Abstract
The prevalence of obesity is increasing and progressively influencing physician-patient interactions. While there is a sizable amount of data demonstrating that obesity is a state of low-grade inflammation, to our knowledge, there is no single review summarizing its effects on hematologic parameters and thrombotic risk. We performed a literature search which largely surfaced observational studies, with a few systematic reviews and meta-analyses of these studies. We took care to review the mechanisms driving an inflammatory state and obesity’s effect on white blood cells, red blood cells, platelets and thrombotic risk. There is an observed relative, and sometimes absolute leukocytosis driven by this inflammatory state. Obesity is also associated with increased platelet counts and an increased risk for venous thromboembolism (VTE). Lastly, the association between obesity, iron deficiency (ID) and red blood cell counts may be present but remains uncertain. Recognizing the above associations may provide clinicians with reassurance regarding otherwise unexplained hematologic abnormalities in obese individuals. We hope this review will prompt future studies to further understand the underlying mechanisms driving these abnormalities and identify modifiable risk factors and potential therapeutic targets to prevent the development of probable obesity-associated conditions with significant morbidity and mortality, such as ID and VTE.
Keywords: leukocytosis, anemia, iron deficiency, thrombocytosis, venous thromboembolism
Introduction
The pervasiveness of obesity in the United States has been dramatically increasing over the last several decades and shows no signs of slowing. In 2015–2016 the prevalence of obesity in the US population was 39.8%, accounting for about 93.3 million US adults1, with new data predicting that by 2030 nearly 1 in 2 adults will be obese2. As our patient interactions become progressively influenced by the health effects of obesity, it is becoming increasingly important to understand the consequences of the hematologic alterations observed in these individuals.
Obesity has been associated with a state of low-grade systemic inflammation characterized by an adipose tissue driven acute phase response, with interleukin (IL)-6, IL-1, IL-8 and tumor necrosis factor (TNF)-α playing the largest role and resulting in subsequent elevations of acute phase proteins such as c-reactive protein (CRP). This produces an environment defined by inflammation, with theoretical and established down-stream effects. This review will summarize our current understanding of this pro-inflammatory state and its alteration of hematologic parameters, particularly with regards to white blood cell, red blood cell and platelet counts and perturbances to thrombosis.
The pro-inflammatory state of obesity
Macrophages and adipose tissue
There is ample evidence that adipose tissue is a primary source of inflammatory mediators3,4. White adipose tissue is the most abundant type of adipose tissue and is composed of many cell types. Adipocytes are the most plentiful, but adipose tissue macrophages are also present, with a relative population size that correlates with the level of adiposity5. Adipose tissue macrophages are estimated to comprise up to 40% of the cells in obese adipose tissue, compared to under 10% in lean individuals6, and elevated macrophage infiltration is noted in visceral compared to subcutaneous fat7. Although it has been reported that preadipocytes can function as macrophage-like cells8, adipose tissue macrophages are most likely bone marrow-derived circulating monocytes that subsequently infiltrated adipose tissue6. Leptin and other chemokines such as monocyte chemotactic protein-1 and leukotriene B49 contribute to this, and increasing concentrations of recombinant human leptin have been shown to result in an increased adhesion and transmigration of blood monocytes in a concentration-dependent manner5, though all factors attracting immune cells into obese tissues are not yet fully understood. See Boutens et al. (2016)10 for a full review of adipose tissue macrophages in obesity.
Adipose tissue and the acute phase response
The acute phase response that accompanies inflammatory states is characterized by increased production of acute phase proteins, largely released by hepatocytes. The role of these acute phase proteins varies from mediating inflammation, to inhibiting proteases, to scavenging free radicals. IL-6 is a principle regulator for most positive acute phase proteins and stimulates the production of serum amyloid A, c-reactive protein, α1-acid glycoprotein, α1-antichymotrypsin, haptoglobin, α1-antitrypsin, fibrinogen, complement component C3 and caeruloplasmin11. Human adipose tissue can independently produce and release cytokines that are known to be major inducers of the acute phase response, including IL-6, IL-1, IL-8 and TNF-α12. Both adipocytes and macrophages contribute to cytokine production, though there is some evidence that macrophages are the major source of white adipose tissue-derived IL-6 and TNF-α6. Cottam et al. (2004)13 comprehensively summarized all acute phase reactants and inflammatory mediators observed in obesity.
