This feature is coordinated by Stuart Abramson, MD, Giselle Mosnaim, MD, and Andrew Murphy, MD, from the American Academy of Allergy, Asthma & Immunology Federation of Regional, State, and Local Allergy, Asthma, and Immunology Societies Assembly and by Editorial Board member Matthew Rank, MD.
Practice Challenge
The 2019 viral pandemic of SARS-CoV-2 has led to enhanced respiratory precautions because of its high infectivity.1 Aerosol-generating procedures such as pulmonary function tests (PFTs) pose an increased risk for viral transmission and therefore require adaptation by clinical personnel.
Practice Solution
We converted an existing outpatient PFT laboratory into a negative pressure room through a mobile unit. This unit employs a centrifugal fan, using inertia (centrifugal force) and Bernoulli's principle so that air is sucked into the impeller's (fan) center and accelerated radially.2 The surface area for airflow widens, reducing velocity and converting dynamic pressure into static pressure before exiting. A high-efficiency particulate air filter and ultraviolet C lamp should be paired with the fan for air sanitization. Negative pressure rooms require a sealed and enclosed space in which the inside pressure is less than the outside pressure by 2.5 Pascals.
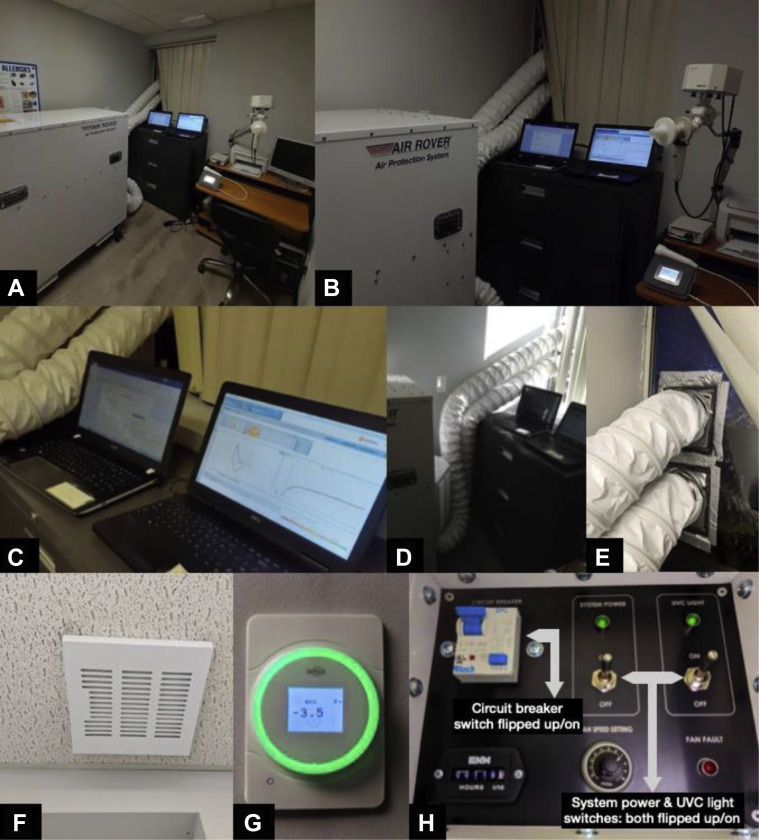
We installed a mobile Air Rover APS2000 (Air Rover, Inc., Tyler, Texas) negative pressure machine. Electricians converted an outlet to 1200 W 25 A. The window was replaced with polycarbonate with two 6-inch ventilation outlets. C-clamps connected military-grade 6-inch vinyl exhaust tubes between the unit and window. One-way dryer vent flapper covers were installed. The HVAC vent was taped shut with duct tape and an Elima-Draft (East Setauket, NY) pollen filter cover was placed over the original vent. A Setra Lite (Boxborough, Mass) pressure monitor was installed (Figure 1 ). Other measures entailed an ultraviolet C bulb in the furnace and pollen filter covers over each HVAC register. Environmental Science Consultants (Ronkonkoma, NY) is an industrial hygienist company that certified the negative pressure room as a permanent solution according to American Society of Heating, Refrigerating, and Air-Conditioning Engineers standards.
