introduce a technique for repairing ramp lesions under anterior visualization using a medial collateral ligament (MCL) pie-crusting technique (Video 1).
Surgical Technique
The patient is placed in the supine position on the operating table with an appropriate tourniquet applied over the cast padding. Routine arthroscopic examination is planned using the anteromedial, anterolateral, and superomedial portals. First, the superomedial portal for the drainage system is created 2 fingerbreadth lateral to the lateral patellar margin and 1 finger breadth superior to the superior patellar margin. Thereafter, the anterolateral portal is made using a No. 10 blade for arthrotomy; the arthroscope is advanced through this portal. Observing through the anterolateral portal and using a transillumination technique, the surgeon explores the preferred position for the anteromedial portal with an 18-gauge needle. Arthroscopic examination of both compartments is performed, and the status of the menisci is determined using a probe. Suspected medial meniscal ramp lesions are examined with posteromedial visualization of the posterior meniscocapsular attachment of the medial meniscus by pushing the arthroscope through the anterolateral portal deep into the intercondylar notch between the posterior cruciate ligament and the medial femoral condyle (Fig 1).
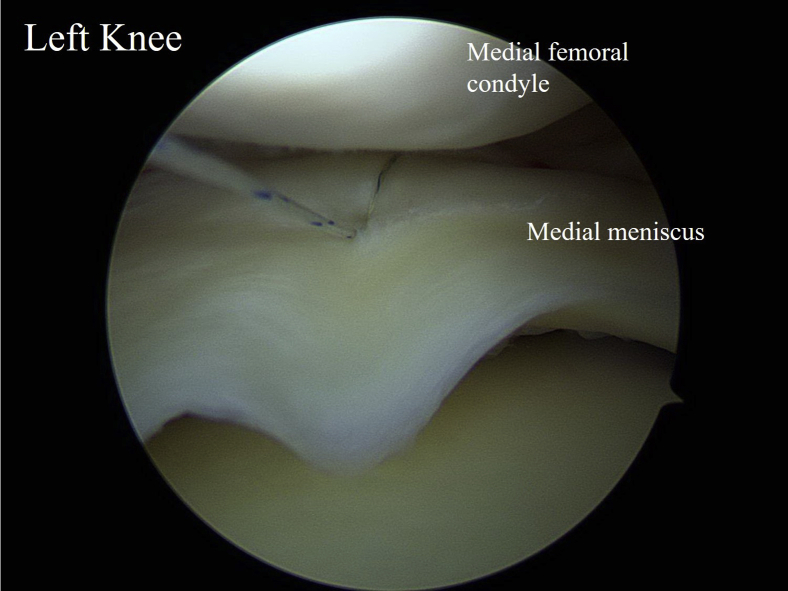
Fig 1.
Arthroscopic view of posteromedial compartment of left knee. The patient is positioned in the semi-lithotomy position with 80° of flexion of the left knee. The suspected ramp lesion is confirmed by advancing the arthroscope from the posteromedial portal and by probing it with a probe coming from the standard anterolateral portal through the intercondylar notch. This technique is performed to confirm that a ramp lesion is present.
Typically, with the use of standard anterior portals, the ramp lesion is not fully exposed and space can be insufficient for repair. Under these circumstances, MCL release to widen the medial compartment with a pie-crusting technique (needling of the superficial MCL in the valgus position at 15° of flexion with manual assistance) and repair under anterior visualization is considered an alternative to repair using the posteromedial portal (Fig 2). Using this technique, we can secure sufficient space in the medial compartment. As a result, both the arthroscope from the anterolateral portal and a probe or FasT-Fix needle from the anteromedial portal can approach the posteromedial meniscocapsular junction without the need to place the arthroscope deep into the intercondylar notch (Video 1, Fig 3).
