In a national sample of pediatric ED visits, we studied trends in LOS for mental health visits and characteristics associated with prolonged visits.
Abstract
BACKGROUND AND OBJECTIVES:
Children seeking care in the emergency department (ED) for mental health conditions are at risk for prolonged length of stay (LOS). A more contemporary description of trends and visit characteristics associated with prolonged ED LOS at the national level is lacking in the literature. Our objectives were to (1) compare LOS trends for pediatric mental health versus non–mental health ED visits and (2) explore patient-level characteristics associated with prolonged LOS for mental health ED visits.
METHODS:
We conducted an observational analysis of ED visits among children 6 to 17 years of age using the National Hospital Ambulatory Medical Care Survey (2005–2015). We assessed trends in rates of prolonged LOS and the association between prolonged LOS and demographic and clinical characteristics (race and ethnicity, payer type, and presence of a concurrent physical health diagnosis) using descriptive statistics and survey-weighted logistic regression.
RESULTS:
From 2005 to 2015, rates of prolonged LOS for pediatric mental health ED visits increased over time from 16.3% to 24.6% (LOS >6 hours) and 5.3% to 12.7% (LOS >12 hours), in contrast to non–mental health visits for which LOS remained stable. For mental health visits, Hispanic ethnicity was associated with an almost threefold odds of LOS >12 hours (odds ratio 2.74; 95% confidence interval 1.69–4.44); there was no difference in LOS by payer type.
CONCLUSIONS:
The substantial rise in prolonged LOS for mental health ED visits and disparity for Hispanic children suggest worsening and inequitable access to definitive pediatric mental health care. Policy makers and health systems should work to provide equitable and timely access to pediatric mental health care.
What’s Known on This Subject:
Over time, more children are visiting the emergency department (ED) for mental health conditions and are vulnerable to prolonged length of stay (LOS). National trends in ED LOS and characteristics associated with prolonged LOS have not been well described.
What This Study Adds:
LOS for pediatric mental health ED visits is increasing over time. By 2014 to 2015, on average, 12.7% of visits exceeded 12 hours. Hispanic children are nearly 3 times as likely to have a prolonged visit than non-Hispanic white children.
For the increasing number of children who use the emergency department (ED) for mental health needs,1–12 prolonged ED length of stay (LOS) is a common adverse outcome13–17 that impacts quality, the patient experience, and efficiency of our health care system.18–20 Time spent in the ED represents a delay in accessing definitive mental health care.9,21–23 The ED environment is not well suited to address mental health needs and can be traumatic because of loud noise, frequent changes in providers, and security presence.24 Furthermore, prolonged LOS leads to general ED crowding, rendering other patients at risk for delays, decreased quality of care,9,25–28 and leaving the ED without being seen by a provider.26,29 Acknowledging the impact of prolonged LOS on quality, The Joint Commission defined ED visits >4 hours as prolonged,30 and the National Quality Forum endorsed 2 relevant measures: NQF0495 and NQF0496.31
Previous literature reveals that children who present to the ED with mental health needs are susceptible to prolonged LOS.13–17,22,32–34 Recent changes to the health care landscape, including the 2010 Affordable Care Act,35 coupled with efforts at the state, local, and institutional level, may have impacted access to care over time.11,36–44 Children who are traditionally marginalized as racial and ethnic minorities,9,16,33 living in poverty and/or publicly insured,6,8,15 or who are without a concurrent physical health diagnosis may be particularly vulnerable to prolonged LOS.12,45 More current, nationally representative, pediatric-specific data that describe trends over time and visit characteristics associated with prolonged ED LOS for mental health visits are lacking.
Accordingly, we described more than a decade (2005–2015) of national, temporal trends in ED LOS, comparing pediatric mental health visits with non–mental health visits. Second, we examined whether demographic and clinical characteristics (race and ethnicity, payer type, absence of a concurrent physical health diagnosis) were associated with prolonged ED LOS for mental health visits.
Methods
Study Design and Data Source
We conducted an observational analysis of pediatric ED visits between 2005 and 2015 using the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is a cross-sectional survey of ambulatory and ED visits to US hospitals (excluding federal, military, and Veterans Affairs facilities) administered by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention. The NHAMCS uses 3-stage probability sampling to provide survey-weighted national estimates.46 All NHAMCS data are deidentified and publicly available; this study was exempt from the local institutional review board.
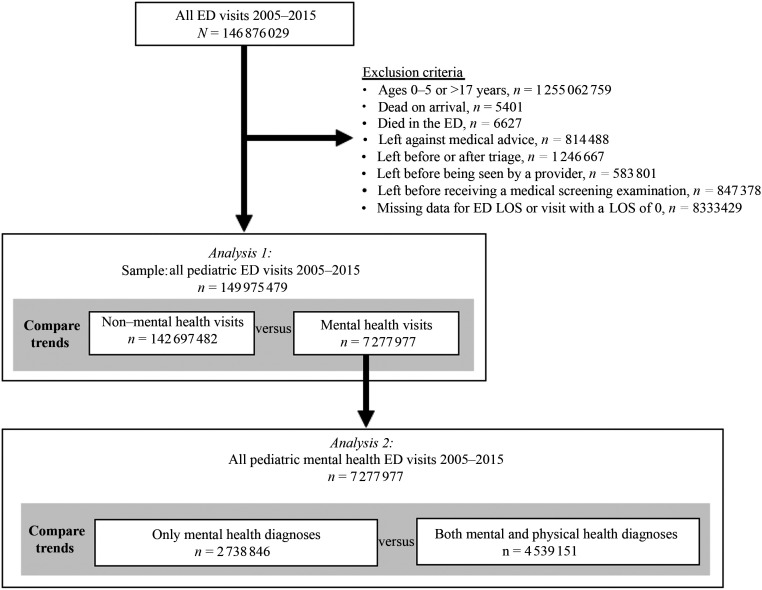
Study Sample
We included ED visits for patients ages 6 to 17 years6,9,47 between 2005 and 2015. We excluded visits with missing ED LOS data and a LOS of 0 minutes (5% of the total ED visits for ages 6–17), visits of patients who were dead on arrival or died in the ED, and visits of patients who left before or after triage, before being seen by a provider, or against medical advice (Fig 1).
