Abstract
The World Health Organization (WHO) set targets for a 90% reduction in the incidence of syphilis and gonorrhoea between 2018 and 2030. We review trends in sexually transmitted infections in the WHO South-East Asia Region to assess the feasibility of reaching these targets. Myanmar, Sri Lanka and Thailand reported 90% or greater reductions in the incidence or prevalence of syphilis and/or gonorrhoea between 1975 and 2005. Evidence suggests that smaller, more recent reductions in trends in sexually transmitted infections in India have driven regional declines. In other countries, sexually transmitted infections remain high or are increasing or data are not reliable enough to measure change. Sri Lanka and Thailand have strong control programmes for sexually transmitted infections that ensure universal access to services for these infections and targeted interventions in key populations. India and Myanmar have implemented targeted control efforts on a large scale. Other countries of the region have prioritized control of human immunodeficiency virus, and limited resources are available for other sexually transmitted infections. At national and subnational levels, data show rapid declines in sexually transmitted infections when targeted promotion of condom use and sexually transmitted infection services are scaled up to reach large numbers of sex workers. In contrast, recent outbreaks of sexually transmitted infections in underserved populations of men who have sex with men have been linked to rising trends in sexually transmitted infections in the region. A renewed and focused response to sexually transmitted infections in the region is needed to meet global elimination targets.
Résumé
L'Organisation mondiale de la Santé (OMS) a fixé des objectifs pour réduire à 90% l'incidence de la syphilis et de la gonorrhée entre 2018 et 2030. Nous avons étudié les tendances en matière d'infections sexuellement transmissibles dans la Région d'Asie du Sud-Est de l'OMS afin d'évaluer la faisabilité de ces objectifs. Le Myanmar, le Sri Lanka et la Thaïlande ont signalé une diminution de 90% ou plus dans l'incidence ou la prévalence de la syphilis et/ou de la gonorrhée entre 1975 et 2005. Les données semblent indiquer une tendance à la baisse plus récente et moins significative des infections sexuellement transmissibles en Inde, entraînant une décrue régionale. Dans d'autres pays, soit le nombre d'infections sexuellement transmissibles demeure élevé ou continue sa progression, soit les informations disponibles ne sont pas suffisamment fiables pour en mesurer l'évolution. Le Sri Lanka et la Thaïlande ont établi de solides programmes de lutte contre les infections sexuellement transmissibles, permettant d'accéder à des services spécialement conçus pour leur prise en charge et prévoyant une intervention ciblée au sein des populations clés. De leur côté, l'Inde et le Myanmar ont déployé des efforts à grande échelle afin de mener des actions ciblées. D'autres pays de la région ont privilégié la lutte contre le virus de l'immunodéficience humaine; pour les autres infections sexuellement transmissibles, leurs ressources sont limitées. Aux niveaux national et infranational, les données révèlent un rapide déclin des infections sexuellement transmissibles lorsque la promotion ciblée pour encourager l'usage du préservatif et les services dédiés à la prise en charge de telles affections sont renforcés afin de toucher un plus grand nombre de travailleurs du sexe. En revanche, les épidémies d'infections sexuellement transmissibles observées dernièrement au sein de populations défavorisées d'hommes ayant des relations sexuelles avec d'autres hommes ont entraîné une hausse dans la région. Il est donc indispensable d'apporter une réponse remaniée et ciblée face aux infections sexuellement transmissibles dans la région en vue d'atteindre les objectifs mondiaux d'élimination.
Resumen
La Organización Mundial de la Salud (OMS) fijó como objetivo una reducción del 90% en la incidencia de la sífilis y la gonorrea entre 2018 y 2030. Revisamos las tendencias de las infecciones de transmisión sexual en la Región del Sudeste Asiático de la OMS para evaluar la viabilidad de alcanzar estos objetivos. Myanmar, Sri Lanka y Tailandia informaron de reducciones del 90% o más en la incidencia o prevalencia de sífilis y/o gonorrea entre 1975 y 2005. Los datos sugieren que las reducciones más pequeñas y recientes en las tendencias de las infecciones de transmisión sexual en la India han impulsado los descensos regionales. En otros países, las infecciones de transmisión sexual siguen siendo elevadas o están aumentando, o los datos no son lo suficientemente fiables como para medir el cambio. Sri Lanka y Tailandia tienen sólidos programas de control de las infecciones de transmisión sexual que garantizan el acceso universal a los servicios para estas infecciones e intervenciones específicas en poblaciones clave. India y Myanmar han implementado esfuerzos de control específicos a gran escala. Otros países de la región han dado prioridad a la lucha contra el virus de la inmunodeficiencia humana y disponen de recursos limitados para otras infecciones de transmisión sexual. A nivel nacional y subnacional, los datos muestran un rápido descenso de las infecciones de transmisión sexual cuando se amplía la promoción del uso del preservativo y los servicios para las infecciones de transmisión sexual para llegar a un gran número de profesionales del ámbito sexual. Por el contrario, los recientes brotes de infecciones de transmisión sexual en poblaciones desatendidas de hombres que tienen relaciones sexuales con otros hombres se han relacionado con las tendencias al alza de las infecciones de transmisión sexual en la región. Se necesita una respuesta renovada y centrada en las infecciones de transmisión sexual en la región para alcanzar los objetivos mundiales de eliminación.
