In this multi-institutional case-control study, we describe how lower SES, increased social vulnerability, and minority racial and/or ethnic background increase the risk of MIS-C.
Abstract
OBJECTIVES:
To characterize the socioeconomic and racial and/or ethnic disparities impacting the diagnosis and outcomes of multisystem inflammatory syndrome in children (MIS-C).
METHODS:
This multicenter retrospective case-control study was conducted at 3 academic centers from January 1 to September 1, 2020. Children with MIS-C were compared with 5 control groups: children with coronavirus disease 2019, children evaluated for MIS-C who did not meet case patient criteria, children hospitalized with febrile illness, children with Kawasaki disease, and children in Massachusetts based on US census data. Neighborhood socioeconomic status (SES) and social vulnerability index (SVI) were measured via a census-based scoring system. Multivariable logistic regression was used to examine associations between SES, SVI, race and ethnicity, and MIS-C diagnosis and clinical severity as outcomes.
RESULTS:
Among 43 patients with MIS-C, 19 (44%) were Hispanic, 11 (26%) were Black, and 12 (28%) were white; 22 (51%) were in the lowest quartile SES, and 23 (53%) were in the highest quartile SVI. SES and SVI were similar between patients with MIS-C and coronavirus disease 2019. In multivariable analysis, lowest SES quartile (odds ratio 2.2 [95% confidence interval 1.1–4.4]), highest SVI quartile (odds ratio 2.8 [95% confidence interval 1.5–5.1]), and racial and/or ethnic minority background were associated with MIS-C diagnosis. Neither SES, SVI, race, nor ethnicity were associated with disease severity.
CONCLUSIONS:
Lower SES or higher SVI, Hispanic ethnicity, and Black race independently increased risk for MIS-C. Additional studies are required to target interventions to improve health equity for children.
What’s Known on This Subject:
The pandemic has highlighted racial and socioeconomic disparities in children affected by coronavirus disease 2019. Data suggest that children from Black or Hispanic racial and/or ethnic backgrounds are also at increased risk for development of multisystem inflammatory syndrome in children.
What This Study Adds:
In this multi-institutional case-control study, children from minority racial and/or ethnic backgrounds were disproportionately at risk for development of multisystem inflammatory syndrome in children, and this finding could not be entirely accounted for by socioeconomic status or social vulnerability index.
Early in the coronavirus disease 2019 (COVID-19) pandemic, which first emerged in December 2019, most children appeared to only develop mild, if any, clinical manifestations of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.1–3 However, cases soon began to emerge of a hyperinflammatory condition occurring in children 3 to 4 weeks after COVID-19 infection that has since been termed multisystem inflammatory syndrome in children (MIS-C).4–8 MIS-C is characterized by fever, elevated levels of inflammatory markers, multisystem organ involvement, and evidence of COVID-19 infection (current or previous) or confirmed contact with COVID-19.9,10 MIS-C shares features of Kawasaki disease (KD), including fever, elevated levels of inflammatory markers, rash, mucocutaneous findings, and coronary artery complications. However, significant differences in patient demographics and laboratory values between MIS-C and KD have also been reported.6,11,12
The pandemic has highlighted several racial, ethnic, and socioeconomic disparities among individuals with COVID-19. National data from the Centers for Disease Control and Prevention (CDC) reveal that Black and Hispanic/Latino individuals have disproportionately higher rates of infection and death from COVID-19 compared with white individuals.13 County- and neighborhood-level studies reveal disproportionately higher rates of SARS-CoV-2 infection, morbidity, and/or death in areas that have a greater percentage of minorities or are socioeconomically disadvantaged.14–17
In the pediatric population, racial and/or ethnic minority background and lower socioeconomic status (SES) (measured by median family income) have been shown to independently increase risk for SARS-CoV-2 infection.18 In early case series, authors reported that MIS-C, like SARS-CoV-2 infection, may also disproportionately affect minority populations.7,19 As of January 2021, 37% of MIS-C cases reported to the CDC were in children who are Hispanic and 34% were in non-Hispanic Black children, compared with 19% in white children.4 However, the impact of socioeconomic disparities on MIS-C has not been investigated. Previous research has revealed that SES has an important impact on health outcomes in several pediatric diseases.20–26 It is essential, therefore, to further characterize the impact of social and economic determinants of health and racial disparities in MIS-C.
Methods
Population
This retrospective case-control study included patients diagnosed with MIS-C between January 1, 2020, and September 1, 2020, in Massachusetts. Patients treated at Boston Children’s Hospital (BCH), Massachusetts General Hospital (MGH), and Boston Medical Center (BMC) were included.
To better evaluate the impact of SES on MIS-C, we compared children with MIS-C with the following groups (Supplemental Table 5):
children with COVID-19 infection (excluding patients with MIS-C), including both symptomatic and asymptomatic cases, between January 1, 2020, and July 1, 2020;
the MIS-C “rule-out” group of children evaluated for MIS-C at BCH who ultimately did not meet CDC criteria for MIS-C diagnosis between January 1, 2020, and September 1, 2020;
children hospitalized for a febrile illness (excluding KD, COVID-19, and MIS-C) at BCH between January 1, 2020, and September 1, 2020;
children diagnosed with KD at BCH27 between 2010 and 2016; and
children in Massachusetts based on the 2010 US Census.
Exclusion criteria included age >21 years, a non-Massachusetts address, and congenital heart disease, except for bicommissural aortic valve, mitral valve prolapse, and hemodynamically insignificant ventricular septal defects. This study was approved or exempted by the institutional review board of each institution, and patient consent was obtained when applicable.
