Abstract
Aims
The primary aim of this study was to identify independent predictors associated with nonunion and delayed union of tibial diaphyseal fractures treated with intramedullary nailing. The secondary aim was to assess the Radiological Union Scale for Tibial fractures (RUST) score as an early predictor of tibial fracture nonunion.
Methods
A consecutive series of 647 patients who underwent intramedullary nailing for tibial diaphyseal fractures were identified from a trauma database. Demographic data, comorbidities, smoking status, alcohol consumption, use of non-steroidal anti-inflammatory drugs (NSAIDs), and steroid use were documented. Details regarding mechanism of injury, fracture classification, complications, and further surgery were recorded. Nonunion was defined as the requirement for revision surgery to achieve union. Delayed union was defined as a RUST score < 10 at six months postoperatively.
Results
There were 41 nonunions (6.3%), of which 13 were infected (31.7%), and 77 delayed unions (11.9%). There were 127 open fractures (19.6%). Adjusting for confounding variables, NSAID use (odds ratio (OR) 3.50; p = 0.042), superficial infection (OR 3.00; p = 0.026), open fractures (OR 5.44; p < 0.001), and high-energy mechanism (OR 2.51; p = 0.040) were independently associated with nonunion. Smoking (OR 1.76; p = 0.034), open fracture (OR 2.82; p = 0.001), and high-energy mechanism (OR 1.81; p = 0.030) were independent predictors associated with delayed union. The RUST score at six-week follow-up was highly predictive of nonunion (sensitivity and specificity of 75%).
Conclusion
NSAID use, high-energy mechanisms, open fractures, and superficial infection were independently associated with nonunion in patients with tibial diaphyseal fractures treated with intramedullary nailing. The six-week RUST score may be useful in identifying patients at risk of nonunion.
Cite this article: Bone Jt Open 2021;2(4):227–235.
Keywords: Nonunion, RUST, Intramedullary nail, Revision
Introduction
Tibial diaphyseal fractures are the most common long bone fracture, accounting for 2% of all adult fractures.1 Overall incidence is approximately 16.9 to 21.5 per 100,000 per year.2,3 The majority of these fractures are successfully managed with reamed intramedullary (IM) nailing, although nonunion remains a recognized outcome, complicating between 5% and 33% of injuries.4,5 Tibial shaft nonunion may cause considerable patient morbidity and require significant resources to manage.6,7 Furthermore, delayed union may also result in prolonged disability and prolonged absence from work.
There remains a paucity of evidence identifying factors that predict a patient’s risk of progression to nonunion following a tibial shaft fracture. Existing studies have been limited by small sample sizes,7 inclusion of limited prognostic factors being investigated,8 or assessed outcomes following both reamed and unreamed IM nails.8,9 Other studies have assessed the rate of deep infection following tibial IM nailing, which is known to have a clear association with nonunion.9-11
The Radiological Union Score for Tibial fractures (RUST) has garnered substantial attention as a useful tool in assessing tibial fracture healing.12,13 The role of the RUST score in enabling the early identification of patients at increased risk of nonunion has not been well explored.
The primary aim of this study was to identify independent predictors of aseptic nonunion and delayed union of tibial diaphyseal fractures treated with intramedullary nailing. The secondary aim was to assess the effectiveness of the RUST score as an early (six-week) predictor of tibial fracture nonunion following intramedullary nailing.
Methods
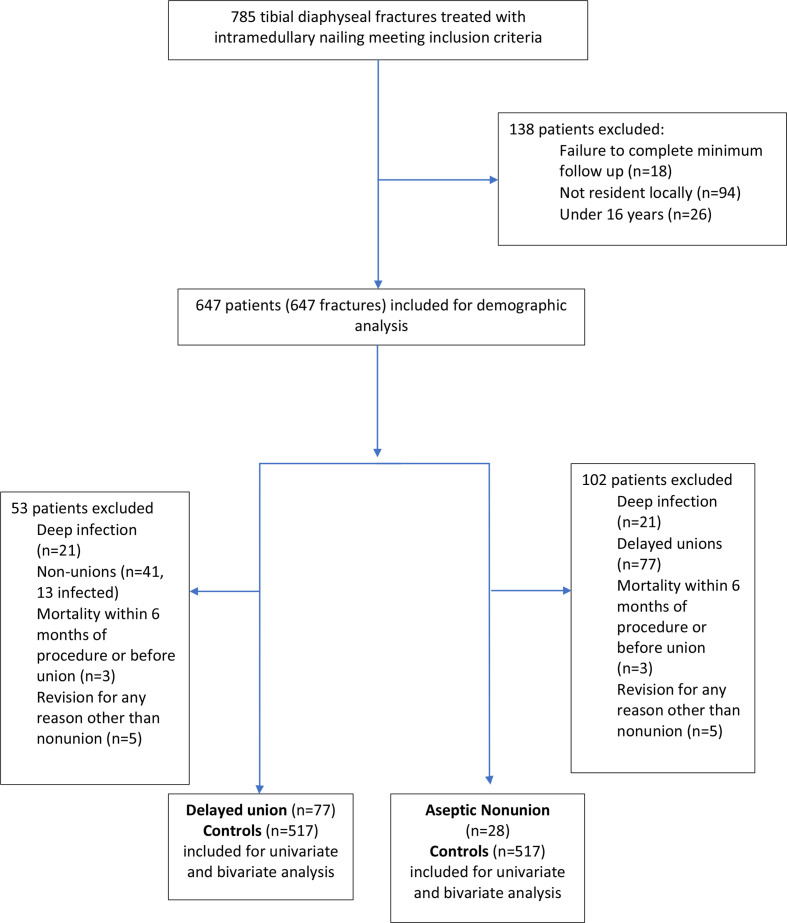
Ethical approval was not required, due to the retrospective nature of this study assessing routinely collected data. Electronic theatre logbooks were used to identify a consecutive series of patients undergoing reamed, locked IM nailing for a tibial diaphyseal fracture at a large university teaching hospital over an 11-year period (January 2008 to August 2019). During the study period, 785 IM nails were implanted in 785 patients. The study centre serves a catchment adult population of approximately 780,000.14 Casenotes and radiographs were reviewed. Patients who were aged under 16 years (n = 26), non-resident (n = 94), or lost to follow-up (prior to fracture union or any secondary operation to address nonunion, n = 18) were excluded. The study cohort comprised 647 consecutive patients who were included for retrospective analysis (Figure 1).
