Abstract
Objective:
Treatment in a disproportionately minority serving hospital has been associated with worse outcomes in a variety of illnesses. We examined the association of treatment in disproportionately minority hospitals on outcomes in patients with sepsis across the United States.
Design:
Retrospective Cohort Analysis
Setting:
The National Inpatient Sample from 2008–2014
Methods:
Disproportionately minority hospitals were defined as hospitals having twice the relative minority patient population than the surrounding geographical mean. Minority hospitals for Black and Hispanic patient populations were identified based on US Census demographic information. A multivariate model employing a validated algorithm for mortality in sepsis using administrative data was utilized.
Interventions:
None
Measurements and Main Results:
A total of 4,221,221 patients with sepsis were identified. Of these, 612,217 (14.5%) patients were treated at hospitals disproportionately serving the black community (Black hospitals) while 181,141 (4.3%) were treated at hospitals disproportionately serving the Hispanic community (Hispanic hospitals). After multivariate analysis, treatment in a Black hospital was associated with a 4% higher risk of mortality compared to treatment in a non-minority hospital (OR 1.04, 95% CI 1.03–1.05, p<0.01). Treatment in a Hispanic hospital was associated with a 9% higher risk of mortality (OR 1.09, 95% CI 1.07–1.11, p<0.01). Median hospital length of stay was almost 1 day longer at each of the disproportionately minority hospitals (5.9 days IQR 3.1–11.0 Non-Minority Hospitals vs 6.9 days IQR 3.6–12.9 Hispanic and 6.7 days IQR 3.4–13.2 Black, both p<0.01).
Conclusion:
Patients with sepsis regardless of race who were treated in disproportionately high minority hospitals suffered significantly higher rates of in-hospital mortality.
Keywords: Sepsis, Minority Hospital, Health Disparities, Nationwide Inpatient Sample
Introduction
Disparities in health-care delivery continue to be a major barrier in the United States. Racial and ethnic disparities have been demonstrated to be associated with a myriad of poor outcomes including higher rates of heart disease, stroke, cancer, HIV/AIDs and homicide.(1) A recent article found a lack of improvement in outcomes for patients with critical illness in minority serving hospitals, regardless of the race of the patient.(2) While factors such as genetics, socioeconomic disparity and lifestyle factors play a role, increasing evidence supports a lack of access to quality care for minority patients as a factor in inferior outcome.(3) Minority patients face provider bias, receive less routine preventative care, less advanced care, less referral for hospital transfer and are otherwise subject to discrimination in access to quality healthcare.(4–8)
Reduced access to quality hospitals may be another reason for poor outcomes in minority patients. Care for minority patients tends to be clustered into relatively few hospitals with disproportionately high minority patient populations.(9) Disproportionately minority hospitals in the United States have poorer outcomes including: higher procedural complication rates, lower rates of palliative care, worse pain control, higher readmission rates, increased mortality rates in elderly, trauma, myocardial infarction, and post-partum patients.(10–15)
The impact of treatment in a minority hospital for patients with critical illness is not well understood. We attempted to study the impact of treatment in a minority hospital on outcomes in sepsis. The primary outcome of this analysis was the association of treatment in a minority hospital with in-hospital mortality.
Methods
The National Inpatient Sample (NIS) dataset was used for this analysis. The NIS is a U.S. Federal all-payer database created by the Agency for Healthcare Research and Quality (AHRQ) using a complex survey design that captures approximately 20% of all US hospitalizations and allows for the use of weighting to approximate 97% of all inpatient care delivered across the United States.
The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement was followed during the reporting of this study.(16) A waiver of consent was obtained from the Research Ethics Board at the University of Manitoba for this study as the NIS utilizes de-identified data.
Cohort Selection
All patients ≥18 years of age included in the 2008–2014 NIS sample years who met the Angus definition of sepsis were included in the analysis.(17) The Angus definition has been validated to have a sensitivity of 50.4% and a specificity of 96.3% in identifying patients with sepsis.(18) A flow diagram displaying cohort selection can be found in Figure 1.