ملخص
وضعت منظمة الصحة العالمية (WHO) أهدافًا لخفض بنسبة 90% في الإصابة بالزهري والسيلان بين عامي 2018 و2030. نحن نقوم بمراجعة الاتجاهات في الأمراض المنقولة جنسيًا في منطقة جنوب شرق آسيا التابعة لمنظمة الصحة العالمية، لتقييم جدوى الوصول إلى هذه الأهداف. أعلنت كل من ميانمار وسري لانكا وتايلند عن انخفاضات بنسبة 90% أو أكبر في الإصابة بالزهري و/أو السيلان، وانتشارهما بين عامي 1975 و2005. وتشير الدلائل إلى أن الانخفاضات الأصغر والأحدث في اتجاهات الإصابة بالأمراض المنقولة جنسيًا في الهند قد حفزت حدوث انخفاضات إقليمية. في بلدان أخرى، تظل الأمراض المنقولة جنسياً مرتفعة، أو متجهة للازدياد، أو أن البيانات غير موثوقة بشكل كاف لقياس التغيير. يوجد لدى كل من سري لانكا وتايلند برامج قوية لمكافحة الأمراض المنقولة جنسياً والتي تضمن الوصول الشامل إلى خدمات هذه الأمراض والتدخلات المستهدفة في الفئات السكانية الرئيسية. قامت كل من الهند وميانمار بتنفيذ جهود المكافحة المستهدفة على نطاق واسع. منحت بلدان أخرى في المنطقة الأولوية لمكافحة فيروس نقص المناعة البشرية، مع توفير موارد محدودة للأمراض الأخرى المنقولة جنسياً. على المستويين الوطني ودون الوطني، توضح البيانات انخفاضًا سريعًا في الأمراض المنقولة جنسياً عندما يتم توسيع نطاق الترويج المستهدف لاستخدام الواقي الذكري، وخدمات الأمراض المنقولة جنسياً للوصول إلى أعداد كبيرة من المشتغلين بالجنس. في المقابل، فإن الحالات الحديثة لتفشي الأمراض المنقولة جنسياً بين فئات السكان المحرومين من الخدمات من الرجال الذين يمارسون الجنس مع الرجال، قد ارتبطت بالاتجاهات المتزايدة في الأمراض المنقولة جنسياً في المنطقة. هناك حاجة إلى استجابة متجددة ومركزة للأمراض المنقولة جنسياً في المنطقة، وذلك بهدف تلبية الأهداف العالمية للقضاء على الأمراض.
摘要
世界卫生组织 (WHO) 制定了目标,计划在 2018 年至 2030 年期间将梅毒和淋病发病率降低 90%。我们回顾了 WHO 东南亚地区性传播感染的趋势,以评估实现这些目标的可行性。缅甸、斯里兰卡和泰国报告在 1975 年至 2005 年期间梅毒和/或淋病的发病率或患病率下降了 90% 以上。有证据表明,印度性传播感染趋势近期出现较小幅度的降低,这一结果推动了地区性疾病的减少。在其他国家,性传播感染仍居高不下,或者正在增加,或者数据不足以衡量变化。斯里兰卡和泰国针对性传播感染制定了强有力的控制计划,确保普及针对这些感染的服务,并在关键人群中采取针对性干预措施。印度和缅甸大规模实施了有针对性的防控工作。该地区的其他国家已将人类免疫缺陷病毒的控制列为优先工作事项,用于其他性传播感染的资源有限。数据显示,在国家和国家以下各级层面,当有针对性地推广使用避孕套和扩大针对性传播感染的服务,以便可以惠及大量性工作者时,性传播感染率迅速下降。相比之下,最近在医疗资源不足地区的男男性行为者中爆发的性传播感染,与该地区性传播感染的上升趋势有一定的联系。为了实现全球消除目标,需要针对该地区的性传播感染侧重点重新制定新的应对措施。
Резюме
Всемирная организация здравоохранения (ВОЗ) определила цели по снижению заболеваемости сифилисом и гонореей на 90% в период с 2018 по 2030 год. Авторы анализируют тенденции распространения инфекций, передаваемых половым путем, в регионе Юго-Восточной Азии ВОЗ, чтобы оценить возможность достижения этих целей. Мьянма, Таиланд и Шри-Ланка сообщили о сокращении заболеваемости или распространенности сифилиса и (или) гонореи в период с 1975 по 2005 год на уровне 90% или выше. Факты свидетельствуют о том, что недавнее не такое масштабное снижение тенденций инфекций, передаваемых половым путем в Индии, привело к снижению на региональном уровне. В других странах число инфекций, передаваемых половым путем, остается высоким или продолжает расти либо данные недостаточно надежны для измерения изменений. В Таиланде и Шри-Ланке действуют сильные программы по борьбе с инфекциями, передаваемыми половым путем, которые обеспечивают всеобщий доступ к услугам по лечению этих инфекций и адресным мероприятиям для ключевых групп населения. В Индии и Мьянме были предприняты широкомасштабные адресные усилия по борьбе с этими инфекциями. Другие страны региона уделяют приоритетное внимание борьбе с вирусом иммунодефицита человека, а на борьбу с другими инфекциями, передаваемыми половым путем, выделяются ограниченные ресурсы. На национальном и субнациональном уровнях данные свидетельствуют о быстром сокращении инфекций, передаваемых половым путем, когда адресное продвижение использования презервативов и услуг по борьбе с инфекциями, передаваемыми половым путем, расширяется с целью охвата большего числа работников секс-индустрии. И наоборот, недавние вспышки инфекций, передаваемых половым путем, среди не охваченных услугами групп мужчин, имеющих половые контакты с мужчинами, были связаны с тенденциями регионального роста инфекций, передаваемых половым путем. Для достижения глобальных целей по ликвидации инфекций, передаваемых половым путем, в регионе необходимы обновленные и целенаправленные ответные меры.
Introduction
The World Health Organization’s (WHO’s) global health-sector strategy on sexually transmitted infections (2016–2021) has set targets for 90% reductions in the incidence of Treponema pallidum (syphilis) and Neisseria gonorrhoeae (gonorrhoea) infections between 2018 and 2030.1 Here, we review trends in sexually transmitted infections and the experiences of countries in the WHO South-East Asia Region to determine the current status of control programmes for sexually transmitted infections and the feasibility of reaching the global targets. We focus primarily on control of common curable sexually transmitted infections such as syphilis, gonorrhoea and to a lesser extent Chlamydia trachomatis (chlamydia) and Haemophilus ducreyi (chancroid) infections.