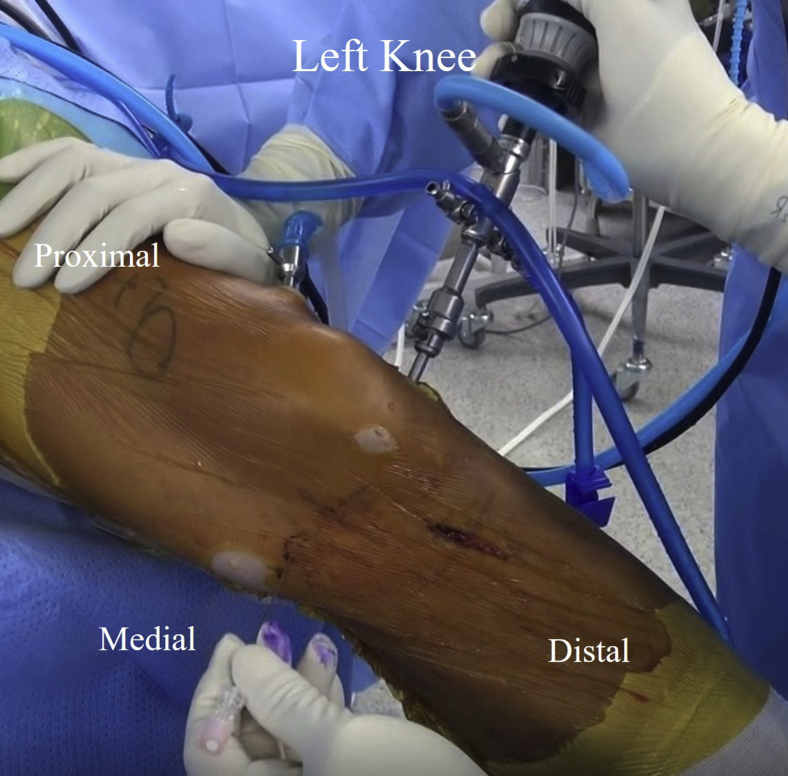
Fig 2.
Left knee shown from lateral side of patient lying in semi-lithotomy position. On the basis of an examination of the surface anatomy, the medial collateral ligament (MCL) and joint line are marked. With a spinal needle, pie crusting of the superficial MCL is performed in the valgus position at 15° of flexion with manual assistance. By use of this position, the surgeon can more clearly feel the margin of the superficial MCL.
Fig 3.
Patient positioned in semi-lithotomy position with 80° of flexion of left knee and arthroscope advanced from standard anterolateral portal. By means of medial collateral ligament release, the ramp lesion, which is usually covered by the medial femoral condyle, can be seen from the standard anterolateral viewing portal. By use of the FasT-Fix system from anteromedial portal, the ramp lesion is repaired. The torn gap is approximated. This process is performed through a standard anterior portal.
All repair procedures are performed using the FasT-Fix 360 Meniscal Repair system. The FasT-Fix 360 needle is first adjusted to the desired depth of 12 mm. It is introduced through the anteromedial portal over a slotted cannula to avoid catching soft tissues. The first needle is fired at the posterior capsule, and the second, into the meniscal body. The suture is then tightened to approximate the tear site, and an additional suture is placed as needed according the tear size (Video 1). Finally, an arthroscope is advanced through the posteromedial portal, and a well-reduced ramp lesion is confirmed (Fig 4). After completing repair of the ramp lesion and other meniscal tears, the surgeon performs ACL reconstruction of the ruptured ACL using autologous semitendinosus and gracilis tendons. All repair and reconstruction procedures are performed from anterior portals.
Fig 4.
Arthroscopic view of posteromedial compartment of left knee. The patient is positioned in the semi-lithotomy position with 80° of flexion of the left knee, and the arthroscope is inserted from the posteromedial portal. Repair of the ramp lesion is confirmed. This technique is performed to confirm the repaired state of a ramp lesion.
After repair and reconstruction, full range of motion (ROM) of the knee is confirmed. A hinged brace is applied for the first 6 weeks postoperatively during recovery of the reconstructed ACL and punctured MCL. Weight bearing is prohibited for 6 weeks to protect the repaired meniscus. ROM exercises are started and gradually increased to 90° until 2 weeks postoperatively and are maintained until 6 weeks postoperatively. After 6 weeks, patients are allowed to walk with crutches and proceed with active ROM. They should not return to sports activities until 6 months after surgery.