IL-6 and TNF-α are the most evidently increased in the serum and white adipose tissue of obese individuals14–21, and Mohamed-Ali et al. (1997)22 calculated that the whole body adipose tissue mass is responsible for the production of 15–35% of systemic IL-6. IL-6 and TNF-α levels are also noted to decrease with weight loss23–28, particularly secondary to bariatric surgery29–31. Local adipose tissue IL-6 production is also noted to be greater in subjects with a higher waist-to-hip ratio17,19,22. A higher waist-to-hip ratio often indicates increased visceral adipose tissue, which has been shown to have elevated inflammatory status, compared to subcutaneous adipose tissue10. This supports the observation that omental adipose tissue has been shown to release 2–3 times more IL-6 than its subcutaneous counterpart32,33. As IL-6 regulates CRP production, it is not surprising that CRP elevation significantly corresponds to the level of adiposity present in the body17,19,21,23,34–36 and also decreases with weight loss24–26,37,38; this association has been shown to be stronger in women compared to men35. There is even some evidence that CRP is produced by the adipose tissue itself39.
Conclusion
In summary, in obesity, leptin and other chemokines contribute to the transmigration of bone marrow-derived monocytes into adipose tissue, with a resultant elevation of IL-6, TNF-α and other cytokines. This subsequently results in the rise in acute phase proteins, such as CRP, and all of this in combination accounts for the resultant chronic low-grade inflammation which actively contributes to alterations in hematologic parameters and alter the risk of thrombosis, as discussed below. While there may be a cycle at play in which bone marrow-derived monocytes are likely not only the source but also the target of pro-inflammatory signals, this is not clear from the current literature. This is something that should be further researched as it could identify additional potential therapeutic targets upstream of the acute phase response.
Obesity and white blood cell count
Obesity and leukocytosis
A significant number of patients referred for investigation of unexplained leukocytosis have no identifiable cause of a persistent and stable leukocytosis, other than their being obese. Multiple studies have worked to elucidate the connection between leukocytosis and body mass index (BMI). We discuss these studies below, as well as the hypothesized mechanisms driving this observation.
Herishanu et al. (2006)12 analyzed patients (n = 327) referred to their outpatient hematology clinic for persistent leukocytosis and found that 15% were asymptomatic, obese, mostly middle-aged females with a mild leukocytosis (mean white blood cell count 13.05 ± 1.44 · 109/L) characterized mostly by neutrophilia without bandemia and accompanied by elevated acute-phase reactants (CRP and erythrocyte sedimentation rate). No other recognized cause for the leukocytosis (e.g. infection, inflammation, smoking, malignancy, etc.) was identified, and the elevated count persisted through a mean follow-up of 45 months. In three individuals, reduction in weight was accompanied by a gradual reduction and normalization of the white blood cell count and accompanying CRP levels. To further validate this association, they performed a cross-sectional analysis of non-smoking individuals without underlying inflammatory or infectious conditions and showed that subjects found to have a leukocytosis (n = 62) had a higher BMI when compared to the population with normal white blood count ranges. Raghavan et al. (2016)40 similarly noted that white blood counts are relatively high in obese women, meaning that while mean values for total leukocyte count did not exceed accepted physiological range, there was a relative leukocytosis between categories, with a progressive numerical increase in the values of the total leukocyte count as the BMI increased. Additionally, absolute neutrophil count and differential neutrophil count showed a progressive increase with increase in BMI. The absolute lymphocyte counts likewise showed statistically significant differences between the control group and obese group, but the strength of the association appeared to be less than that observed with absolute neutrophil count. Of note, the differential lymphocyte count displayed a progressive decrease with increase in BMI, suggesting that the increase in absolute lymphocyte counts was counterbalanced by a respectively greater increase in neutrophils. Although traditionally neutrophils have been acknowledged as key players in acute inflammation, their contribution to chronic inflammation is recently being appreciated, particularly in conditions such as chronic obstructive pulmonary disease, arthritis, neurodegenerative disease and cardiovascular inflammation41. Given this, the myeloid skewing observed in obesity is unsurprising. Additionally, evidence from animal models shows that high fat diets lead to myeloid hyperplasia, especially of the granulocytic compartment42. Their findings are summarized in Table 1, adapted from their paper. Several other studies support the positive correlation between leukocyte count and BMI21,36,43–45.
