Abstract
Heterotopic ossification (HO) can occur as a complication of various pathologies affecting the hip including trauma, tendon avulsions, chronic injury, spinal cord injury, and soft-tissue disruption caused by surgery. When HO is present alongside intra-articular hip pathology such as femoroacetabular impingement syndrome (FAIS) or labral pathology, consideration should be made to combine the surgical excision of the HO with the FAIS decompression or labral repair if the location and size of the HO is appropriate for arthroscopic excision. Often times, the HO is located in such a position that any central compartment work can be completed before turning to the HO excision. If an open approach is required, the modified Gibson approach can be used for lateral hip access, whereas the Smith-Petersen approach provides anterior hip access. In this Technical Note we discuss arthroscopic techniques for excision of HO in the setting of concomitant FAIS, with discussion of when HO excision occurs in relation to cam decompression and labral repair, and mention tips on how to approach HO excision through an open approach.
Technique Video
In this video we present numerous cases and associated imaging of symptomatic heterotopic ossification (HO). We discuss the arthroscopic excision of HO using a radiofrequency ablation device and grasper to remove the HO from the surrounding tissue and remove it from the joint space. We discuss the removal of HO in relation to other arthroscopic work, including labral repair, cam decompression, and capsule repair. We also show the modified Gibson approach as an example of 1 approach to remove HO through an open incision. We demonstrate preoperative and postoperative imaging of the cases presented and provide a summary of the presented techniques.
Heterotopic ossification (HO) is commonly found in the hip after blunt trauma, surgical trauma, or chronic muscle injury. Certain medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or the use of prophylactic radiation are frequently prescribed to minimize the risk of developing HO in the postsurgical setting, although there is currently no gold standard for postoperative HO prophylaxis. Various HO prevention regimens are described in the literature, including 325 mg aspirin twice daily after surgery for 6 weeks, celecoxib 200 mg/d for 4 weeks, and naproxen 500 mg daily for 3 weeks after surgery, or a single dose of 700 cGy radiation or indomethacin 75 mg.1, 2, 3, 4 Previous studies have shown an HO incidence of 1.6% to 5.6% after hip arthroscopy with NSAID prophylaxis, compared to 25% to 44% without NSAID prophylaxis.3,5 Risk factors for the development of HO are prolonged postsurgical immobility, burns, spinal cord trauma, traumatic brain injury, male gender, and certain rare genetic conditions.6 The development of high-grade HO negatively impacts clinical outcomes by decreasing range of motion about the hip joint, with studies showing associated loss of terminal hip flexion, abduction, and internal rotation.7 Definitive treatment of HO requires that the bone be removed surgically. Successful removal of HO has been previously documented in the literature with both open and arthroscopic techniques.1,5,8
Some patients with symptomatic HO in the hip joint may present with concurrent pathology amenable to arthroscopic treatment, such as femoroacetabular impingement syndrome (FAIS) or labral tears. If the patient is symptomatic of both the HO and the concurrent intra-articular pathology, conservative treatment fails, and the location of the HO makes arthroscopic removal feasible, treatment of HO and concomitant pathology can take place simultaneously via hip arthroscopy.
In this Technical Note, we present techniques to remove HO arthroscopically, as well as tips on how to approach HO excision through an open approach. Arthroscopic HO excision can be technically challenging, because significant emphasis must be placed on maintenance of the soft tissues of the hip joint, including the joint capsule. Additionally, the unique osseous anatomy of each patient requires a personalized approach to HO excision. This Technical Note describes techniques that can be used to remove HO safely in both arthroscopically and arthroscopically assisted open approaches.