Data Collection and Definitions
Electronic medical records were reviewed to obtain patients’ demographics and clinical course. MIS-C was defined, by using the CDC case definition, as an individual aged <21 years presenting with fever, laboratory evidence of inflammation, clinically severe illness with multisystem (≥2) organ involvement requiring hospitalization, no alternative plausible diagnosis, and test results positive for current or recent SARS-CoV-2 infection by reverse transcriptase polymerase chain reaction (RT-PCR), serology, or antigen testing or COVID-19 exposure within the 4 weeks before the onset of symptoms.10 All cases of MIS-C (and MIS-C rule-out) were adjudicated by a multidisciplinary team of experts, including rheumatologists, cardiologists, infectious disease specialists, and hematologists. Relevant clinical information, including age, past medical history, clinical symptoms at presentation, and laboratory and diagnostic testing results (excluding sociodemographic data), was included in a form sent to members of the expert team, who were then asked whether the patient met the CDC definition for MIS-C. The final adjudication was based on the majority vote, and any tied cases were discussed as a group to reach a consensus.
Patients’ race and ethnicity were self-reported by patients or parents at the time of hospital admission. Understanding that race and ethnicity are complex sociopolitical constructs, patients were grouped into categories according to the US Census and Office of Management and Budget.28 Race was classified as white, Black, Asian American, or other (including American Indian or Alaskan native and native Hawaiian or other Pacific Islander). Patients of mixed race were classified as “other.” Ethnicity was classified as Hispanic (ie, Cuban, Mexican, Puerto Rican, South or Central American, or other Spanish culture or origin regardless of race) or non-Hispanic. Ventricular dysfunction was defined as a left ventricular ejection fraction <55%. Coronary artery z scores were calculated for the left main coronary artery, proximal right coronary artery, and proximal left anterior descending artery by using the Boston formula.27 Coronary artery dilation was defined as a coronary artery z score ≥2 but <2.5, and coronary artery aneurysms were defined as having a coronary artery z score ≥2.5.27
A neighborhood SES summary score and the social vulnerability index (SVI) were calculated by using the 2010 US Census on the basis of patient address.29,30 The variables for the neighborhood SES summary score included the following: (1) a log of the median household income; (2) a log of the median value of housing units; (3) the percentage of households receiving interest, dividend, or net rental income; (4) the percentage of adults 25 years of age or older in the household who had completed high school; (5) the percentage of adults 25 years of age or older in the household who had completed college; and (6) the percentage of employed persons 16 years of age or older in the household in executive, managerial, or professional specialty occupations.29 The SVI was calculated by using 15 variables classified in 4 themes: (1) SES; (2) housing composition and disability; (3) minority status and language; and (4) housing and transportation (Supplemental Fig 2).30 Neighborhood SES summary scores were reported as z scores for each of the variables by using all census tracts in Massachusetts and then summed to determine the overall neighborhood SES summary score. SVI was reported as a percentage; a higher SVI denotes increased vulnerability of a community. For children in Massachusetts, the neighborhood SES summary score and SVI were calculated by weight-adjusting the score for each census tract on the basis of the number of children <18 years of age in each tract.
Outcomes
The primary outcome was the diagnosis of MIS-C, and predictor variables included SES, SVI, race, and ethnicity. As a secondary aim, we explored the impact of the neighborhood SES summary score, the SVI, race, and ethnicity on treatment needs and disease severity (days of fever, hospital length of stay, ICU admission and length of stay, inotrope requirement, positive pressure ventilation, intubation, and cardiac involvement).
Statistical Analyses
In the descriptive analysis, continuous variables were summarized with median and interquartile range (IQR), and categorical variables were summarized as frequencies and percentages. The neighborhood SES summary score and SVI were compared across groups by using the Kruskal-Wallis test with pairwise comparisons. The proportion of patients in the lowest SES quartile and highest SVI quartile, as well as race and/or ethnicity in each group, was compared by using the Fisher’s exact test. Univariable and multivariable logistic regressions were used to examine the impact of neighborhood SES or SVI and race and/or ethnicity on children diagnosed with MIS-C (versus children in Massachusetts without MIS-C). Patients with MIS-C in the lowest SES quartile and highest SVI quartile were compared with those in the other quartiles by using the Kruskal-Wallis test and Fisher’s exact test. All analyses were performed with Rstudio: Integrated Development Environment for R (Rstudio, Inc, Boston, MA). A 2-tailed adjusted P value <.05 was deemed statistically significant. The P values were adjusted for false discovery rate by using the Benjamini Y and Hochberg Y method.
Results
Sample Characteristics
During the study period, a total of 43 patients (25 boys [58%]) were diagnosed with MIS-C, including 29 patients from BCH, 12 from MGH, and 2 from BMC. The median age was 9.7 years (IQR 6.5 to 16.3) at the time of diagnosis. Regarding race and/or ethnicity, 19 (44%) were Hispanic (white, n = 5; Black, n = 4; other, n = 10), and of the non-Hispanic patients, 7 (16%) were white, 7 (16%) were Black, 2 (5%) were Asian American, and 3 (7%) were classified as other. Overall, 19 patients (44%) had preexisting comorbidities, with the most common being obesity (n = 17 [40%]) and asthma (n = 6 [14%]). ICU admission was required for 19 patients (44%): fluid resuscitation and monitoring in 7 (16%) patients, vasopressors or vasoactive support in 8 (19%) patients, noninvasive positive pressure ventilation in 5 (12%) patients, and mechanical ventilation in 4 (9%) patients. Cardiac involvement was found in 33 (77%) patients, including elevated brain natriuretic peptide levels in 25 (63%) patients, elevated troponin levels in 13 (32%) patients, ventricular dysfunction in 21 (49%) patients, and coronary artery dilation or aneurysm in 10 (23%) patients. The majority of patients with MIS-C had positive antibody test results for SARS-CoV-2 (n = 29 [67%]). Results of RT-PCR tests for SARS-CoV-2 were positive for 20 patients (47%), and 15 patients (35%) had a COVID-19 exposure but negative RT-PCR and antibody test results. A majority of patients were treated with intravenous immunoglobulin (n = 34 [79%]); other treatments used included steroids for 30 (70%) patients and anakinra for 9 (21%) patients. Six patients (14%) received no immunomodulatory treatment.