Fig. 1.
Identification of study cohort and subsequent inclusion for demographic and regression analyses.
Demographic data were collected, including age, sex, comorbidities, non-steroidal anti-inflammatory drug (NSAID) and steroid use, smoking status, and alcohol intake. NSAID use was defined according to documentation in the clinical notes as regular use at the time of surgery and during postoperative recovery to final follow-up. Injury characteristics, including mechanism of injury (low- or high-energy) and fracture classification (closed or open), were recorded. High-energy injuries comprised any falls from greater than standing height or road traffic collisions.
Postoperative complications, including development of superficial or deep infection, compartment syndrome, venous thromboembolism, cardiac, respiratory or cerebrovascular events, and the need for revision surgery were recorded. Infection was classified as either superficial or deep, according to Dellinger et al15 and Centers for Disease Control and Prevention guidelines. A superficial wound infection was one located above (superficial to) the deep fascia, defined clinically as infection at either the operative wound or the open wound if the fracture was compound, and recorded through documentation in the medical records. Deep infection involved the tissues deep to muscular fascia and involvement of bone, which required revision surgical intervention.
Treatment protocol
Surgery was undertaken at a median of one day (interquartile range (IQR) 1 to 2) post-injury. Surgical fixation at our centre is performed with reamed, locked IM nails (Stryker T2, USA or Smith or Nephew Trigen meta-nail, UK). Routine follow-up consisted of clinic review with radiographs at two weeks, six weeks, 12 weeks, and 16 weeks postoperatively.
At our centre the surgical intervention of choice for nonunion is exchange IM nailing. Other procedures used to treat nonunion included external fixator and fracture dynamization.
Nonunion and delayed union
Fracture union was defined as bridging callus in at least three out of four cortices on anteroposterior and lateral radiographs, with clinical correlation.16 Nonunion was defined as the lack of clinical or radiological evidence of healing, as determined by the attending surgeon, and which required revision surgical intervention.8 Delayed union was defined as a RUST score of less than 10 at six months post-injury, or fewer than three bridging cortices on orthogonal radiographs at six-month follow-up.13 RUST score was evaluated by two authors independently (NSM and JML), and mean score was used to assess predictive value for nonunion.
During analysis of the delayed and nonunion sub-groups, any patients with a deep infection were excluded. There is an established association between deep infection and tibial nonunion,9,11 and virtually all tibial nonunions due to deep infection would have a subsequent surgical intervention. Thus, the inclusion of these patients in the regression analysis was considered both unnecessary and at risk of confounding the relationship between other variables and impaired union.
To identify factors associated with nonunion, all deep infections (n = 21, of which 13 went on to nonunion), delayed unions (n = 77), patients who died within six months of procedure or before union (n = 3), and revision for any reason other than nonunion (n = 5) were excluded to minimize confounding bias. Similarly, all deep infections (n = 21), nonunions (n = 41) and revision for any reason other than nonunion (n = 5) were excluded for the purposes of identifying factors associated with delayed union.
Statistical analysis
Statistical analysis was performed using Statistical Product and Service Solutions version 17.0 (SPSS, USA) The relationship between groups of dichotomous variables was assessed using a chi-squared or Fisher’s exact test. For parametric continuous data an independent-samples t-test was used. Logistic regression was used to assess the independent influence of variables associated with nonunion and delayed union. Receiver operating characteristic (ROC) curve analysis was used to identify a threshold RUST score on the six-week radiograph, for use as a potential predictive tool associated with a patient progressing to nonunion. The area under the ROC curve (AUC) ranges from 0.5, indicating a test with no accuracy, to 1.0 where the test is perfectly accurate in identifying all patients progressing to nonunion. The threshold value was defined as the point at which the sensitivity and specificity were maximal in predicting nonunion.17 All variables that were significant on univariate analyses were included in the multivariate model. A p-value of < 0.05 was defined as statistically significant.
Results
The mean age of the cohort was 40.5 years (16.0 to 92.5) and 410 patients (63.3%) were male. A total of 38 patients (5.9%) had a history of diabetes mellitus. There were 127 open fractures (19.6%) and 184 (28.4%) fractures resulted from a high-energy mechanism.