FIGURE 1.
Inclusion and exclusion criteria and visit sample used for each analysis.
Variables
We examined 3 definitions of our primary outcome, prolonged ED LOS: >6, >12, and >24 hours. ED LOS >6 hours is a conservative approximation of The Joint Commission definition (>4 hours)30 and consistent with most studies used to examine mental health ED visits.15,16,32–34,48 We explored 2 additional definitions of prolonged ED LOS, >12 and >24 hours, with face validity as being disruptive to patients’ care and experience. We defined prolonged ED LOS by time cutoffs as opposed to mutually exclusive time intervals to optimize our sample size and ensure model stability.
Consistent with previous studies in which researchers use NHAMCS data,8,9,15,17,49–51 we defined an ED visit as a mental health visit if any of the first 3 discharge diagnoses contained a mental health International Classification of Diseases, Ninth Revision diagnosis code, defined by the Child and Adolescent Mental Health Disorder Classification System. The Child and Adolescent Mental Health Disorder Classification System classifies pediatric mental health disorders across International Classification of Diseases coding systems and aligns with the Diagnostic and Statistical Manual of Mental Health Disorders, Fifth Edition and Clinical Classifications Software.52 The full list of diagnostic codes is publicly available on the Children’s Hospital Association Web site.53 We included diagnoses of autism spectrum disorder and developmental delay and injury codes related to suicide attempt and intentional self-harm. We further categorized pediatric mental health ED visits as visits with only mental health diagnoses or visits with both mental and physical health diagnoses.
On the basis of clinical relevance and previous literature, we explored the relationship between prolonged ED LOS and demographic variables: race and ethnicity (NCHS-generated 4-level variable); payer type (private, public, other); and clinical variables: mental health visits with only mental health diagnoses versus mental health visits with both mental and physical health diagnoses.
We reported visits as survey-weighted estimates and rates of prolonged ED LOS as proportions (ED visits with LOS >x hours)/total visits). As recommended by the NCHS, to ensure reliable estimates, we grouped data into 2-year increments and did not report population-level estimates for <30 observations or relative SEs >30%.46
Analysis
Using descriptive statistics, we compared rates and temporal trends (2005–2015) in prolonged LOS between pediatric mental health and non–mental health ED visits. We then used survey-weighted logistic regression, examining the relationship between our 3 prolonged LOS outcomes, mental health versus non–mental health visits, and year. We used an interaction term to assess whether changes over time (by 1-year intervals) differed by mental health versus non–mental health visit. We adjusted for sex, age, payer type, race and ethnicity, and visit occurring during a school month (September to June).
We used survey-weighted logistic regression to examine the relationship between our 3 prolonged LOS outcomes and demographic and clinical visit characteristics. For demographic variables, we prespecified comparisons between Black non-Hispanic, Hispanic, and other race and ethnicity versus white non-Hispanic, as well as public and other payer type versus private payer. For clinical variables, we prespecified comparisons between visits with only mental health diagnoses versus visits with both physical and mental health diagnoses. We adjusted for age, sex, year, and school versus summer month. To statistically test whether trends over time differed between visits with only mental health diagnoses and visits with both physical and mental health diagnoses, we added an interaction term between year and type of mental health visit to the regression model.
Because of sample size constraints, we largely restricted our reported results to ED LOS >6 and >12 hours and limited reported results for ED LOS >24 hours to summary statistics.
To test the robustness of our findings using categorical ED LOS variables, we repeated each analysis using ED LOS as a continuous variable.
ED mental health visits resulting in admission or transfer often have longer LOS.32 To assess whether differences in prolonged LOS might be explained by differences in disposition type, we compared mental health and non–mental health ED visits by disposition type and examined changes in disposition type over time.
All models were examined at the visit level by using survey sampling weights. Analyses were conducted by using R version 3.6.3.
Results
We studied 36 125 records, which, after survey weighting, represent 149 975 479 pediatric ED visits between 2005 and 2015, 7 277 997 (4.9%) of which were mental health visits. Mental health visits had higher rates of prolonged LOS compared with non–mental health ED visits: 21.2% vs 4.8% >6 hours, 7.7% vs 1.2% >12 hours, and 1.9% vs 0.3% >24 hours. On average each year, 12 279 ED visits had an LOS >24 hours. Of mental health visits, 61% were white non-Hispanic, 20% were Black non-Hispanic, and 17% were Hispanic; 46% used a public payer and 35% used private insurance only; 62.4% had both mental health and physical health diagnoses associated with the visit and 37.6% had only mental health diagnoses associated with the visit (Table 1).
TABLE 1.