Association of SES, SVI, and Race and/or Ethnicity With MIS-C Diagnosis
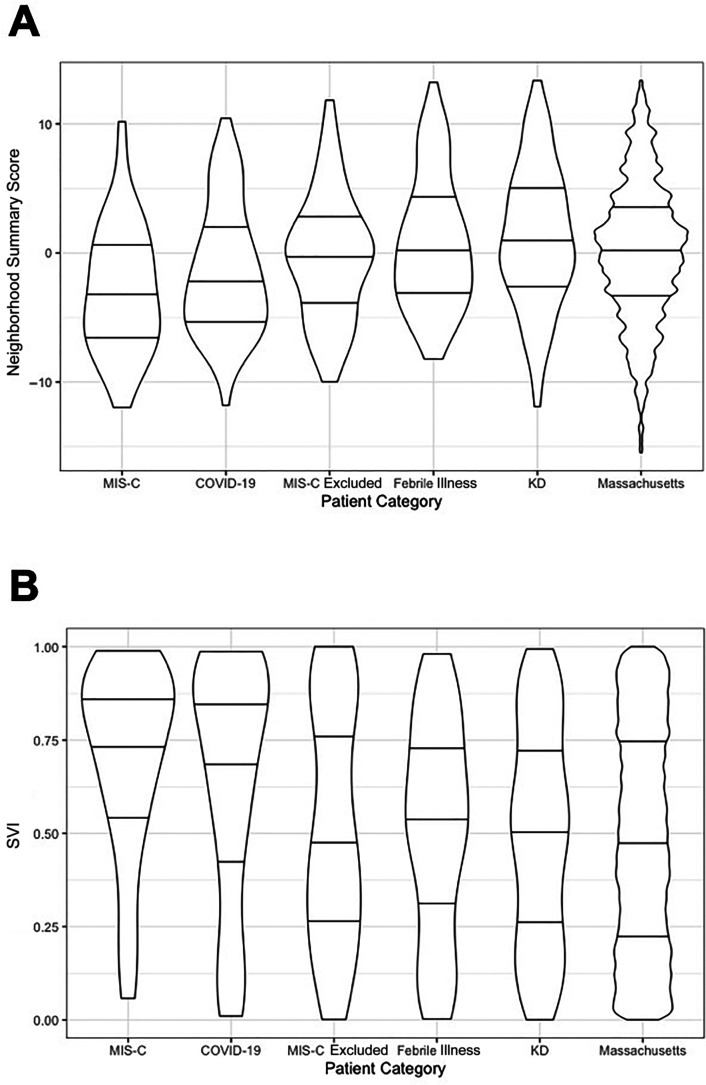
Table 1 summarizes the neighborhood SES summary score, the SVI, race, and ethnicity across the comparison groups. Table 2 reveals expanded results with the specific variables and themes included in both measures of SES. There was no significant difference in the neighborhood SES summary score and the SVI between each of the 3 hospitals’ MIS-C groups. In patients with MIS-C, the neighborhood SES summary z score ranged from −12.0 to 10.2, with a median of −3.5 (IQR −6.7 to 0.3). The neighborhood SES summary score was significantly lower for patients with MIS-C than for children in Massachusetts (P = .0009), children hospitalized with febrile illness (P = .0009), children with MIS-C rule-out (P = .02), and children with KD (P < .0001); but it was similar for patients with COVID-19 (P = .23) (Fig 1, Table 2). More than half of children with MIS-C were in the lowest SES quartile (n = 22 [51%]). The SVI score, in which higher score denotes increased vulnerability, ranged from 5.8% to 98.9%, with a median of 76.5% (IQR 57.6% to 91.8%) in patients with MIS-C. SVI was significantly higher for patients with MIS-C than for children in Massachusetts (P < .0001), children hospitalized with febrile illness (P = .0006), children with MIS-C rule-out (P = .04), and children with KD (P = .0001); but it was similar for patients with COVID-19 (P = .78) (Fig 1, Table 2). This association was not only found for the overall SVI but also found for all individual categories (SES, housing composition and disability, minority status and language, and housing and transportation; Table 2). More than half of children with MIS-C were in the highest SVI quartile (n = 23 [53%]). Patients with MIS-C and COVID-19 were more likely to be from racial and/or ethnic minority groups (Black and Hispanic) compared with children hospitalized with febrile illness, MIS-C rule-out, or KD or children in Massachusetts (Table 1).
TABLE 1.
Distribution of Neighborhood SES, SVI, and Race and/or Ethnicity in Children With MIS-C, Children With COVID-19, and Children in Massachusetts
| MIS-C (n = 43) | COVID-19 (n = 67) | Massachusetts | P | MIS-C Versus COVID-19, P | MIS-C Versus Massachusetts, P | |
|---|---|---|---|---|---|---|
| Neighborhood SES summary score,a median (IQR) | −3.5 (−6.7 to 0.3) | −2.4 (−5.4 to 1.8) | 0.2 (−3.3 to 3.5) | <.001 | .15 | <.001 |
| Lowest quartile, n (%) | 22 (51) | 28 (42) | (24) | <.001 | .44 | <.001 |
| SVI, median (IQR) | 76.5 (57.6 to 91.8) | 73.4 (46.7 to 92.2) | 47.6 (22.2 to 75.3) | <.001 | .73 | <.001 |
| Highest quartile, n (%) | 23 (53) | 31 (46) | (25) | <.001 | .59 | <.001 |
| Race and/or ethnicity, n (%) | ||||||
| White, non-Hispanic | 7 (16) | 12 (18) | (77) | <.001 | .99 | <.001 |
| White, Hispanic | 5 (12) | 1 (1) | (5) | .04 | .03 | .04 |
| Black, non-Hispanic | 7 (16) | 11 (16) | (6) | <.001 | .99 | .02 |
| Black, Hispanic | 4 (10) | 3 (4) | (1) | <.001 | .43 | <.001 |
| Asian American | 2 (5) | 3 (4) | (5) | .99 | .99 | .99 |
| Other, non-Hispanic | 3 (7) | 5 (7) | (0.1) | <.001 | .99 | <.001 |
| Other, Hispanic | 10 (23) | 18 (27) | (1) | <.001 | .82 | <.001 |
Neighborhood SES summary scores are reported as z scores.