Mean follow-up was 27 weeks (11 to 115). There were 41 nonunions (6.3%), of which 13 were infected (31.7%), and 77 delayed unions (11.9%). The overall superficial infection rate was 11.0% (n = 71/647) and deep infection rate 3.2% (n = 21/647).
Predictors of nonunion and delayed union
There were 28 aseptic nonunions and 517 controls for univariate and subsequent multivariate analysis. Unadjusted analysis demonstrated that smoking (odds ratio (OR) 2.42; p = 0.021), NSAID use (OR 4.48; p = 0.002), open fracture (OR 8.84; p < 0.001), high-energy mechanism (OR 4.29; p < 0.001), and superficial infection (OR 4.54; p < 0.001) were significantly associated with nonunion (Table I).
Table I.
Univariate analysis of factors associated with nonunion following intramedullary nailing of tibial diaphyseal fractures.
| Demographic detail | Nonunion (n = 28) | Control (n = 517) | OR/ difference (95% CI) | p-value |
|---|---|---|---|---|
| Sex, n (%) | 0.768 (0.341 to 1.731) | 0.523* | ||
| Male | 19 (67.9) | 319 (61.7) | ||
| Female | 9 (32.1) | 198 (38.3) | ||
| Mean age, yrs (SD) | 45.6 (14.8) | 41.6 (18.3) | 3.52 (-10.9 to 2.92) | 0.070† |
| Comorbidity, n (% of group) | ||||
| Diabetes mellitus | 1 (3.6) | 29 (5.6) | 0.626 (0.082 to 4.769) | 0.648* |
| Neuropathy | 0 (0) | 10 (1.9) | 0.981 (0.969 to 0.993) | 0.999‡ |
| Respiratory disease | 3 (10.7) | 53 (10.2) | 1.055 (0.308 to 3.613) | 0.999‡ |
| Osteoporosis | 1 (3.6) | 25 (4.8) | 0.732 (0.096 to 5.606) | 0.999‡ |
| Hypothyroid | 0 (0) | 17 (3.3) | 0.967 (0.952 to 0.983) | 0.999‡ |
| Vascular disease | 1 (3.6) | 7 (1.3) | 2.709 (0.322 to 22.813) | 0.345‡ |
| Social factors | ||||
| Smoking | 13 (46.4) | 137 (26.4) | 2.417 (1.121 to 5.208) | 0.021* |
| Alcohol excess | 7 (25) | 78 (15.0) | 1.885 (0.775 to 4.583) | 0.156* |
| NSAID use | 5 (17.9) | 24 (4.6) | 4.484 (1.569 to 12.817) | 0.002* |
| Steroid use | 0 (0) | 6 (1.2) | 0.988 (0.979 to 0.998) | 0.999‡ |
| Open fracture, n (% of group) | 16 (57.1) | 68 (13.1) | 8.843 (4.011 to 19.499) | < 0.001* |
| High-energy, n (% of group) | 16 (57.1) | 123 (23.7) | 4.293 (1.977 to 9.321) | < 0.001* |
| Complications, n (% of group) | ||||
| Superficial infection | 8 (28.6) | 42 (8.1) | 4.543 (1.187 to 10.936) | < 0.001* |
| Compartment syndrome | 2 (7.1) | 41 (7.9) | 1.115 (0.256 to 4.865) | 0.999‡ |
| DVT/PE | 1 (3.6) | 6 (1.2) | 3.167 (0.368 to 27.242) | 0.309‡ |
| Cardiac | 0 (0) | 0 (0) | N/A | N/A |
| CVA | 0 (0) | 2 (0.39) | 0.996 (0.991 to 1.001) | 0.999‡ |
Chi-squared test.
Independent-samples t-test.
Fisher’s exact test.
CI, confidence interval; CVA, cerebrovascular accident; DVT, deep-vein thrombosis; N/A, not available; NSAID, non-steroidal anti-inflammatory drugs; OR, odds ratio; PE, pulmonary embolism; SD, standard deviation.
When adjusting for confounding variables, NSAID use (OR 3.50; p = 0.042), open fracture (OR 5.44; p < 0.001), high-energy mechanism (OR 2.51; p = 0.040) and superficial infection (OR 3.00; p = 0.026) were independently associated with an increased risk of nonunion (Table II). Although smoking was not independently associated with nonunion, there was a trend towards statistical significance (p = 0.082), with an OR of 2.12.
Table II.
Regression analysis for factors associated with nonunion adjusting for confounding variables.
| Variable | OR (95% CI for Exp (B)) | p-value |
|---|---|---|
| Smoking status | 0.082 | |
| Non-smoker | Reference | |
| Smoker | 2.124 (0.910 to 4.958) | |
| NSAID use | 0.042 | |
| No NSAID postoperatively | Reference | |
| NSAID postoperaively | 3.503 (1.049 to 11.701) | |
| Fracture status | 0.000 | |
| Closed | Reference | |
| Open | 5.436 (2.259 to 13.077) | |
| Superficial infection | 0.026 | |
| Absent | Reference | |
| Present | 3.002 (1.140 to 7.905) | |
| Energy | 0.040 | |
| Low | Reference | |
| High | 2.513 (1.044 to 6.049) |
CI, confidence interval; NSAID, non-steroidal anti-inflammatory drugs; OR, odds ratio.