Characteristics of Pediatric Mental Health and Non–Mental Health Visits by Prolonged ED LOS (2005–2015)
| Mental Health Visits | Non–Mental Health Visits | |||||
|---|---|---|---|---|---|---|
| Total, n | LOS >6, n (%) | LOS >12, n (%) | Total, n | LOS >6, n (%) | LOS >12, n (%) | |
| All visits | 7 277 997 | 1 539 414 | 561 278 | 142 697 482 | 6 793 349 | 1 718 164 |
| Race and ethnicity | ||||||
| White non-Hispanic | 4 427 845 | 866 872 (56.3) | 241 163 (43.0) | 77 358 245 | 3 183 556 (46.9) | 762 815 (44.4) |
| Black non-Hispanic | 1 430 509 | 306 981 (19.9) | N/R | 33 046 369 | 1 686 758 (24.8) | N/R |
| Hispanic | 1 224 556 | 322 639 (21.0) | 199 329 (35.5) | 27 660 569 | 1 744 265 (25.7) | 465 041 (27.1) |
| Other | 195 087 | N/R | N/R | 4 632 299 | N/R | N/R |
| Payer type | ||||||
| Private | 3 340 180 | 752 729 (48.9) | 283 633 (50.5) | 64 752 748 | 2 748 806 (40.5) | 780 518 (45.4) |
| Public | 2 515 057 | 476 346 (30.9) | 119 393 (21.3) | 52 952 825 | 2 518 046 (37.1) | 502 109 (29.2) |
| Other | 1 422 760 | 310 339 (20.2) | N/R | 24 991 909 | 1 526 497 (22.5) | N/R |
| Type of diagnoses | ||||||
| Mental and physical health | 4 539 151 | 949 135 (61.7) | 325 998 (58.1) | N/A | N/A | N/A |
| Mental health only | 2 738 846 | 590 279 (38.3) | 235 280 (41.9) | N/A | N/A | N/A |
| Age, y | ||||||
| 6–12 | 1 695 010 | 271 709 (17.7) | N/R | 78 217 056 | 3 329 969 (49.0) | N/R |
| 13–17 | 5 582 987 | 1 267 705 (82.3) | 461 318 (82.2) | 64 480 426 | 3 463 380 (51.0) | 838 028 (48.8) |
| Sex | ||||||
| Female | 3 779 689 | 806 413 (52.4) | 250 433 (44.6) | 69 791 871 | 3 609 860 (53.1) | 845 648 (49.2) |
| Male | 3 498 308 | 733 001 (47.6) | 310 845 (55.4) | 72 905 611 | 3 183 489 (46.9) | 872 516 (50.8) |
| School month | ||||||
| No | 1 062 387 | 225 124 (14.6) | N/R | 22 420 533 | 1 071 082 (15.8) | N/R |
| Yes | 6 215 610 | 1 314 290 (85.4) | 462 045 (82.3) | 120 276 949 | 5 722 267 (84.2) | 1 410 754 (82.1) |
All results represent weighted estimates. N/A, not applicable to visit sample; N/R, not reportable because of unreliable survey-weighted estimates (<30 unweighted observations or relative SEs >30%).
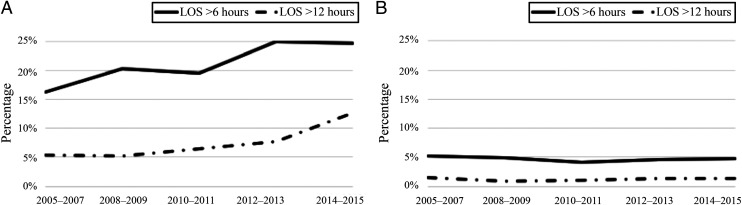
Between 2005 and 2015, rates of prolonged ED LOS remained stable for non–mental health visits but increased for mental health visits. From 2005–2006 to 2014–2015, the average annual rate of ED LOS >6 hours for mental health visits increased from 16.3% to 24.6% (441 542 visits) and from 5.3% (86 791 visits) to 12.7% (227 010 visits) for LOS >12 hours (Fig 2, Supplemental Table 4).
FIGURE 2.
Trends over time in rates of prolonged ED LOS for pediatric mental health and non–mental health visits (2005–2015). All results represent weighted estimates. We were unable to report population-level estimates for visits with prolonged LOS >24 hours because of sample size. A, Mental health ED visits. B, Non–mental health ED visits.
After adjusting for visit characteristics in regression analysis (Table 2), the odds of prolonged LOS were greater for mental health visits compared with non–mental health visits at each LOS outcome: a 3.3-times greater odds of LOS >6 hours (95% confidence interval [CI] 2.2–4.9) and a 2.9-times greater odds of LOS >12 hours (95% CI 1.3–6.2). Additionally, the interaction between mental health visit and year was statistically significant for LOS >6 hours (odds ratio [OR] 1.1; 95% CI 1.0–1.2) and LOS >12 hours (OR 1.15; 95% CI 1.0–1.3) revealing that the relationship between prolonged ED LOS and year differed by type of visit. Stratified models revealed a statistically significant and positive relationship between prolonged ED LOS and year for mental health visits but not for non–mental health visits (Supplemental Table 5).
TABLE 2.
Adjusted ORs of Prolonged ED LOS for Pediatric Mental Health Versus Non–Mental Health Visits and Year of Visit (2005–2015)
| LOS >6 h | LOS >12 h | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | P | aOR | 95% CI | P | |
| Type of ED visit | ||||||
| Non–mental health visit | Reference | Reference | Reference | Reference | Reference | Reference |
| Mental health visit | 3.29 | 2.23–4.88 | <.001 | 2.86 | 1.31–6.24 | .009 |
| Yeara | 0.99 | 0.96–1.02 | .41 | 0.98 | 0.92–1.04 | .53 |
| Mental health visit × year | 1.08 | 1.00–1.16 | .04 | 1.15 | 1.02–1.30 | .03 |
Adjusted for age, sex, payer type, race and ethnicity, and visit during school month. P < .05 is considered statistically significant. aOR, adjusted odds ratio.
Year in 1-year intervals.
Whereas a higher proportion of mental health visits resulted in admission or transfer (27.9%) compared with non–mental health visits (4.4%) (Supplemental Table 6, Supplemental Fig. 3), the distribution of disposition type did not change over time for mental health or non–mental health visits (Supplemental Fig. 4).
Regression analysis (Table 3) revealed that visits for Hispanic compared with white non-Hispanic children had increased odds of LOS >12 hours (OR 2.74; 95% CI 1.7–4.4). There was otherwise no statistically significant difference in prolonged LOS by race and ethnicity or payer type. After adding an interaction term to the model (Supplemental Table 7), there was a statistically significant relationship between LOS >12 hours and the interaction between year and type of mental health visit (OR 1.3; 95% CI 1.1–1.6), revealing that the relationship between prolonged ED LOS and year differed by type of mental health visit. Stratified models revealed a statistically significant and positive relationship between prolonged ED LOS and year for mental health visits with only mental health diagnoses but not for mental health visits with both mental and physical health diagnoses (Supplemental Table 8).