Table 1:
A summary of the mean of particularly interesting variables, across BMI categories; adapted from Raghavan et al. (2016) Table/Fig-2. Met. Syndrome = metabolic syndrome; BMI = body mass index (kg/m2); WC = waist circumference (cm); TLC = total leukocyte count (/mm3); ANC = absolute neutrophil count (/mm3); ALC = absolute lymphocyte count (/mm3); PLT = platelet count (x109/L).
| Control BMI ≤24.9 Mean ± SD |
Overweight BMI ≥25 – ≤ 29.9 Mean ± SD |
Obese BMI ≥30 Mean ± SD |
Met. Syndrome BMI ≥30 Mean ± SD |
|
|---|---|---|---|---|
| Age | 42.41±13.22 | 44.77±10.41 | 45.95±11.00 | 52.29±10.30 |
| BMI | 22.15±2.76 | 27.02±1.44 | 34.29±3.50 | 34.77±4.44 |
| WC | 74.82±6.44 | 83.92±4.79 | 98.53±9.53 | 101.7±10.14 |
| TLC | 6590±1608 | 7405±1711 | 8759±1882 | 10110±1947 |
| ANC | 3706±1315 | 4268±1269 | 5310±1471 | 6148±1499 |
| ALC | 2203±527 | 2340±583 | 2554±613 | 2916±786 |
| PLT | 265.4±50.02 | 279.7±70.34 | 307.8±87.01 | 320.1±66.73 |
The role of cytokines and adipokines
Peripheral blood leukocytosis is a hallmark of inflammation and in obesity is likely driven by the chronic low-grade inflammatory state discussed in detail above. Pro-inflammatory cytokines such as IL-6 and IL-8 are important inducers of leukocytosis, particularly neutrophilia, through multiple mechanisms including demargination of intravascular neutrophils, acceleration of bone marrow neutrophil release and enhancement of bone marrow granulopoiesis46–50.
Adipokines such as leptin may also be playing a role. Wilson et al. (1997)51 showed a positive, though indirect, correlation between white blood cell count and fasting plasma leptin concentrations in obese Pima Indians. Laharrague et al. (2000)52 developed a homologous system where purified CD34+ progenitors from adult human bone marrow were treated with recombinant human leptin. They found that leptin (at high levels, but levels which are observed in obesity) significantly stimulated the appearance of granulocyte-macrophage colonies, the precursor for monocytes and granulocytes (Figure 1), and that plasma leptin concentration was significantly correlated with leukocyte count in overweight and obese subjects. They also found that leptin concentrations were significantly higher in women than men, a difference which persisted even after controlling for BMI. Furthermore, human and mouse hematopoietic stem cells have been shown to express the leptin receptor53 and a murine model has shown that treatment with a synthetic fragment of leptin resulted in a two-fold increase in the number of hematopoietic stem cells with an associated increase in the number of granulocyte/macrophage colony-forming units produced by bone marrow cells54. Leptin clearly has a role in regulation of hematopoiesis through a mechanism that is multifactorial and indirect. Zhou et al. (2014)55 have shown that bone marrow mesenchymal stromal cells are leptin receptor positive and although these are defined as non-hematopoietic, as they rather differentiate into osteogenic, chondrogenic, and adipogenic progeny, they do give rise to bony ossicles that become invested with hematopoietic bone marrow as well as directly expressing hematopoietic stem cells niche factors such as stem cell factor and Cxcl12, suggesting they contribute to the organization of a hematopoietic microenvironment as important components of the hematopoietic stem cells niche. For an excellent review on the hematopoietic stem cells niche, see Sugiyama et al. (2018)56.
