Abstract
Background:
The US Dietary Guidelines for Americans provide dietary recommendations for individuals aged ≥2 y and metrics exist to assess alignment. Nonfederal feeding recommendations exist for children <2 y, but limited metrics and assessment of dietary quality are available.
Objective:
We aimed to assess dietary quality of children aged 6 mo–4 y using a modified Diet Quality Index Score (DQIS).
Methods:
NHANES 2011–2016 dietary data were used to estimate the dietary quality of children 6 mo–4 y old using a modified DQIS. Differences in mean modified DQIS by demographics were assessed using linear regression.
Results:
Mean modified DQIS ± SE was 22.4 ± 0.23 out of 45 possible points (50%) for children 6 mo–4 y of age on a given day. Modified DQIS scores on a given day decreased with age (27.7 ± 0.27 for 6- to 11-mo-olds, 23.9 ± 0.31 for 1-y-olds, 21.4 ± 0.26 for 2- to 3-y-olds, and 20.6 ± 0.49 for 4-y -olds; P < 0.0001 for trend). Children 6–11 mo old had 16% higher overall modified DQIS scores than 1-y-olds (P < 0.0001) and higher modified DQIS subcomponent scores for refined grains and protein, indicating higher age-appropriate intakes (P < 0.05). Similarly, children 6–11 mo old also had higher modified DQIS subcomponent scores, indicating no or limited intake, for 100% fruit juice, sugar-sweetened beverages, other added sugars, and salty snacks (P < 0.02).
Conclusions:
Dietary quality declines with age and may begin as early as 1 y. The modified DQIS tool could help assess the dietary quality of young children. This may be important when identifying programmatic and policy efforts aimed at establishing and maintaining healthy dietary patterns beginning at an early age.
Keywords: diet quality, young children, NHANES, Diet Quality Index Score, healthy diet, children less than 2 years
Introduction
A healthy dietary pattern, in addition to regular physical activity, is important to maintaining good health and reducing chronic disease across the life span (1, 2). There is mounting evidence of the importance of early dietary patterns and their lasting impact on health (3–6). For example, children who are breastfed are more likely to have healthier dietary patterns at age 6 y (5). Similarly, children who eat more fruits and vegetables in late infancy are more likely to continue eating fruits and vegetables at age 6 y (4). Other studies have indicated associations between early dietary patterns and high weight for age at 1 y (7) and early parenting interventions have shown reductions in childhood weight outcomes at 3 y (8).
However, defining a healthy dietary pattern and determining the metrics to assess it can be challenging. Currently, there are no federal dietary guidelines for children <2 y of age and associated metrics to assess dietary quality are limited. The 2015–2020 US Dietary Guidelines for Americans (DGAs) provide recommendations and guidance on healthy dietary patterns for the US population ≥2 y of age; however, with the 2020–2025 edition, for the first time recommendations will include children from birth to 24 mo of age and pregnant women (1, 9). Supporting metrics, such as the Healthy Eating Index (HEI), assess how well eating patterns align with the DGAs (10). Internationally, the WHO has infant and young child feeding indicators including global targets to reduce stunting, wasting, anemia, and low birth weight in low- and middle-income countries and a measure to assess whether diets are minimally acceptable for infants and young children (11). However, these indicators may not be as applicable to the United States because of the low prevalence of conditions such as stunting and wasting or because the measures have lower sensitivity in identifying poor dietary quality due to the high intake of added sugars and solid fats which is common in the United States (12).
Given the limited metrics to measure dietary quality at early ages, we are not aware of studies in the United States assessing dietary quality of young children with a dietary quality index using nationally representative data. An understanding of children’s early dietary quality could provide important information for programs and policies that provide or support healthy eating environments for this population. Therefore, the purpose of this study is to assess the dietary quality among US children aged 6 mo to <2 y using a recently developed assessment tool for children <2 y of age—the Diet Quality Index Score (DQIS)—that may be more applicable for the United States than other international measures (13). We also examined differences by age and sociodemographic characteristics and expanded the DQIS to children ages 2–4 y.
Methods
NHANES
We used data from NHANES, a nationally representative survey of the noninstitutionalized civilian US population, for this analysis. NHANES is conducted using a stratified multistage probability design; more detailed information on study design and methods has already been published (14). Participants complete a household interview and a physical examination conducted in the Mobile Examination Center. All participants provide written informed consent, with parents or guardians providing consent for minors to participate. The NHANES protocol was approved by the National Center of Health Statistics Research Ethics Review Board. For this study, we combined data from 3 survey cycles: 2011–2012, 2013–2014, and 2015–2016. Response rates for children aged <1 y and children aged 1–5 y who underwent the physical examination were 83.4% and 77.6% in 2011–2012, 79.3% and 74.6% in 2013–2014, and 69.4% and 64.4% in 2015–2016, respectively (15).
Dietary intake and modified DQIS
Dietary intakes are collected using two 24-h dietary recalls. We used day 1 of the dietary recalls, which are conducted during the in-person physical examination to estimate mean population intakes representing intake on a given day, consistent with NHANES analytic guidance (16). Dietary recalls for this age group are completed by a proxy (generally a parent) who is most familiar with the child’s intake. Dietary data are collected using a standardized format to help respondents remember and report all foods and drinks consumed in the previous 24 h (17).
The original DQIS was developed for children from birth to 5 mo of age and children 8–24 mo of age using a semiquantitative FFQ (13). The DQIS includes 9 subcomponents, including drinking milk (breast milk, infant formula, and cow milk/other milks), grains (whole and refined grains), proteins (e.g., meat, poultry, eggs), vegetables, whole fruit, 100% fruit juice, sugar-sweetened beverages, other added sugars (originally labelled as sweets in the DQIS), and salty snacks. Table 1 provides the scoring criteria for the modified DQIS and Supplemental Table 1 provides specific details about how the scoring criteria were developed. For this study, all foods and beverages reported in the 24-h dietary recall were disaggregated into their components and assigned to 1 of the 9 mutually exclusive modified DQIS subcomponents using the USDA’s Food Patterns Equivalent Databases and Food and Nutrient Database for Dietary Studies corresponding to the appropriate NHANES survey year (18–21).
TABLE 1.