Discussion
A ramp lesion is a meniscal injury that frequently occurs concomitantly with ACL injury.5 Unrepaired ramp lesions can cause failure of ACL reconstruction, and acute rupture or chronic deficiency of the ACL can also cause ramp lesions owing to anteroposterior and rotational laxity.5,9, 10, 11, 12 Thus, unstable ramp lesions need to be repaired to ensure successful ACL repair.5,13 However, unlike other meniscal injuries, ramp lesions can easily be misdiagnosed or overlooked.14 Even if diagnosed properly, more surgical experience is required for the repair, making it difficult for inexperienced surgeons.15
Diverse surgical approaches have been used to repair ramp lesions, from arthroscopic-only techniques to techniques performed in combination with open surgery, including all-inside, inside-out, and outside-in repairs.2,4,9 Different suture techniques have been reported, such as repair with a suture hook using nonabsorbable suture material and with a suture device such as the FasT-Fix system.4,9,15 However, to our knowledge, no techniques have been reported that enable full visualization of the ramp lesion directly from the anterior compartment using an arthroscope placed through the anterolateral portal (without posteromedial visualization through the intercondylar notch) and repair of the lesion from the anteromedial portal using an MCL pie-crusting technique. Although Mostafa Zaky Abdelrazek et al.8 introduced a technique to repair ramp lesions using standard anterior portals, they visualized the posteromedial compartment by positioning the arthroscope through the intercondylar notch, which requires a high level of surgical skill.
The technique introduced in this article does not require a posterior portal or placement of the arthroscope through the intercondylar notch to visualize the posteromedial compartment. Instead, we visualize the posteromedial part of the meniscus, which is usually covered by the medial femoral condyle, directly from the anterolateral portal via an MCL pie-crusting technique. Simultaneous probing and repair of meniscal lesions including ramp lesions are possible through the anteromedial working portal. By means of this simple MCL pie-crusting technique, surgeons can overcome the limitations of the suture hook technique, such as the risk of neurovascular injury, as well as cartilage injury, and the relatively steep learning curve for novice surgeons. Moreover, there is no need for surgeons to alternate between 30° and 70° scopes and to shift portals during the repair, resulting in a reduced operating time. Considering that ramp lesion repair is usually accompanied by ACL reconstruction, shortening the operating time is an advantage.
Unlike previous reports that introduced MCL release as a technique only for patients with a tight medial compartment, we use this technique in all cases; it allows direct anterior visualization of the posteromedial part of the medial meniscus from the anterolateral portal.8 Many previous studies have established that MCL release is a safe and minimally harmful technique.16, 17, 18, 19 MCL pie crusting has typically generated grade I MCL laxity without saphenous nerve or vein damage, which usually diminished or resolved over time and did not require brace application.17,19 In addition, the functional outcome scores and postoperative pain of patients undergoing MCL release did not differ from those of patients undergoing the same procedure without MCL release.17 The results of a study on valgus instability at our institution, which followed up 5 cases for more than 6 months, also supported previous academic results. Every patient recovered to within grade I laxity with no clinical evidence of giving way at 3 months postoperatively.
It is important to identify the border of the superficial MCL to prevent unintended injury to the medial neurovascular structures such as the saphenous nerve or vein. It can be identified more easily if some valgus force is applied with 15° of flexion. Maximal valgus force and excessive pie crusting could cause complete iatrogenic MCL rupture. We recommend performing MCL release while checking the medial joint space under arthroscopic surveillance. Widening of the medial joint space can be confirmed, and it can help prevent unintended, iatrogenic complete MCL rupture (Video 1). Because surgeons do not advance the arthroscopic light source through the intercondylar notch or through the posterior portal, the risk of cartilage injury, which is a particular concern in procedures performed by inexperienced surgeons, can be decreased (Table 1).
Table 1.
Benefits and Limitations
| Benefits |
| Visualization is improved with MCL pie crusting, and surgeons could regulate the degree of widening under the arthroscope. |
| Repair using a suture hook through the posteromedial portal or visualization through the intercondylar notch is not required. |
| There is no risk of cartilage injury. |
| Limitations |
| There is a risk of iatrogenic complete MCL rupture. |
MCL, medial collateral ligament.
The described technique has both advantages and disadvantages. First, the learning curve for surgeons is less steep. Manipulation of arthroscopic devices in the anteromedial and anterolateral compartments is relatively safer than in the posterior compartment because of the lack of vital structures. Second, this technique requires fewer instruments, and surgeons do not need to shift between portals, reducing the operating time. To visualize the posteromedial compartment from the posterior portal or through the intercondylar notch, a 70° arthroscope is preferred. However, by releasing the medial compartment, the posteromedial compartment can be used for visualization without the 70° scope. This also enables surgeons to examine the whole meniscus from the same portal, which may lessen the risk of distortion due to a narrow visual field. Third, our technique can prevent the neurovascular and cartilage injuries that can occur during the posterior portal technique. However, the unpredictability of the degree of medial-compartment widening as well as risk of iatrogenic complete MCL rupture is a limitation that surgeons should be aware of (Table 2). Our all-inside repair technique for ramp lesions of the medial meniscus under direct visualization through anterior portals via MCL pie crusting provides a good visual field and an easier learning curve with satisfactory clinical results.