Historically, sexually transmitted infections have been among the most serious public health problems in the WHO South-East Asia Region, with substantial associated morbidity, mortality, disability and adverse pregnancy outcomes.2–4 The incidence and prevalence of curable sexually transmitted infections were high in urban areas and along migrant and trucking routes, and were closely linked to the rapid early spread of human immunodeficiency virus (HIV), particularly ulcerative chancroid and syphilis. However, large-scale preventive measures that focused on sex work in several countries of the region during the 1990s and early 2000s led to substantial declines in sexually transmitted infections and the slowing of the HIV epidemic.2–4
Recent reports of increases in the incidence of syphilis and gonorrhoea raise concerns about the adequacy of the current efforts to prevent sexually transmitted infections as control programmes focus increasingly on HIV-specific interventions such as antiretroviral therapy and pre-exposure prophylaxis without maintaining investment in primary prevention.5–7 Declining use of condoms and behavioural risk compensation (that is, riskier behaviour that may dilute or offset preventive benefits), particularly in key populations, may facilitate a resurgence in transmission of sexually transmitted infections at a time when primary prevention, condom programming and basic services for sexually transmitted infections are underresourced.
In this paper, we assess the current epidemiology and control of sexually transmitted infections in the WHO South-East Asia Region. We base our assessment on a 2018 report on the elimination of sexually transmitted infections in the region and other recent data.8 In countries with improved infection control, we discuss what constitutes an effective response to sexually transmitted infections. We consider the challenges faced by programmes for sexually transmitted infections and what actions may help to counter those challenges.
Historical trends
WHO global estimates for four common curable infections – syphilis, gonorrhoea, chlamydia and trichomoniasis – have shown little change over three decades.9–13 However, the proportion of new cases of sexually transmitted infections estimated for the WHO South-East Asia Region has declined by two thirds, from 118 million (35% of the global estimate) in the 1990s to 39 million (11% of the global estimate) in 2012.8 Despite limitations in the methods used for these estimations, such a large magnitude of change requires further analysis to assess whether sexually transmitted infections have indeed declined in the South-East Asia Region relative to other WHO regions.
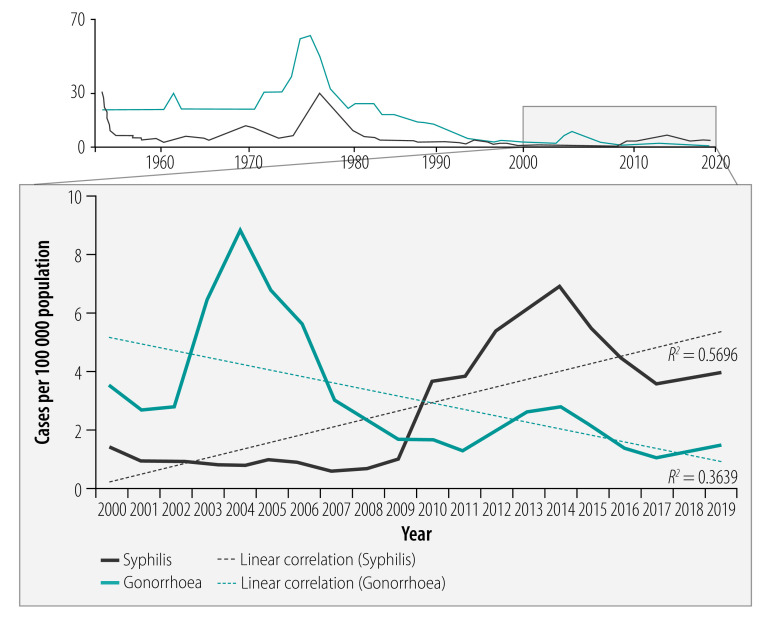
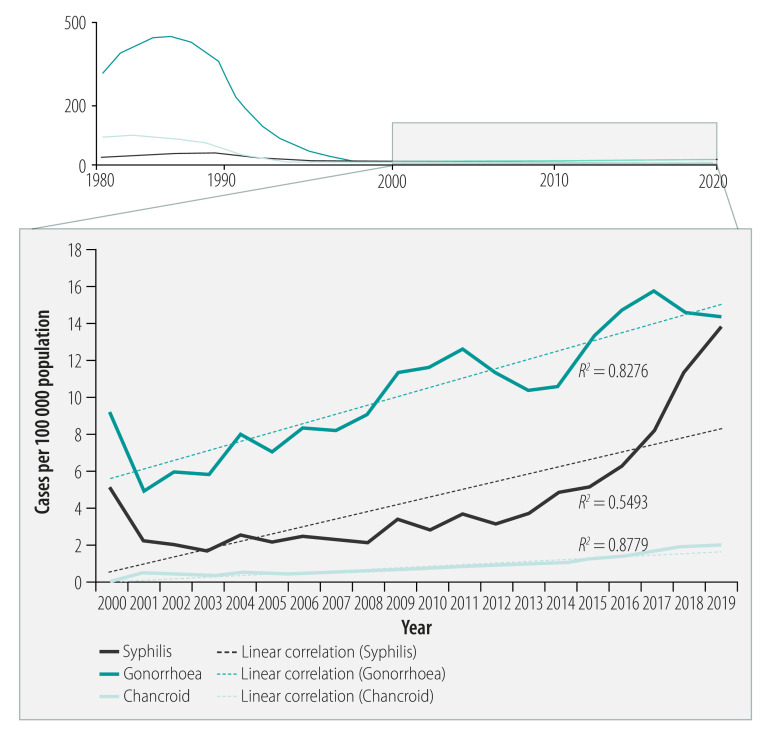
Although routinely reported surveillance data on sexually transmitted infections vary in completeness and reliability across the region, national data from Myanmar, Sri Lanka and Thailand, obtained from their health ministries, are good enough to examine long-term trends. In these countries, sexually transmitted infections have decreased by more than 90%.8 For example, in Sri Lanka, the incidence of gonorrhoea decreased from 61.6 to 3.5 cases per 100 000 population (94.3% reduction) between 1975 and 2000 (Fig. 1), while in Thailand, the incidence decreased from 445 to 7 cases per 100 000 population (98.4% reduction) between 1985 and 2005 (Fig. 2). In Myanmar, the incidence of gonorrhoea decreased from 15.4 to 1.4 per 10 000 male population (90.6% reduction, based on non-rounded figures) between 1985 and 2005. In addition, in Sri Lanka between 1975 and 2000, the incidence of syphilis decreased from 21.5 to 1.4 cases per 100 000 population (93.5% reduction) (Fig. 1), and in Thailand between 1985 and 2005 the incidence decreased from 32.0 to 2.1 cases per 100 000 population (93.4% reduction) (Fig. 2). In Myanmar between 1996 and 2016, the prevalence of syphilis among women attending antenatal clinics decreased from 4.2% to 0.3%, a 92.9% reduction. Large reductions in the incidence of chancroid were also reported between 1985 and 2005, from 93.0 to 0.4 cases per 100 000 population (99.6% reduction) in Thailand (Fig. 2). and from 7.5 to 0.4 cases per 10 000 male population (94.5% reduction, based on non-rounded figures) in Myanmar.