Figure 1:
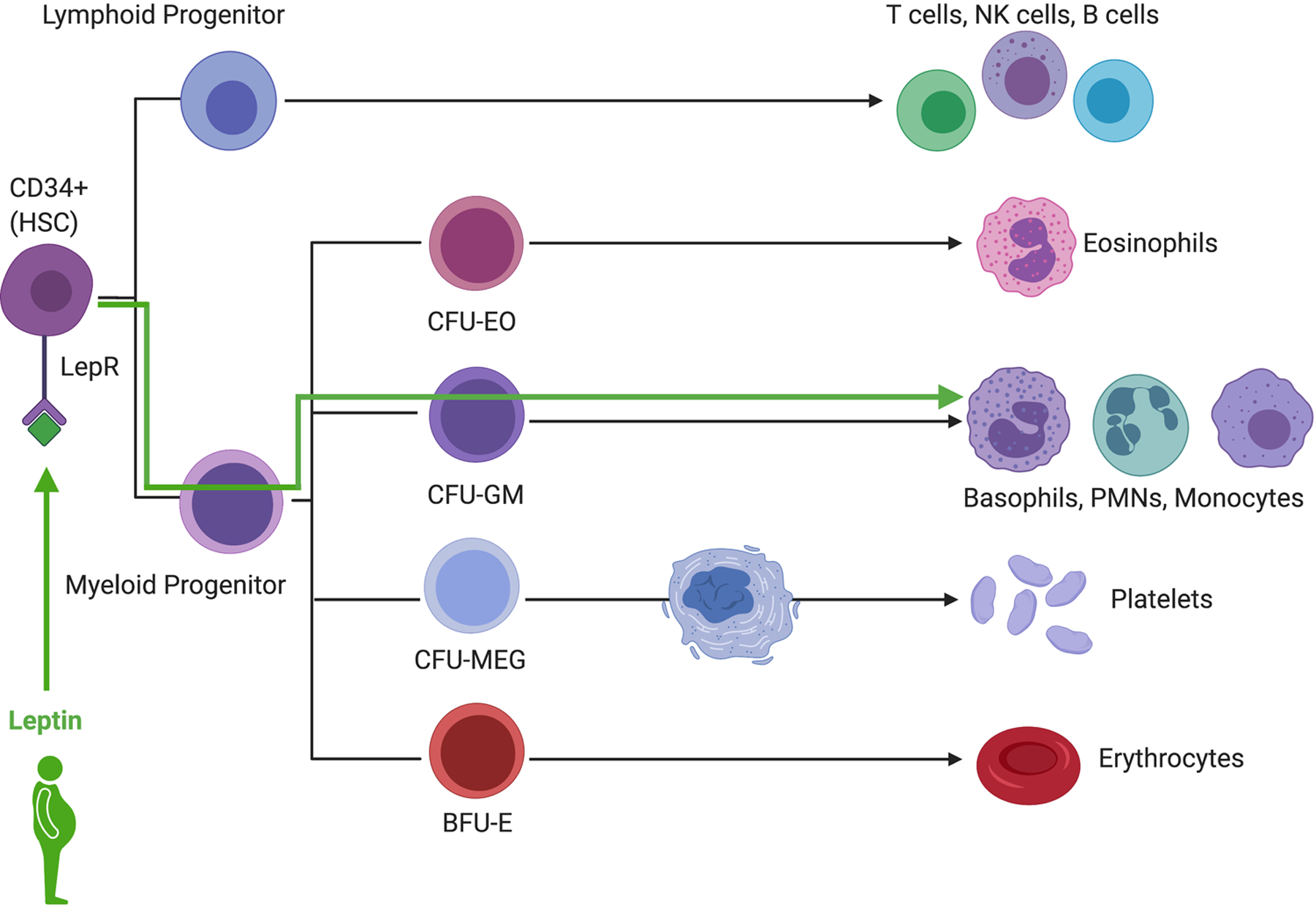
In hematopoiesis, leptin significantly stimulates the appearance of granulocyte-macrophage colonies (CFU-GM), the precursor for monocytes and granulocytes. CFU-EO = colony forming uniteosinophils; CFU-GM = colony forming unit-granulocyte, macrophage; CFU-MEG = colony forming unitmegakaryocyte; BFU-E, burst-forming unit-erythroid; LepR = leptin receptor. All figures were created with BioRender.com
Sex differences
As there is a clear predominance of obesity associated leukocytosis in women compared to men, it is important to discuss this observation. In women, even more than men, the etiology behind this leukocytosis is likely multifactorial. Higher levels of inflammatory mediators (e.g. CRP) and leptin are likely contributing, though the underlying mechanisms driving this difference remain unclear. As obesity in women is sometimes accompanied by polycystic ovarian syndrome (PCOS), this could also be contributing. Some cytokines, including IL-6 and TNF-α, are greater in women with PCOS compared to women of similar BMI57. Furthermore, total white cell count, due to a higher mean neutrophil count, has been found to be significantly greater in women with PCOS when compared to control subjects, despite matching for BMI and insulin resistance58,59. Also, as women with obesity and PCOS are at increased risk of developing obstructive sleep apnea (OSA)60,61, this could be considered a contributing factor. However, while there are multiple studies that have shown a positive association between OSA and the neutrophil to lymphocyte ratio62–65, a value sensitive to physiologic stress, few studies have independently associated OSA with leukocytosis, though it has been noted66. While we can theorize that the known elevated levels of systemic inflammatory markers in OSA (including CRP, IL-6 and TNF-α)67, or increased sympathetic activity associated with OSA68 would result in a leukocytosis, further studies are needed to solidify or reject this claim.