Modified DQIS for children 6 mo–4 y of age1
| Portions consumed2 | |||||
|---|---|---|---|---|---|
| Subcomponent | Score | 6–11 mo | 1 y | 2–3 y | 4 y |
| Drinking milk for 6–11 mo | |||||
| Breast milk3 | 5 | Yes | — | — | — |
| — | — | — | |||
| Infant formula | 2.5 | 20–28 | |||
| 1.25 | 8.0–19.9 or 28.1–35.0 | ||||
| 0 | <8 or >35 | ||||
| Cow milk/other milks,3,4 fl oz/d | 0 | Yes | — | — | — |
| Drinking milk for 1- to 4-y-olds | |||||
| Infant formula/cow milk/other milks,4 fl oz/d | 5 | — | 14.0–18.0 | 16.0–20.0 | 20.0–24.0 |
| 2.5 | — | 8.0–13.9 or 18.1–24.0 | 8.0–15.9 or 20.1–24.0 | 8.0–19.9 or 24.1–28.0 | |
| 0 | — | <8.0 or >24.0 | <8.0 or >24.0 | <8.0 or >28.0 | |
| Grains5 | |||||
| Whole grains, oz/d | 2.5 | 1.0–2.0 | 1.0–2.0 | 1.5–3.0 | 2.0–4.0 |
| 1.25 | 0.1–0.9 | 0.1–0.9 | 0.1–1.4 | 0.1–1.9 | |
| 0 | 0 or >2.0 | 0 or >2.0 | 0 or >3.0 | 0 or >4.0 | |
| Refined grains, oz/d | 2.5 | 0–1.0 | 0–1.0 | 0–1.5 | 0–2.0 |
| 1.25 | 1.1–2.0 | 1.1–2.0 | 1.6–3.0 | 2.1–4.0 | |
| 0 | >2.0 | >2.0 | >3.0 | >4.0 | |
| Proteins,6 oz/d | 5 | 3.0–6.0 | 2.0–3.0 | 1.5–2.5 | 2.5–3.5 |
| 2.5 | 0.1–2.9 | 0.1–1.9 | 0.1–1.4 | 0.1–2.4 | |
| 0 | 0 or >6.0 | 0 or >3.0 | 0 or >2.5 | 0 or >3.5 | |
| Vegetables,7 oz/d | 5 | ≥4.0 | ≥8.0 | ≥8.0 | ≥12.0 |
| 2.5 | 0.1–3.9 | 0.1–7.9 | 0.1–7.9 | 0.1–11.9 | |
| 0 | 0 | 0 | 0 | 0 | |
| Fruits, oz/d | 5 | ≥4.0 | ≥8.0 | ≥8.0 | ≥8.0 |
| 2.5 | 0.1–3.9 | 0.1–7.9 | 0.1–7.9 | 0.1–7.9 | |
| 0 | 0 | 0 | 0 | 0 | |
| 100% fruit juices, fl oz/d | 5 | 0 | 0–4.0 | 0–4.0 | 0–6.0 |
| 2.5 | 0.1–4.0 | 4.1–6.0 | 4.1–6.0 | 6.1–8.0 | |
| 0 | >4.0 | >6.0 | >6.0 | >8.0 | |
| Sugar-sweetened beverages,8 fl oz/d | 5 | 0 | 0 | 0 | 0 |
| 2.5 | 0.1–4.0 | 0.1–4.0 | 0.1–4.0 | 0.1–4.0 | |
| 0 | >4.0 | >4.0 | >4.0 | >4.0 | |
| Other added sugars,9 tsp/d | 5 | 0 | 0 | <3.1 | <3.8 |
| 2.5 | 0.1–6.0 | 0.1–6.0 | 3.1–6.3 | 3.8–7.5 | |
| 0 | >6.0 | >6.0 | > 6.3 | >7.5 | |
| Salty snacks,10 oz/d | 5 | 0 | 0 | 0 | 0 |
| 2.5 | 0.1–1.0 | 0.1–1.0 | 0.1–1.0 | 0.1–1.0 | |
| 0 | >1.0 | >1.0 | >1.0 | >1.0 | |
The DQIS was originally developed for children 8–24 mo of age (13). The DQIS was modified to extend to 6- to 7-mo-olds and 2- to 4-y-olds. Conversion factors for metric units: fluid ounces to milliliters is 1 fl oz = 29.5735 mL; ounces to grams is 1 oz = 28.3495 g; teaspoons to grams is 1 tsp equivalent of added sugar = 4.2 g. AAP, American Academy of Pediatrics; DQIS, Diet Quality Index Score.
Portion sizes and scoring criteria for children 6–11 mo of age and 1-y-olds were modified from the original DQIS and used updated guidelines and recommendations from the USDA’s Child and Adult Care Food Program and the AAP for breast milk, infant formula, cow milk/other milks, whole and refined grains, protein, vegetables, and fruit (24, 26, 27). Added sugars were based on recommendations from the American Heart Association (28). Portion sizes and scoring criteria for 2- to 4-y-olds were based on the US Dietary Guidelines for Americans 2015–2020 recommended intakes for a sedentary 2- to 4-y-old with an estimated calorie need of 1000–1200 calories/d for whole and refined grains, protein, vegetables, fruit, and added sugars (1). Scoring and portion sizes for milk were based on AAP recommendations (29). For all children, portion sizes and scoring criteria for 100% fruit juice were based on AAP recommendations (25); sugar-sweetened beverages and salty snacks were based on original DQIS criteria for 1-y-olds and were consistent with AAP recommendations (13, 27, 29).
The score for breast milk for children 6–11 mo of age was based on a yes/no response to any consumption of breast milk in the previous 24 h, without quantifying the amount. The score for cow milk/other milks for children 6–11 mo of age was based on a yes/no response to any consumption in the previous 24 h, without quantifying the amount. A child who consumed breast milk was assigned a score of 5 unless they consumed cow milk/other milks. A child 6–11 mo of age who consumed any cow milk/other milks was assigned a score of 0.
Includes fluid milk, buttermilk, evaporated milk, dry milk, fortified or nonfortified soy milk, flavored milk, or goat milk.
The grain subcomponent is divided between whole grains (maximum score 2.5) and refined grains (maximum score 2.5) for a total of 5.0.
Includes meat, poultry, seafood, organ meats, cured meat, eggs, soy, nuts and seeds, yogurt, and cheese. For infants 6–11 mo, these portions consider diluted and pureed meats and beans.
Includes legumes.
Includes teas, carbonated soft drinks, and fruit and nonfruit drinks with sugar added.
Includes other added sugars except those from sugar-sweetened beverages.
Includes potato chips and sticks, French and home fries, hash browns, and higher-sodium crackers.
As described in Ríos et al. (13), portion sizes for children 8–24 mo of age were estimated using the USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) feeding guidelines (22), WHO guidelines (23), and USDA’s Child and Adult Care Food Program (CACFP) Meal Pattern (24). We modified the DQIS in several ways. First, several guidelines or recommendations were published after Ríos et al. developed the original DQIS, and we used these updated values to modify the original DQIS portion sizes and scoring criteria. For example, the USDA’s CACFP meal patterns for infants and children were revised in 2016 (24) and the American Academy of Pediatrics (AAP) updated its recommendations on 100% fruit juice consumption in 2017 (25). A more detailed description of how portion sizes were set for each age group is provided below. Second, we included children 6–7 mo of age by using updated portion sizes and scoring criteria as per those for children 8–11 mo of age (13). Children 6–7 mo of age had originally been excluded because this was the age when food was introduced and may have changed more quickly than at other time periods. We included children 6–7 mo of age for comprehensiveness by using updated portion sizes and scoring criteria as per those for children 8–11 mo of age as described below (13). We conducted a sensitivity analysis excluding these children and found that, regardless of whether or not 6- to 7-mo-olds were included or excluded, our overall interpre- tation of the findings did not change. Third, we modified the original DQIS drinking milk subcomponent to ensure the same maximum score of 45, regardless of age. The original DQIS awarded an additional 10 points for any breast-milk consumption for children 6–24 mo of age (maximum score 55 for this age group). Lastly, we separated consumption of infant formula and cow milk/other milks into 2 separate subcomponents of milk for children 6–11 mo of age.