Fig. 1.
Trends in sexually transmitted infections, Sri Lanka, 1952–2019
Source: National STD/AIDS Control Programme, Colombo, Sri Lanka.
Fig. 2.
Trends in sexually transmitted infections, Thailand, 1982–2019
Source: Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, Bangkok, Thailand.
Evidence from many sources suggests that smaller reductions in sexually transmitted infections in India’s large population – more than two thirds of the region’s total population – have driven regional declines.3,4 However, reporting on sexually transmitted infections in India is not consistent enough to detect trends as is the case in Sri Lanka and Thailand. On the other hand, many epidemiological studies, particularly over a period of increased investment in control of sexually transmitted infections (including the large Avahan India AIDS Initiative), show changing trends and patterns in the incidence and prevalence of sexually transmitted infections in India.14,15 Studies from the 1990s in India indicate poor control, with a high prevalence of bacterial and ulcerative sexually transmitted infections including chancroid, concentration of these infections in urban areas linked to migration and mobility, and strong associations with HIV acquisition and transmission.16–20 Later studies show a very different picture, with evidence of large declines in sexually transmitted infections between the late 1990s and 2010 among key populations (sex workers, men who have sex with men, people who use drugs and prisoners); male bridge groups (higher risk men, e.g. migrants or transport workers, who have contact with both key populations and lower-risk populations); and pregnant women.21–42 Taken together, these studies provide additional evidence of declining trends, closely linked to intervention efforts, and of an epidemiological transition from predominately bacterial to viral sexually transmitted infections.21–42 The strongest intervention-linked data show declines in the incidence or prevalence of sexually transmitted infections between 21.3% (from 8.9% to 7.0%) and 77.3% (from 9.7% to 2.2%) across several large Indian states between 2004 and 2010.36,41
Some of the earliest and largest decreases in sexually transmitted infections were reported among female sex workers in Kolkata, India. The prevalence of syphilis, assessed by sentinel surveillance, declined by more than 99%, from more than 25% in 1992 to 0.2% in 2005.43 Another community-led intervention among sex workers in Karnataka, India, reported significant reductions in the prevalence of syphilis (45.4%, from 24.9% to 13.6%), gonorrhoea (83.3%, from 5.4% to 0.9%) and chlamydia (63.0%, from 10.8% to 4.0%) from the start of the intervention in 2004 until 2009 – with more recent routine clinical data suggesting near elimination of symptomatic cases of sexually transmitted infections.22,23,25 Increasing condom use and statistically significant declines in sexually transmitted infections and HIV were reported in surveys from other districts in Karnataka from 2004 to 2011.24,25 Large reductions in syphilis and HIV prevalence were also reported in pregnant women over the same period.23,44
Among the remaining seven countries in the South-East Asia Region, routine surveillance of sexually transmitted infections is neither complete nor reliable enough to assess trends and few studies are reported in the literature. Where declines in sexually transmitted infections have been documented in a few specific locations, these reductions are linked to programmes that have increased condom use in sex work while also improving clinical services for sexually transmitted infections, or are associated with specific interventions for sexually transmitted infections such as periodic presumptive treatment. In Bangladesh, for example, a community-based randomized controlled trial reported an 83% decrease (from 41% to 7%) in the prevalence of either gonorrhoea or chlamydia in female sex workers 9 months after a periodic presumptive treatment intervention and enhanced syndromic management.45 In Bintan Island, Indonesia, the prevalence of gonorrhoea and/or chlamydia decreased by 78.9% (from 36.1% to 7.6%, P < 0.01) in female sex workers over 15 months in 2008–2009, with a lower prevalence among those who received periodic presumptive treatment (P < 0.01).46 Of note, the prevalence of consistent condom use reported in this study doubled to 40% (P < 0.01). Elsewhere in Indonesia, the prevalence of active syphilis (defined as rapid plasma reagin ≥ 1:8) was 35.0% lower (3.9% after the intervention compared with 6.0% before) in 10 cities between 2005 and 2007 among those who received at least one dose of periodic presumptive treatment (P = 0.008).47
Current trends
The large decreases in sexually transmitted infections documented in several countries of the region from 1980 to 2010 can be at least partly attributed to comprehensive prevention efforts – in particular, promotion of condom use in targeted high-risk groups and programmes to control sexually transmitted infections – in response to the rapidly growing HIV epidemics. During the past decade, however, these trends appear to have levelled off or reversed in at least some populations, with a growing number of outbreaks of sexually transmitted infections being reported or rising trends being seen across the region.5–7,48 The importance of reliable surveillance of sexually transmitted infections and strong programme capacity is evident in the context of this recent resurgence. Countries with reliable national surveillance have been able to detect rising trends of sexually transmitted infections at the national level, while evidence from other countries is limited to surveys conducted in a few locations in specific population groups. In Thailand and Sri Lanka, reported syphilis cases rose on average 2.4 and 5.1 times, respectively, from 2000–2009 to 2010–2019, while gonorrhoea cases increased 1.7 times in Thailand over the same periods (Fig. 1 and Fig. 2).