Figure 1 –
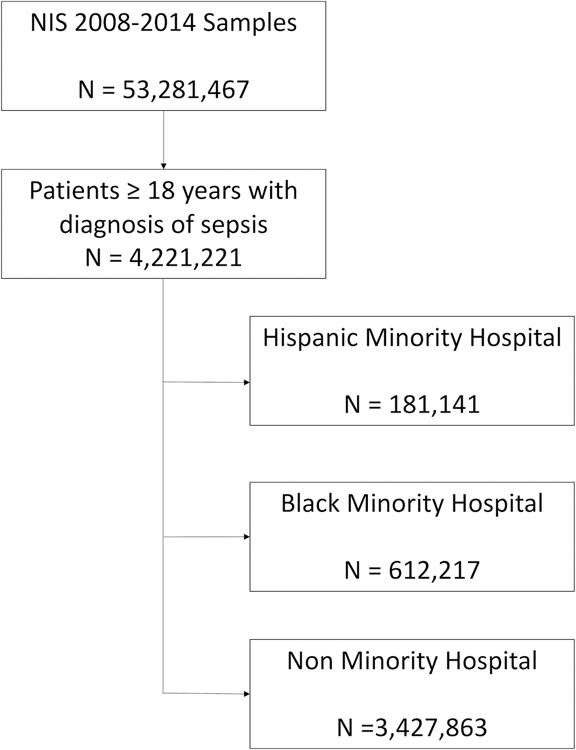
Patient selection cohort flow diagram
Covariates
Patient characteristics obtained from the NIS included: age, gender, race (White, Black, Hispanic, Other), in-hospital mortality, length of stay, zip-code income quartile, insurance coverage (Private, Medicare, Medicaid, No Insurance), use of mechanical ventilation, dialysis, ICU admission as well as the 29 Elixhauser co-morbidity indices.(19) Patients with missing race information were categorized into Other race. Hospital level characteristics obtained included: hospital size (small, medium, large as per AHRQ definition), rural vs urban, teaching status, and which Census Division the hospital was located in.
Minority Hospital Definition
The NIS provides hospital location according to the US Census Bureau Divisions. To prevent identification of individual hospitals, the most granular location data available is the Census Divisions. Utilizing the 2010 US Census race and ethnicity data, we defined hospitals that treated twice the census division mean Black population as Black hospitals.(20) For example, the mean black population for the Census Division 1 (New England) is 6.6%. If a hospitals Black patient population represented more than 13.2% of its census, it would be categorized as a Black hospital. Similarly, hospitals that had patient populations made up of Hispanic patients that were twice the geographical mean were defined as Hispanic hospitals. Less than 0.5% of all hospitals qualified as both a minority Black and minority Hispanic hospital. Since the absolute number of double minority hospitals was so small, we did not separate these hospitals from the pre-specific groups. The reason we chose this definition of minority hospital rather than selecting hospitals with the highest numbers of minority patients treated is we wanted to isolate hospitals which treated disproportionately high numbers of minority patients relative to the populations they served.
As an additional method of analyzing the outcomes of patients in disproportionately serving minority hospitals we have added an absolute definition as a secondary analysis. We identified hospitals that had minority (either Black or Hispanic) patient censuses of 25%, 50%, and 75% and categorized them as such for additional strength of our associations.
Statistical Analysis
All statistical analysis was performed in SAS v9.4 (Cary, NC, USA) utilizing the correct survey procedures to handle the weighted sampling nature of the NIS. A two-sided alpha level of 0.05 was used for all statistical testing. For univariate analysis, normally distributed data was compared using the independent t-test whereas non-normal data was compared using the Wilcoxon Rank-Sum test. Categorical data was compared using chi-squared analyses.