There were 77 delayed unions and 517 controls for univariate and subsequent multivariate analysis.Unadjusted analysis demonstrated that smoking (p = 0.022, OR 1.78), NSAID use (p = 0.011, OR 2.73), open fracture (p < 0.001, OR 3.38), and high-energy mechanism (p = 0.001, OR 2.29) were significantly associated with delayed union (Table III).
Table III.
Univariate analysis of factors associated with delayed union following intramedullary nailing of tibial diaphyseal fractures.
| Demographic detail | Delayed union (n = 77) | Control (n = 517) | OR/ difference (95% CI) | p-value |
|---|---|---|---|---|
| Sex, n (% of group) | 0.734 (0.439 to 1.23) | 0.237* | ||
| Male | 53 (68.8) | 319 (61.8) | ||
| Female | 24 (31.2) | 198 (38.3) | ||
| Mean age, yrs (SD) | 42.9 (15.8) | 42.0 (19.4) | 2.20 (-5.62 to 3.00) | 0.551† |
| Comorbidity, n (% of group) | ||||
| Diabetes mellitus | 6 (7.8) | 29 (5.6) | 1.428 (0.573 to 3.560) | 0.443* |
| Neuropathy | 4 (5.2) | 10 (1.9) | 2.789 (0.853 to 9.124) | 0.094‡ |
| Respiratory disease | 11 (14.3) | 53 (10.2) | 1.465 (0.729 to 2.947) | 0.281* |
| Osteoporosis | 3 (3.9) | 25 (4.8) | 0.801 (0.236 to 2.719) | 1.000‡ |
| Hypothyroid | 1 (1.3) | 17 (3.3) | 0.389 (0.051 to 2.962) | 0.493‡ |
| Vascular disease | 2 (2.6) | 7 (1.3) | 1.950 (0.398 to 9.565) | 0.328‡ |
| Social factors | ||||
| Smoking | 30 (39.0) | 137 (26.4) | 1.780 (1.082 to 2.928) | 0.022* |
| Alcohol excess | 15 (19.5) | 78 (15.0) | 1.368 (0.741 to 2.526) | 0.315* |
| NSAID use | 6 (7.8) | 24 (4.6) | 2.730 (1.218 to 6.118) | 0.011* |
| Steroid use | 0 (0) | 6 (12) | 0.988 (0.979 to 0.998) | 1.000‡ |
| Open fracture, n (% of group) | 26 (33.8) | 68 (13.1) | 3.381 (1.977 to 5.783) | < 0.001* |
| High-energy, n (% of group) | 45 (58.4) | 123 (23.7) | 2.289 (1.394 to 3.76) | 0.001* |
| Complications, n (% of group) | ||||
| Superficial infection | 6 (7.8) | 42 (8.1) | 0.960 (0.394 to 2.339) | 0.740* |
| Compartment syndrome | 9 (11.7) | 41 (7.9) | 1.543 (0.718 to 3.316) | 0.263* |
| DVT/PE | 0 (0) | 6 (1.2) | 0.988 (0.979 to 0.998) | 1.000* |
| Cardiac | 0 (0) | 0 (0) | N/A | N/A |
| CVA | 0 (0) | 2 (0.39) | 0.996 (0.991 to 1.00) | 1.000* |
Chi-squared test.
Student’s t-test.
Fisher’s exact test.
CI, confidence interval; CVA, cerebrovascular accident; DVT, deep vein thrombosis; N/A, not available; NSAID, non-steroidal anti-inflammatory drugs; OR, odds ratio; PE, pulmonary embolism; SD, standard deviation.
When adjusting for confounding variables, smoking (p = 0.034, OR 1.76), open fracture (p = 0.001, OR 2.82) and high-energy mechanism (p = 0.030, OR 1.81) were independently associated with increased risk of delayed union (Table IV). NSAID use was not independently significantly associated with delayed union, but demonstrated a trend towards significance (p = 0.093), with OR of 2.09.
Table IV.
Regression analysis for factors associated with delayed union adjusting for confounding variables.
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Smoking status | 0.034 | |
| Non-smoker | Reference | |
| Smoker | 1.756 (1.044 to 2.954) | |
| NSAID use | 0.093 | |
| No NSAID postoperatively | Reference | |
| NSAID postoperatively | 2.090 (0.885 to 4.938) | |
| Fracture status | 0.001 | |
| Closed | Reference | |
| Open | 2.821 (1.572 to 5.065) | |
| Energy | 0.030 | |
| Low | Reference | |
| High | 1.808 (1.058 to 3.090) |
CI, confidence interval; NSAID, non-steroidal anti-inflammatory drugs; OR, odds ratio.
RUST score as a predictor of nonunion
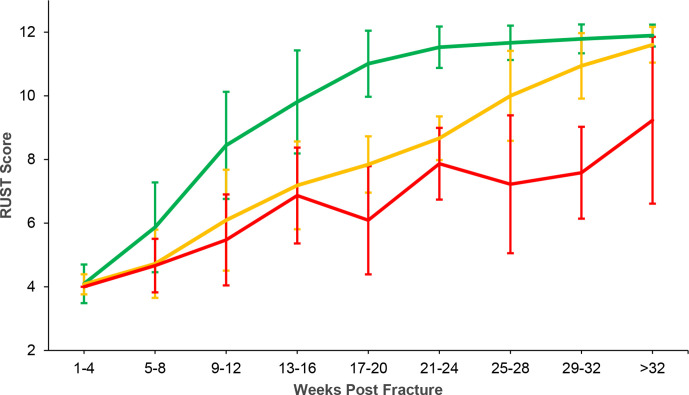
Mean time to union (using RUST score of ≥ 10, indicating more the three healed cortices) was 16.4 weeks (95% CI 12.6 to 20.2). Mean time to union in the delayed union group was 32.3 weeks (95% CI 22.9 to 41.7). Union rates for controls, delayed union, and nonunion groups are illustrated in Figure 2.