Conclusion
In summary the low-grade systemic inflammation that accompanies obesity results in elevated levels of cytokines (primarily IL-6 and IL-8) and adipokines such as leptin, which induce leukocytosis through multiple mechanisms, including demargination of intravascular neutrophils, acceleration of bone marrow neutrophil release and enhancement of bone marrow granulopoiesis; leptin in particular promotes the differentiation of granulocytes from hemopoietic progenitor cells. Several studies support the positive correlation between leukocyte count and BMI and there is a clear predominance of obesity associated leukocytosis in women compared to men. Possible explanations include an amplified inflammatory state and associated comorbidities such as PCOS and OSA.
Obesity and red blood cell count
Obesity and iron deficiency
Wenzel et al. (1962)69 were the first to report lower serum iron levels in obese compared to non-obese adolescents. Although it appears counterintuitive to expect iron deficiency (ID) in the setting of calorie and nutrient excess, lower concentrations of serum iron have been observed in relation to increasing BMI for many decades. Zhao et al. (2015)70 conducted a metanalysis of 26 cross-sectional and case-control studies, including a total of 13,393 overweight and obese individuals and 26,621 non-overweight subjects. They found that compared with the non-overweight group, the serum iron and transferrin saturation percentage were significantly different in the overweight/obese populations, with only a marginally significant difference in the serum ferritin level between the same groups. The pooled odds ratio (OR) of developing ID in the overweight/obese subjects was 1.31 (95% CI, 1.01– 1.68). Importantly, the method used to diagnose ID differed among the 15 studies that were included in that analysis, with only 8 studies using ferritin-based ID diagnosis. In the studies using a ferritin-based diagnosis, the association between ID and overweight/obesity was not significant (OR 1.04, 95% CI, 0.69–1.56). In contrast, the pooled OR calculated from the 7 studies that did not use a ferritin-based ID diagnosis was significant (OR 1.49, 95% CI, 1.19–1.85); using ferritin as the sole biomarker for assessment of ID may underestimate ID, due to the elevation of serum ferritin through obesity related chronic inflammation and the possibility that in overweight and obese individuals, ferritin is a marker of inflammation rather than iron status71. A review by Aigner et al. (2014)72 reported similar findings, as well as reported some improvements in iron status in the setting of weight loss.
It is important to acknowledge that many of the investigations included in the above metanalysis and review were performed in children and adolescents, and that in adults, the results are even more complex. In their metanalysis, Zhao et al. (2015) performed a subgroup analysis which revealed no association between obesity and ID in adults. Cheng et al. (2012)73 conducted a systematic review of 25 studies, looking at the association in adults only. They noted a tendency for higher ferritin and lower transferrin saturations in obese individuals, compared to their non-obese counterparts. Additional studies in non-pregnant adults (or a mean age ≥18), not included in either Zhao et al. (2015) or Cheng et al. (2012) have conflicting results. Some studies suggest an association between obesity and ID71,74–78, while multiple others note no difference79–82.
Given the literature, a relationship between obesity and ID likely exists in children and adolescents but remains unclear in adults. The reviews and metanalysis available are limited by the number of available studies, high heterogeneity in these studies, lack of consistent non-obese control groups, frequently uncontrolled confounders (e.g. acute infection, menopausal status, oral contraceptive use, iron supplementation, obesity-related comorbidities) and lack of standardization in diagnosing ID (e.g. some studies used ferritin alone, others used serum iron and transferrin saturation, very few used soluble transferrin receptor). This is particularly important given that obesity is associated with chronic low-grade inflammation which will potentially elevate ferritin and may alter the sensitivity of ferritin as an indicator of iron status; the use of additional biomarkers is something to be considered in future studies. While an association may be present between obesity and ID, future higher quality studies are needed to solidify this claim, as well as establish if a causal relationship exists.