In order to adjust for the severity of illness, we modelled our analysis on the work of Ford et al, who developed and validated a sepsis severity model using administrative data.(21) A multivariate model predicting in-hospital mortality was created with all variables determined a priori. The model included the following variables: age, gender, race, treatment in a Black Hospital, treatment in a Hispanic hospital, zip-code income quartile, early mechanical ventilation (<2 days), need for hemodialysis, teaching status of hospital, rural vs urban hospital, insurance coverage, hospital size, presence of shock, ICU admission, and the 29 Elixhauser co-morbidity indices. A hospital random effect was utilized in our model to account for clustering by hospital. The c statistic for the final model was 0.76.
Sensitivity Analyses
In order to ensure our model performed well we completed several sensitivity analyses. We analyzed the performance of the model by restricting to specific races, which showed no significant change or algorithmic bias (C stat 0.71–0.75).
Results
A total of 4,221,221 patients with sepsis treated in 7,401 unique hospitals were identified from the 2008–2014 NIS samples. Of these, 612,217 (14.5%) patients were treated at Black hospitals while 181,141 (4.3%) were treated at Hispanic hospitals. Of the 7,401 hospitals, 638 (8.6%) were classified as Hispanic hospitals whereas 1,557 (21.0%) hospitals were classified as Black hospitals. The baseline characteristics of the patients treated at each type of hospital are displayed in Table 1.
Table 1 –
Baseline characteristics of cohort. Statistical comparisons for Black Hospital and Hispanic Hospital patients are to the Non-Minority Hospital group.
| Variable | Non Minority Hospitals (n= 3,427,863) | Black Hospitals (n= 612,217) |
p value | Hispanic Hospitals (n=181,141) | p value |
|---|---|---|---|---|---|
| Age, mean (SD) | 69.1 (16.1) | 65.6 (16.8) | <0.01 | 67.8 (16.9) | <0.01 |
| Female gender, n(%) | 1,803,957 (52.5) | 310,801 (50.7) | <0.01 | 91,402 (50.5) | <0.01 |
| In-hospital mortality, n(%) | 380,994 (11.1) | 75,147 (12.3) | <0.01 | 22,951 (12.7) | <0.01 |
| Length of Stay, median (IQR) | 5.9 (3.1–11.0) | 6.7 (3.4–13.2) | <0.01 | 6.9 (3.6–12.9) | <0.01 |
| Race, n(%) | |||||
| White | 2,407,206 (70.3) | 277,502 (45.1) | <0.01 | 52,446 (29.0) | <0.01 |
| African American | 316,113 (9.2) | 219,100 (36.0) | <0.01 | 23,841 (13.2) | <0.01 |
| Hispanic | 171,066 (5.0) | 61,736 (10.1) | <0.01 | 91,327 (50.5) | <0.01 |
| Other | 535,835 (15.6) | 54,185 (8.8) | <0.01 | 13,482 (7.4) | <0.01 |
| Insurance Coverage, n(%) | |||||
| Private Insurance | 560,310 (16.3) | 95,075 (15.5) | 24,632 (13.6) | ||
| Medicare | 2,379,619 (69.4) | 374,818 (61.1) | 113,716 (62.8) | ||
| Medicaid | 296,682 (8.6) | 99,517 (16.3) | 27,413 (15.1) | ||
| No Coverage | 193,872 (5.6) | 43,121 (7.0) | <0.01 | 15,380 (8.4) | <0.01 |
| Teaching Hospital, n(%) | 1,599,116 (46.5) | 402,864 (66.5) | <0.01 | 102,779 (56.3) | 0.01 |
| Rural Hospital, n(%) | 402,084 (11.7) | 20,304 (3.5) | <0.01 | 8,151 (4.6) | <0.01 |
| Income Quartile, n(%) | |||||
| 1st | 940,935 (28.0) | 231,836 (39.2) | 75,266 (43.8) | ||
| 2nd | 921,258 (27.4) | 129,383 (21.8) | 37,855 (21.8) | ||
| 3rd | 810,400 (24.1) | 132,252 (22.1) | 37,883 (21.6) | ||
| 4th | 685,542 (20.4) | 100,014 (16.8) | <0.01 | 22,101 (12.8) | <0.01 |
Patients treated at Black hospitals were younger (mean 65.6 years vs 69.1 years at non-minority hospitals, p<0.01), more likely to be on Medicaid (16.3% vs 8.6%, p<0.01) as well as be in the lowest household income quartile compared to non-minority hospitals (39.2% vs 29.8, p<0.01). The unadjusted mortality for patients with sepsis treated at Black hospitals was also higher compared to non-minority hospitals (12.3% vs 11.1%, p<0.01). Similarly, patients treated at Hispanic hospitals were more likely to be from the lowest income quartile (43.8% vs 29.8%, p<0.01) as well as suffer from higher rates of in-hospital mortality (12.7% vs 11.1%, p<0.01). Median hospital length of stay was almost 1 day longer at each of the disproportionately minority hospitals (5.9 days IQR 3.1–11.0 non-minority Hospitals vs 6.9 days IQR 3.6–12.9 Hispanic and 6.7 days IQR 3.4–13.2 Black, both p<0.01).