Arthroscopic Approach
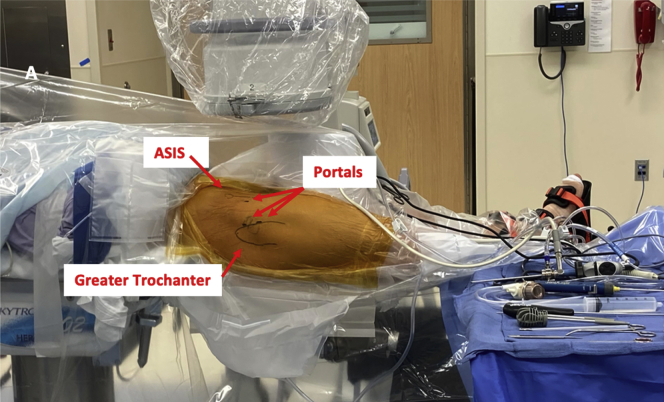
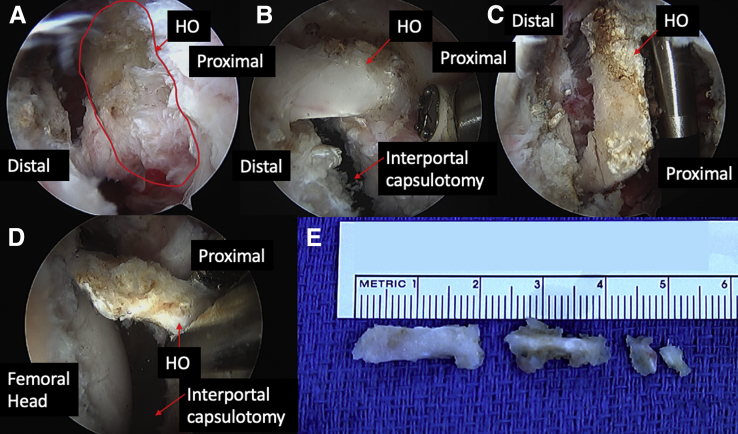
In the arthroscopic method, the patient is placed supine on a traction table with a standard hip arthroscopy setup (Table 1). The hip is then distracted approximately 1 cm, with either postless traction (the senior author’s current preferred method) or with a traction post (Fig 1). The joint is then accessed via an anterolateral portal created using the Seldinger technique and a midanterior portal created under direct visualization (Fig 2). An interportal cut is made using an arthroscopic knife for optimal central compartment access. At this point, the joint is examined. The labrum is visualized, and any labral pathology may be addressed. Depending on the location of the HO, the HO may be removed before or after any necessary cam or pincer decompression. In most cases, the HO does not impede central compartment work because cannulas can be placed either medial or lateral to the HO. Once the HO is located, often on taking the hip off of traction and flexing the hip to 30° to 45°, an ablation device is used to separate the HO from the surrounding soft tissue, removing as little soft tissue as necessary by directing the radiofrequency ablation device toward the bony fragment (Fig 3). Care must be taken not to damage the labral repair and to maintain the integrity of the joint capsule. Particular attention is paid to the proximal capsule flap, in anticipation of complete interportal capsulotomy repair at the completion of the case. Depending on the size of the HO, portal enlargement may be required, the HO piece may be fragmented and removed piecemeal, or an additional portal may be needed to approach the HO fragment with graspers or burrs. Once the labrum and HO have been addressed, a capsular repair is performed for the interportal capsulotomy (and T capsulotomy if one was created to remove the cam lesion at the femoral head-neck junction). Excess fluid is removed from the joint, and interrupted nylon sutures are used to close the portals before application of a sterile dressing.
Table 1.
Equipment Required for Hip Arthroscopy
| Hip Arthroscopy table: Stryker Guardian or Smith and Nephew traction table (with post or pink pad) |
| Crossflow Arthroscopy Pump (Stryker) |
| Entry Needles: Portal entry kit (Stryker) |
| Scope Cannulas: Flowport (Stryker) |
| Capsule Cutting: Samurai Full Radius (Stryker) |
| Labral Repair Suture Passer: Nanopass Crescent (Stryker) |
| Labral Anchors: Nanotack Flex (Stryker) |
| Labral Anchor Drill Bit: Nanotack Flex (Stryker) |
| Working Cannula: 6.5 mm × 90 mm Dri-lok (Stryker) |
| Capsule closure device: Slingshot 45° (Stryker) |
| Capsule closure suture: 1.2 mm Xbraid tape (Stryker) |
| Shaver Blade: 3.5 mm dual edge (Stryker) |
| Burr: 5.5 mm round (Stryker) |
| Radio Frequency Device: SERFAS Cruise (Stryker) |
Fig 1.