SVI is a percentage, with higher percentages denoting increased vulnerability.
TABLE 2.
Distribution of Neighborhood SES and SVI in MIS-C Versus All Comparison Groups
| MIS-C (n = 43) | COVID-19 (n = 67) | MIS-C Rule-Out (n = 52) | Febrile Illness (n = 96) | KD (n = 297) | Massachusetts | P | |
|---|---|---|---|---|---|---|---|
| Neighborhood summary score,a median (IQR) | −3.5 (−6.7 to 0.3) | −2.4 (−5.4 to 1.8) | −0.1 (−3.9 to 2.5) | 0.4 (−3.0 to 4.2) | 0.8 (−2.5 to 5.1) | 0.2 (−3.3 to 3.5) | <.001 |
| Household income | −0.6 (−1.2 to 0.3) | −0.2 (−0.9 to 0.5) | 0.1 (−0.7 to 0.5) | 0.1 (−0.4 to 0.7) | 0.3 (−0.3 to 0.8) | 0.3 (−0.4 to 0.8) | <.001 |
| Household value | 0 (−0.2 to 0.3) | 0.1 (−0.3 to 0.6) | 0.1 (−0.2 to 0.5) | 0.2 (−0.3 to 0.8) | 0.2 (−0.2 to 0.8) | 0 (−0.6 to 0.5) | <.001 |
| Percentage of households with income | −0.6 (−1.2 to 0.1) | −0.5 (−1.1 to 0.1) | 0 (−0.8 to 0.3) | −0.2 (−0.7 to 0.6) | 0 (−0.6 to 0.7) | 0 (−0.7 to 0.6) | <.001 |
| Percentage of adults who completed high school | −0.6 (−1.5 to 0.4) | −0.2 (−1.1 to 0.5) | 0.4 (−0.5 to 0.5) | 0.3 (−0.5 to 0.7) | 0.4 (−0.3 to 0.8) | 0.4 (−0.3 to 0.7) | <.001 |
| Percentage of adults who completed college | −0.7 (−1.3 to −0.2) | −0.6 (−1.1 to 0.2) | −0.1 (−0.9 to 0.3) | −0.1 (−0.8 to 0.7) | −0.1 (−0.7 to 1.0) | −0.2 (−0.8 to 0.6) | <.001 |
| Percentage of employees in executive jobs | −0.6 (−1.4 to 0) | −0.4 (−0.9 to 0.2) | −0.3 (−0.8 to 0.4) | −0.1 (−0.7 to 0.8) | 0.1 (−0.6 to 1.0) | −0.1 (−0.6 to 0.6) | <.001 |
| SVI,b median (IQR) | 76.5 (57.6 to 91.8) | 73.4 (46.7 to 92.2) | 44.3 (26.1 to 84.6) | 52.8 (28.7 to 75.3) | 51.9 (22.7 to 74.8) | 47.6 (22.2 to75.3) | <.001 |
| SES | 75.8 (52.5 to 86.5) | 73.8 (26.6 to 91.6) | 42.6 (25.7 to 81.3) | 43.0 (20.3 to 72.5) | 45.0 (19.3 to 70.2) | 46.5 (22.1 to 73.8) | <.001 |
| Housing composition and disability | 59.0 (47.7 to 78.5) | 63.2 (38.4 to 87.1) | 48.7 (24.2 to 74.2) | 50.5 (32.9 to 80.1) | 48.4 (28.9. 75.5) | 52.5 (30.0 to 75.8) | .04 |
| Minority status and language | 84.8 (70.7 to 90.0) | 84.1 (39.6 to 91.4) | 58.0 (28.7 to 90.0) | 58.9 (32.6 to 79.5) | 58.0 (31.0 to 78.1) | 46.5 (22.8 to 74.4) | <.001 |
| Housing and transportation | 63.8 (47.1 to 84.1) | 66.3 (38.9 to 82.4) | 58.2 (22.8 to 80.3) | 52.4 (32.9 to 69.3) | 49.9 (25.9 to 72.3) | 46.2 (23.1 to 71.1) | <.001 |
Neighborhood summary scores are reported as z scores.
SVI is a percentage, with higher percentages denoting increased vulnerability.
FIGURE 1.
A and B, Violin plot of neighborhood SES summary score (A) and SVI (B), including the median and 25th and 75th percentiles in patients with MIS-C versus children (1) with COVID-19, (2) evaluated for MIS-C who did not meet CDC criteria, (3) hospitalized for febrile illness, (4) with KD, and (5) in Massachusetts. In this figure, we compare the distribution of the neighborhood SES summary score and SVI between each group studied. The vertical axis corresponds to the neighborhood SES summary score or the SVI, and the width of each curve corresponds to the frequency of patients within the group with that score or index.
The neighborhood SES summary score, the SVI, race, and ethnicity were all associated with MIS-C diagnosis in the univariable analysis (Table 3). In the multivariable analysis (with inclusion of SES and SVI in separate models), measures of SES and race and/or ethnicity independently conferred higher risk for MIS-C diagnosis (Table 3). Specifically, Black and Hispanic children, as well as children in the lowest SES quartile and highest SVI quartile, had significantly increased odds of developing MIS-C.