Obesity and red blood cell count
Given that ID can progress to iron deficiency anemia (IDA), one may expect to see an association between obesity and IDA. In the metanalysis by Zhao et al. (2015), only 4 studies of the 26 analyzed looked at the risks of developing IDA in the obese population and the results differed, with only one reporting a higher risk of IDA in their obese group; the pooled OR of IDA in overweight/obese individuals was 1.09 (95% CI, 0.57–2.10). The review by Cheng et al. (2012) actually noted higher hemoglobin concentrations in the obese compare to non-obese controls. There have been additional studies not included in the above analysis which show lower levels of hemoglobin in obese compared to non-obese controls21,71, while others show no correlation80,81 or a protective effect83,84. Comorbidities associated with obesity, such as OSA or obesity hypoventilation syndrome, may be leading to a secondary polycythemia. Regardless, future studies are needed to look into this possible association.
Possible mechanisms driving iron deficiency
In children and adolescents, a possible explanation for the observed ID is higher iron demands, in the setting of accelerated body growth85. Poor dietary intake may also be playing a role86,87, though multiple studies have shown that this is unlikely88–91. Another theory is that increased iron requirements are due to a larger blood volume which increases iron requirements and confounds iron biomarkers by hemodilution92,93. The largest body of evidence actually points towards the chronic inflammatory state associated with obesity driving the observation, with hepcidin, and its role in iron homeostasis being the main player.
Iron homeostasis is regulated through hepcidin, a small peptide hormone largely produced by the liver, which controls the activity of ferroportin-1, an iron exporter. Increased serum levels of hepcidin result in reduced dietary iron absorption through downregulation of the exporter and increased iron sequestration within enterocytes, hepatocytes and iron-storing macrophages, leading to reduced iron bioavailability94,95 (Figure 2). It has been shown that obese subjects demonstrate impaired ability to absorb iron76,96–98.
Figure 2:
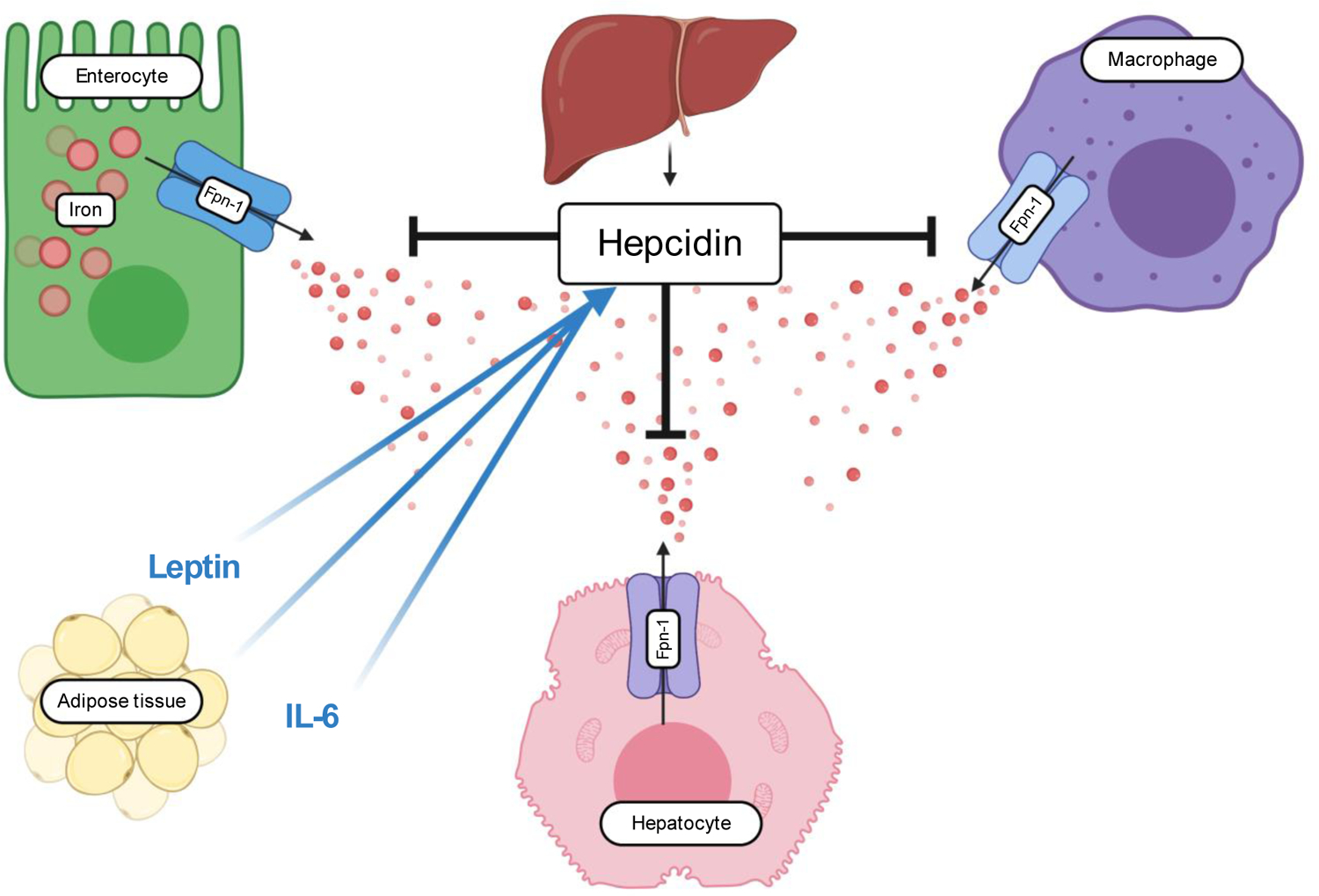
Hepcidin expression has been shown to be increased in obese individuals and correlates with inflammation, mainly driven by IL-6. Leptin also stimulates hepcidin expression. Additionally, adipose tissue has been shown to express hepcidin itself, marking hepcidin as an adipokine. Fpn-1 = ferroportin-1. All figures were created with BioRender.com
Hepcidin expression correlates with inflammation99. Given that obesity is a state of chronic low-grade inflammation, it comes as no surprise that hepcidin expression has been shown to be increased in obese individuals89,100. This increase in hepcidin is likely driven by cytokines, with significant data pointing to IL-6 as a main driver99,101–103. There is also in vitro evidence that leptin also stimulates hepcidin expression104. Additionally, adipose tissue has been shown to express hepcidin itself, marking hepcidin as an adipokine102, though this has been questioned105. It should also be noted that not all studies agree that hepcidin plays a role at all106.
Conclusion