The unadjusted mortality of patients stratified by race and minority hospital type are displayed in Table 2. White patients had an 11.1% mortality at non-minority hospital whereas they had 12.7% mortality at Black hospitals and 12.9% mortality at Hispanic hospitals (p<0.01). Black patients had an 10.6% mortality at non-minority hospitals compared to 11.3% and 12.4% at Black and Hispanic hospitals respectively (p<0.01). Hispanic patients also demonstrated lower mortality at non-minority hospitals (11.1%) compared to Black (11.8%) and Hispanic hospitals (12.4%, p<0.01).
Table 2 –
Mortality rate by race stratified by minority hospital status
| Race | Non-Minority Hospital | Black Hospital | Hispanic Hospital | p value |
|---|---|---|---|---|
| White | 11.1% | 12.7% | 12.9% | <0.01 |
| Black | 10.6% | 11.3% | 12.4% | <0.01 |
| Hispanic | 11.1% | 11.8% | 12.4% | <0.01 |
| Other | 11.6% | 14.5% | 14.3% | <0.01 |
The results of the multivariate analysis predicting in-hospital mortality are displayed in Table 3. After adjustment for all variables in the model, treatment in a Black hospital was associated with a 4% higher risk of mortality than treatment in a non-minority hospital (OR 1.04, 95% CI 1.03–1.05, p<0.01). Treatment in a Hispanic hospital was associated with a 9% higher risk of mortality (OR 1.09, 95% CI 1.07–1.11, p<0.01). The rest of the Elixhauser variables included in the multivariate model are included in Supplementary Table 1.
Table 3 –
Results of multivariate analysis predicting in-hospital mortality. The 29 Elixhauser co-morbidities were also included in the final model and are displayed in Supplementary Table 1. For race, White served as the reference. For Hospital size, small hospitals served as the reference. For insurance coverage, Private Insurance served as the reference.