TABLE 3.
Adjusted ORs of Prolonged ED LOS for Pediatric Mental Health Visits by Demographic and Clinical Characteristics (2005–2015)
| LOS >6 h | LOS >12 h | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | P | aOR | 95% CI | P | |
| Race and ethnicity | ||||||
| White non-Hispanic | Reference | Reference | Reference | Reference | Reference | Reference |
| Black non-Hispanic | 1.11 | 0.69–1.79 | .67 | 1.16 | 0.57–2.36 | .68 |
| Hispanic | 1.36 | 0.94–1.97 | .11 | 2.74 | 1.69–4.44 | <.001 |
| Other | 1.19 | 0.53–2.67 | .67 | 2.54 | 0.69–9.31 | .16 |
| Payer type | ||||||
| Private | Reference | Reference | Reference | Reference | Reference | Reference |
| Public | 1.17 | 0.83–1.66 | .37 | 1.42 | 0.80–2.54 | .23 |
| Other | 1.06 | 0.65–1.73 | .82 | 1.74 | 0.78–3.89 | .18 |
| Type of diagnoses | ||||||
| Mental and physical health | Reference | Reference | Reference | Reference | Reference | Reference |
| Mental health only | 0.92 | 0.65–1.28 | .61 | 1.39 | 0.85–2.27 | .19 |
| Age, y | ||||||
| 6–12 | Reference | Reference | Reference | Reference | Reference | Reference |
| 13–17 | 1.59 | 1.09–2.31 | .02 | 1.54 | 0.79–3.02 | .21 |
| Sex | ||||||
| Female | Reference | Reference | Reference | Reference | Reference | Reference |
| Male | 1.03 | 0.75–1.41 | .86 | 1.36 | 0.88–2.10 | .16 |
| School month | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.01 | 0.64–1.60 | .96 | 0.76 | 0.38–1.51 | .43 |
| Yeara | 1.07 | 1.00–1.13 | .04 | 1.12 | 1.01–1.25 | .03 |
P < .05 is considered statistically significant. aOR, adjusted odds ratio.
Year in 1-year intervals.
Repeating regression analyses by using ED LOS as a continuous as opposed to a categorical variable yielded similar results.
Discussion
Over the 11-year study period, the odds of prolonged LOS for mental health ED visits were threefold greater and increased over time compared with non–mental health ED visits, which remained stable. Compared with white non-Hispanic children, Hispanic children had an increased risk of prolonged ED LOS. There was no difference in ED LOS by payer type. Additionally, the odds of prolonged ED LOS for visits with only mental health diagnoses increased over time in comparison with visits with both mental and physical health diagnoses.
This study builds on previous literature suggesting that pediatric mental health ED visits are more vulnerable to prolonged LOS,13–17,22,32–34 as well as recent literature indicating a rise in pediatric mental health ED visits over time, most notably from Kalb et al9 and Lo et al,54 who examine two different nationally representative data sets over the same time period as our study. Our study reveals that this increasing number of children seeking mental health care in the ED are also increasingly vulnerable to prolonged ED LOS. Although a higher percentage of mental health ED visits resulted in admission or transfer compared with non–mental health visits, the proportion of mental health visits resulting in admission or transfer did not change over time and thus cannot explain increasing rates of prolonged ED LOS for these visits. Although the etiology of prolonged ED LOS is likely multifactorial, the increasing rate of prolonged ED LOS over time, especially at the extremes of LOS >12 and >24 hours, likely represents worsening access to essential mental health services across the care continuum, namely, in the ED, inpatient, and outpatient settings. Concurrent with an increasing incidence of mental health conditions, over the past half century, the number of inpatient psychiatric beds has declined without compensatory expansion of outpatient services.55–57 Mental health care for children is expensive, and suboptimal reimbursement limits incentives to expand services.56 There continues to be a dearth of child psychiatrists and community supports.3,58 EDs struggle to safely discharge children who present in crisis to appropriate care settings in light of limited services and poor coverage, which in turn leads to prolonged ED LOS.59
Although limited previous literature explicitly examines the association between ED LOS and race and ethnicity for mental health visits,9,16,33 our study reveals that mental health ED visits for Hispanic patients have an increased odds of prolonged LOS compared with visits for white non-Hispanic patients. Further research should be used to explore etiologies of prolonged ED LOS for the Hispanic population, which likely include structural drivers of poor access to mental health care such as racism,49,51,60–64 language barriers, fear of accessing care, and limited insurance coverage related to immigration status.65,66 Individual institutions should examine their own ED LOS data to ensure equity for all children with mental health needs.
We were interested in the relationship between LOS and payer type, as an indicator of socioeconomic status and comparative access based on insurance. Previous literature reveals inconsistent results.8,15,32 Our study revealed no significant difference in rates of prolonged ED LOS by payer type. Examining the relationship between payer type and ED LOS on a national level is challenging. Approximately 40% of children in the United States are covered by state-run Medicaid programs67; therefore, differences in coverage and reimbursement between private and public insurers vary by state. The Affordable Care Act mandated inclusion of mental health treatment under minimum standards for Medicaid coverage; however, states often define these mandated services differently. In some states, Medicaid might provide more comprehensive coverage for mental health care than private insurers, and in other states, less coverage is provided. Future analysis should be used to examine ED LOS among patients with Medicaid at the state level to understand variation in access.68–70
Previous literature reveals that a concurrent physical health diagnosis impacts use patterns in mental health visits.12,45 We hypothesized that visits with both mental and physical health diagnoses would be associated with decreased rates of prolonged ED LOS because they would include presentations necessitating prompt admission to a medical unit, such as injuries or toxidromes secondary to attempts at self-harm. In contrast, the disposition and LOS for visits with only mental health diagnoses would be dictated by the mental health condition and associated with higher rates of prolonged ED LOS. We found that the rate of prolonged ED LOS for visits with only mental health diagnoses increased over time compared with visits with a concurrent physical health diagnosis, which supports our primary finding: for children requiring definitive access to mental health care, the rate of prolonged ED LOS is increasing over time.