In summary, a link between ID and obesity likely exists in children and adolescents but the association remains unclear in adults; a link between obesity and anemia remains even less certain. Given current limited studies of high heterogeneity and with conflicting results, future studies are needed to further assess this. Special care should be taken to include a non-obese control group, to include additional biomarkers of iron status which may not be as easily altered by the chronic inflammatory state accompanying obesity as is ferritin, and to control for confounders of iron status such as acute infection, menopausal status, and iron supplementation. Driving this possible association is the chronic inflammatory state associated with obesity, which through the secretion of cytokines such as IL-6, results in increased hepcidin expression and subsequent impaired duodenal absorption of iron. Leptin may also be playing a role in increased hepcidin expression and hepcidin itself may also be secreted by adipose tissue.
Obesity, platelets count and thrombosis
Obesity and platelet count
Obesity is also associated with increased platelet counts. Platelet counts have been found to be increased in obese non-diabetic rats107 as well as obese individuals, when compared to non-obese controls12,21,40, though the correlation has sometimes only been noted in women108. This correlation is further supported by observed reductions in platelet count in the setting of weight loss following bariatric surgery109. IL-6 is likely the main driver, working synergistically with other interleukins to increase thrombopoietin and subsequently stimulate megakaryocytopoiesis110–115. Visceral adipose tissue itself may also be an additional source of thrombopoietin116.
Obesity and thrombosis
There is substantial evidence that obesity as a proinflammatory condition, promotes a prothrombotic state, supporting arterial and venous thrombosis. A meta-analysis by Ageno et al. (2008)117 on the influence of obesity on the risk of first episode of venous thromboembolism (VTE) estimated an overall odds ratio for VTE of 2.33 (95% CI, 1.68–3.24). Tsai et al. (2002)118, included in that meta-analysis, found an even higher hazards ratio of 2.7 for patients with severe obesity (BMI≥40kg/m2). Di Minno et al. (2005)119, reported the OR of obesity for deep vein thrombosis to be 1.97 (95% CI, 1.4–2.78) for males and 2.29 (95% CI, 1.85–2.84) for females. There are many additional studies not included in the meta-analysis but with similar observations120–123. Borch et al. (2010)124 and Hansson et al. (1999)125 also noted associations with abdominal obesity and VTE. Eichinger et al. (2008)126 reported obesity as a risk factor for VTE recurrence, a risk which may be even higher in women compared to men127. In general, clinically men and women appear to experience different thrombotic phenotypes. As noted above, obese women appear to be at higher risk for VTE and data has shown, though not exclusive to obese individuals, that women appear to be at higher risk for stroke, while men are more likely to be affected by cardiovascular disease128. The relative protection of women against atherosclerosis before menopause is poorly understood with some thought that a more beneficial lipid profile contributes or that there is some protection conferred by sex hormones129.