A detailed description of scoring and portion sizes for each age group and within each subcomponent is provided in Supplemental Table 1. Briefly, scoring and portion sizes for children 6–11 mo of age and for children 1 y of age were based on CACFP meal patterns for grains, proteins, vegetables, and fruit (24). For breast milk, infant formula, and cow milk/other milks, scoring and portion sizes were based on recommendations from the AAP or CACFP (for infant formula only) (24, 26, 27). Added sugars were based on recommendations from the American Heart Association (28). For 2- to 4-y-olds, the scoring and portion sizes for whole and refined grains, protein, fruit, vegetables, and added sugars were developed based on the DGAs for a sedentary 2- to 4-y-old with an estimated calorie need of 1000–1200 calories/d (1). Scoring and portion sizes for drinking milk were based on AAP recommendations (29). For all children, portion sizes and scoring criteria for 100% fruit juice were based on AAP recommendations (25); sugar-sweetened beverages and salty snacks were based on the original DQIS criteria for 1-y-olds and were consistent with AAP recommendations (13, 27, 29).
The maximum score possible is 45 (Table 1). These scores take into account whether or not and how much of the subcomponent was consumed (see Supplemental Table 1 for detailed scoring information). If the child met recommended intakes for each subcomponent, they received a maximum score of 5.0 [the grain subcomponents had 2 parts—refined (2.5 points) and whole (2.5)—to sum to 5.0]. Under- and overconsumption received a score of 2.5; if the subcomponent was not consumed or intake was excessive, they received a score of 0. For the subcomponent of drinking milk among children 6–11 mo of age, any breast-milk consumption received the highest score (5.0), whereas any consumption of cow milk/other milks was scored a 0, regardless of any consumption of breast milk, because of recommendations from the AAP (27). For some subcomponents such as sugar-sweetened beverages, salty snacks, or other added sugars (for children aged <2 y only), no consumption received the highest score (5.0). For 100% fruit juice, exceeding 4–8 ounces/d, depending on age, was scored as 0. Children who limited intake to 4–6 ounces/d, depending on age, achieved the highest score (5.0). The conversion for fluid ounces to milliliters is 1 fl oz = 29.5735 mL. (See Supplemental Table 1 for detailed information on how the scoring criteria were developed.)
Analytic sample
We limited our analyses to children who were 6 mo–4 y of age at the time of the physical examination (n = 3445). Children were excluded if the dietary interview was not completed (n = 492), or if the following variables were missing information: poverty:income ratio (PIR) (n = 229), highest education level in the household (n = 37), or household income (n = 6). We also excluded 6 children who consumed only breast milk even though this is consistent with AAP recommendations of exclusive breastfeeding for about the first 6 mo (26). This left a final sample size of 2675 children 6 mo–4 y of age with complete information.
Covariates
Covariates include age at the time of the exam, highest education level in the household, household income, race/Hispanic origin, and family PIR. Children’s age was categorized as 6–11 mo old, 1 y old (12–23 mo old), 2–3 y old (24–47 mo old), and 4 y old (48–59 mo old). The highest education level in the household was defined as less than high school, high school graduate or General Education Diploma, some college, college graduate, or higher. Household income was classified into 3 categories: <$30,000, $30,000–59,999, and ≥$60,000. Race/Hispanic origin was reported as non-Hispanic white, non-Hispanic black, Hispanic, and other race including multiracial. PIR was defined as <1.85, 1.85–3.49, and ≥3.50.
Statistical analyses
We estimated the mean energy consumed and the mean percentage of energy coming from carbohydrates, protein, and fat on a given day. In addition, we estimated mean sodium intake on a given day and tabulated the number of foods and beverages consumed on the day of recall. Overall mean modified DQIS scores and subcomponent scores on a given day are presented. All estimates are presented for the total analytic sample and by age, education level, household income, race/Hispanic origin, and PIR. Children who consumed breast milk are included in all analyses. However, the quantity of breast milk consumed is not collected in NHANES; therefore, total energy and macronutrient intakes (mean percentage of energy from carbohydrates, protein, and fat on a given day) are not available for these children (n = 197). Although breast-milk volume and nutrient values from breast milk can be imputed (30), we chose not to include this because the main outcome of interest was whether or not children had breastfed, not the nutrient content coming from breast milk.
We assessed trends (overall differences by race/Hispanic origin) in mean scores and mean percentage energy from macronutrients on a given day by sociodemographic categories using linear regression. Linear contrasts were used to detect differences in means by age (i.e., differences in 6- to 11-mo-olds compared with 1-y-olds). SAS survey procedures (version 9.4; SAS Institute Inc.) were used in all analyses to account for the complex survey design. Analyses were weighted using day 1 dietary weights which adjust for over-sampling, nonresponse, and noncoverage.
Results
Among our analytic sample of US children 6 mo–4 y of age, 19% were 6–11 mo old, 22% were 1-y-olds, 42% were 2- to 3-y-olds, and 17% were 4-y-olds. There were no differences in the analytic sample by age for education level, household income, race/Hispanic origin, or PIR (P > 0.4, data not shown).
Table 2 presents the mean modified DQIS scores and macronutrient intakes on a given day for children 6 mo–4 y of age overall and by different sociodemographic characteristics. Mean modified DQIS score on a given day for children 6 mo–4 y of age was 22.4 out of 45 possible points (50%). Mean modified DQIS scores on a given day decreased with age (27.7 for 6- to 11-mo-olds, 23.9 for 1-y-olds, 21.4 for 2- to 3-y-olds, and 20.6 for 4-y-olds; P < 0.0001 for trend). Overall decreases in the modified DQIS score were significant as age increased (P < 0.02 for 6- to 11-mo-olds compared with 1-y-olds, 1-y-olds compared with 2- to 3-y-olds, and 2- to 3-y-olds compared with 4-y-olds; P values not shown in the table). Higher modified DQIS scores were reported among children who lived in households with higher education levels, higher household income levels, and higher PIR (P < 0.0001 for trend). Modified DQIS score varied by race/Hispanic origin, with children who are non-Hispanic black having significantly lower scores than children who are non-Hispanic white.
TABLE 2.