Patient positioning for the arthroscopic approach with the greater trochanter, anterior superior iliac spine, and portals marked
Fig 2.
Anterolateral and mid-anterior portals in place, with the outline of the greater trochanter and anterior superior iliac spine (ASIS) marked.
Fig 3.
In this left hip: (A) Heterotopic ossification (HO) visible during surgery, viewed through the anteromedial portal, outlined in red. (B) A radiofrequency ablation device is used to separate the HO while minimizing damage to the surrounding tissue. (C) A grasper is used to manipulate the HO into position for removal. (D) A grasper is used to remove the HO from the left hip. (E) Multiple removed HO fragments
Common Presentation/Indication
The treating physician should be suspicious of HO in the patient with pain or loss of range of motion in the setting of previous hip surgery, trauma, or chronic overuse injury that does not improve with physical therapy, rest, NSAIDS, or other conservative measures. Radiographs will provide definitive diagnosis. Arthroscopic removal of HO is indicated if the HO is located within the hip joint such that it can be accessed arthroscopically and is of a size that it can be removed arthroscopically or broken into smaller pieces with a burr or grasper, and then removed via arthroscopic portals. If the 3-dimensional (3D) quality of the HO is not appreciated on 2-dimensional radiographs, a low-dose, 3D computed tomography (CT) can clarify the location of the HO.
Patient Evaluation
The physician should evaluate range of motion, paying particular attention to hip internal and external rotation of the hip in supine extension and 90 degrees of flexion. Provocative tests include the Flexion ABduction External Rotation test (FABER), the Flexion ADduction Internal Rotation test (FADIR), and the Stinchfield test, as well as other provocative maneuvers, to evaluate for hip impingement, extra-articular impingement (including subspine, trochanteric pelvic, and ischiofemoral), and signs of instability (Table 2).9,10
Table 2.
| Maneuver | Technique | Interpretation |
|---|---|---|
| FADIR | Flex, ADduct, and Internally Rotate the hip in the supine position | Pain in the groin suggests FAI |
| FABER |
Flex, ABduct, and Externally Rotate the hip in the supine position |
Pain in the groin may indicate FAI or iliopsoas pathology |
| Subspine impingement sign | Passively flex the hip in the supine position | Anterior pain may indicate FAI |
| Lateral rim impingement sign | Externally rotate and abduct the hip while moving from flexion to extension | Pain may indicate FAI |
| Stinchfield | Resisted straight leg raise in the supine position | Pain or weakness may indicate intra-articular hip or iliopsoas pathology |
| Ischiofemoral impingement sign | Extend and externally rotate the hip in the prone position | Posterior pain may indicate impingement |
| Instability | Extend and externally rotate the hip in the prone position, while applying a downward pressure to the greater trochanter | Anterior pain is indicative of instability |
| Prone Apprehension Relocation Test (PART) | In the prone position, extend the hip 10 degrees while supporting the knee, abduct the hip 10-15 degrees, place downward pressure on the femur | Anterior pain, relieved when the downward pressure on the femur is released, is indicative of anterior acetabular undercoverage |
FAI, femoroacetabular impingement.