While rebounding transmission of sexually transmitted infections is a challenge, overall rates in Sri Lanka and Thailand are still low compared with historical trends, and both countries have recently been validated as having achieved elimination of mother-to-child transmission of HIV and congenital syphilis.1 Viewed in a broader context comparing rates across regions, the incidence rates of syphilis and gonorrhoea in Thailand (respectively, 8.2 and 15.8 cases per 100 000 population) and Sri Lanka (respectively, 3.6 and 1.1 cases per 100 000 population) in 2017 were comparable to those reported in Europe (7.1 and 22.2 cases per 100 000 population).49,50
Elsewhere in the region, the trends in sexually transmitted infections are less clear. In Indonesia, trend data from integrated biological and behavioural surveys in key populations show high and stable prevalence rates of gonorrhoea and chlamydia between 2009 and 2019, with no sign of a downward trend. The prevalence of syphilis in Jakarta and Bandung increased 3–5 times between 2007 and 2018 in men who have sex with men and transgender groups. Syphilis rates were lower but also increasing in people who inject drugs over the same period.51
Components of a strong response
Reflecting on the elements of good control of sexually transmitted infections in the South-East Asia Region, it is striking that countries that have invested in four key areas have shown much better progress compared with countries that have not.51
First, the responses of the countries that have made progress have been data driven, and investment in sexually transmitted infection surveillance systems and programme monitoring has been maintained and linked to antibiotic resistance monitoring.
Second, countries that have ensured universal access to screening, diagnosis and treatment of syphilis and HIV for pregnant women attending antenatal care (such as Bhutan, Maldives, Sri Lanka and Thailand) have been able to reduce the prevalence of these diseases in pregnancy more than countries that have not provided such access. Furthermore, successful access has been obtained through collaboration across primary care, reproductive health and maternal and child health services.
Third, these countries have had a strong focus on key population interventions and, apart from screening, diagnosis and treatment of HIV, they have made large investments in primary prevention. As part of prevention, not only have these countries improved the provision of condoms and lubricants, they have also ensured access to regular sexually transmitted infection screening and tackled structural drivers of risk and vulnerability. For example, Thailand’s 100% condom-use programme put the responsibility for condom use on the client and ensured that brothel owners had a duty to ensure safe sex practices.2 Furthermore, community voices and concerns were heard and integrated into programme design and service delivery models in Bangladesh, India and elsewhere.21,22
Fourth, and perhaps most importantly, countries that have ensured adequate resources for a decentralized programme within the context of access to universal health coverage have been more effective in controlling sexually transmitted infections. Having a separate and clearly articulated strategy to control sexually transmitted infections and substantial domestic investments have helped secure adequate resources. For example, the programme for the elimination of mother-to-child transmission of HIV and syphilis in Sri Lanka builds on the strong foundations of public health and primary health care services that have operated for several decades: Sri Lanka started its so-called antivenereal disease campaign in 1952, and the National sexually transmitted disease and AIDS control programme was established in 1987, with a key objective of preventing HIV and sexually transmitted infections in the community. The programme for the elimination of mother-to-child transmission of HIV and syphilis is funded entirely by the Ministry of Health of Sri Lanka. Similarly, in Thailand, the National Health Security Office ensures access to syphilis screening and treatment not just for all pregnant mothers, but also for key populations. In India, a large targeted intervention programme working with key populations in the community is funded through domestic investments and has been delivered on a large scale for over 20 years.8
Looking ahead, these elements of effective control of sexually transmitted infections are still relevant. However, risk behaviours have changed, particularly through the use of social media and the Internet by many young and key populations. These changes challenge the effectiveness of facility-based programming in preventing and treating sexually transmitted infections. To respond to this challenge requires programmes to innovate and explore the potential of digital health tools.
Many services for sexually transmitted infections have depended heavily on HIV funding, which is likely to become less plentiful in the future. With less funding, sexually transmitted infection services will need to find opportunities for integration and efficiency. Integrating regular sexually transmitted infection screening in men’s health clinics and moving towards newer testing approaches, such as self-testing and provider-initiated testing, is one approach. Other options include making use of the triple elimination agenda for the elimination of mother-to-child transmission of HIV, syphilis and hepatitis B infection, as well as dual diagnostic kits for HIV and syphilis testing, point-of-care tests and molecular diagnostic testing.
Control of sexually transmitted infections cannot be achieved only through a government-led response in the South-East Asia Region, because the private sector is responsible for a large proportion of health-care provision, and out-of-pocket health expenditure is high. Therefore, including screening and treatment of sexually transmitted infections as part of a minimum essential service package for outpatients, provided by social health insurance through an accredited service provider (public, private or nongovernmental), would go a long way to improving access and provider choice. As countries such as India and Indonesia move forward in improving social health insurance, programmes to control sexually transmitted infections have the opportunity to make use of the wider health system and domestic funding.
Conclusion
Outstanding, although uneven, progress has been made in controlling sexually transmitted infections in the South-East Asia Region over the years. In several countries, this progress has been sustained so that elimination of several sexually transmitted infections has become a possible objective. However, while historical trends support the feasibility of reducing the incidence of syphilis and gonorrhoea by 90%, new challenges have emerged to reaching these global elimination targets.
For countries such as Sri Lanka and Thailand which have well established programmes for control of sexually transmitted infections, new strategies will clearly be needed to address rebounding transmission. Since the global targets for syphilis and gonorrhoea use 2018 as the baseline, reducing incidence further will require more intensive case finding to identify small clusters and interrupt transmission early. Disease elimination is always most difficult at this final stage when cases become rare and more difficult to detect. It is worth noting that further reductions in the incidence of syphilis and gonorrhoea in Sri Lanka and Thailand would bring their rates to lower than the rates of many high-income countries.