TABLE 3.
Association of Neighborhood SES and Race and/or Ethnicity With MIS-C Diagnosis
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Neighborhood SES summary scorea | ||||
| Lowest SES quartile | 3.2 (1.8–5.9) | <.001 | 2.2 (1.1–4.4) | .02 |
| Race | ||||
| White, non-Hispanic | 1 | — | — | — |
| White, Hispanic | 12.1 (3.6–38.0) | <.001 | 8.7 (2.5–28.2) | <.001 |
| Black, non-Hispanic | 12.0 (4.1–37.0) | <.001 | 10.8 (3.7–31.8) | <.001 |
| Black, Hispanic | 84.0 (22.0–278.4) | <.001 | 49.8 (12.4–176.8) | <.001 |
| Asian American | 4.6 (0.7–19.2) | .06 | 5.4 (0.7–40.8) | .05 |
| Other, non-Hispanic | 21.4 (4.6–77.2) | <.001 | 14.8 (3.1–55.3) | <.001 |
| Other, Hispanic | 19.2 (3.6–38.0) | <.001 | 18.8 (7.2–51.8) | <.001 |
| SVIb | ||||
| Highest SVI quartile | 3.4 (1.9–6.3) | <.001 | 2.8 (1.5–5.1) | .02 |
| Race | ||||
| White, non-Hispanic | 1 | — | — | — |
| White, Hispanic | 12.1 (3.6–38.0) | <.001 | 8.8 (2.5–28.5) | <.001 |
| Black, non-Hispanic | 12.0 (4.1–37.0) | <.001 | 10.3 (3.5–30.3) | <.001 |
| Black, Hispanic | 84.0 (22.0–278.4) | <.001 | 51.4 (12.8–182.3) | <.001 |
| Asian American | 4.6 (0.7–19.2) | .06 | 4.5 (0.7–18.8) | .06 |
| Other, non-Hispanic | 21.4 (4.6–77.2) | <.001 | 15.4 (3.2–57.3) | <.001 |
| Other, Hispanic | 19.2 (3.6–38.0) | <.001 | 19.3 (7.4–53.1) | <.001 |
Comparisons were made between patients with MIS-C and the general Massachusetts population. CI, confidence interval; OR, odds ratio; —, not applicable.
Neighborhood summary scores are reported as z scores.
SVI is a percentage, with higher percentages denoting increased vulnerability.
Association of SES, SVI, and Race and/or Ethnicity With MIS-C Outcomes
There was no significant difference in demographics, hospital course, or cardiac complications in patients with MIS-C in the lowest SES quartile versus others or in the highest SVI quartile versus others (Table 4). There was also no difference in hospital course or cardiac complications based on race or ethnicity.
TABLE 4.
Associations Between SES and Demographics and Clinical Outcomes in Patients With MIS-C
| Neighborhood SES Summary Scorea | SVIb | |||||
|---|---|---|---|---|---|---|
| Lowest Quartile (n = 22) | Top 3 Quartiles (n = 21) | P | Highest Quartile (n = 23) | Bottom 3 Quartiles (n = 20) | P | |
| Demographics | ||||||
| Age, y, median (IQR) | 9.6 (6.3 to 13.3) | 10.3 (7.0 to 16.6) | .58 | 9.7 (6.5 to 14.9) | 9.3 (6.3 to 16.6) | .88 |
| Male sex, n (%) | 13 (61) | 12 (57) | .99 | 14 (61) | 11 (55) | .76 |
| Weight, kg, median (IQR) | 44.1 (27.2 to 61.7) | 36.0 (22.7 to 726.3) | .58 | 45.1 (28.5 to 74.1) | 33.7 (21.6 to 72.5) | .53 |
| BMI, median (IQR) | 21.3 (18.4 to 26.2) | 22.3 (16.7 to 27.6) | .95 | 24.2 (18.6 to 29.8) | 19.9 (16.5 to 25.2) | .10 |
| Comorbidities, n (%) | 11 (50) | 8 (38) | .54 | 11 (48) | 8 (40) | .76 |
| Obesity, n (%) | 8 (36) | 9 (43) | .76 | 10 (43) | 7 (35) | .76 |
| Hospital course | ||||||
| Days of fever, median (IQR) | 6.0 (4.0 to 7.8) | 7.0 (5.0 to 7.0) | .52 | 7.0 (4.5 to 7.5) | 6.5 (5.0 to 7.3) | .94 |
| Hospital LOS, d, median (IQR) | 6.5 (4.0 to 9.8) | 6.0 (3.0 to 10.0) | .78 | 6.0 (4.0 to 9.5) | 5.5 (3.0 to 10.5) | .67 |
| ICU admission, n (%) | 11 (50) | 8 (38) | .54 | 12 (52) | 7 (35) | .36 |
| ICU LOS, d, median (IQR) | 4.5 (2.0 to 6.6) | 4.0 (3.0 to 7.0) | .77 | 4.5 (2.0 to 7.0) | 4.0 (3.0 to 8.0) | .56 |
| Inotropes, n (%) | 4 (18) | 4 (19) | .99 | 4 (17) | 4 (20) | .99 |
| PPV, n (%) | 3 (14) | 2 (10) | .99 | 2 (9) | 3 (15) | .65 |
| Intubation, n (%) | 2 (9) | 2 (10) | .99 | 3 (13) | 1 (5) | .61 |
| Cardiac involvement, n (%) | ||||||
| Elevated BNP level | 15 (68) | 10 (48) | .33 | 14 (61) | 11 (55) | .75 |
| Elevated troponin level | 5 (23) | 8 (38) | .733 | 6 (26) | 7 (35) | .74 |
| Ventricular dysfunction | 9 (41) | 12 (57) | .37 | 10 (43) | 11 (55) | .55 |
| Coronary artery dilation | 8 (36) | 2 (10) | .07 | 8 (35) | 2 (10) | .08 |
| Atrioventricular block | 2 (9) | 2 (10) | .99 | 2 (9) | 2 (10) | .99 |
| Treatment, n (%) | ||||||
| IVIg | 17 (77) | 17 (81) | .99 | 19 (83) | 15 (75) | .71 |
| Steroids | 16 (73) | 14 (67) | .74 | 17 (74) | 13 (65) | .74 |
| Anakinra | 6 (27) | 3 (14) | .46 | 5 (22) | 4 (20) | .99 |
BNP, brain natriuretic peptide; IVIg, intravenous immunoglobulin; LOS, length of stay; PPV, positive pressure ventilation.