Mean modified DQIS scores and mean percentage of energy from macronutrients on a given day among US children aged 6 mo–4 y overall and by demographics, NHANES 2011–20161
| n2 | n foods | Modified DQIS score (max 45) | n3 | Energy, kcal | % Energy from carbohydrate | % Energy from protein | % Energy from total fat | Sodium, mg | |
|---|---|---|---|---|---|---|---|---|---|
| Overall | 2675 | 15.5 | 22.4 | 2484 | 1350.9 | 53.6 | 14.3 | 33.4 | 1881.6 |
| Age | |||||||||
| 6–11 mo | 495 | 13.1 | 27.7 | 377 | 858.1 | 52.4 | 10.0 | 38.3 | 532.3 |
| 1 y | 590 | 15.7 | 23.9 | 535 | 1213.8 | 51.9 | 15.6 | 33.8 | 1620.4 |
| 2–3 y | 1128 | 16.0 | 21.4 | 1110 | 1409.5 | 54.1 | 14.7 | 32.6 | 2049.3 |
| 4 y | 462 | 15.5 | 20.6 | 462 | 1534.5 | 54.6 | 14.1 | 32.8 | 2267.7 |
| P value for trend4 | 0.0002 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| Highest household education level | |||||||||
| <High school | 503 | 14.4 | 21.5 | 482 | 1375.5 | 53.5 | 14.2 | 33.6 | 1902.5 |
| High school graduate/GED | 525 | 14.3 | 21.0 | 506 | 1357.4 | 53.2 | 14.5 | 33.3 | 1906.7 |
| Some college | 836 | 15.2 | 21.4 | 788 | 1356.3 | 54.8 | 13.8 | 32.7 | 1854.2 |
| ≥College graduate | 811 | 16.6 | 24.2 | 708 | 1334.7 | 52.9 | 14.8 | 33.8 | 1883.3 |
| P value for trend4 | <0.0001 | <0.0001 | 0.2750 | 0.6286 | 0.0528 | 0.6653 | 0.6822 | ||
| Household income | |||||||||
| <$30,000 | 905 | 14.6 | 21.1 | 871 | 1359.2 | 53.6 | 14.3 | 33.3 | 1918.8 |
| $30,000–59,999 | 803 | 15.1 | 21.8 | 750 | 1375.7 | 54.2 | 14.1 | 32.9 | 1868.8 |
| ≥$60,000 | 967 | 16.2 | 23.7 | 863 | 1330.7 | 53.2 | 14.5 | 33.7 | 1866.8 |
| P value for trend4 | <0.0001 | <0.0001 | 0.2038 | 0.4860 | 0.3556 | 0.3405 | 0.3682 | ||
| Race/Hispanic origin | |||||||||
| Hispanic | 865 | 14.95 | 22.56 | 800 | 1371.3 | 53.56 | 14.76 | 33.0 | 1901.0 |
| Non-Hispanic white | 769 | 16.0 | 22.8 | 691 | 1321.5 | 53.2 | 14.4 | 33.9 | 1832.3 |
| Non-Hispanic black | 624 | 14.65 | 20.25 | 606 | 1449.15 | 54.95 | 13.55 | 32.8 | 2051.35 |
| Other race—includes multiracial | 417 | 15.4 | 23.5 | 387 | 1320.1 | 54.0 | 14.5 | 32.6 | 1856.7 |
| PIR | |||||||||
| <1.85 | 1601 | 14.8 | 21.3 | 1528 | 1371.0 | 54.0 | 14.1 | 33.1 | 1896.6 |
| 1.85 ≤ PIR ≤ 3.49 | 568 | 15.6 | 23.0 | 509 | 1335.6 | 52.5 | 14.5 | 34.3 | 1843.4 |
| ≥3.50 | 506 | 16.6 | 24.2 | 447 | 1325.6 | 53.8 | 14.6 | 33.2 | 1885.7 |
| P value for trend4 | <0.0001 | <0.0001 | 0.1083 | 0.5741 | 0.1320 | 0.6488 | 0.7542 |
DQIS, Diet Quality Index Score; GED, General Education Diploma; PIR, poverty:income ratio.
n represents the total analytic sample. This n was used for all calculations with the exception of total energy and macronutrient intakes.
n represents the sample of children who did not consume any breast milk. Total energy and macronutrient intakes are not available for 197 children who consumed breast milk.
P values for trend are calculated using linear regression.
Significantly different from non-Hispanic whites, calculated using linear regression.
Significantly different from non-Hispanic blacks, calculated using linear regression.
Children in the older age groups consumed a higher number of foods, as well as having higher mean caloric and sodium intake, a higher mean percentage of energy from carbohydrates and protein, and a lower percentage of energy from total fat on a given day (P < 0.0001 for trend). There were not any statistically significant differences of mean caloric intake; mean percentage of energy from carbohydrates, protein, and fat on a given day; and mean sodium intake by education level, household income, or PIR. Significant differences by race/Hispanic origin varied. For example, compared with children who are non-Hispanic white, children who are non-Hispanic black consumed a lower number of foods on a given day (P < 0.0003), had a lower percentage of energy from protein (P < 0.0066), higher mean caloric intake on a given day (P < 0.0162), a higher percentage of energy from carbohydrates (P < 0.0186), and higher sodium intake (P < 0.0183).
Figure 1 presents the mean modified DQIS for 5 subcomponents among children aged 6 mo–4 y by age group, with higher scores indicating higher age-appropriate intake. Modified DQIS subcomponent scores on a given day decreased with age for drinking milk, refined grains, vegetables, and whole fruits (P < 0.02 for trend). For example, modified DQIS subcomponent scores on a given day for refined grains were 2.1 for 6- to 11-mo-olds, 0.8 for 1-y-olds, and 0.7 for both 2- to 3-y-olds and 4-y-olds (P < 0.0001 for 6- to 11-mo-olds compared with 1-y-olds).
FIGURE 1.