Countries with weaker control programmes for sexually transmitted infections should be motivated by knowing that the global 90% reduction targets for syphilis and gonorrhoea are feasible, particularly for syphilis. Data on syphilis are more available and reliable than for other sexually transmitted infections because of inexpensive diagnostics and, in countries with limited capacity to diagnose other sexually transmitted infections, tracking syphilis trends is useful for monitoring overall control efforts for sexually transmitted infections. Evidence of a decrease in syphilis, as well as progress in eliminating mother-to-child transmission of the infection in several countries, supports the feasibility of regional elimination of syphilis as a public health problem. Weak surveillance of sexually transmitted infections and limited syphilis screening of key populations and pregnant women are the main barriers to elimination of syphilis in the region. Recent increases in syphilis among men who have sex with men in several countries of the region and elsewhere underline the importance of routinely screening key populations for this disease and other sexually transmitted infections, and monitoring prevalence trends. Such outbreaks and rebounding trends, together with increasing antimicrobial resistance, are the main new challenges for countries aiming to reach the global targets for elimination of sexually transmitted infections.
A focused and prioritized response targeting the most important sexually transmitted infections from a public health perspective is clearly needed now. To move this agenda forward, sexually transmitted infections need to become visible again. Political attention to these infections has been half-hearted at best and this is compounded by the lack of any specific targets within the sustainable development goals that address sexually transmitted infections. Raising awareness of the large and preventable disease burden of sexually transmitted infections and its effect on people and societies will require not just data, but also investment to generate demand for services and high-level advocacy.
Competing interests:
None declared.
References
- 1.Global health sector strategy on sexually transmitted infections 2016–2021. Towards ending STIs. Geneva: World Health Organization; 2016. Available from: https://www.who.int/reproductivehealth/publications/rtis/ghss-stis/en/ [cited 2020 Nov 5]
- 2.Ruxrungtham K, Brown T, Phanuphak P. HIV/AIDS in Asia. Lancet. 2004. July 3-9;364(9428):69–82. 10.1016/S0140-6736(04)16593-8 [DOI] [PubMed] [Google Scholar]
- 3.Garg R, Yu D, Narain JP. Epidemiology and transmission dynamics. In: Narain JP, editor. Three decades of HIV/AIDS in Asia. New Delhi: Sage Publications; 2012. [Google Scholar]
- 4.Steen R, Zhao P, Wi TE, Punchihewa N, Abeyewickreme I, Lo Y-R. Halting and reversing HIV epidemics in Asia by interrupting transmission in sex work: experience and outcomes from ten countries. Expert Rev Anti Infect Ther. 2013. October;11(10):999–1015. 10.1586/14787210.2013.824717 [DOI] [PubMed] [Google Scholar]
- 5.Holtz TH, Wimonsate W, Mock PA, Pattanasin S, Chonwattana W, Thienkrua W, et al. Why we need pre-exposure prophylaxis: incident HIV and syphilis among men, and transgender women, who have sex with men, Bangkok, Thailand, 2005-2015. Int J STD AIDS. 2019. April;30(5):430–9. 10.1177/0956462418814994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). HIV and syphilis infection among men who have sex with men–Bangkok, Thailand, 2005-2011. MMWR Morb Mortal Wkly Rep. 2013. June 28;62(25):518–20. [PMC free article] [PubMed] [Google Scholar]
- 7.Ahn JY, Boettiger D, Kiertiburanakul S, Merati TP, Huy BV, Wong WW, et al. ; Treat Asia HIV Observational Database. Incidence of syphilis seroconversion among HIV-infected persons in Asia: results from the TREAT Asia HIV Observational Database. J Int AIDS Soc. 2016. October 21;19(1):20965. 10.7448/IAS.19.1.20965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moving ahead on elimination of sexually transmitted infections (STIs) in WHO South-East Asia Region – progress and challenge. New Delhi: World Health Organization, Regional Office for South-East Asia; 2018. Available from: https://apps.who.int/iris/handle/10665/330031 [cited 2020 Nov 5].
- 9.Global prevalence and incidence of selected curable sexually transmitted infections: overview and estimates. Geneva: World Health Organization; 2001. Available from: https://www.who.int/reproductivehealth/publications/rtis/HIV_AIDS_2001_2/en/ [cited 2020 Nov 5].
- 10.Prevalence and incidence of selected sexually transmitted infections, Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis and Trichomonas vaginalis: methods and results used by WHO to generate 2005 estimates. Geneva: World Health Organization; 2011. Available from: https://www.who.int/reproductivehealth/publications/rtis/9789241502450/en/ [cited 2020 Nov 5].
- 11.Global incidence and prevalence of selected curable sexually transmitted infections – 2008. Geneva: World Health Organization; 2011. Available from: https://apps.who.int/iris/bitstream/10665/75181/1/9789241503839_eng.pdf [cited 2020 Nov 5].