Fig. 2.
Healing rates for control group (green), delayed union group (yellow), and non-union group (red). RUST, Radiological Union Scale for Tibial fractures.
Receiver operating characteristic (ROC) curve analysis illustrated that, at six-week postoperative follow-up, the RUST score was an accurate predictor of fractures at risk of progressing to nonunion, with an area under the curve (AUC) of 75% (95% CI 66 to 84; p < 0.001) (Figure 3). Using the point of maximum sensitivity and specificity as the threshold value, a RUST score < 6 at six-week follow-up was 75% sensitive and 75% specific to predict nonunion. There were 22 patients who had a RUST < 6 at six weeks, of whom 16 (72.3%) went on to aseptic nonunion.
Fig. 3.
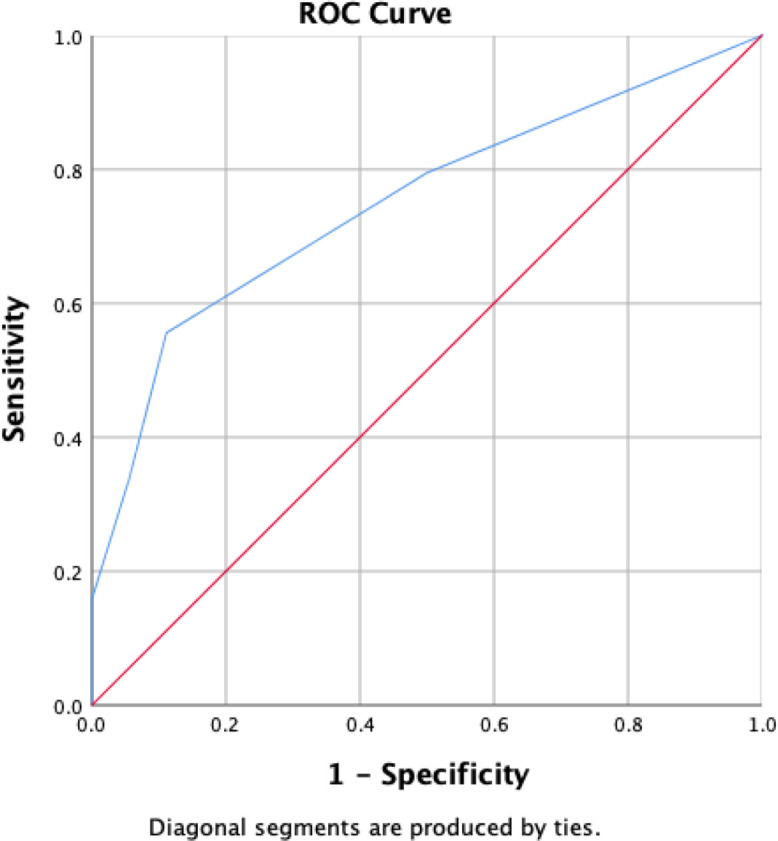
Receiver operative characteristic (ROC) curve for Radiological Union Scale for Tibial fractures score < 6 at six-week follow-up as a predictor of nonunion.
Discussion
This study has demonstrated that NSAID use, a high-energy injury mechanism, open fractures, and superficial infection were independently associated with increased risk of nonunion in patients undergoing IM nailing for a tibial diaphyseal fracture. Smoking, high-energy injuries, and open fractures were associated with an increased risk of delayed union. The use of the RUST score at six weeks postoperatively appears to be a sensitive and specific early predictor of fractures at risk of developing nonunion, and could serve as a useful prognostic tool to identify patients who may benefit from early intervention.
Predictors of nonunion
We found that open tibial diaphyseal fractures confer a five-fold increased risk nonunion, which is consistent with the current literature.18-20 In our series, almost one-third of nonunions had coexisting deep infection, which supports existing evidence demonstrating the association between deep infection and nonunion.9,11 Given this association, and to minimize confounding bias, all patients with deep infection were excluded from further analysis. Thus, factors which have been proposed to have an association with nonunion but remain poorly investigated could be more accurately analyzed.
NSAID use has been previously proposed to inhibit fracture healing. A number of animal and laboratory studies have supported this theory, however clinical studies have been inconclusive.21-23 Fader et al24 recently showed that NSAID use prolonged the average time to union of tibial diaphyseal fractures, however this difference was not statistically significant. We observed a significantly increased rate of nonunion with NSAID use. Further evidence in the form of prospective randomized controlled trials are required to verify this finding.
Independently, high-energy mechanisms conferred a two-fold increased risk of nonunion in our cohort, consistent with the literature.8,20 This is perhaps unsurprising given that higher-energy mechanisms imply increased fracture displacement, comminution, and soft-tissue compromise, all of which appear to be associated with nonunion.9,10
Our analysis identified that superficial wound infections conferred a three-fold increase in nonunion risk. We are not aware of any previous studies reporting an association between superficial infection and tibial shaft nonunion. Our findings suggest that, in some instances, observation of a superficial wound infection may conceal a deeper infection. Surgeons may therefore need to consider careful assessment and further imaging for patients with clinical superficial infections, given their association with a greater risk of nonunion. An alternative explanationcould be that there is overlap between patient and injury factors that predispose to superficial wound infection, and those that increase nonunion risk. Although the reasons why superficial infection should increase nonunion risk are beyond the scope of this study, we have attempted to adjust for this overlap in our regression analysis.