| Covariates | Odds Ratio | Confidence Interval (95%) | p |
|---|---|---|---|
| Age | 1.03 | 1.02–1.03 | <0.01 |
| Female Sex | 0.97 | 0.96–0.98 | <0.01 |
| Black Hospital | 1.04 | 1.03–1.05 | <0.01 |
| Hispanic Hospital | 1.09 | 1.07–1.11 | <0.01 |
| White Race | 1.0 | - | - |
| Black Race | 1.01 | 1.00–1.02 | 0.02 |
| Hispanic Race | 1.05 | 1.03–1.06 | <0.01 |
| Other Race | 1.13 | 1.12–1.14 | <0.01 |
| Teaching Hospital | 1.02 | 1.01–1.03 | <0.01 |
| Rural Hospital | 1.02 | 1.01–1.03 | <0.01 |
| Small Hospital | 1.0 | - | - |
| Medium Hospital | 1.03 | 1.02–1.04 | <0.01 |
| Large Hospital | 1.09 | 1.08–1.10 | <0.01 |
| Private Insurance | 1.0 | - | - |
| Medicare | 0.91 | 0.90–0.92 | <0.01 |
| Medicaid | 1.02 | 1.01–1.04 | 0.03 |
| No Insurance | 1.20 | 1.18–1.22 | <0.01 |
| Shock | 2.50 | 2.48–2.52 | <0.01 |
| Early Mechanical Ventilation | 3.07 | 3.05–3.10 | <0.01 |
| ICU Admission | 1.81 | 1.79–1.82 | <0.01 |
The results of the outcomes for patients treated in minority hospitals as defined on an absolute basis are displayed in Table 4. Patients treated at hospitals with at least 25% Black patients or 25% Hispanic patients had a significantly higher risk of death compared to non-minority hospitals (25% Black Hospital OR 1.20 (1.18–1.23, p<0.01) and 25% Hispanic Hospital OR 1.20 (1.17–1.23, p<0.01)). Treatment at hospitals who’s patient census was at least 50% Black or Hispanic was also associated with worse outcomes (50% Black OR 1.10 (1.06–1.15, p<0.01) and 50% Hispanic OR 1.34 (1.29–1.39, p<0.01)). The worst outcomes were seen in those patients treated at hospitals with at least 75% minority patients (75% Black OR 1.56 (1.33–1.84, p<0.01) and 75% Hispanic OR 1.24 (1.17–1.33, p<0.01)).
Table 4 –
Results of regression analysis using absolute definition of hospital minority patient census rather than relative definition used in Table 2. OR for each category is for in-hospital mortality, using same model variables listed in Table 2.
| Percentage of Hospital Census | Black | P value | Hispanic | P value |
|---|---|---|---|---|
| >25% | 1.20 (1.18–1.23) | <0.01 | 1.20 (1.17–1.23) | <0.01 |
| >50% | 1.10 (1.06–1.15) | <0.01 | 1.34 (1.29–1.39) | <0.01 |
| >75% | 1.56 (1.33–1.84) | <0.01 | 1.24 (1.17–1.33) | <0.01 |
Discussion
In this nationwide study of patients with sepsis, we found that treatment in a disproportionately minority hospital was associated with significantly increased risk of mortality. The risk was higher for those treated in Hispanic minority hospitals compared to those treated in Black minority hospitals. These are the first findings that treatment in a disproportionately minority hospital is associated with worse outcomes in patients with sepsis.
Our findings build on the evidence that treatment in predominately minority hospitals is associated with worse outcomes. As had been shown for a variety of other health outcomes, the treatment all patients receive in disproportionately minority hospitals may be inferior to that provided in non-minority hospitals. Early identification of sepsis and administration of appropriate antibiotics and intravenous fluids remain the cornerstone of sepsis therapy.(22, 23) Minority hospitals are more likely to have overcrowded emergency rooms and suffer from ambulance diversion, both of which have been shown to delay time to antibiotic therapy.(24–26) In one study of 28 US medical centers, hospitals that treated a higher proportion of Black patients were less likely to administer appropriate antibiotic therapy in a timely manner.(27) Another US study showed that hospitals treating predominately Black patients had significantly longer delays to antibiotic therapy than non-minority serving hospitals.(28) Additionally overcrowded emergency rooms and intensive care units have been shown to be associated with higher rates of in-hospital mortality for critically ill patients.(29, 30) Patients treated at disproportionately minority hospitals may lack access to subspecialty services, timely procedural intervention and may have less chance of undergoing hospital transfer.(13, 31)
Exploring the relationship between treatment in disproportionately minority hospitals and worse outcomes requires further detailed study. Understanding driving factors behind these disproportionate outcomes may lead to actionable targets which can improve the disparity that patients treated in these hospitals experience.