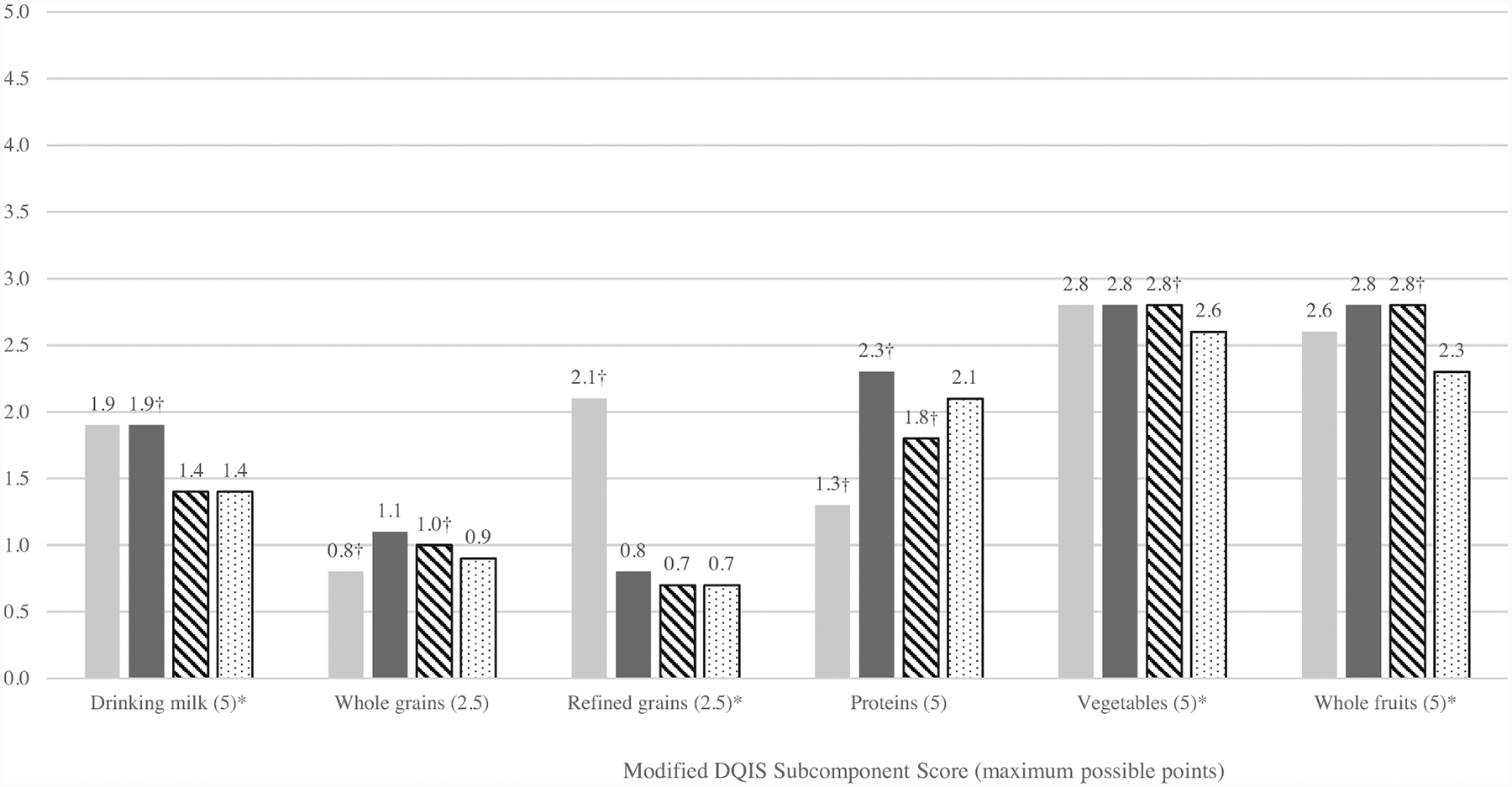
Mean modified DQIS subcomponent scores among US children aged 6 mo–4 y on a given day by age, NHANES 2011–2016. The score for drinking milk includes several subcomponents: breast milk (children 6–11 mo only), infant formula, and cow milk/other milks. Higher subcomponent scores indicate higher age-appropriate intakes. See Table 1 or Supplemental Table 1 for additional information on scoring criteria. *P values for trend are calculated using linear regression, P < 0.02. †P values < 0.05 for difference between footnoted age group and the next successive age group using linear contrasts (6- to 11-mo-olds compared with 1-y-olds, 1-y-olds compared with 2- to 3-y-olds, 2- to 3-y-olds compared with 4-y-olds). Gray bars, 6- to 11-mo-olds (n = 495); black bars, 1-y-olds (n = 590); striped bars, 2- to 3-y-olds (n = 1128); dotted bars, 4-y-olds (n = 462). DQIS, Diet Quality Index Score.
Figure 2 presents the mean modified DQIS for the remaining 4 subcomponents among children aged 6 mo–4 y by age group, with higher scores indicating limited or no intake. Modified DQIS subcomponent scores on a given day decreased with age for sugar-sweetened beverages, other added sugars, and salty snacks (P < 0.001 for trend). For example, modified DQIS subcomponent scores on a given day for sugar-sweetened beverages and other added sugars were 4.9 and 3.4 for 6- to 11-mo-olds, 4.0 and 1.9 for 1-y-olds, 3.3 and 1.7 for 2- to 3-y-olds, and 3.0 and 1.6 for 4-y-olds, respectively.
FIGURE 2.
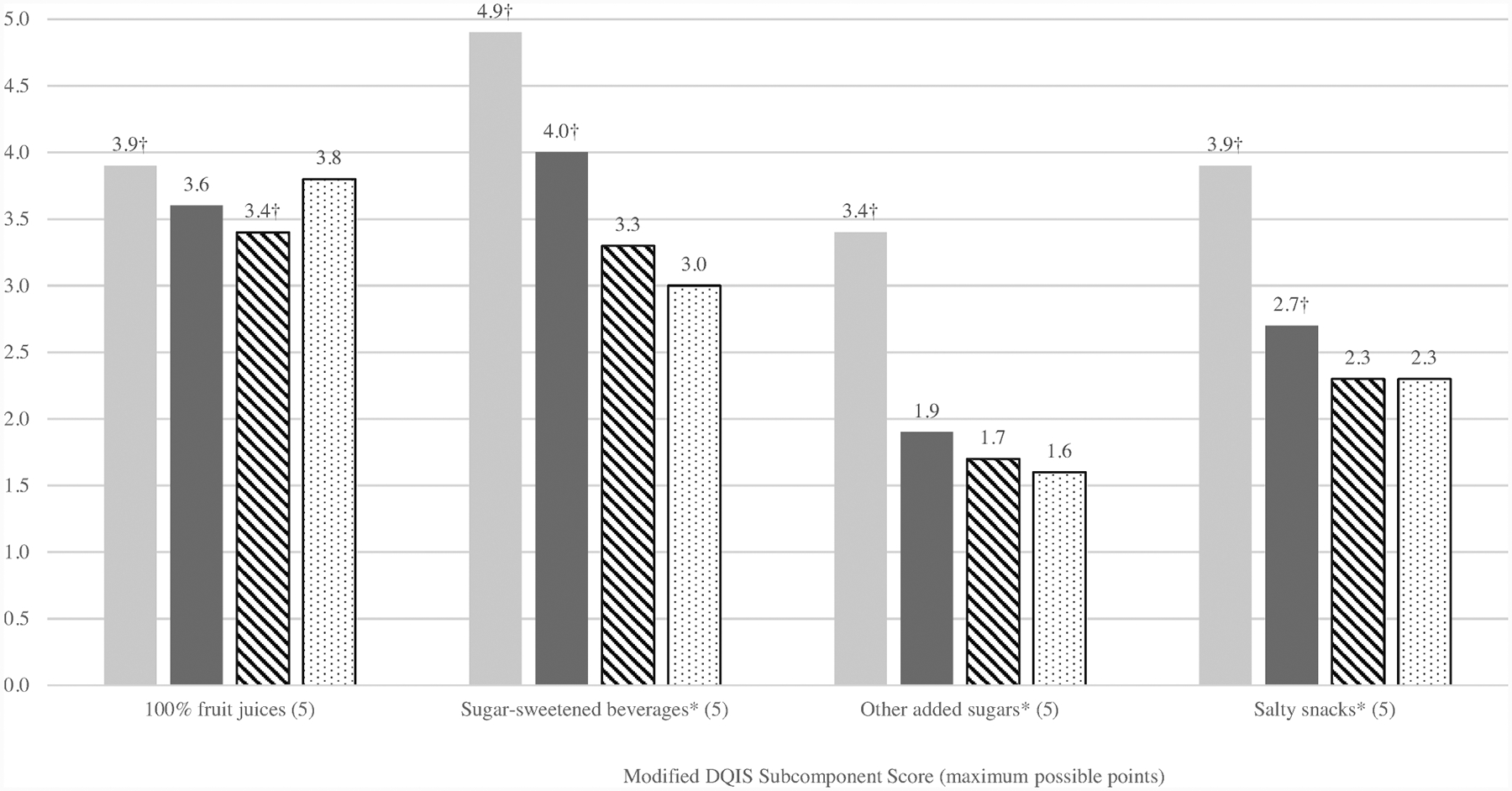
Mean modified DQIS subcomponent scores among US children aged 6 mo–4 y on a given day by age, NHANES 2011–2016. Higher subcomponent scores indicate no or limited intake. See Table 1 or Supplemental Table 1 for additional information on scoring criteria. *P values for trend are calculated using linear regression, P < 0.0001. †P values < 0.05 for difference between footnoted age group and the next successive age group using linear contrasts (6- to 11-mo-olds compared with 1-y-olds, 1-y-olds compared with 2- to 3-y-olds, 2- to 3-y-olds compared with 4-y-olds). Gray bars, 6- to 11-mo-olds (n = 495); black bars, 1-y-olds (n = 590); striped bars, 2- to 3-y-olds (n = 1128); dotted bars, 4-y-olds (n = 462). DQIS, Diet Quality Index Score.