Our study did not identify an independent association between the presence of diabetes and an increased risk of delayed union or nonunion. Aderinto et al25 noted a trend for diabetic patients to have an increased frequency of delayed union and nonunion following IM nailing of the tibia, although this did not reach statistical significance. It may be that the small number of diabetic patients identified in this series (n = 28) and other studies accounts for the lack of convincing evidence linking diabetes to nonunion. Our exclusion of patients with deep infection in regression analysis may also have eliminated a possible correlation.
Delayed union
Smoking, open fractures, and high-energy injuries were independently associated with an increased risk of delayed union. Our definition of delayed union, based on the RUST score, uses a reliable and consistent method of evaluating tibial shaft fracture healing. This has been a limitation in prior studies, which have often used varying definitions.20,23
The association between smoking and nonunion trended towards statistical significance on multivariate analysis. Previous literature has identified smoking as a risk factor for both delayed and nonunion in tibial diaphyseal fractures treated with IM nailing.26,27 It may be that our sample size of aseptic nonunions was not large enough to identify a potentially significant association between smoking and nonunion, and the larger sample size of aseptic delayed unions was able to identify this association. The relatively small sample size of aseptic nonunions in our cohort could mean that this observation was the result of a type II error.
A similarly evident finding was that NSAIDs, which were found to be significantly associated with nonunion, were not associated with delayed union. This may represent a type 1 error for nonunion or a type 2 error for delayed union due to the limited sample size of patients comprising these cohorts. Furthermore, this may reflect sampling bias as those patients who developed a nonunion were not included in the delayed union model and vice versa. Therefore, a patient on NSAIDs who developed a nonunion was not included in the delayed union model, which could have resulted in this variable not being associated with delayed union. An alternative explanation is that the mechanisms of delayed union and nonunion are different and thus differentially affected by NSAIDs. Marsh et al28 described that delayed union occurs through development of late intramedullary callus with periosteal osteogenesis having ceased, in contrast to nonunion which develops through cessation of both endosteal and periosteal osteogenesis. NSAIDS may disproportionately induce the cessation of periosteal osteogenesis through inhibition of prostaglandin production, but may not affect intramedullary callus formation. Further basic science studies are required to investigate the specific mechanisms by which NSAIDs contribute to delayed and nonunion.
The RUST score and prediction of nonunion
We found a RUST score of < 6 at six-week follow-up to be a sensitive and specific predictor of subsequent nonunion. Ross et al29 reported that their nonunion cohort had a mean RUST score of 5.4 at the six-week timepoint, which supports the use of our threshold score for predicting nonunion. They did not perform ROC analysis to determine a sensitivity or specificity for their predictive model. Using the six-week RUST score of < 6 would have identified the majority (57.1%, n = 16/28) of patients that developed an aseptic nonunion. Early identification of this smaller group of “at risk” patients may allow for targeted intervention to reduce the nonunion risk. In addition, patients in this “at risk” group with a RUST score of < 6 could be further classified according to the risk factors associated with nonunion identified in this study to assign their own risk of nonunion.
There are few prior studies that have attempted to assess the value of the postoperative RUST score in predicting nonunion following tibial diaphyseal fractures.29,30 Mundi et al30 showed in a retrospective analysis of 155 tibial fracture patients that the three-month RUST score was highly predictive of nonunion at 12 months, with a mean score of 4.8. Prior literature has shown the strong predictive value of cortical bridging and subsequent union rates,31 however this is a subjective method of radiological assessment and has been largely superseded by objective assessment.13,32,33 Identifying a threshold score at the six-week timepoint, as has been attempted for other nonoperatively managed fractures such as those involving the humeral shaft,34 may enable surgeons to identify patients at risk of nonunion at a relatively early postoperative stage, thus facilitating more frequent monitoring and early intervention.
Strengths and limitations
The strengths of this study include the assessment of a large, consecutive cohort of patients undergoing reamed IM nailing for tibial diaphyseal fractures at a single university hospital. Previous literature has included cohorts with variable methods of management, comprising fractures managed nonoperatively, with framing, and with plate fixation.8 In studies where only IM nailing has been considered, both reamed and unreamed nails have often been included, with variability or a lack of clarity in locking status.10,35 We included a number of variables which have been proposed to have an association with impaired fracture healing.8,20 We assessed the association of these variables with both nonunion and delayed union, whereas previous literature has assessed only nonunion, or merged nonunion and delayed union into a single entity.8,20 We used a validated method of quantifying delayed union through the RUST score.
The principal limitation of this study was its retrospective design. A number of patients were therefore excluded due to loss to follow-up or having incomplete data. Exclusion of patients could theoretically add bias to our cohort, however we attempted to limit this through our strict selection criteria and specific exclusions from regression analysis.