- 12.Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015. December 8;10(12):e0143304. 10.1371/journal.pone.0143304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019. August 1;97(8):548–562P. 10.2471/BLT.18.228486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandrasekaran P, Dallabetta G, Loo V, Rao S, Gayle H, Alexander A. Containing HIV/AIDS in India: the unfinished agenda. Lancet Infect Dis. 2006. August;6(8):508–21. 10.1016/S1473-3099(06)70551-5 [DOI] [PubMed] [Google Scholar]
- 15.Steen R, Mogasale V, Wi T, Singh AK, Das A, Daly C, et al. Pursuing scale and quality in STI interventions with sex workers: initial results from Avahan India AIDS Initiative. Sex Transm Infect. 2006. October;82(5):381–5. 10.1136/sti.2006.020438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamat HA, Banker DD. Human immunodeficiency virus-1 infection among patients with sexually transmitted diseases in Bombay. Natl Med J India. 1993. Jan-Feb;6(1):11–3. [PubMed] [Google Scholar]
- 17.Bhave G, Lindan CP, Hudes ES, Desai S, Wagle U, Tripathi SP, et al. Impact of an intervention on HIV, sexually transmitted diseases, and condom use among sex workers in Bombay, India. AIDS. 1995. July;9 Suppl 1:S21–30. [PubMed] [Google Scholar]
- 18.Rodrigues JJ, Mehendale SM, Shepherd ME, Divekar AD, Gangakhedkar RR, Quinn TC, et al. Risk factors for HIV infection in people attending clinics for sexually transmitted diseases in India. BMJ. 1995. July 29;311(7000):283–6. 10.1136/bmj.311.7000.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Risbud A, Chan-Tack K, Gadkari D, Gangakhedkar RR, Shepherd ME, Bollinger R, et al. The etiology of genital ulcer disease by multiplex polymerase chain reaction and relationship to HIV infection among patients attending sexually transmitted disease clinics in Pune, India. Sex Transm Dis. 1999. January;26(1):55–62. 10.1097/00007435-199901000-00009 [DOI] [PubMed] [Google Scholar]
- 20.Mehendale SM, Rodrigues JJ, Brookmeyer RS, Gangakhedkar RR, Divekar AD, Gokhale MR, et al. Incidence and predictors of human immunodeficiency virus type 1 seroconversion in patients attending sexually transmitted disease clinics in India. J Infect Dis. 1995. December;172(6):1486–91. 10.1093/infdis/172.6.1486 [DOI] [PubMed] [Google Scholar]
- 21.Jana S, Dey B, Reza-Paul S, Steen R. Combating human trafficking in the sex trade: can sex workers do it better? J Public Health (Oxf). 2014. December;36(4):622–8. 10.1093/pubmed/fdt095 [DOI] [PubMed] [Google Scholar]
- 22.Reza-Paul S, Beattie T, Syed HUR, Venukumar KT, Venugopal MS, Fathima MP, et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS. 2008. December;22 Suppl 5:S91–100. 10.1097/01.aids.0000343767.08197.18 [DOI] [PubMed] [Google Scholar]
- 23.Reza-Paul S, Steen R, Maiya R, Lorway R, Wi TE, Wheeler T, et al. Sex worker community-led interventions interrupt sexually transmitted infection/human immunodeficiency virus transmission and improve human immunodeficiency virus cascade outcomes: a program review from South India. Sex Transm Dis. 2019. August;46(8):556–62. 10.1097/OLQ.0000000000001020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Isac S, Ramesh BM, Rajaram S, Washington R, Bradley JE, Reza-Paul S, et al. Changes in HIV and syphilis prevalence among female sex workers from three serial cross-sectional surveys in Karnataka state, South India. BMJ Open. 2015. March 27;5(3):e007106. 10.1136/bmjopen-2014-007106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boily MC, Pickles M, Lowndes CM, Ramesh BM, Washington R, Moses S, et al. Positive impact of a large-scale HIV prevention programme among female sex workers and clients in South India. AIDS. 2013. June 1;27(9):1449–60. 10.1097/QAD.0b013e32835fba81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Charles B, Jeyaseelan L, Edwin Sam A, Kumar Pandian A, Thenmozhi M, Jeyaseelan V. Trends in risk behaviors among female sex workers in south India: priorities for sustaining the reversal of HIV epidemic. AIDS Care. 2013;25(9):1129–37. 10.1080/09540121.2012.752562 [DOI] [PubMed] [Google Scholar]
- 27.Ramanathan S, Deshpande S, Gautam A, Pardeshi DB, Ramakrishnan L, Goswami P, et al. Increase in condom use and decline in prevalence of sexually transmitted infections among high-risk men who have sex with men and transgender persons in Maharashtra, India: Avahan, the India AIDS Initiative. BMC Public Health. 2014. August 3;14(1):784. 10.1186/1471-2458-14-784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subramanian T, Ramakrishnan L, Aridoss S, Goswami P, Kanguswami B, Shajan M, et al. Increasing condom use and declining STI prevalence in high-risk MSM and TGs: evaluation of a large-scale prevention program in Tamil Nadu, India. BMC Public Health. 2013. September 17;13(1):857. 10.1186/1471-2458-13-857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Souverein D, Euser SM, Ramaiah R, Narayana Gowda PR, Shekhar Gowda C, Grootendorst DC, et al. Reduction in STIs in an empowerment intervention programme for female sex workers in Bangalore, India: the Pragati programme. Glob Health Action. 2013. December 27;6(1):22943. 10.3402/gha.v6i0.22943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mogasale V, Wi TC, Das A, Kane S, Singh AK, George B, et al. Quality assurance and quality improvement using supportive supervision in a large-scale STI intervention with sex workers, men who have sex with men/transgenders and injecting-drug users in India. Sex Transm Infect. 2010. February;86 Suppl 1:i83–8. 10.1136/sti.2009.038364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prabhakar P, Narayanan P, Deshpande GR, Das A, Neilsen G, Mehendale S, et al. Genital ulcer disease in India: etiologies and performance of current syndrome guidelines. Sex Transm Dis. 2012. November;39(11):906–10. 10.1097/OLQ.0b013e3182663e22 [DOI] [PubMed] [Google Scholar]
- 32.Setia MS, Jerajani HR, Brassard P, Boivin JF. Clinical and demographic trends in a sexually transmitted infection clinic in Mumbai (1994-2006): an epidemiologic analysis. Indian J Dermatol Venereol Leprol. 2010. Jul-Aug;76(4):387–92. 10.4103/0378-6323.66590 [DOI] [PubMed] [Google Scholar]