During our study period and more recently, prolonged ED LOS for children with mental health conditions has become increasingly visible among the medical and lay community,71,72 leading to promising changes at the health system and policy level.42,43,47 However, there is still much to be done. Currently, the majority of EDs are not adequately resourced nor have written policies to care for children with mental health conditions.23 Kalb et al9 note that only 16% of children who presented to the ED for a mental health visit are seen by a mental health provider. Every ED should establish protocols, based on existing recommendations and tool kits,73–77 that address pediatric mental health and secure 24-hour access to pediatric-trained mental health providers via in-person consultation or telepsychiatry.78 ED staff should be trained in trauma-informed care, verbal de-escalation, pharmacologic, and when necessary, physical restraint for children. EDs with high volumes of pediatric mental health patients should consider dedicating space within or adjacent to the ED to ensure a therapeutic environment and to help manage throughput.59 Furthermore, quality improvement programs that include root cause analyses and institution-specific interventions have the potential to improve care for children with mental health needs.18,38
Beyond the ED, inadequate access to mental health care for children must also be addressed through changes in state and federal policy.18,36 High-profile court cases, such as in Washington State,37,39 have resulted in significant local policy change and have motivated other states to pursue legislation protective against prolonged LOS.40,79,80 Policy must address the shortage of providers3,4 and expand coverage and reimbursement for the full spectrum of mental health services including inpatient treatment, community-based interventions, and integrated primary care and medical home models to ensure increased and equitable access to care across payer types.44,59,81,82
This study has limitations. First, NHAMCS collects data at the visit as opposed to at the patient level; therefore, we cannot assess the impact of repeat visits. Second, sample size constraints and the quality of discharge diagnosis data limited more granular visit categorization and our ability to determine if a mental health diagnosis was the primary reason for visit or if there was a contributing comorbid condition or noncontributing but significant comorbid condition. Although the NHAMCS is a national database and our sample represents millions of ED visits, the relatively small number of mental health visits limited our ability to report accurate estimates for ED LOS >24 hours, as well as some subanalyses, such as stratification of regression models by disposition type. Because prolonged LOS and admission or transfer are likely related, it is possible that demographic characteristics associated with prolonged LOS actually represent predictors of admission or transfer. Further research should be used to explore characteristics associated with prolonged LOS, specifically for visits resulting in admission or transfer. Finally, the NHAMCS does not provide hospital location data beyond region. State-level data might have provided additional insight into the association between payer type and ED LOS.
Conclusions
Rates of prolonged ED LOS for pediatric mental health visits are increasing over time. Despite national attention to a pediatric mental health epidemic, our study suggests that timely and definitive access to mental health care for children is worsening. By 2014–2015, nearly 450 000 annual ED visits exceeded 6 hours and 227 010 visits exceeded 12 hours. Over the 11-year study period, 135 070 visits exceeded 24 hours. Vulnerability to prolonged ED LOS in mental health visits is not equitable: Hispanic patients have an almost threefold increased odds of prolonged LOS compared with white non-Hispanic patients. We found no difference in ED LOS by payer type; however, aggregate national data can obscure variation and important relationships at the state level. Although future research should be used to further explore drivers of prolonged LOS, we must address this crisis in access to acute mental health care for children through changes in our health care delivery systems, state policy, and federal policy.
Acknowledgment
We dedicate this article in memory of our coauthor Dr Marjorie Rosenthal.
Glossary
- CI
confidence interval
- ED
emergency department
- LOS
length of stay
- NCHS
National Center for Health Statistics
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- OR
odds ratio
Footnotes
Dr Nash conceptualized and designed the study, drafted the initial manuscript, and revised the manuscript; Drs Zima contributed to the conceptualization and design of the study, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript; Mr Rothenberg conducted data analyses and reviewed and revised the manuscript; Drs Moreno, Hoffmann, and Rosenthal contributed to the conceptualization and design of the study and critically reviewed and revised the manuscript; Dr Venkatesh conceptualized and designed the study, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This publication was made possible by the National Clinician Scholars Program and the Clinical and Translational Science Award grant TL1 TR001864 from the National Center for Advancing Translational Science, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH. Dr Venkatesh reports support of the American Board of Emergency Medicine–National Academy of Medicine Anniversary Fellowship and previous support of award KL2 TR001862 from the National Center for Advancing Translational Science, a component of the NIH. The funders/sponsors did not participate in the work. Dr Hoffmann reports support from the US Agency for Healthcare Research and Quality (5K12HS026385-03). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-049843.