Subgroup analysis of nonunions and delayed unions involved relatively small sample sizes, after patients were excluded due to the presence of coexisting deep infection and revision surgery for reasons other than nonunion. The factors demonstrated to be associated with nonunion and delayed union were consistent with previous studies.8,20,23 Prior literature has highlighted the importance of cortical contact and fracture gap when assessing risk factors for nonunion.8,23,36,37 However, two authors (NSM and JFK) independently reviewed all postoperative radiographs for patients proceeding to nonunion (n = 41); none were identified as having significant malreduction, bone loss or distraction (> 1 mm).
Patients who self-dynamized due to screw breakage and went on to union were not classed as nonunion in out cohort. However, on review seven patients were noted from our cohort to have screw breakage. We do recognize that by not considering those patients who have self-dynamized in the nonunion group, we may have underestimated the true incidence of nonunion without further intervention.
Nonunion was limited to patients requiring further surgical intervention with revision. It is worth noting that a limitation of prior studies to date has been the inconsistent and wide-ranging definitions for nonunion.8,10 There remains a lack of consensus regarding the assessment of bony union, for which there are currently no available standard criteria.
In conclusion, we identified that NSAID use, high-energy injuries, open fractures, and superficial wound infections were independent risk factors for nonunion following reamed, locked IM nailing for tibial diaphyseal fractures. We also identified independent risk factors associated with delayed union, comprising of smoking, open fractures, and high-energy mechanisms. Finally, we identified the RUST score at six weeks postoperatively as an accurate early predictor of patients at increased risk of nonunion, which may enhance the management of such patients.
Footnotes
Author contributions: N. S. Makaram: Conceptualized the project, Collected the data, Conducted the statistical analysis, Prepared the manuscript.
J. M. Leow: Collected the data, Prepared the manuscript.
N. D. Clement: Conducted the statistical analysis, Prepared the manuscript.
W. M. Oliver: Collected the data, Prepared the manuscript.
Z. H. Ng: Collected the data, Prepared the manuscript.
C. Simpson: Collected the data, Prepared the manuscript.
J. F. Keating: Conceptualized the project, Prepared the manuscript.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Twitter: Follow N. S. Makaram @MakOrtho
Follow J. M. Leow @leowjunmin
Follow W. M. Oliver @OrthoOliver
Follow Z. H. Ng @DZH_Ng
Follow Edinburgh Orthopaedics @EdinOrthopaedic
References
- 1. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 2. Larsen P, Elsoe R, Hansen SH, Graven-Nielsen T, Laessoe U, Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury. 2015;46(4):746–750. [DOI] [PubMed] [Google Scholar]
- 3. Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29(7):529–534. [DOI] [PubMed] [Google Scholar]
- 4. Court-Brown CM, Keating JF, Christie J, McQueen MM. Exchange intramedullary nailing. its use in aseptic tibial nonunion. J Bone Joint Surg Br. 1995;77-B(3):407–411. [PubMed] [Google Scholar]
- 5. Wu CC, Shih CH, Chen WJ, Tai CL. High success rate with exchange nailing to treat a tibial shaft aseptic nonunion. J Orthop Trauma. 1999;13(1):33–38. [DOI] [PubMed] [Google Scholar]
- 6. Dahabreh Z, Calori GM, Kanakaris NK, Nikolaou VS, Giannoudis PV. A cost analysis of treatment of tibial fracture nonunion by bone grafting or bone morphogenetic protein-7. Int Orthop. 2009;33(5):1407–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dahabreh Z, Dimitriou R, Giannoudis PV. Health economics: a cost analysis of treatment of persistent fracture non-unions using bone morphogenetic protein-7. Injury. 2007;38(3):371–377. [DOI] [PubMed] [Google Scholar]
- 8. Fong K, Truong V, Foote CJ, et al. . Predictors of nonunion and reoperation in patients with fractures of the tibia: an observational study. BMC Musculoskelet Disord. 2013;14(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schemitsch EH, Bhandari M, Guyatt G, et al. . Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. 2012;94-A(19):1786–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Metsemakers W-J, Handojo K, Reynders P, Sermon A, Vanderschot P, Nijs S. Individual risk factors for deep infection and compromised fracture healing after intramedullary nailing of tibial shaft fractures: a single centre experience of 480 patients. Injury. 2015;46(4):740–745. [DOI] [PubMed] [Google Scholar]
- 11. Galvain T, Chitnis A, Paparouni K, Tong C, Holy CE, Giannoudis PV. The economic burden of infections following intramedullary nailing for a tibial shaft fracture in England. BMJ Open. 2020;10(8):e035404–e04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Whelan DB, Bhandari M, Stephen D, et al. . Development of the radiographic Union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma. 2010;68(3):629–632. [DOI] [PubMed] [Google Scholar]
- 13. Leow JM, Clement ND, Tawonsawatruk T, Simpson CJ, Simpson AHRW. The radiographic Union scale in tibial (rust) fractures: reliability of the outcome measure at an independent centre. Bone Joint Res. 2016;5(4):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. No authors listed . National Records of Scotland. https://www.nrscotland.gov.uk/ (date last accessed 6 April 2021).