The strengths of this analysis lie in the large number of patients studied across the United States over a period of 7 years. The NIS allows for data from all types and sizes of hospitals to be utilized and thus our findings are strongly generalizable to the US patient population. Using the national sampling frame, we were able to gather data from a large number of hospitals, thus allowing us to capture data from a large number of disproportionately minority hospitals compared to prior studies.(27)
The results of this analysis must be interpreted in the context of its study design. The use of administrative data contains inherent risks of coding error, misclassification and selection bias. Several limitations to our analysis must be highlighted. The NIS does not provide granular information to calculate well validated sepsis severity of illness scores such as the Sequential Organ Failure Assessment Score. Our use of the severity of illness algorithm developed by Ford et al. attempted to best adjust our model for illness severity but these findings need to be confirmed on datasets with more granular clinical data. Additionally, we were unable to use state level data to calculate the relative disproportionate minority population. The NIS prevents the identification of individual hospitals on a state-level basis and only provides for the location within one of the 9 Census Divisions throughout the country. Thus, it is possible that some of the hospitals that we characterized as minority could have been not twice the local relative population of that minority. We felt that using a definition of twice the Census Division mean would minimize the number of hospitals that were falsely characterized in this regard. We added the secondary definition of minority status by absolute minority patient populations treated in order to add additional strength to our analysis. Various authors have utilized different definitions for minority serving hospitals and there is no clear commonly accepted definition in the literature.(2) The classification of hospitals as minority serving could have also been influenced by the NIS having a coding for “other” race. It is possible that there was mis-allocation bias introduced into the analysis because some of the patients who were considered “other” may have in fact been Black or Hispanic.
While our preliminary findings are interesting, the authors would like to stress that these should be characterized as hypothesis generating findings and not definitive conclusions about the relationships between treatment in a disproportionately minority hospital and outcomes.
Conclusion
Treatment in hospitals that serve disproportionately more minority patients was associated with significantly higher rates of mortality in patients with sepsis in this nationwide analysis. Further research is needed to confirm these findings and investigate factors contributing to these disparities.
Supplementary Material
Footnotes
Conflict of Interest: No authors disclose any conflicts of interest
Copyright form disclosure: Drs. Rush and Celi received support for article research from the National Institutes of Health. Dr. Danziger received funding from law firms for serving as an expert witness. Dr. Walley disclosed that he is a founder and shareholder of Cyon Therapeutics. Dr. Kumar disclosed that he does not have any potential conflicts of interest.
References
- 1.Schneider EC, Zaslavsky AM, Epstein AM: Racial disparities in the quality of care for enrollees in medicare managed care. JAMA 2002; 287:1288–94 [DOI] [PubMed] [Google Scholar]
- 2.Danziger J, Ángel Armengol de la Hoz M, Li W, et al. : Temporal Trends in Critical Care Outcomes in United States Minority Serving Hospitals. Am J Respir Crit Care Med 2020; [DOI] [PMC free article] [PubMed]
- 3.Cooper RS: Genetic Factors in Ethnic Disparities in Health. In: Anderson NB, Bulatao RACB, editor(s). Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. National Academies Press (US); 2004. [PubMed] [Google Scholar]
- 4.Kogan MD, Kotelchuck M, Alexander GR, et al. : Racial disparities in reported prenatal care advice from health care providers. Am J Public Health 1994; 84:82–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kendrick J, Nuccio E, Leiferman JA, et al. : Primary Care Providers Perceptions of Racial/Ethnic and Socioeconomic Disparities in Hypertension Control. Am J Hypertens 2015; 28:1091–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Regenbogen SE, Gawande AA, Lipsitz SR, et al. : Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Ann Surg 2009; 250:424–31 [DOI] [PubMed] [Google Scholar]