Imaging
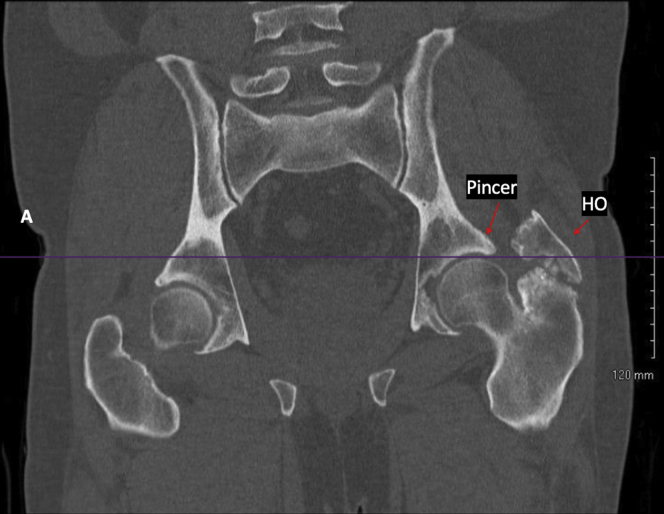
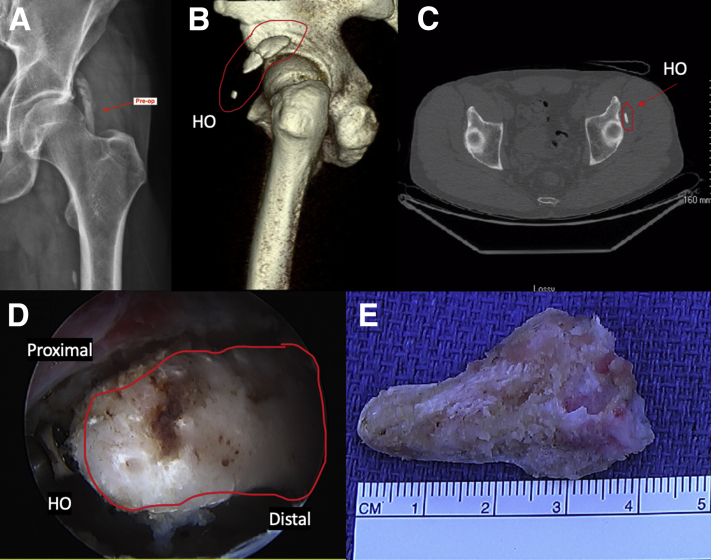
A standing radiograph and magnetic resonance imaging should be performed to evaluate for both bony and soft tissue abnormalities, which may be addressed concurrently with HO removal (Fig 4). Additional radiographs can include a 45° Dunn lateral to evaluate femoral head-neck offset and a false profile view to evaluate anterior acetabular coverage and subspine morphology. A CT scan can help to further delineate the location and borders of the HO. Most commonly, HO is located at the direct or indirect heads of the rectus femoris (Fig 5).
Fig 4.
Coronal computed tomography scan demonstrating heterotopic ossification within the hip abductors of the left hip, alongside cam and pincer lesions consistent with femoroacetabular impingement.
Fig 5.
(A) Preoperative left hip radiograph with heterotopic ossification (HO) visible, marked with arrow. (B) Three-dimensional computed tomography (CT) scan of the left hip with HO circled in red. (C) Axial CT scan with HO circled in red, just lateral to the acetabular rim of the left hip. (D) Intraoperative arthroscopic photo of HO and ablation device, visible through the anteromedial portal in the left hip. (E) Fragment of HO after excision.
Rehabilitation and Aftercare
HO prophylaxis should be prescribed postoperatively to prevent recurrence, unless the patient cannot tolerate NSAIDs. The senior author typically prescribes indomethacin 75 mg daily for 4 days, followed by Naprosyn 500 mg 2 times daily through postoperative day 30.
Open Approach
To perform an open HO excision, the patient is repositioned as necessary for the planned approach for open excision. In our video, a modified Gibson approach was used, so the patient was positioned in the lateral decubitus position. The patient’s incision from a previous intramedullary nail for femur fracture was marked and deemed too posterior to incorporate into the surgical incision (Fig 6). The dissection was carried down through the subcutaneous fat to the iliotibial band. The iliotibial band was incised, and the incision was carried superiorly along the anterior fibers of the gluteus maximus, per the modified Gibson approach.11 If HO is within the distal gluteus medius and minimus insertions, as is shown in our video, bone will be evident after the trochanteric bursa is excised (Fig 6). HO can be removed with the use of chisels in multiple pieces, with careful preservation of surrounding soft tissue. As we demonstrate in our video, tendons can be reapproximated to their anatomical positions and affixed to their insertions/origins with sutures or suture anchors. The overlying soft tissues are closed in layers, and a running absorbable suture can be used to close skin. In our demonstration, the gluteus medius and minimus tendons were reapproximated to the greater trochanter with suture anchors (Video 1).