Neighborhood summary scores are reported as z scores.
SVI is a percentage, with higher percentages denoting increased vulnerability.
Discussion
In this retrospective case-control study, we found that patients diagnosed with MIS-C had lower SES, had increased social vulnerability, and were more likely to be Black and/or Hispanic compared with the general population of Massachusetts children.
Previous studies have revealed that that higher rates of SARS-CoV-2 infection are found in neighborhoods with lower income and educational attainment, both of which are factors that were incorporated into the neighborhood SES summary score used in this study.29 Goyal et al18 most recently showed that SARS-CoV-2 infection rates among children, in particular, were associated with lower median family income. Furthermore, the SVI was used in this study to characterize factors beyond education and income that could contribute to disparities. In Massachusetts, neighborhood proportion of foreign-born citizens, mean household size, and proportion of food service workers were associated with increased COVID-19 rate.31 Individuals more likely to work in essential occupations, more likely to be unable to work from home, and more likely to need to use public transportation have likely increased exposure to the virus.32,33 Our findings revealed lower neighborhood household income and educational attainment and greater neighborhood social vulnerability regarding housing, transportation, minority status, and language among both the MIS-C and COVID-19 groups. It is therefore plausible that the elevated risk of MIS-C in the lower SES and greater SVI neighborhoods is a result of increased exposure to COVID-19.
Although SES and underrace and/or ethnicity are strongly correlated,34 there appears to be an independent risk of MIS-C in Black and Hispanic patients. Our findings are consistent with data from the CDC in which the highest rates of childhood COVID-19 were found in children of Hispanic ethnicity.13 Two recent studies reveal that Black children have higher rates of COVID-19 infection than white children, similar to the disparities seen in adult COVID-19 cases.18,35 However, the increased risk in patients from minority racial and/or ethnic groups appears to extend beyond their SES on the basis of our findings revealing an association of race and/or ethnicity with MIS-C even after adjustment for SES via 2 measures. Although the neighborhood SES summary score is limited to an assessment of income and education to quantify SES, the use of the SVI enabled an even more complex representation of contributing socioeconomic factors by including an array of measures ranging from housing composition to language to transportation, which were also found to be associated with MIS-C in our study.30 The effect of race and ethnicity on health disparities can be related to a multitude of alternate complex factors, including increased risk of comorbidities, differential access to care, provider bias, and the effects of ongoing racism and/or discrimination and subsequent chronic stress.14,36–38 These factors can cause racial and ethnic disparities independent of SES and could be targets for interventions to improve outcomes.36,38
Although we looked at race and ethnicity in our study, the role of host and environmental factors underlying differential MIS-C rates remains unclear. Despite being an early hot spot with a high incidence of patients with SARS-CoV-2 infection, China, Japan, and South Korea have not reported patients with MIS-C or similar KD-like presentations.39,40 The cause of this variation remains unclear and may be related to genetic or environmental predisposition.41–43 Genetic polymorphisms and environmental factors have been implicated in the development of KD and could play a similar role in MIS-C.44–46 The artificial nature of racial and ethnic grouping as a social and political construct limits conclusions regarding the role of population genetics in our findings.47,48 It is, however, well documented that inequities in environmental exposure exist on the basis of race and/or ethnicity and SES.49,50 Future studies exploring genetic sequencing and environmental factors will be key to better understanding their role in MIS-C.
Our findings provide insight into avenues for interventions to reduce racial and socioeconomic disparities in MIS-C and children’s health during and beyond this pandemic. Steps to ameliorate risk for exposure to COVID-19 are key to limiting incidence of MIS-C. Identifying neighborhoods in which children are most likely to have COVID-19 exposure can inform public health efforts and may allow for proactive protection of at-risk populations. This may include increasing available testing, prioritizing vulnerable neighborhoods for vaccination, and ensuring that families can access health care resources without barriers due to language or insurance status.14,51–53 Pediatricians also may support ongoing advocacy efforts to combat systemic racism, discrimination, and implicit bias, which can contribute to race- and ethnicity-related health disparities irrespective of SES.54–57
Limitations of our study include the small sample size of patients with MIS-C in a single state and the potential lack of generalizability to other states with different demographics. The inclusion of 3 large pediatric centers that cared for pediatric patients during the pandemic ensured that we captured most patients in Massachusetts admitted with MIS-C (43 of 54 reported to the Department of Public Health). The control groups consisted of patients treated at BCH, whereas patients were diagnosed with MIS-C across 3 academic centers. We did not find significant differences in SES between patients with MIS-C treated at the 3 centers, and we compared patients with MIS-C with children in Massachusetts to minimize that possible bias. Although we did not find any significant association between SES or race and/or ethnicity and treatment course or outcomes, statistical power was limited by the small number of patients, and this question would be more effectively answered through large multicenter registries. Patients reporting their race and ethnicity also may not have been given options within the confines of the electronic medical record or verbal questioning to accurately self-identify. Although all MIS-C case adjudication was performed by using forms that included only relevant clinical information, experts were not specifically blinded, and known sociodemographic information from participating in the patients’ clinical care may have influenced their decision. Lastly, this study relied on the 2010 US Census, and neighborhoods may have changed SES characteristics over the last decade.