- 7.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, et al. : Racial differences in the use of revascularization procedures after coronary angiography. JAMA 1993; 269:2642–6 [PubMed] [Google Scholar]
- 8.Tyler PD, Stone DJ, Geisler BP, et al. : Racial and Geographic Disparities in Interhospital ICU Transfers. Crit Care Med 2018; 46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bach PB, Pham HH, Schrag D, et al. : Primary care physicians who treat blacks and whites. N Engl J Med 2004; 351:575–84 [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, Orav EJ, Li Z, et al. : Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med 2007; 167:1177–82 [DOI] [PubMed] [Google Scholar]
- 11.Joynt KE, Orav EJ, Jha AK: Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA 2011; 305:675–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creanga AA, Bateman BT, Mhyre JM, et al. : Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol 2014; 211:647.e1–16 [DOI] [PubMed] [Google Scholar]
- 13.Ly DP, Lopez L, Isaac T, et al. : How do black-serving hospitals perform on patient safety indicators? Implications for national public reporting and pay-for-performance. Med Care 2010; 48:1133–7 [DOI] [PubMed] [Google Scholar]
- 14.Faigle R, Ziai WC, Urrutia VC, et al. : Racial Differences in Palliative Care Use After Stroke in Majority-White, Minority-Serving, and Racially Integrated U.S. Hospitals. Crit Care Med 2017; 45:2046–2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haider AH, Ong’uti S, Efron DT, et al. : Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg 2012; 147:63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vandenbroucke JP, von Elm E, Altman DG, et al. : Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 2007; 18:805–835 [DOI] [PubMed] [Google Scholar]
- 17.Angus DC, Linde-Zwirble WT, Lidicker J, et al. : Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29:1303–1310 [DOI] [PubMed] [Google Scholar]
- 18.Iwashyna TJ, Odden A, Rohde J, et al. : Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care 2014; 52:e39–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elixhauser a, Steiner C, Harris DR, et al. : Comorbidity measures for use with administrative data. Med Care 1998; 36:8–27 [DOI] [PubMed] [Google Scholar]
- 20.Census Bureau: 2010 US Census [Internet]. 2010; [cited 2019 May 15] Available from: www.statisticalatlas.com
- 21.Ford DW, Goodwin AJ, Simpson AN, et al. : A Severe Sepsis Mortality Prediction Model and Score for Use With Administrative Data. Crit Care Med 2015; 12–15 [DOI] [PMC free article] [PubMed]
- 22.Kumar A, Roberts D, Wood KE, et al. : Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34:1589–96 [DOI] [PubMed] [Google Scholar]
- 23.Angus DC, van der Poll T: Severe sepsis and septic shock. N Engl J Med 2013; 369:2063. [DOI] [PubMed] [Google Scholar]
- 24.Peltan ID, Bledsoe JR, Oniki TA, et al. : Emergency Department Crowding Is Associated With Delayed Antibiotics for Sepsis. Ann Emerg Med 2019; 73:345–355 [DOI] [PubMed] [Google Scholar]
- 25.Sikka R, Mehta S, Kaucky C, et al. : ED crowding is associated with an increased time to pneumonia treatment. Am J Emerg Med 2010; 28:809–12 [DOI] [PubMed] [Google Scholar]
- 26.Hsia RY-J, Asch SM, Weiss RE, et al. : California hospitals serving large minority populations were more likely than others to employ ambulance diversion. Health Aff (Millwood) 2012; 31:1767–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mayr FB, Yende S, D’Angelo G, et al. : Do hospitals provide lower quality of care to black patients for pneumonia? Crit Care Med 2010; 38:759–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor SP, Karvetski CH, Templin MA, et al. : Hospital Differences Drive Antibiotic Delays for Black Patients Compared With White Patients With Suspected Septic Shock. Crit Care Med 2018; 46:e126–e131 [DOI] [PubMed] [Google Scholar]
- 29.Sprivulis PC, Da Silva J-A, Jacobs IG, et al. : The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 2006; 184:208–12 [DOI] [PubMed] [Google Scholar]
- 30.Fergusson NA, Ahkioon S, Nagarajan M, et al. : Association of intensive care unit occupancy during admission and inpatient mortality: a retrospective cohort study. Can J Anaesth 2019; [DOI] [PubMed]
- 31.Rush B, Tyler PD, Stone DJ, et al. : Outcomes of Ventilated Patients with Sepsis Who Undergo Interhospital Transfer: A Nationwide Linked Analysis. Crit Care Med 2018; 46 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