Table 2.
Advantages and Disadvantages
| Advantages |
| Easy technique without steep learning curve |
| Requirement for fewer instruments and reduction of operating time |
| Fewer morbidities than associated with posterior portal access (neurovascular injury, cartilage injury) |
| Disadvantages |
| Inability to predict degree of medial-compartment widening |
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A patient who visited the outpatient clinic for left knee pain after a fall from a height while climbing showed a complete anterior cruciate ligament (ACL) tear and complex meniscal tear on magnetic resonance imaging (MRI). With the patient lying in the semi-lithotomy position under general anesthesia, routine arthroscopic examination is performed using the anteromedial, anterolateral, and superomedial portals. To confirmatively show the ramp lesion, an additional posteromedial portal is made, which is not necessary in our technique. The suspected ramp lesion can also be examined with posteromedial visualization by diving the arthroscope deep through the intercondylar notch between the posterior cruciate ligament (PCL) and the medial femoral condyle. Typically, through standard anterior portals, the ramp lesion is not fully exposed because it is covered by the medial femoral condyle and the sufficient space necessary for the repair technique is not secured. In this case, an additional longitudinal meniscal tear is observed on the posterior and inferior side of the meniscal body. The probe from the anteromedial portal can examine the ramp lesion by pulling, but the medial femoral condyle blocks fine manipulation. Medial-compartment release is performed with multiple applications of the pie-crusting technique to the medial collateral ligament (MCL) in the valgus position at 15° of flexion with manual assistance. After assessment of the surface anatomy, multiple applications of pie crusting on the superficial MCL are performed with a spinal needle. In the process of puncturing, the surgeon can monitor whether the needle tip penetrates into the capsule. The surgeon should take care not to injure the meniscocapsular junction and saphenous nerve and vein. Moreover, under the surveillance of the scope, a sufficient medial-compartment release can be confirmed and, at the same time, excessive widening can be avoided. As a result, the ramp lesion can be fully visualized from the anterolateral portal and a probe or Fast-Fix needle from the anteromedial portal can approach the posteromedial meniscocapsular junction without any other help. All repair procedures are performed with the Fast-Fix 360 Meniscal Repair system. This system is introduced through the anteromedial portal over a slotted cannula to avoid lodging of soft tissues. The first needle is fired at the posterior capsule, and the second needle is fired on the meniscal body. The suture is then tightened, and the surgeon can observe that the gap made by the ramp lesion is approximated. The stability of the repaired lesion and the necessity for additional suture are evaluated. In this case, additional suturing is performed for more desirable sutures with about a 7-mm interval from the previous suture. The repaired lesion is examined again and confirmed to be stable with proper tension. Thereafter, suturing for the longitudinal meniscal tear is also performed with Fast-Fix suture device. Finally, the stability of the sutured meniscus is checked with a probe. To show the repaired state, the arthroscope is advanced through the posteromedial portal and the well-reduced ramp lesion is confirmed. ACL reconstruction is then performed. At 3 months postoperatively, no valgus instability is observed on the valgus stress radiograph compared with the preoperative radiograph.