Conclusions
Measures of lower SES or higher social vulnerability, Black race, and Hispanic ethnicity were independent risk factors for MIS-C in children in Massachusetts. The disproportionate number of cases of MIS-C in minority and socioeconomically disadvantaged pediatric populations may be due to increased risk of SARS-CoV-2 infection. In future studies, researchers should explore the underlying social, structural, economic, environmental, and genetic risk factors to allow for targeted interventions to support vulnerable pediatric populations most affected by MIS-C and improve health equity.
Glossary
- BCH
Boston Children’s Hospital
- BMC
Boston Medical Center
- CDC
Centers for Disease Control and Prevention
- COVID-19
coronavirus disease 2019
- IQR
interquartile range
- KD
Kawasaki disease
- MGH
Massachusetts General Hospital
- MIS-C
multisystem inflammatory syndrome in children
- RT-PCR
reverse transcriptase polymerase chain reaction
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- SES
socioeconomic status
- SVI
social vulnerability index
Footnotes
Drs Javalkar and Robson contributed to study design, collected data, contributed to data interpretation, and drafted the initial manuscript; Ms Bohling and Drs Arya, Servattalab, Sekhavat, and Kobayashi collected data; Drs Roberts and Campell collected data and contributed to data interpretation; Drs Gaffney, Newburger, and de Ferranti, Ms Baker, Dr Lee, Ms Day-Lewis, and Drs Bucholz, Son, Henderson, and Kheir contributed to data interpretation; Dr Friedman conceptualized and designed the study and reviewed and revised the manuscript; Dr Dionne conceptualized and designed the study, coordinated and supervised data collection, and conducted the data analysis; and all authors reviewed and revised the manuscript and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Campbell was supported by Agency for Healthcare Research and Quality grant T32HS000063 as part of the Harvard-wide Pediatric Health Services Research Fellowship Program. Dr Roberts was supported by National Institutes of Health grant 5T32AI007512-34. The funder or sponsor did not participate in the work. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Castagnoli R, Votto M, Licari A, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020;174(9):882–889 [DOI] [PubMed] [Google Scholar]
- 2.Patel NA. Pediatric COVID-19: systematic review of the literature. Am J Otolaryngol. 2020;41(5):102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu X, Zhang L, Du H, et al.; Chinese Pediatric Novel Coronavirus Study Team . SARS-CoV-2 infection in children. N Engl J Med. 2020;382(17):1663–1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Health department-reported cases of multisystem inflammatory syndrome in children (MIS-C) in the United States. Available at: https://www.cdc.gov/mis-c/cases/index.html. Accessed January 28, 2021
- 5.Belhadjer Z, Méot M, Bajolle F, et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020;142(5):429–436 [DOI] [PubMed] [Google Scholar]
- 6.Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020;395(10239):1771–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607–1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toubiana J, Poirault C, Corsia A, et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19. Available at: https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed July 12, 2020
- 10.Centers for Disease Control and Prevention. Information for healthcare providers about multisystem inflammatory syndrome in children (MIS-C). Available at: https://www.cdc.gov/mis-c/hcp/. Accessed July 12, 2020
- 11.Whittaker E, Bamford A, Kenny J, et al.; PIMS-TS Study Group and EUCLIDS and PERFORM Consortia . Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324(3):259–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee PY, Day-Lewis M, Henderson LA, et al. Distinct clinical and immunological features of SARS-COV-2-induced multisystem inflammatory syndrome in children. J Clin Invest. 2020;130(11):5942–5950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. COVID data tracker. Available at: https://www.cdc.gov/covid-data-tracker/index.html#demographics. Accessed September 1, 2020
- 14.Millett GA, Jones AT, Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths across New York city boroughs. JAMA. 2020;323(21):2192–2195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahajan UV, Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. J Public Health (Oxf). 2020;42(3):445–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–1262 [DOI] [PubMed] [Google Scholar]
- 18.Goyal MK, Simpson JN, Boyle MD, et al. Racial and/or ethnic and socioeconomic disparities of SARS-CoV-2 infection among children. Pediatrics. 2020;146(4):e2020009951. [DOI] [PubMed] [Google Scholar]
- 19.Dufort EM, Koumans EH, Chow EJ, et al.; New York State and Centers for Disease Control and Prevention Multisystem Inflammatory Syndrome in Children Investigation Team . Multisystem inflammatory syndrome in children in New York state. N Engl J Med. 2020;383(4):347–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kehm RD, Spector LG, Poynter JN, Vock DM, Altekruse SF, Osypuk TL. Does socioeconomic status account for racial and ethnic disparities in childhood cancer survival? Cancer. 2018;124(20):4090–4097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rossen LM, Talih M. Social determinants of disparities in weight among US children and adolescents. Ann Epidemiol. 2014;24(10):705–713.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKay S, Parente V. Health disparities in the hospitalized child. Hosp Pediatr. 2019;9(5):317–325 [DOI] [PubMed] [Google Scholar]
- 23.Mitchell SJ, Bilderback AL, Okelo SO. Racial disparities in asthma morbidity among pediatric patients seeking asthma specialist care. Acad Pediatr. 2016;16(1):64–67 [DOI] [PubMed] [Google Scholar]
- 24.O’Connor MR, Carlin K, Coker T, Zierler B, Pihoker C. Disparities in insulin pump therapy persist in youth with type 1 diabetes despite rising overall pump use rates. J Pediatr Nurs. 2019;44:16–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epstein D, Reibel M, Unger JB, et al. The effect of neighborhood and individual characteristics on pediatric critical illness. J Community Health. 2014;39(4):753–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Didsbury MS, Kim S, Medway MM, et al. Socio-economic status and quality of life in children with chronic disease: a systematic review. J Paediatr Child Health. 2016;52(12):1062–1069 [DOI] [PubMed] [Google Scholar]