There were some statistically significant differences in subcomponent scores by demographics for drinking milk, whole grains, protein, whole fruits, 100% fruit juice, sugar-sweetened beverages, other added sugars, and salty snacks (Supplemental Table 2). For example, higher scores for drinking milk, whole grains, and whole fruits, indicating higher age-appropriate intakes, were observed with higher education, income, and PIR. In addition, higher scores for 100% fruit juice and sugar-sweetened beverages, indicating limited or no intake, were observed with higher education, income, and PIR.
Discussion
Among US children aged 6 mo–4 y, we found that overall dietary quality needs improvement. On average, children aged 6–11 mo scored 62% of the total possible points, whereas children 1–4 y of age scored between 46% and 53% of the total possible points. Overall, dietary quality declined with age. These declines started as early as 1 y of age and were consistent across most of the subcomponents that made up the overall score. Dietary quality scores were higher among children who lived in households with higher household incomes, education levels, and PIR.
The trend of declining dietary quality by age among children >2 y of age, adolescents, and adults is not new. However, our study, using an adapted dietary quality score for young children, found that these declines may begin as early as 1 y of age. Studies using the HEI-2010 among US children aged 2–18 y found that the youngest children, those 2–5 y of age, had higher HEI-2010 scores than children aged 6–11 or 12–18 y (31). Similarly, Banfield et al. (32) reported that compared with 9- to 13-y-olds, 4- to 8-y-olds had higher component scores for total fruit, whole fruit, whole grains, and dairy. These findings align with our observations that the youngest children, even beginning as early as 6–11 mo, had higher dietary quality scores than children 1–4 y of age. The time period of 6–11 mo is often the time period in which foods are first introduced, and children begin trying a wide range of foods and beverages. However, as children move into toddlerhood, they begin to have more influence on what they eat (33), which could have a range of both positive and negative impacts on overall dietary quality. In addition, families may begin to transition away from foods or beverages designed specifically for infants and shift to a diet that is more similar to the family diet. These may be some of the reasons for the higher dietary quality scores among the youngest children, but we cannot be certain. Having a tool, such as the modified DQIS, that can assess dietary quality among young children could be helpful to practitioners as they attempt to understand and influence the diets of young children.
Early dietary patterns have been associated with later health outcomes and behaviors (5–7, 34). Our findings suggest that an emphasis on healthy dietary patterns can be appropriate even very early in a child’s life and efforts may need to focus on children from households with lower incomes, education levels, and PIR. There are multiple efforts to help support optimal nutrition and feeding practices for US children that begin as early as birth and continue as a child gets older. For example, policies and programs aimed at supporting evidence-based maternity care practices have been found to increase breastfeeding initiation and duration (35). WIC provides supplemental foods, breastfeeding support, healthcare referrals, and nutrition education for low-income women and children and has recently revised the WIC Food Packages to more fully align with updated nutrition science (36–39). After the implementation of the new food packages, studies have reported positive changes in dietary patterns as well as consumption of different food categories (i.e., vegetables, grains) among children participating in WIC (40, 41). Nutrition standards for meals provided to infants and children in centers and daycare homes covered under the CACFP were also revised to align with the DGAs and went into effect in October 2017 (24). Studies have found that childcare providers who participate in the CACFP are more likely to implement obesity prevention measures such as serving fruits, vegetables, and whole grains and limiting fast food (42–44). Early care and education providers are also adopting more obesity prevention standards that can directly affect what children eat and drink, how active they are, reduce their screen time, and support moms who breastfeed (45).
Healthcare providers can also play an active role in helping parents and families understand the importance of a healthy diet starting at a very early age and these efforts may be especially important for families with lower household incomes, education levels, and PIR. This period of introduction to complementary foods and exploring different foods in a child’s life may be an opportune moment to engage families and caregivers in discussions about healthy eating patterns for their child(ren), especially given that research has found that families trust their healthcare provider for information on nutrition (46). The AAP has developed resources for both parents and providers that support healthy active living among children from birth to 5 y and support the AAP policy statement on the role of the pediatrician in primary prevention of obesity (47, 48). Given our findings, and other evidence that suggests the quality of dietary patterns decreases with age (12, 31, 32), efforts to work with families and caregivers beginning at an early age, and continuing throughout a child’s life, could help ensure children establish and maintain a healthy dietary pattern.