References
- 1.Strobel M. Springer; New York, NY: 1988. Manual of Arthroscopic Surgery. [Google Scholar]
- 2.DePhillipo N.N., Cinque M.E., Kennedy N.I., et al. Inside-out repair of meniscal ramp lesions. Arthrosc Tech. 2017;6:e1315–e1320. doi: 10.1016/j.eats.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malatray M., Raux S., Peltier A., Pfirrmann C., Seil R., Chotel F. Ramp lesions in ACL deficient knees in children and adolescent population: A high prevalence confirmed in intercondylar and posteromedial exploration. Knee Surg Sports Traumatol Arthrosc. 2018;26:1074–1079. doi: 10.1007/s00167-017-4471-4. [DOI] [PubMed] [Google Scholar]
- 4.Li W.P., Chen Z., Song B., Yang R., Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27:56–60. doi: 10.5792/ksrr.2015.27.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stephen J.M., Halewood C., Kittl C., Bollen S.R., Williams A., Amis A.A. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400–408. doi: 10.1177/0363546515617454. [DOI] [PubMed] [Google Scholar]
- 6.Thaunat M., Fayard J.M., Guimaraes T.M., Jan N., Murphy C.G., Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acosta J., Ravaei S., Brown S.M., Mulcahey M.K. Examining techniques for treatment of medial meniscal ramp lesions during anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2020;36:2921–2933. doi: 10.1016/j.arthro.2020.05.041. [DOI] [PubMed] [Google Scholar]
- 8.Mostafa Zaky Abdelrazek B.H., Waly M.R., Abdel Aziz M.A., Abdel Aziz A. Different techniques for the management of meniscal ramp lesions using standard anterior portals. Arthrosc Tech. 2020;9:e39–e44. doi: 10.1016/j.eats.2019.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 10.Markolf K.L., Jackson S.R., McAllister D.R. Force measurements in the medial meniscus posterior horn attachment: Effects of anterior cruciate ligament removal. Am J Sports Med. 2012;40:332–338. doi: 10.1177/0363546511426100. [DOI] [PubMed] [Google Scholar]
- 11.Hatayama K., Terauchi M., Saito K., Takase R., Higuchi H. Healing status of meniscal ramp lesion affects anterior knee stability after ACL reconstruction. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120917674. 2325967120917674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bumberger A., Koller U., Hofbauer M., et al. Ramp lesions are frequently missed in ACL-deficient knees and should be repaired in case of instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:840–854. doi: 10.1007/s00167-019-05521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu X., Zhang H., Feng H., Hong L., Wang X.S., Song G.Y. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45:1004–1011. doi: 10.1177/0363546516682493. [DOI] [PubMed] [Google Scholar]
- 14.Greif D.N., Baraga M.G., Rizzo M.G., et al. MRI appearance of the different meniscal ramp lesion types, with clinical and arthroscopic correlation. Skeletal Radiol. 2020;49:677–689. doi: 10.1007/s00256-020-03381-4. [DOI] [PubMed] [Google Scholar]
- 15.Negrín R., Reyes N.O., Iñiguez M., Pellegrini J.J., Wainer M., Duboy J. Meniscal ramp lesion repair using an all-inside technique. Arthrosc Tech. 2018;7:e265–e270. doi: 10.1016/j.eats.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Claret-Garcia G., Montañana-Burillo J., Tornero-Dacasa E., et al. Pie crust technique of the deep medial collateral ligament in knee arthroscopy: Ultrasound and anatomic study. J Knee Surg. 2019;32:764–769. doi: 10.1055/s-0038-1668125. [DOI] [PubMed] [Google Scholar]
- 17.Moran T.E., Awowale J.T., Werner B.C., Fox M.A., Miller M.D. Associated morbidity after the percutaneous release of the medial collateral ligament for knee arthroscopy. Arthroscopy. 2020;36:891–900. doi: 10.1016/j.arthro.2019.08.051. [DOI] [PubMed] [Google Scholar]
- 18.Moran T.E., Demers A., Awowale J.T., Werner B.C., Miller M.D. The outside-in, percutaneous release of the medial collateral ligament for knee arthroscopy. Arthrosc Tech. 2020;9:e393–e397. doi: 10.1016/j.eats.2019.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polat B., Aydın D., Polat A.E., et al. Objective measurement of medial joint space widening with percutaneous "pie crust" release of medial collateral ligament during knee arthroscopy. J Knee Surg. 2020;33:94–98. doi: 10.1055/s-0039-1694711. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A patient who visited the outpatient clinic for left knee pain after a fall from a height while climbing showed a complete anterior cruciate ligament (ACL) tear and complex meniscal tear on magnetic resonance imaging (MRI). With the patient lying in the semi-lithotomy position under general anesthesia, routine arthroscopic examination is performed using the anteromedial, anterolateral, and superomedial portals. To confirmatively show the ramp lesion, an additional posteromedial portal is made, which is not necessary in our technique. The suspected ramp lesion can also be examined with posteromedial visualization by diving the arthroscope deep through the intercondylar notch between the posterior cruciate ligament (PCL) and the medial femoral condyle. Typically, through standard anterior portals, the ramp lesion is not fully exposed because it is covered by the medial femoral condyle and the sufficient space necessary for the repair technique is not secured. In this case, an additional longitudinal meniscal tear is observed on the posterior and inferior side of the meniscal body. The probe from the anteromedial portal can examine the ramp lesion by pulling, but the medial femoral condyle blocks