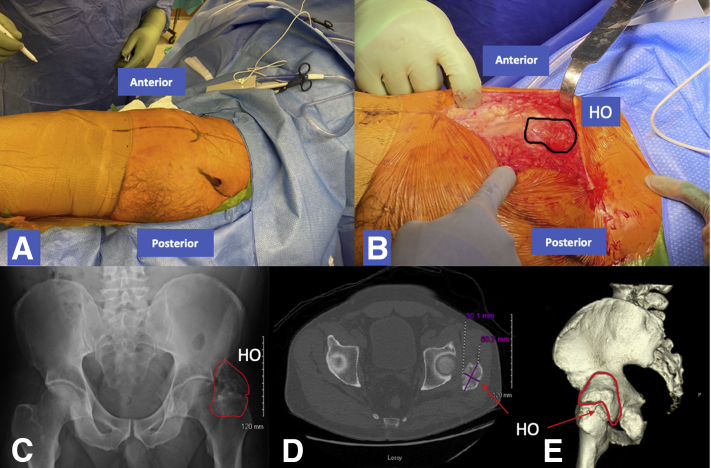
Fig 6.
(A) With the patient in the right lateral decubitus position, an incision for the modified Gibson approach is marked on the left hip. The patient’s previous incision from an intermedullary nail for a femur fracture is also marked. (B) After incision and soft tissue dissection the heterotopic ossification (HO) is visible within the insertions of the gluteus medius and minimus, circled in black. (C) HO visible on an anteroposterior radiograph of the left hip, circled in red, just superior to the greater trochanter and lateral to the femoral head of the left hip. (D) HO visible on an axial cut of the computed tomography (CT) scan, marked in purple, lateral to the left femoral head. (E) HO visible on a 3-dimensional CT scan of the left hip, circled in red.
Indications
An open approach is indicated if the HO is either too large to be removed arthroscopically or in a superficial location that is not accessible via arthroscope.
Patient Evaluation
Similar to the evaluation for the arthroscopic approach to HO excision, the physician should evaluate range of motion, paying particular attention to internal and external rotation of the hip in the supine position with the hip extended and flexed to 90°. Special tests to be performed include FABER, FADIR, Stinchfield test, extra-articular impingement (including subspine, trochanteric pelvic, and ischiofemoral) and for signs of instability (Table 2). It is important to detect any intra-articular pathology that may be addressed concurrently with the HO excision to determine the need for concomitant arthroscopic surgery.
Imaging
A standing radiograph and magnetic resonance imaging should be performed to evaluate for both bony and soft tissue abnormalities, which may be addressed concurrently with HO removal (Fig 4). Additional radiographs can include a 45° Dunn lateral to evaluate femoral head-neck offset and a false profile view to evaluate anterior acetabular coverage and subspine morphology. CT images can help to further delineate the location and borders of the HO.
Rehabilitation and Aftercare
HO prophylaxis should be prescribed to prevent recurrence. The senior author prescribes indomethacin 75 mg daily for 4 days, followed by Naprosyn 500 mg 2 times daily through postoperative day 30.