This study has several limitations. The original DQIS was developed and tested among children participating in WIC in Puerto Rico, where 99% of the population is Hispanic, the median household income is 34% lower than in the continental United States, and poverty is almost 4 times higher (49, 50). However, the subcomponents of DQIS are similar to those in the HEI (10) and the DQIS may be more applicable than other measures that are available. The DQIS was developed using a semiquantitative FFQ and our modified DQIS was applied to data obtained using 24-h dietary recalls. This allowed us to disaggregate foods into their subcomponents, which could have changed overall scores. In addition, data from a single 24-h recall were used to compute the DQIS scores in this study; this describes dietary quality on a given day and does not capture the usual intake or usual DQIS. We adapted the DQIS to include children 6–7 mo of age and children 2–4 y of age. Inclusion or exclusion of children 6–7 mo of age did not change our findings. For the extension of the modified DQIS to older children (2–4 y of age), we used the DGA recommendations associated with a sedentary child. Had we modelled on a more active child, then caloric needs would have been higher and modified DQIS scores may have changed. In addition, DGA recommendations were used to inform the scoring process of the modified DQIS subcomponents; however, we kept the original DQIS subcomponents. This resulted in having a drinking milk category but not a dairy category. Therefore, protein coming from dairy products (i.e., yogurt and cheese) was included in the modified DQIS protein category, which is not what occurs in the DGAs. We found that the protein subcomponent score and the overall modified DQIS score did not change regardless of including or excluding the protein from yogurt and cheese. Lastly, the reported dietary intake for young children was reported by a caregiver, usually the mother. However, they may not be aware of everything that a child ate during the day, especially if they were not with the child for the entire day. This could mean that we over- or underestimated overall intake for some children. There are also several strengths of this analysis. We used nationally representative data and were able to assess differences on a range of sociodemographic factors. We also used an existing coding scheme for food categories from the USDA’s Food Patterns Equivalent Database. And, lastly, when we extended the DQIS to other age groups and updated it, we based our scoring determination on existing recommendations from the DGAs, the USDA’s CACFP, the AAP, or the American Heart Association (1, 24, 25, 28).
In conclusion, our findings describe the dietary quality of young children in the United States. We found that dietary quality needs improvement and declines with age beginning as early as 1 y of age. Scores of dietary quality varied by sociodemographic factors and were higher among children who lived in households with higher incomes, education levels, and PIR. The modified DQIS is one tool that could be used to assess the dietary quality of young children. This may be important when identifying programmatic and policy efforts aimed at establishing and maintaining healthy dietary patterns beginning at an early age.
Supplementary Material
Acknowledgments
We acknowledge Dr Jennifer Seymour for her helpful review and comments on the manuscript and data analysis.
The authors reported no funding received for this study.
Abbreviations used:
- AAP
American Academy of Pediatrics
- CACFP
Child and Adult Care Food Program
- DGAs
2015–2020 US Dietary Guidelines for Americans
- DQIS
Diet Quality Index Score
- HEI
Healthy Eating Index
- PIR
poverty:income ratio
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
Footnotes
The authors’ responsibilities were as follows—LVM: analyzed the data; HCH: wrote the paper and had primary responsibility for the final content; and both authors: conceptualized and designed the study, critically reviewed and revised the paper, and read and approved the final manuscript. The authors report no conflicts of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Supplemental Tables 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Data described in the article, code book, and analytic code will be made available upon request to the corresponding author.
References
- 1.US Department of Health and Human Services, US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th ed. Washington (DC): US Department of Health and Human Services and USDA; 2015. [Google Scholar]
- 2.US Department of Health and Human Services. Physical activity guidelines for Americans. 2nd ed. Washington (DC): US Department of Health and Human Services; 2018. [Google Scholar]
- 3.Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days. Am J Prev Med 2016;50(6):761–79. [DOI] [PubMed] [Google Scholar]
- 4.Grimm KA, Kim SA, Yaroch AL, Scanlon KS. Fruit and vegetable intake during infancy and early childhood. Pediatrics 2014;134(Suppl 1):S63–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perrine CG, Galuska DA, Thompson FE, Scanlon KS. Breastfeeding duration is associated with child diet at 6 years. Pediatrics 2014;134(Suppl 1):S50–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan L, Li R, Park S, Galuska DA, Sherry B, Freedman DS. A longitudinal analysis of sugar-sweetened beverage intake in infancy and obesity at 6 years. Pediatrics 2014;134(Suppl 1):S29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rose CM, Savage JS, Birch LL. Patterns of early dietary exposures have implications for maternal and child weight outcomes. Obesity 2016;24:430–8. [DOI] [PubMed] [Google Scholar]
- 8.Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Beiler JS, Hess LB, Loken E, Birch LL. Effect of a responsive parenting educational intervention on childhood weight outcomes at 3 years of age: the INSIGHT randomized clinical trial. JAMA 2018;320(5):461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Office of Disease Prevention and Health Promotion. About the Dietary Guidelines: evolution, Rockville, MD: [Internet] [cited 19 December, 2018]. Available from: https://health.gov/dietaryguidelines/evolution.asp, US Department of Health and Human Services. Last updated 10/October/2019. [Google Scholar]
- 10.US Department of Agriculture, Center for Nutrition Policy and Promotion [Internet] [cited 4 December, 2018]. Available from: https://www.fns.usda.gov/resource/healthy-eating-index-hei, Healthy Eating Index, Alexandria, VA, January/31/2019, US Department of Agriculture. [Google Scholar]
- 11.World Health Organization. Indicators for the global monitoring framework on maternal, infant and young child nutrition. Geneva: WHO; 2014. [Google Scholar]
- 12.National Cancer Institute. Usual dietary intakes: food intakes, U.S. population, 2007–10: methods [Internet] [cited 4 December, 2018]. Bethesda, MD: National Institutes of Health; updated 24 April, 2018. Available from: https://epi.grants.cancer.gov/diet/usualintakes/pop/2007-10/index.html#results. [Google Scholar]
- 13.Ríos EM, Sinigaglia O, Biaz B, Campos M, Palacios C. Development of a diet quality score for infants and toddlers and its association with weight. J Nutrit Health Food Sci 2016;4(4):doi: 10.15226/jnhfs.2016.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. Vital Health Stat 2 2014;(162):1–33. [PubMed] [Google Scholar]
- 15.National Center for Health Statistics. NHANES response rates and population totals [Internet]. Last updated October/30/2018. Hyattsville, MD: Centers for Disease Control and Prevention. [cited 4 December, 2018]. Available from: https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx. [Google Scholar]
- 16.National Center for Health Statistics. NHANES dietary web tutorial: estimate population mean intakes [Internet]. Last updated May/3/2013. Hyattsville, MD: Centers for Disease Control and Prevention; [cited 26 August, 2019]. Available from: https://www.cdc.gov/nchs/tutorials/Dietary/Basic/PopulationMeanIntakes/intro.htm. [Google Scholar]