- 15. Dellinger EP, Miller SD, Wertz MJ, Grypma M, Droppert B, Anderson PA. Risk of infection after open fracture of the arm or leg. Arch Surg. 1988;123(11):1320–1327. [DOI] [PubMed] [Google Scholar]
- 16. Shisha T. Parameters for defining efficacy in fracture healing. Clin Cases Miner Bone Metab. 2010;7(1):15–16. [PMC free article] [PubMed] [Google Scholar]
- 17. Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. et al. [DOI] [PubMed] [Google Scholar]
- 18. Mundi R, Axelrod D, Heels-Ansdell D, et al. . Nonunion in patients with tibial shaft fractures: is early physical status associated with fracture healing? Cureus. 2020;12(4):e7649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karladani AH, Granhed H, Kärrholm J, Styf J. The influence of fracture etiology and type on fracture healing: a review of 104 consecutive tibial shaft fractures. Arch Orthop Trauma Surg. 2001;121(6):325–328. [DOI] [PubMed] [Google Scholar]
- 20. Audigé L, Griffin D, Bhandari M, Kellam J, Rüedi TP. Path analysis of factors for delayed healing and nonunion in 416 operatively treated tibial shaft fractures. Clin Orthop Relat Res. 2005;438:221–232. [DOI] [PubMed] [Google Scholar]
- 21. Adolphson P, Abbaszadegan H, Jonsson U, Dalén N, Sjöberg HE, Kalén S. No effects of piroxicam on osteopenia and recovery after Colles’ fracture. A randomized, double-blind, placebo-controlled, prospective trial. Arch Orthop Trauma Surg. 1993;112(3):127–130. [DOI] [PubMed] [Google Scholar]
- 22. Davis TR, Ackroyd CE. Non-Steroidal anti-inflammatory agents in the management of Colles’ fractures. Br J Clin Pract. 1988;42(5):184–189. [PubMed] [Google Scholar]
- 23. Bhandari M, Tornetta P, Sprague S, et al. . Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma. 2003;17(5):353–361. [DOI] [PubMed] [Google Scholar]
- 24. Fader L, Whitaker J, Lopez M, et al. . Tibia fractures and NSAIDs. does it make a difference? A multicenter retrospective study. Injury. 2018;49(12):2290–2294. [DOI] [PubMed] [Google Scholar]
- 25. Aderinto J, Keating JF. Intramedullary nailing of fractures of the tibia in diabetics. J Bone Joint Surg Br. 2008;90-B(5):638–642. [DOI] [PubMed] [Google Scholar]
- 26. Schmitz MA, Finnegan M, Natarajan R, Champine J. Effect of smoking on tibial shaft fracture healing. Clin Orthop Relat Res. 1999;365:184–200. [DOI] [PubMed] [Google Scholar]
- 27. Dailey HL, Wu KA, Wu P-S, McQueen MM, Court-Brown CM, , PS W. Tibial fracture nonunion and time to healing after Reamed intramedullary nailing: risk factors based on a single-center review of 1003 patients. J Orthop Trauma. 2018;32(7):e263–e69. [DOI] [PubMed] [Google Scholar]
- 28. Marsh D, Lane JM. Concepts of fracture Union, delayed union, and nonunion. Clin Orthop Relat Res. 1998;355(355 Suppl):S22–S30. [DOI] [PubMed] [Google Scholar]
- 29. Ross KA, O’Halloran K, Castillo RC, et al. . Prediction of tibial nonunion at the 6-week time point. Injury. 2018;49(11):2075–2082. [DOI] [PubMed] [Google Scholar]
- 30. Mundi R, Axelrod D, Chaudhry H, et al. . Association of three-month radiographic Union score for tibia fractures (rust) with nonunion in tibial shaft fracture patients. Cureus. 2020;12(5):e8314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lack WD, Starman JS, Seymour R, et al. . Any cortical bridging predicts healing of tibial shaft fractures. J Bone Joint Surg Am. 2014;96-A(13):1066–1072. [DOI] [PubMed] [Google Scholar]
- 32. Litrenta J, Tornetta P, Mehta S, et al. . Determination of radiographic healing: an assessment of consistency using rust and modified rust in Metadiaphyseal fractures. J Orthop Trauma. 2015;29(11):516–520. [DOI] [PubMed] [Google Scholar]
- 33. Franzone JM, Finkelstein MS, Rogers KJ, Kruse RW. Evaluation of fracture and osteotomy Union in the setting of osteogenesis imperfecta: reliability of the modified radiographic Union score for tibial fractures (rust). J Pediatr Orthop. 2020;40(1):48–52. [DOI] [PubMed] [Google Scholar]
- 34. Oliver WM, Smith TJ, Nicholson JA, et al. . The radiographic Union score for humeral fractures (RUSHU) predicts humeral shaft nonunion. Bone Joint J. 2019;101-B(10):1300–1306. [DOI] [PubMed] [Google Scholar]
- 35. Hendrickx LAM, Virgin J, van den Bekerom MPJ, Doornberg JN, Kerkhoffs GMMJ, Jaarsma RL. Complications and subsequent surgery after intra-medullary nailing for tibial shaft fractures: review of 8110 patients. Injury. 2020;51(7):1647–1654. [DOI] [PubMed] [Google Scholar]
- 36. Panjabi MM, Walter SD, Karuda M, White AA, Lawson JP. Correlations of radiographic analysis of healing fractures with strength: a statistical analysis of experimental osteotomies. J Orthop Res. 1985;3(2):212–218. [DOI] [PubMed] [Google Scholar]
- 37. Oni OO, Dunning J, Mobbs RJ, Gregg PJ. Clinical factors and the size of the external callus in tibial shaft fractures. Clin Orthop Relat Res. 1991;273:278–283. [PubMed] [Google Scholar]