Discussion
HO is a well-known complication after hip arthroscopy, acute tendon avulsion, or chronic hip injury. Varying prophylaxis regimens are commonly prescribed to prevent HO form forming after hip surgery, although the literature describes a rate of 1.6% to 5.6% even with prophylaxis.3 It is thought that in patients without previous surgery or inciting trauma, repetitive mechanical stress or microtrauma may be the inciting factor for the formation of HO.12 In the athletic population, where chronic muscular injury or acute tendon avulsion is the most common cause of HO, it is most commonly found in the direct and indirect heads of the rectus femoris (at the anterior inferior iliac spine and superior acetabular ridge, respectively) or the origin of the sartorius at the anterior superior iliac spine. HO can be characterized using the Brooker classification system, which divides the HO into 4 classes. Class 1 consists of bony islands within the soft tissue about the hip. Class 2 adds bone spurs that may emanate from the pelvis or femur with at least 1 cm between their opposing surfaces. Class 3 includes bone spurs emanating from the pelvis or femur with less than 1 cm between their opposing surfaces, and Class 4 describes ankyloses of the hip. Notably, this classification system was developed for use in the post-total hip arthroplasty patient group.13
In this Technical Note we focus on the arthroscopic approach to removal of HO, as well as one open technique for HO about the hip joint. Combining the removal of HO with hip arthroscopy is one method for removal of HO in patients with or without concurrent intra-articular pathology, if the size and location of the HO make it amenable to arthroscopic removal. This technique mitigates the need for repositioning of the patient and the use of an additional open incision after completion of intra-articular surgical procedures. Arthroscopic surgery is also associated with quicker recovery times, lower complication rates, decreased opioid need, and higher patient satisfaction when compared to open surgery (Table 3). Arthroscopic surgery may also minimize the disruption of the surrounding soft tissue, which could decrease the risk of HO recurrence.14,15 Certain modifications during arthroscopy may be made, such as with portal placement, to accommodate removal of the HO fragments (Table 4).
Table 3.
Advantages, Risks, and Limitations
| Advantages to Arthroscopy |
| Faster recovery and earlier mobilization compared with open procedures |
| Less disruption of soft-tissue, potentially minimizing the risk of HO recurrence |
| Lower complication rates compared to open procedures |
| Risks with Arthroscopy |
| Risk of traction neurapraxia with a post (mitigated if post-less traction is used) |
| May necessitate conversion to open technique if initial access and visualization is not adequate, which may require repositioning of the patient, with separate prep and draping. |
| Use of the arthroscopic technique may be limited by the size and location of the HO in relation to the joint capsule |
HO, heterotopic ossification.
Table 4.
Pearls and Pitfalls
| Pearls |
| Most HO is located at the indirect and direct heads of the rectus femoris, so very often central compartment work can be accomplished around the existing HO. |
| Depending on the location of HO, the anterolateral and anteromedial portals may have to be modified slightly, but using the spinal needle to confirm trajectory before making skin incisions can be helpful. |
| Using the RF ablation device, facing the HO fragment, can allow for careful removal of the bone alone, with maintenance of the surrounding soft tissues. |
| Be prepared to remove the HO with a Kocher or locking grasper so that the fragment is not lost in soft tissues as the fragment is being removed. Portals may need to be enlarged, or additional percutaneous portals created for placement of grasping instruments. |
| Postoperative treatment with Indomethacin (75 mg extended release daily for 4 days) (with optional Naprosyn 500 mg twice daily from postoperative days 5-30) is recommended by the authors to prevent recurrence of HO. |
| Pitfalls |
| HO can be very vascular, so if using a burr to remove a fragment of bone, be prepared to use the RF device to obtain hemostasis. |
| HO must be mature before removal, because removing HO when it has not yet matured can lead to recurrence. The maturation process typically takes 8-10 weeks from the inciting injury.17 |
| If HO prevents entry into the central compartment, an outside-in approach can be used, where the peripheral compartment is accessed first, HO is arthroscopically removed, and then the central compartment is accessed. |
HO, heterotopic ossification; RF, radiofrequency.