fine manipulation. Medial-compartment release is performed with multiple applications of the pie-crusting technique to the medial collateral ligament (MCL) in the valgus position at 15° of flexion with manual assistance. After assessment of the surface anatomy, multiple applications of pie crusting on the superficial MCL are performed with a spinal needle. In the process of puncturing, the surgeon can monitor whether the needle tip penetrates into the capsule. The surgeon should take care not to injure the meniscocapsular junction and saphenous nerve and vein. Moreover, under the surveillance of the scope, a sufficient medial-compartment release can be confirmed and, at the same time, excessive widening can be avoided. As a result, the ramp lesion can be fully visualized from the anterolateral portal and a probe or Fast-Fix needle from the anteromedial portal can approach the posteromedial meniscocapsular junction without any other help. All repair procedures are performed with the Fast-Fix 360 Meniscal Repair system. This system is introduced through the anteromedial portal over a slotted cannula to avoid lodging of soft tissues. The first needle is fired at the posterior capsule, and the second needle is fired on the meniscal body. The suture is then tightened, and the surgeon can observe that the gap made by the ramp lesion is approximated. The stability of the repaired lesion and the necessity for additional suture are evaluated. In this case, additional suturing is performed for more desirable sutures with about a 7-mm interval from the previous suture. The repaired lesion is examined again and confirmed to be stable with proper tension. Thereafter, suturing for the longitudinal meniscal tear is also performed with Fast-Fix suture device. Finally, the stability of the sutured meniscus is checked with a probe. To show the repaired state, the arthroscope is advanced through the posteromedial portal and the well-reduced ramp lesion is confirmed. ACL reconstruction is then performed. At 3 months postoperatively, no valgus instability is observed on the valgus stress radiograph compared with the preoperative radiograph.
A patient who visited the outpatient clinic for left knee pain after a fall from a height while climbing showed a complete anterior cruciate ligament (ACL) tear and complex meniscal tear on magnetic resonance imaging (MRI). With the patient lying in the semi-lithotomy position under general anesthesia, routine arthroscopic examination is performed using the anteromedial, anterolateral, and superomedial portals. To confirmatively show the ramp lesion, an additional posteromedial portal is made, which is not necessary in our technique. The suspected ramp lesion can also be examined with posteromedial visualization by diving the arthroscope deep through the intercondylar notch between the posterior cruciate ligament (PCL) and the medial femoral condyle. Typically, through standard anterior portals, the ramp lesion is not fully exposed because it is covered by the medial femoral condyle and the sufficient space necessary for the repair technique is not secured. In this case, an additional longitudinal meniscal tear is observed on the posterior and inferior side of the meniscal body. The probe from the anteromedial portal can examine the ramp lesion by pulling, but the medial femoral condyle blocks fine manipulation. Medial-compartment release is performed with multiple applications of the pie-crusting technique to the medial collateral ligament (MCL) in the valgus position at 15° of flexion with manual assistance. After assessment of the surface anatomy, multiple applications of pie crusting on the superficial MCL are performed with a spinal needle. In the process of puncturing, the surgeon can monitor whether the needle tip penetrates into the capsule. The surgeon should take care not to injure the meniscocapsular junction and saphenous nerve and vein. Moreover, under the surveillance of the scope, a sufficient medial-compartment release can be confirmed and, at the same time, excessive widening can be avoided. As a result, the ramp lesion can be fully visualized from the anterolateral portal and a probe or Fast-Fix needle from the anteromedial portal can approach the posteromedial meniscocapsular junction without any other help. All repair procedures are performed with the Fast-Fix 360 Meniscal Repair system. This system is introduced through the anteromedial portal over a slotted cannula to avoid lodging of soft tissues. The first needle is fired at the posterior capsule, and the second needle is fired on the meniscal body. The suture is then tightened, and the surgeon can observe that the gap made by the ramp lesion is approximated. The stability of the repaired lesion and the necessity for additional suture are evaluated. In this case, additional suturing is performed for more desirable sutures with about a 7-mm interval from the previous suture. The repaired lesion is examined again and confirmed to be stable with proper tension. Thereafter, suturing for the longitudinal meniscal tear is also performed with Fast-Fix suture device. Finally, the stability of the sutured meniscus is checked with a probe. To show the repaired state, the arthroscope is advanced through the posteromedial portal and the well-reduced ramp lesion is confirmed. ACL reconstruction is then performed. At 3 months postoperatively, no valgus instability is observed on the valgus stress radiograph compared with the preoperative radiograph.