- 27.McCrindle BW, Rowley AH, Newburger JW, et al.; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Epidemiology and Prevention . Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. [published correction appears in Circulation. 2019;140(5):e181–e184]. Circulation. 2017;135(17):e927–e999 [DOI] [PubMed] [Google Scholar]
- 28.United States Census Bureau. Population. Available at: https://www.census.gov/topics/population.html. Accessed October 2, 2020
- 29.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106 [DOI] [PubMed] [Google Scholar]
- 30.Agency for Toxic Substances and Disease Registry. CDC social vulnerability index. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Accessed October 2, 2020
- 31.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood). 2020;39(11):1984–1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63(9):817–820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sy KTL, Martinez ME, Rader B, White LF. Socioeconomic disparities in subway use and COVID-19 outcomes in New York City [published online ahead of print December 29, 2020]. Am J Epidemiol. doi:10.1093/aje/kwaa277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng TL, Goodman E; Committee on Pediatric Research . Race, ethnicity, and socioeconomic status in research on child health. Pediatrics. 2015;135(1). Available at: www.pediatrics.org/cgi/content/full/135/1/e225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Otto WR, Geoghegan S, Posch LC, et al. The epidemiology of severe acute respiratory syndrome coronavirus 2 in a pediatric healthcare network in the United States. J Pediatric Infect Dis Soc. 2020;9(5):523–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simons RL, Lei MK, Beach SRH, et al. Discrimination, segregation, and chronic inflammation: testing the weathering explanation for the poor health of Black Americans. Dev Psychol. 2018;54(10):1993–2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care . In: Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press (US); 2003 [PubMed] [Google Scholar]
- 38.Jones BL, Staggs V, Woods-Jaeger B. Chronic stress exposure among young African American children with asthma: racism is a factor. Ann Allergy Asthma Immunol. 2019;123(5):507–508 [DOI] [PubMed] [Google Scholar]
- 39.Xu S, Chen M, Weng J. COVID-19 and Kawasaki disease in children. Pharmacol Res. 2020;159:104951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yung CF, Nadua KD, Oh BK, Thoon KC. Epidemiologic trends in Kawasaki disease during coronavirus disease-19 in Singapore. J Pediatr. 2020;226:314–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gruber CN, Patel RS, Trachtman R, et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). Cell. 2020;183(4):982–995.e14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang CA, Chiang BL. Inflammasomes and childhood autoimmune diseases: a review of current knowledge [published online ahead of print November 25, 2020]. Clin Rev Allergy Immunol. 2020. doi: 10.1007/s12016-020-08825-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.La Torre F, Leonardi L, Giardino G, et al.; Immunology Commission of the Italian Society of Pediatric Allergy, Immunology (SIAIP) . Immunological basis of virus‐host interaction in COVID‐19. Pediatr Allergy Immunol. 2020;31(suppl 26):75–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Onouchi Y. The genetics of Kawasaki disease. Int J Rheum Dis. 2018;21(1):26–30 [DOI] [PubMed] [Google Scholar]
- 45.Fujii F, Egami N, Inoue M, Koga H. Weather condition, air pollutants, and epidemics as factors that potentially influence the development of Kawasaki disease. Sci Total Environ. 2020;741:140469. [DOI] [PubMed] [Google Scholar]
- 46.Buteau S, Belkaibech S, Bilodeau-Bertrand M, Hatzopoulou M, Smargiassi A, Auger N. Association between Kawasaki disease and prenatal exposure to ambient and industrial air pollution: a population-based cohort study. Environ Health Perspect. 2020;128(10):107006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fine MJ, Ibrahim SA, Thomas SB. The role of race and genetics in health disparities research. Am J Public Health. 2005;95(12):2125–2128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351(6273):564–565 [DOI] [PubMed] [Google Scholar]
- 49.Woo B, Kravitz-Wirtz N, Sass V, Crowder K, Teixeira S, Takeuchi DT. Residential segregation and racial/ethnic disparities in ambient air pollution. Race Soc Probl. 2019;11(1):60–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richmond-Bryant J, Mikati I, Benson AF, Luben TJ, Sacks JD. Disparities in distribution of particulate matter emissions from US coal-fired power plants by race and poverty status after accounting for reductions in operations between 2015 and 2017. Am J Public Health. 2020;110(5):655–661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Commonwealth of Massachusetts . Find a COVID-19 Test. Available at: https://www.mass.gov/info-details/find-a-covid-19-test. Accessed March 20, 2021.
- 52.Kreider AR, French B, Aysola J, Saloner B, Noonan KG, Rubin DM. Quality of health insurance coverage and access to care for children in low-income families. JAMA Pediatr. 2016;170(1):43–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lazar M, Davenport L. Barriers to health care access for low income families: a review of literature. J Community Health Nurs. 2018;35(1):28–37 [DOI] [PubMed] [Google Scholar]
- 54.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988-1994). Soc Sci Med. 2008;66(1):72–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zook HG, Kharbanda AB, Flood A, Harmon B, Puumala SE, Payne NR. Racial differences in pediatric emergency department triage scores. J Emerg Med. 2016;50(5):720–727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Payne NR, Puumala SE. Racial disparities in ordering laboratory and radiology tests for pediatric patients in the emergency department. Pediatr Emerg Care. 2013;29(5):598–606 [DOI] [PubMed] [Google Scholar]
- 57.Harrison B, Finkelstein M, Puumala S, Payne NR. The complex association of race and leaving the pediatric emergency department without being seen by a physician. Pediatr Emerg Care. 2012;28(11):1136–1145 [DOI] [PubMed] [Google Scholar]