- 33.Becker M, Stephen J, Moses S, Washington R, Maclean I, Cheang M, et al. Etiology and determinants of sexually transmitted infections in Karnataka state, south India. Sex Transm Dis. 2010. March;37(3):159–64. 10.1097/OLQ.0b013e3181bd1007 [DOI] [PubMed] [Google Scholar]
- 34.Hochberg CH, Schneider JA, Dandona R, Lakshmi V, Kumar GA, Sudha T, et al. Population and dyadic-based seroincidence of herpes simplex virus-2 and syphilis in southern India. Sex Transm Infect. 2015. August;91(5):375–82. 10.1136/sextrans-2014-051708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rachakulla HK, Kodavalla V, Rajkumar H, Prasad SP, Kallam S, Goswami P, et al. Condom use and prevalence of syphilis and HIV among female sex workers in Andhra Pradesh, India - following a large-scale HIV prevention intervention. BMC Public Health. 2011. December 29;11 Suppl 6:S1. 10.1186/1471-2458-11-S6-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thilakavathi S, Boopathi K, Girish Kumar CP, Santhakumar A, Senthilkumar R, Eswaramurthy C, et al. Assessment of the scale, coverage and outcomes of the Avahan HIV prevention program for female sex workers in Tamil Nadu, India: is there evidence of an effect? BMC Public Health. 2011. December 29;11 Suppl 6:S3. 10.1186/1471-2458-11-S6-S3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gurung A, Narayanan P, Prabhakar P, Das A, Ranebennur V, Tucker S, et al. Large-scale STI services in Avahan improve utilization and treatment seeking behaviour amongst high-risk groups in India: an analysis of clinical records from six states. BMC Public Health. 2011. December 29;11 Suppl 6:S10. 10.1186/1471-2458-11-S6-S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pandey A, Mishra RM, Sahu D, Benara SK, Sengupta U, Paranjape RS, et al. Heading towards the Safer Highways: an assessment of the Avahan prevention programme among long distance truck drivers in India. BMC Public Health. 2011. December 29;11 Suppl 6:S15. 10.1186/1471-2458-11-S6-S15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gutierrez JP, McPherson S, Fakoya A, Matheou A, Bertozzi SM. Community-based prevention leads to an increase in condom use and a reduction in sexually transmitted infections (STIs) among men who have sex with men (MSM) and female sex workers (FSW): the Frontiers Prevention Project (FPP) evaluation results. BMC Public Health. 2010. August 18;10(1):497. 10.1186/1471-2458-10-497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ramesh BM, Beattie TS, Shajy I, Washington R, Jagannathan L, Reza-Paul S, et al. Changes in risk behaviours and prevalence of sexually transmitted infections following HIV preventive interventions among female sex workers in five districts in Karnataka state, south India. Sex Transm Infect. 2010. February;86 Suppl 1:i17–24. 10.1136/sti.2009.038513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ramakrishnan L, Gautam A, Goswami P, Kallam S, Adhikary R, Mainkar MK, et al. Programme coverage, condom use and STI treatment among FSWs in a large-scale HIV prevention programme: results from cross-sectional surveys in 22 districts in southern India. Sex Transm Infect. 2010. February;86 Suppl 1:i62–8. 10.1136/sti.2009.038760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rajaram SP, Banandur P, Thammattoor UK, Thomas T, Mainkar MK, Paranjape R, et al. Two cross-sectional studies in south India assessing the effect of an HIV prevention programme for female sex workers on reducing syphilis among their clients. Sex Transm Infect. 2014. November;90(7):556–62. 10.1136/sextrans-2013-051301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rojanapithatykorn W, Jana S, Steen R. Interventions with sex workers: from the 100% condom-use programme to community empowerment. In: Narain JP, editor. Three decades of HIV/AIDS in Asia. New Delhi: Sage Publications; 2012. [Google Scholar]
- 44.Sethi S, Sharma K, Dhaliwal LK, Banga SS, Sharma M. Declining trends in syphilis prevalence among antenatal women in northern India: a 10-year analysis from a tertiary healthcare centre. Sex Transm Infect. 2007. December;83(7):592. 10.1136/sti.2007.025551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCormick DF, Rahman M, Zadrozny S, Alam A, Ashraf L, Neilsen GA, et al. Prevention and control of sexually transmissible infections among hotel-based female sex workers in Dhaka, Bangladesh. Sex Health. 2013. December;10(6):478–86. 10.1071/SH12165 [DOI] [PubMed] [Google Scholar]
- 46.Bollen LJ, Anartati AS, Morineau G, Sulami S, Prabawanti C, Silfanus FJ, et al. Addressing the high prevalence of gonorrhoea and chlamydia among female sex workers in Indonesia: results of an enhanced, comprehensive intervention. Sex Transm Infect. 2010. February;86(1):61–5. 10.1136/sti.2009.038299 [DOI] [PubMed] [Google Scholar]
- 47.Majid N, Bollen L, Morineau G, Daily SF, Mustikawati DE, Agus N, et al. Syphilis among female sex workers in Indonesia: need and opportunity for intervention. Sex Transm Infect. 2010. October;86(5):377–83. 10.1136/sti.2009.041269 [DOI] [PubMed] [Google Scholar]
- 48.Werner RN, Gaskins M, Nast A, Dressler C. Incidence of sexually transmitted infections in men who have sex with men and who are at substantial risk of HIV infection - a meta-analysis of data from trials and observational studies of HIV pre-exposure prophylaxis. PLoS One. 2018. December 3;13(12):e0208107. 10.1371/journal.pone.0208107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Syphilis and congenital syphilis in Europe – a review of epidemiological trends (2007–2018) and options for response. Stockholm: European Centre for Disease Prevention and Control; 2019. Available from: https://www.ecdc.europa.eu/en/publications-data/syphilis-and-congenital-syphilis-europe-review-epidemiological-trends-2007-2018 [cited 2020 Nov 5].
- 50.Gonorrhoea. In: Annual epidemiological report for 2017. Stockholm: European Centre for Disease Prevention and Control; 2019. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/gonorrhoea-annual-epidemiological-report-2017.pdf [cited 2021 Jan 5].
- 51.Sexually transmitted infection programme review 2020: revitalising STI services. Jakarta: World Health Organization; 2020. Available from: https://www.who.int/indonesia/news/detail/24-02-2020-sexually-transmitted-infection-programme-review-2020-revitalising-sti-services [cited 2020 Nov 5].