In the open approach presented, a modified Gibson approach was used to access the lateral hip. This approach minimizes the risk of iatrogenic injury to the neurovascular supply of the gluteus maximus muscle and allows better anterosuperior visualization when compared to the Kocher-Langenback approach.11,16 Additional open approaches for removal of HO could include the Smith-Petersen approach, which would allow access to the common areas of HO formation (i.e., direct and indirect heads of the rectus) (Table 5). The Smith-Petersen approach provides anterior access to the hip joint. The initial incision is made just distal to the anterior superior iliac spine and continued distally down the anterior aspect of the proximal thigh. The internervous plane between the femoral and superior gluteal nerves is used superficially between the tensor fasciae latae and sartorius muscles and continued deeply between the rectus femoris and gluteus medius muscles to expose the anterior hip.16 One other consideration if removing more superficial HO is to use a small bikini incision.
Table 5.
Surgical Approaches for Heterotopic Ossification Removal about the Hip16
| Landmarks and Positioning | Incision | Superficial and Deep layers | Dangers | |
|---|---|---|---|---|
| Smith-Petersen | ASIS Iliac crest Greater trochanter Positioning: Supine |
Begin at the inferior aspect of the iliac crest, just below the ASIS. Continue distally about 10cm. | Superficial: Between the sartorius muscle and TFL Deep: Between the rectus femoris and the gluteus medius muscles |
Nerves:
|
| Modified Gibson | Great trochanter Iliac crest Shaft of the proximal femur Positioning: Lateral |
Begins midlateral on the thigh, extending 20-30 cm toward the tip of the greater trochanter, then proximally to the level of the iliac crest, in a straight incision | Superficial: TFL Deep: Gluteus maximus, abductors |
Nerves
|
ASIS, anterior superior iliac spine; LFCN, lateral femoral cutaneous nerve; TFL, tensor fasciae latae.
These approaches provide excellent visualization and access to different regions about the hip to perform excision of HO. Surgeons should consider these techniques when planning for HO excision in the context of concomitant intra-articular pathology.
Footnotes
The authors report the following potential conflict of interest or source of funding: D.C.G. is a paid consultant for Synthes. A.M.S. is a paid consultant for Stryker. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In this video we present numerous cases and associated imaging of symptomatic heterotopic ossification (HO). We discuss the arthroscopic excision of HO using a radiofrequency ablation device and grasper to remove the HO from the surrounding tissue and remove it from the joint space. We discuss the removal of HO in relation to other arthroscopic work, including labral repair, cam decompression, and capsule repair. We also show the modified Gibson approach as an example of 1 approach to remove HO through an open incision. We demonstrate preoperative and postoperative imaging of the cases presented and provide a summary of the presented techniques.
References
- 1.Redmond J.M., Keegan M.A., Gupta A., Worsham J.R., Hammarstedt J.E., Domb B.G. Outcomes of heterotopic ossification excision following revision hip arthroscopy. J Hip Preserv Surg. 2017;4:164–169. doi: 10.1093/jhps/hnx010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behery O.A., Dai A.Z., McLaurin T.M. Posttraumatic heterotopic ossification of the hip. J Orthop Trauma. 2018;32:S18–S19. doi: 10.1097/BOT.0000000000001197. [DOI] [PubMed] [Google Scholar]
- 3.Beckmann J.T., Wylie J.D., Kapron A.L., Hanson J.A., Maak T.G., Aoki S.K. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42:1359–1364. doi: 10.1177/0363546514526361. [DOI] [PubMed] [Google Scholar]
- 4.Zini R., Panascì M. Post-traumatic ossifications of the rectus femoris: Arthroscopic treatment and clinical outcome after 2 years. Injury. 2018;49:S100–S104. doi: 10.1016/j.injury.2018.09.062. [DOI] [PubMed] [Google Scholar]