References
- 1.Cutler GJ, Rodean J, Zima BT, et al. Trends in pediatric emergency department visits for mental health conditions and disposition by presence of a psychiatric unit. Acad Pediatr. 2019;19(8):948–955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alakeson V, Pande N, Ludwig M. A plan to reduce emergency room ‘boarding’ of psychiatric patients. Health Aff (Millwood). 2010;29(9):1637–1642 [DOI] [PubMed] [Google Scholar]
- 3.McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H. Growth and distribution of child psychiatrists in the United States: 2007–2016. Pediatrics. 2019;144(6):e20191576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cama S, Malowney M, Smith AJB, et al. Availability of outpatient mental health care by pediatricians and child psychiatrists in five U.S. Cities. Int J Health Serv. 2017;47(4):621–635 [DOI] [PubMed] [Google Scholar]
- 5.Torio CM, Encinosa W, Berdahl T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: national estimates of cost, utilization and expenditures for children with mental health conditions. Acad Pediatr. 2015;15(1):19–35 [DOI] [PubMed] [Google Scholar]
- 6.Mahajan P, Alpern ER, Grupp-Phelan J, et al.; Pediatric Emergency Care Applied Research Network (PECARN) . Epidemiology of psychiatric-related visits to emergency departments in a multicenter collaborative research pediatric network. Pediatr Emerg Care. 2009;25(11):715–720 [DOI] [PubMed] [Google Scholar]
- 7.Sun D, Abraham I, Slack M, Skrepnek GH. Emergency department visits in the United States for pediatric depression: estimates of charges and hospitalization. Acad Emerg Med. 2014;21(9):1003–1014 [DOI] [PubMed] [Google Scholar]
- 8.Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Acad Emerg Med. 2014;21(1):25–30 [DOI] [PubMed] [Google Scholar]
- 9.Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4):e20182192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann JA, Stack AM, Samnaliev M, Monuteaux MC, Lee LK. Trends in visits and costs for mental health emergencies in a pediatric emergency department, 2010-2016. Acad Pediatr. 2019;19(4):386–393 [DOI] [PubMed] [Google Scholar]
- 11.Rogers SC, Mulvey CH, Divietro S, Sturm J. Escalating mental health care in pediatric emergency departments. Clin Pediatr (Phila). 2017;56(5):488–491 [DOI] [PubMed] [Google Scholar]
- 12.Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Psychiatric disorders and trends in resource use in pediatric hospitals. Pediatrics. 2016;138(5):e20160909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warren MB, Campbell RL, Nestler DM, et al. Prolonged length of stay in ED psychiatric patients: a multivariable predictive model. Am J Emerg Med. 2016;34(2):133–139 [DOI] [PubMed] [Google Scholar]
- 14.Smith JL, De Nadai AS, Petrila J, Storch EA. Factors associated with length of stay in emergency departments for pediatric patients with psychiatric problems. Pediatr Emerg Care. 2019;35(10):716–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nolan JM, Fee C, Cooper BA, Rankin SH, Blegen MA. Psychiatric boarding incidence, duration, and associated factors in United States emergency departments. J Emerg Nurs. 2015;41(1):57–64 [DOI] [PubMed] [Google Scholar]
- 16.Case SD, Case BG, Olfson M, Linakis JG, Laska EM. Length of stay of pediatric mental health emergency department visits in the United States. J Am Acad Child Adolesc Psychiatry. 2011;50(11):1110–1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santillanes G, Axeen S, Lam CN, Menchine M. National trends in mental health-related emergency department visits by children and adults, 2009-2015. Am J Emerg Med. 2020;38(12):2536–2544 [DOI] [PubMed] [Google Scholar]
- 18.Rabin E, Kocher K, McClelland M, et al. Solutions to emergency department ‘boarding’ and crowding are underused and may need to be legislated. Health Aff (Millwood). 2012;31(8):1757–1766 [DOI] [PubMed] [Google Scholar]
- 19.Bekmezian A, Chung PJ. Boarding admitted children in the emergency department impacts inpatient outcomes. Pediatr Emerg Care. 2012;28(3):236–242 [DOI] [PubMed] [Google Scholar]
- 20.Hostetler MA, Mace S, Brown K, et al.; Subcommittee on Emergency Department Overcrowding and Children, Section of Pediatric Emergency Medicine, American College of Emergency Physicians . Emergency department overcrowding and children. Pediatr Emerg Care. 2007;23(7):507–515 [DOI] [PubMed] [Google Scholar]
- 21.Claudius I, Donofrio JJ, Lam CN, Santillanes G. Impact of boarding pediatric psychiatric patients on a medical ward. Hosp Pediatr. 2014;4(3):125–132 [DOI] [PubMed] [Google Scholar]
- 22.O’Donnell EP, Yanek L, Reynolds E, Manning Ryan L, Ngo TL. Characteristics of mental health patients boarding for longer than 24 hours in a pediatric emergency department. JAMA Pediatr. 2020;174(12):1206–1208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gausche-Hill M, Ely M, Schmuhl P, et al. A national assessment of pediatric readiness of emergency departments. JAMA Pediatr. 2015;169(6):527–534 [DOI] [PubMed] [Google Scholar]
- 24.Worsley D, Barrios E, Shuter M, Pettit AR, Doupnik SK. Adolescents’ experiences during “boarding” hospitalization while awaiting inpatient psychiatric treatment following suicidal ideation or suicide attempt. Hosp Pediatr. 2019;9(11):827–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Depinet HE, Iyer SB, Hornung R, Timm NL, Byczkowski TL. The effect of emergency department crowding on reassessment of children with critically abnormal vital signs. Acad Emerg Med. 2014;21(10):1116–1120 [DOI] [PubMed] [Google Scholar]
- 26.Timm NL, Ho ML, Luria JW. Pediatric emergency department overcrowding and impact on patient flow outcomes. Acad Emerg Med. 2008;15(9):832–837 [DOI] [PubMed] [Google Scholar]
- 27.Kennebeck SS, Timm NL, Kurowski EM, Byczkowski TL, Reeves SD. The association of emergency department crowding and time to antibiotics in febrile neonates. Acad Emerg Med. 2011;18(12):1380–1385 [DOI] [PubMed] [Google Scholar]
- 28.Nash KA, Kimia A, Fleegler EW, Guedj R. Equitable and timely care of febrile neonates: a cross-sectional study [published online ahead of print February 1, 2020]. Pediatr Emerg Care. 2020. doi: 10.1097/PEC.0000000000002034 [DOI] [PubMed] [Google Scholar]