Figure 1.
Pictorial view of pulmonary function test (PFT) laboratory. (A) Overview of PFT laboratory. (B) Laptops connect to PFT machine (top right) and exhaled nitric oxide device (lower right). (C) Pulmonary function test volume loops. (D) Air Rover with military-grade exhaust tubes. (E) Military-grade tubes connect through vents to release the filtered air. (F) Elima-Draft pollen filter cover. (G) Pressure meter for PFT laboratory. (H) Air Rover control panel (the potentiometer/fan speed setting is 7).
The cost, $13,611.11, plus 3 hours of labor at $200/h, equals approximately $14,211.11. There was no interruption in other clinical services. Before COVID-19, we performed up to 4 PFTs/h; after COVID-19 we are currently performing up to 2/h with the negative pressure room and enhanced protection protocols (Table I ). These protocols include obtaining a negative COVID-19 polymerase chain reaction nasal swab within 7 days of performing the PFT; using a contactless infrared thermometer to verify the lack of fever; using the Centers for Disease Control and Prevention COVID-19 screening tool paper form; confirming that patients are wearing vent-less masks covering the nose and mouth; having patients use hand sanitizer; cleaning the room with 75% alcohol-based wipes and waiting 5 minutes, based on the negative pressure machine capabilities and the size of the room; and outfitting staff with N95 respirators covered by surgical masks and a face shield, using gowns and gloves. No staff or patients were given the diagnosis of COVID-19 attributable after installing the negative pressure room.
Table I.
Investment versus compensation
| Item | Cost |
|---|---|
| Investment | |
| Air protection system, 2000 ft3/min, 3000 W (1500 ft3/min exhaust, three 5-ft-long ultraviolet C lights, 12-in-high-efficiency particulate air filter) | $9,999.00 |
| Transformer kit, used to convert to 115 V | $713.06 |
| Shipping estimate | $650.00 |
| Freight | $350.00 |
| Splice collar, tape, clamp, aluminum duct | $57.88 |
| LEXAN window | $145.56 |
| Tri-volt transformer | $33.52 |
| Electrical service, two-wire shock | $200.96 |
| Service installation: outlet with circuit | $285.00 |
| Setra Lite pressure monitor (24-V transformer AC/DC, 1900 box, old work 14-in3 gang box) | $405.13 |
| Installation labor costs | $600.00 |
| Military-grade tubes | $771.00 |
| Fixed investment total | $14,211.11 |
The change from 4 PFTs/h to 2 PFTs/h is not directly related to converting the PFT laboratory to a negative airflow environment, but rather to the other enhanced protection protocols outlined earlier.
Project limitations included differential shipping costs and reimbursement.
Installing a negative pressure room in the COVID-19 era is practical, medically necessary, and economically feasible.
Key Pearls
-
1.
This Practice Pearl provides guidance for those who want to undertake this approach based on our experience.
-
2.
This type of negative pressure PFT laboratory is not meant to be a standard of practice or a viable option for everyone.
-
3.
Its effectiveness and necessity in addition to the other precautions have not been proven (which would be beyond the scope of a Practice Pearl).
Acknowledgments
We would like to thank our patients and the health care team at Three Village Allergy and Asthma, PLLC, for their continued hard work and support. T.C. Olsen, S.L. Koo, R.A. Promisloff, and A.M. Szema conceived or designed the study, acquired and analyzed the data, drafted the initial report, critically revised the manuscript, and provided final approval of the manuscript version to be published.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The content is solely the authors' responsibility and does not necessarily represent the official views of the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell or Drexel University College of Medicine.
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
References
- 1.Sungnak W., Huang N., Bécavin C., Berg M., Queen R., Litvinukova M. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li H. Fluid flow analysis of a single-stage centrifugal fan with a ported diffuser. Eng Appl Comput Fluid Mech. 2009;3:147–163. [Google Scholar]