- 5.Amar E., Sharfman Z.T., Rath E. Heterotopic ossification after hip arthroscopy. J Hip Preserv Surg. 2015;2:355–363. doi: 10.1093/jhps/hnv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranganathan K., Loder S., Agarwal S., et al. Heterotopic ossification: Basic-science principles and clinical correlates. J Bone Jt Surg Am. 2014;97:1101–1111. doi: 10.2106/JBJS.N.01056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vasileiadis G.I., Amanatullah D.F., Crenshaw J.R., Taunton M.J., Kaufman K.R. Effect of heterotopic ossification on hip range of motion and clinical outcome. J Arthroplasty. 2015;30:461–464. doi: 10.1016/j.arth.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 8.Ong C., Hall M., Youm T. Surgical technique arthroscopic treatment of heterotopic ossification of the hip after prior hip arthroscopy. Clin Orthop Relat Res. 2013;471:1277–1282. doi: 10.1007/s11999-012-2627-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frangiamore S., Mannava S., Geeslin A.G., Chahla J., Cinque M.E., Philippon M.J. Comprehensive clinical evaluation of femoroacetabular impingement: Part 1, Physical examination. Arthrosc Tech. 2017;6:e1993–e2001. doi: 10.1016/j.eats.2017.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spiker A.M., Fabricant P.D., Wong A.C., Suryavanshi J.R., Sink E.L. Radiographic and clinical characteristics associated with a positive PART (Prone Apprehension Relocation Test): a new provocative exam to elicit hip instability. J Hip Preserv Surg. 2020;7:288–297. doi: 10.1093/jhps/hnaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moed B.R. The modified gibson posterior surgical approach to the acetabulum. J Orthop Trauma. 2010;24:315–322. doi: 10.1097/BOT.0b013e3181c4aef8. [DOI] [PubMed] [Google Scholar]
- 12.Meyers C., Lisiecki J., Miller S., et al. Heterotopic ossification: A comprehensive review. JBMR Plus. 2019;3 doi: 10.1002/jbm4.10172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hug K.T., Alton T.B., Gee A.O. In brief: Classifications in brief: Brooker classification of heterotopic ossification after total hip arthroplasty. Clin Orthop Relat Res. 2015;473:2154–2157. doi: 10.1007/s11999-014-4076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nwachukwu B.U., Rebolledo B.J., McCormick F., Rosas S., Harris J.D., Kelly B.T. Arthroscopic versus open treatment of femoroacetabular impingement. Am J Sports Med. 2015;44:1062–1068. doi: 10.1177/0363546515587719. [DOI] [PubMed] [Google Scholar]
- 15.Botser I.B., Smith T.W., Nasser R., Domb B.G. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: A comparison of clinical outcomes. Arthroscopy. 2011;27:270–278. doi: 10.1016/j.arthro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Weiss D.B., Yarboro S.R., Browne J.A. In: Orthopaedic Surgical Approaches. 2nd ed. Miller M.D., Chhabra A.B., Park J.S., Shen F.H., Weiss D.B., Browne J.A., editors. Elsevier; Philadelphia: 2015. Hip and pelvis; pp. 267–338. [Google Scholar]
- 17.Devilbiss Z., Hess M., Ho G.W.K. Myositis ossificans in sport: A review. Curr Sports Med Rep. 2018;17:290–295. doi: 10.1249/JSR.0000000000000515. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In this video we present numerous cases and associated imaging of symptomatic heterotopic ossification (HO). We discuss the arthroscopic excision of HO using a radiofrequency ablation device and grasper to remove the HO from the surrounding tissue and remove it from the joint space. We discuss the removal of HO in relation to other arthroscopic work, including labral repair, cam decompression, and capsule repair. We also show the modified Gibson approach as an example of 1 approach to remove HO through an open incision. We demonstrate preoperative and postoperative imaging of the cases presented and provide a summary of the presented techniques.
In this video we present numerous cases and associated imaging of symptomatic heterotopic ossification (HO). We discuss the arthroscopic excision of HO using a radiofrequency ablation device and grasper to remove the HO from the surrounding tissue and remove it from the joint space. We discuss the removal of HO in relation to other arthroscopic work, including labral repair, cam decompression, and capsule repair. We also show the modified Gibson approach as an example of 1 approach to remove HO through an open incision. We demonstrate preoperative and postoperative imaging of the cases presented and provide a summary of the presented techniques.