- 29.Conrad HB, Hollenbach KA, Gehlbach DL, Ferran KL, Barham TA, Carstairs KL. The impact of behavioral health patients on a pediatric emergency department’s length of stay and left without being seen. Pediatr Emerg Care. 2018;34(8):584–587 [DOI] [PubMed] [Google Scholar]
- 30.The Joint Commission . The “patient flow standard” and the 4-hour recommendation. Jt Comm Perspect. 2013;33(6):1, 3–4 [PubMed] [Google Scholar]
- 31.National Quality Forum. National Voluntary Consensus Standards for Emergency Care: A Consensus Report. Washington, DC: National Quality Forum; 2009 [Google Scholar]
- 32.Hoffmann JA, Stack AM, Monuteaux MC, Levin R, Lee LK. Factors associated with boarding and length of stay for pediatric mental health emergency visits. Am J Emerg Med. 2019;37(10):1829–1835 [DOI] [PubMed] [Google Scholar]
- 33.Chakravarthy B, Yang A, Ogbu U, et al. Determinants of pediatric psychiatry length of stay in 2 urban emergency departments. Pediatr Emerg Care. 2017;33(9):613–619 [DOI] [PubMed] [Google Scholar]
- 34.Misek RK, DeBarba AE, Brill A. Predictors of psychiatric boarding in the emergency department. West J Emerg Med. 2015;16(1):71–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Assistant Secretary for Public Affairs; US Department of Health and Human Services. Parity policy and implementation. 2020. Available at: https://www.hhs.gov/about/agencies/advisory-committees/mental-health-parity/task-force/resources/index.html. Accessed April 28, 2020
- 36.So M, McCord RF, Kaminski JW. Policy levers to promote access to and utilization of Children’s mental health services: a systematic review. Adm Policy Ment Health. 2019;46(3):334–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Appelbaum PS. “Boarding” psychiatric patients in emergency rooms: one court says “No more”. Psychiatr Serv. 2015;66(7):668–670 [DOI] [PubMed] [Google Scholar]
- 38.Bardach NS, Burkhart Q, Richardson LP, et al. Hospital-based quality measures for pediatric mental health care. Pediatrics. 2018;141(6):e20173554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bloom JD. Psychiatric boarding in Washington state and the inadequacy of mental health resources. J Am Acad Psychiatry Law. 2015;43(2):218–222 [PubMed] [Google Scholar]
- 40.Flowers LM, Maass KT, Melin GJ, et al. Consequences of the 48-h rule: a lens into the psychiatric patient flow through an emergency department. Am J Emerg Med. 2018;36(11):2029–2034 [DOI] [PubMed] [Google Scholar]
- 41.Uspal NG, Rutman LE, Kodish I, Moore A, Migita RT. Use of a dedicated, non-physician-led mental health team to reduce pediatric emergency department lengths of stay. Acad Emerg Med. 2016;23(4):440–447 [DOI] [PubMed] [Google Scholar]
- 42.Rogers SC, Griffin LC, Masso PD Jr., Stevens M, Mangini L, Smith SR Sr.. CARES: improving the care and disposition of psychiatric patients in the pediatric emergency department. Pediatr Emerg Care. 2015;31(3):173–177 [DOI] [PubMed] [Google Scholar]
- 43.Stricker FR, O’Neill KB, Merson J, Feuer V. Maintaining safety and improving the care of pediatric behavioral health patients in the emergency department. Child Adolesc Psychiatr Clin N Am. 2018;27(3):427–439 [DOI] [PubMed] [Google Scholar]
- 44.Belkin G, McCray C. ThriveNYC: delivering on mental health. Am J Public Health. 2019;109(S3):S156–S163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doupnik SK, Rodean J, Feinstein J, et al. Health care utilization and spending for children with mental health conditions in Medicaid. Acad Pediatr. 2020;20(5):678–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Center for Health Statistics; Centers for Disease Control and Prevention. NHAMCS micro-data file documentation. 2015. Available at: https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm. Accessed March 1, 2020
- 47.Holder SM, Rogers K, Peterson E, Shoenleben R, Blackhurst D. The impact of mental health services in a pediatric emergency department: the implications of having trained psychiatric professionals. Pediatr Emerg Care. 2017;33(5):311–314 [DOI] [PubMed] [Google Scholar]
- 48.Pines JM, Russell Localio A, Hollander JE. Racial disparities in emergency department length of stay for admitted patients in the United States. Acad Emerg Med. 2009;16(5):403–410 [DOI] [PubMed] [Google Scholar]
- 49.Kunen S, Prejean C, Gladney B, Harper D, Mandry CV. Disposition of emergency department patients with psychiatric comorbidity: results from the 2004 National Hospital Ambulatory Medical Care Survey. Emerg Med J. 2006;23(4):274–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Opoku ST, Apenteng BA, Akowuah EA, Bhuyan S. Disparities in emergency department wait time among patients with mental health and substance-related disorders. J Behav Health Serv Res. 2018;45(2):204–218 [DOI] [PubMed] [Google Scholar]
- 51.Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv. 2005;56(6):671–677 [DOI] [PubMed] [Google Scholar]
- 52.Zima BT, Gay JC, Rodean J, et al. Classification System for International Classification of Diseases, Ninth Revision, Clinical Modification and Tenth Revision pediatric mental health disorders. JAMA Pediatr. 2020;174(6):620–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Children’s Hospital Association. Mental health disorder codes: Child and Adolescent Mental Health Disorders Classification System (CAMHD-CS). 2019. Available at: https://www.childrenshospitals.org/Research-and-Data/Pediatric-Data-and-Trends/2019/Mental-Health-Disorder-Codes. Accessed January 20, 2020
- 54.Lo CB, Bridge JA, Shi J, Ludwig L, Stanley RM. Children’s mental health emergency department visits: 2007–2016. Pediatrics. 2020;145(6):e20191536. [DOI] [PubMed] [Google Scholar]
- 55.Stone A, Rogers D, Kruckenberg S, Lieser A. Impact of the mental healthcare delivery system on California emergency departments. West J Emerg Med. 2012;13(1):51–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geller JL, Biebel K. The premature demise of public child and adolescent inpatient psychiatric beds: part II: challenges and implications. Psychiatr Q. 2006;77(4):273–291 [DOI] [PubMed] [Google Scholar]
- 57.Geller JL, Biebel K. The premature demise of public child and adolescent inpatient psychiatric beds: part I: overview and current conditions. Psychiatr Q. 2006;77(3):251–271 [DOI] [PubMed] [Google Scholar]