- 17.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88(2):324–32. [DOI] [PubMed] [Google Scholar]
- 18.Bowman SA, Clemens JC, Shimizu M, Friday JE, Moshfegh AJ. Food Patterns Equivalent Database 2015–2016: methodology and user guide. Beltsville, MD: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agriculture Research Service, USDA; 2018. [Google Scholar]
- 19.Bowman SA, Clemens JC, Friday JE, Lynch KL, Moshfegh AJ. Food Patterns Equivalents Database 2013–2014: methodology and user guide. Beltsville, MD: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, USDA; 2017. [Google Scholar]
- 20.US Department of Agriculture. Food Surveys Research Group home page. USDA Food and Nutrient Database for Dietary Studies 2013–2014 [Internet]. Washington (DC): Agricultural Research Service; 2016. [cited 5 January 2018]. Available from: http://www.ars.usda.gov/nea/bhnrc/fsrg. [Google Scholar]
- 21.US Department of Agriculture. Food Surveys Research Group home page, USDA Food and Nutrient Database for Dietary Studies 2015–2016 [Internet]. Washington (DC): Agricultural Research Service; 2018. [cited 5 January 2018]. Available from: http://www.ars.usda.gov/nea/bhnrc/fsrg. [Google Scholar]
- 22.US Department of Agriculture. Infant nutrition and feeding: a guide for use in the WIC and CSF programs. Washington (DC): Food and Nutrition Service, Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); 2009. [Google Scholar]
- 23.Pan American Health Organization, World Health Organization. Guiding principles for complementary feeding of the breastfed child. Washington (DC): WHO; 2003. [Google Scholar]
- 24.USDA. Child and Adult Care Food Program: meal pattern revisions related to the Healthy, Hunger-Free Kids Act of 2010. Final Rule. In: Food and Nutrition Service, editor. 7 CFR Parts 210, 215, 220, and 226. Fed Reg 2016;81(79):24348–83. [PubMed] [Google Scholar]
- 25.Heyman MB, Abrams SA; AAP Section on Gastroenterology, Hepatology, and Nutrition, Committee on Nutrition. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics 2017;139(6):e20170967. [DOI] [PubMed] [Google Scholar]
- 26.Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129(3):e827–e41. [DOI] [PubMed] [Google Scholar]
- 27.American Academy of Pediatrics Committee on Nutrition. Complementary feeding. In: Kleinman RE, Greer FR, editors. Pediatric nutrition. 7th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2014. p. 123–42. [Google Scholar]
- 28.Vos MB, Kaar JL, Welsh JA, Van Horn LV, Feig DI, Anderson CAM, Patel MJ, Cruz Munos J, Krebs NF, Xanthakos SA, et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American Heart Association. Circulation 2017;135(19):e1017–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Academy of Pediatrics Committee on Nutrition. Feeding the child. In: Kleinman RE, Greer FR, editors. Pediatric nutrition. 7th ed. Elk Grove, IL: American Academy of Pediatrics; 2014. p. 143–74. [Google Scholar]
- 30.Ahluwalia N, Herrick KA, Rossen LM, Rhodes D, Kit BK, Moshfegh A, Dodd KW. Usual nutrient intakes of US infants and toddlers generally meet or exceed Dietary Reference Intakes: findings from NHANES 2009–2012. Am J Clin Nutr 2016;104(4):1167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gu X, Tucker KL. Dietary quality of the US child and adolescent population: trends from 1999 to 2012 and associations with the use of federal nutrition assistance programs. Am J Clin Nutr 2017;105: 194–202. [DOI] [PubMed] [Google Scholar]
- 32.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US Dietary Guidelines for children and adolescents in the National Health and Nutrition Examination Survey population. J Acad Nutr Diet 2016;116:21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics. Feeding & nutrition tips: your 3-year-old [Internet] [cited 7 December, 2018]. Itasca, IL: American Academy of Pediatrics; 2016. Available from: https://www.healthychildren.org/English/ages-stages/toddler/nutrition/Pages/Feeding-and-Nutrition-Your-Three-Year-Old.aspx. [Google Scholar]
- 34.Park S, Pan L, Sherry B, Li R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014;134(Suppl 1): S56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feltner C, Weber RP, Stuebe A, Grodensky CA, Orr C, Viswanathan M. Breastfeeding programs and policies, breastfeeding uptake, and maternal health outcomes in developed countries. Comparative Effectiveness Review No. 210. Rockville, MD: Agency for Healthcare Research and Quality; 2018. [PubMed] [Google Scholar]
- 36.US Department of Agriculture, Food and Nutrition Service. About WIC—WIC at a glance [Internet] [cited 1 November, 2017]. Alexandria, VA: Food & Nutrition Service; 2013. Available from: https://www.fns.usda.gov/wic/about-wic-wic-glance. [Google Scholar]
- 37.US Department of Agriculture. USDA proclaims National WIC Breastfeeding Week and launches new campaign. Washington (DC): USDA; 2018. [cited 7 December, 2018]. Available from: https://www.usda.gov/media/press-release/2018/08/01/usda-proclaims-national-wic-breastfeeding-week-and-launches-new. [Google Scholar]
- 38.US Department of Agriculture, Food and Nutrition Service. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): revisions in the WIC food packages (Interim Rule). Fed Reg 2007;72(234):68965–9032. [Google Scholar]
- 39.US Department of Agriculture, Food and Nutrition Service. Final Rule: revisions in the WIC food package. Fed Reg 2014;79(42): 12273–300. [Google Scholar]
- 40.Tester JM, Leung CW, Crawford PB. Revised WIC food package and children’s diet quality. Pediatrics 2016;137(5): e20153557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamner HC, Paolicelli C, Casavale KO, Haake M, Bartholomew A. Food and beverage intake from 12 to 23 months by WIC status. Pediatrics 2019;143(3):e20182274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Blaine RE, Davison KK, Hesketh K, Taveras EM, Gillman MW, Benjamin Neelon SE. Child care provider adherence to infant and toddler feeding recommendations: findings from the Baby Nutrition and Physical Activity Self-Assessment for Child Care (Baby NAP SACC) study. Child Obes 2015;11(3):304–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu ST, Graffagino CL, Leser KA, Trombetta AL, Pirie PL. Obesity prevention practices and policies in child care settings enrolled and not enrolled in the Child and Adult Care Food Program. Matern Child Health J 2016;20:1933–9. [DOI] [PubMed] [Google Scholar]
- 44.Andreyeva T, Henderson KE. Center-reported adherence to nutrition standards of the Child and Adult Care Food Program. Child Obes 2018;14(6):421–8. [DOI] [PubMed] [Google Scholar]
- 45.CDC. Early care and education State Indicator Report, 2016. Atlanta, GA: US Department of Health and Human Services; 2016. [Google Scholar]
- 46.Glanz JM, Wagner NM, Narwaney KJ, Shoup JA, McClure DL, McCormick EV, Daley MF. A mixed methods study of parental vaccine decision making and parent–provider trust. Acad Pediatr 2013;13(5):481–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Academy of Pediatrics, Institute for Healthy Childhood Weight [Internet] [cited 7 December, 2018]. Available from: https://ihcw.aap.org/Pages/EFHALF.aspx. Building a Foundation for Healthy Active Living, Itasca, IL, American Academy of Pediatrics. [Google Scholar]
- 48.Daniels SR, Hassink SG; Committee on Nutrition. The role of the pediatricians in primary prevention of obesity. Pediatrics 2015;136(1):e275–e92. [DOI] [PubMed] [Google Scholar]
- 49.US Census Bureau. Quick facts: United States, 2018. [Internet] [cited 20 December, 2018]. Washington (DC): US Census Bureau. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045218. [Google Scholar]
- 50.US Census Bureau. Quick facts: Puerto Rico, 2018. [Internet] [cited 20 December, 2018]. Washington (DC): US Census Bureau. Available from: https://www.census.gov/quickfacts/fact/table/pr/PST045218. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