- 58.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. 2009;60(10):1323–1328 [DOI] [PubMed] [Google Scholar]
- 59.Nordstrom K, Berlin JS, Nash SS, Shah SB, Schmelzer NA, Worley LLM. Boarding of mentally ill patients in emergency departments: American psychiatric association resource document. West J Emerg Med. 2019;20(5):690–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Trent M, Dooley DG, Dougé J; Section on Adolescent Health; Council on Community Pediatrics; Committee on Adolescence . The impact of racism on child and adolescent health. Pediatrics. 2019;144(2):e20191765. [DOI] [PubMed] [Google Scholar]
- 61.Coker TR, Elliott MN, Kataoka S, et al. Racial/Ethnic disparities in the mental health care utilization of fifth grade children. Acad Pediatr. 2009;9(2):89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marrast L, Himmelstein DU, Woolhandler S. Racial and ethnic disparities in mental health care for children and young adults: a national study. Int J Health Serv. 2016;46(4):810–824 [DOI] [PubMed] [Google Scholar]
- 63.Park CY, Lee MA, Epstein AJ. Variation in emergency department wait times for children by race/ethnicity and payment source. Health Serv Res. 2009;44(6):2022–2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3). Available at: www.pediatrics.org/cgi/content/full/115/3/e310 [DOI] [PubMed] [Google Scholar]
- 65.Lê Cook B, Brown JD, Loder S, Wissow L. Acculturation differences in communicating information about child mental health between Latino parents and primary care providers. J Immigr Minor Health. 2014;16(6):1093–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Caballero TM, DeCamp LR, Platt RE, et al. Addressing the mental health needs of latino children in immigrant families. Clin Pediatr (Phila). 2017;56(7):648–658 [DOI] [PubMed] [Google Scholar]
- 67.Rudowitz R, Garfield R, Hinton E. 10 things to know about Medicaid: setting the facts straight. 2019. Available at: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-setting-the-facts-straight/?gclid=CjwKCAiA-_L9BRBQEiwA-bm5fhfVUy8dvsYZjOWjglEf_odxvXJoVemK0IkhvN5dDJD0XTcNsP7FyBoCpKgQAvD_BwE. Accessed November 23, 2020
- 68.US Centers for Medicare & Medicaid Services. The Mental Health Parity and Addiction Equity Act (MHPAEA). 2020. Available at: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/mhpaea_factsheet. Accessed July 3, 2020
- 69.Huskamp HA, Samples H, Hadland SE, et al. Mental health spending and intensity of service use among individuals with diagnoses of eating disorders following federal parity. Psychiatr Serv. 2018;69(2):217–223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moore H, Astor RA, Benbenishty R. Role of school-climate in school-based violence among homeless and nonhomeless students: individual- and school-level analysis. Child Abuse Negl. 2020;102:104378. [DOI] [PubMed] [Google Scholar]
- 71.Boston Globe Spotlight Team . The desperate and the dead: families in fear. The Boston Globe. June 23, 2016. Available at: https://apps.bostonglobe.com/spotlight/the-desperate-and-the-dead/series/families/. Accessed August 30, 2020
- 72.Ramer H. Amid litigation, milestone hit in ER boarding crisis. Associated Press. April 2, 2020. Available at: https://apnews.com/article/2a71829f81b346717a167609f7326bbc. Accessed August 30, 2020
- 73.Chun TH, Mace SE, Katz ER; American Academy of Pediatrics; Committee on Pediatric Emergency Medicine, and American College of Emergency Physicians; Pediatric Emergency Medicine Committee . Evaluation and management of children and adolescents with acute mental health or behavioral problems. Part I: common clinical challenges of patients with mental health and/or behavioral emergencies. Pediatrics. 2016;138(3):e20161570. [DOI] [PubMed] [Google Scholar]
- 74.Dolan MA, Mace SE; American Academy of Pediatrics, Committee on Pediatric Emergency Medicine; American College of Emergency Physicians and Pediatric Emergency Medicine Committee . Pediatric mental health emergencies in the emergency medical services system. Pediatrics. 2006;118(4):1764–1767 [DOI] [PubMed] [Google Scholar]
- 75.Dolan MA, Mace SE; American Academy of Pediatrics; American College of Emergency Physicians . Pediatric mental health emergencies in the emergency department. Ann Emerg Med. 2006;48(4):484–486 [DOI] [PubMed] [Google Scholar]
- 76.Massachusetts College of Emergency Physicians . Practical solutions to boarding of psychiatric patients in the emergency department. 2015. Massachusetts College of Emergency Physicians. Available at: https://www.macep.org/Files/Behavioral%20Health%20Boarding/Practical%20Solutions%20to%20Boarding%20of%20Psych%20Patients%20in%20EDs.pdf. Accessed August 30, 2020
- 77.US Department of Health and Human Services; Health and Resources and Services Administration; Maternal Child Health Bureau . Critical Crossroads: Pediatric Mental Health Care in the Emergency Department: A Care Pathway Resource Toolkit. Rockville, Maryland: US Department of Health and Human Services; 2019 [Google Scholar]
- 78.Roberts N, Hu T, Axas N, Repetti L. Child and adolescent emergency and urgent mental health delivery through telepsychiatry: 12-month prospective study. Telemed J E Health. 2017;23(10):842–846 [DOI] [PubMed] [Google Scholar]
- 79.McClure JA. Psychiatric boarding in New Hampshire: violation of a statutory right to treatment. University of New Hampshire Law Review. 2016;14(1)
- 80.Massachusetts Department of Mental Health, Division of Insurance . Bulletin 2019-01: Prevention of emergency department boarding of patients with acute behavioral health and/or substance use disorder emergencies. Available at: https://www.mass.gov/regulatory-bulletin/bulletin-2018-01-prevention-of-emergency-department-boarding-of-patients-with. Accessed August 30, 2020
- 81.Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health . Policy statement–The future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421 [DOI] [PubMed] [Google Scholar]
- 82.Ader J, Stille CJ, Keller D, Miller BF, Barr MS, Perrin JM. The medical home and integrated behavioral health: advancing the policy agenda. Pediatrics. 2015;135(5):909–917 [DOI] [PubMed] [Google Scholar]