The biological mechanisms underlying this observed connection are multifactorial and the relationship is confounded by a frequently accompanied metabolic syndrome and associated lifestyle factors, whose individual components (hyperinsulinemia, hypertriglyceridemia, hypertension) have associations with thrombosis by mechanisms independent of obesity. However, despite this, there is notable and consistent evidence of an association between obesity and thrombosis through damage to the venous endothelial layer, increased platelet reactivity, enhanced coagulation and impaired fibrinolysis, all discussed below and summarized in impressive reviews by Vilahur et al. (2017)130 and Schafer & Konstantinides (2011)131. The physical aspects of an obese body habitus may also contribute to the risk by promoting limited venous return through chronically raised intra-abdominal pressure and decreased blood velocity through the femoral vein132; inactivity and poor gait would likely have a compounding effect133.
The role of leptin in thrombosis
Leptin is a suspected driver of these prothrombotic changes through multiple mechanisms. There is significant data surrounding leptin mediated promotion of ADP-induced platelet aggregation134–137, with the inhibition of leptin via a neutralizing antibody being protective against arterial and venous thrombosis in mice138. However, Ozata et al. (2001)139 found no significant increase in platelet aggregation, even at high concentrations of leptin in obese subjects or controls. Other studies have also reported a reduction in the pro-aggregatory effects of leptin from obese individuals, suggesting platelet resistance to leptin in obesity140,141. P-selectin, a significant player in platelet aggregation, has been shown to have leptin mediated increased expression on human platelets in vitro142. However, this observation was not consistent and is without correlation in vivo. Less convincing, but also noted in the literature, is a contribution to elevated levels of tissue plasminogen activator (tPA) antigen143, which would promote thrombosis. Leptin also has been shown to induce elevated levels of plasminogen activator inhibitor-1 (PAI-1)144, which at higher concentrations is known to inhibit fibrinolysis and consequently promote a thrombotic state. Lastly, leptin is associated with increased factor levels, as noted below.
Obesity is associated with elevated levels of coagulation factors and von Willebrand factor
BMI has been shown to positively correlate with elevated factor levels and markers of fibrinolysis (fibrinogen, factor VII, factor VIII, factor IX, PAI-1, tPA antigen)120,145,146, with reductions in thrombin, tissue factor, PAI-1 and (prothrombin fragment 1.2) noted in weight loss147. Plasma levels of tissue factor, a significant driver of thrombus formation, are increased in obese subjects compared to healthy controls148. Leptin has been shown to increase tissue factor in humans149,150, and elevated levels of circulating tissue factor have been recognized as a contributor to the prothrombotic tendency of patients with high-grade obesity31. Levels of fibrinogen, von Willebrand factor and factor VII and VIII have all been found to be increased in obesity, with abdominal obesity noted to have a particular association146,151. Although elevations in factor levels are strongly associated with increased risk of VTE, one study did show that adjusting for clotting factor levels did not affect the risk estimate for obesity and VTE120; we did not find other studies that commented on this possibility. It remains unclear if these factors are merely biomarkers of inflammation, or direct contributors to thrombosis and this is an area that would benefit from further research.
Obesity impairs fibrinolysis
There is evidence tying PAI-1, which blocks the activation of fibrinolysis by inhibiting tPA (Figure 3), to obesity associated thrombosis, particularly through the metabolic syndrome and its interactions with insulin152. PAI-1 levels correlate with BMI146 and body fat distribution plays a role, with an association noted between waist-to-hip ratio and PAI-1 levels151,153. It has also been shown to be produced in adipose tissue154,155 and levels have been shown to decrease with weight loss156,157. As stated above, leptin may be a player in PAI-1 over expression, but TNF-α and transforming growth factor-β, which is produced in visceral fat, have also been proposed to be involved in the regulation of PAI-1 expression in adipose tissue133. CRP may also participate by enhancing the expression of PAI-1 in human endothelial cells158–160. Counter to this, tPA expression has also been associated with BMI146, with noted reductions following weight loss153,161.
Figure 3:
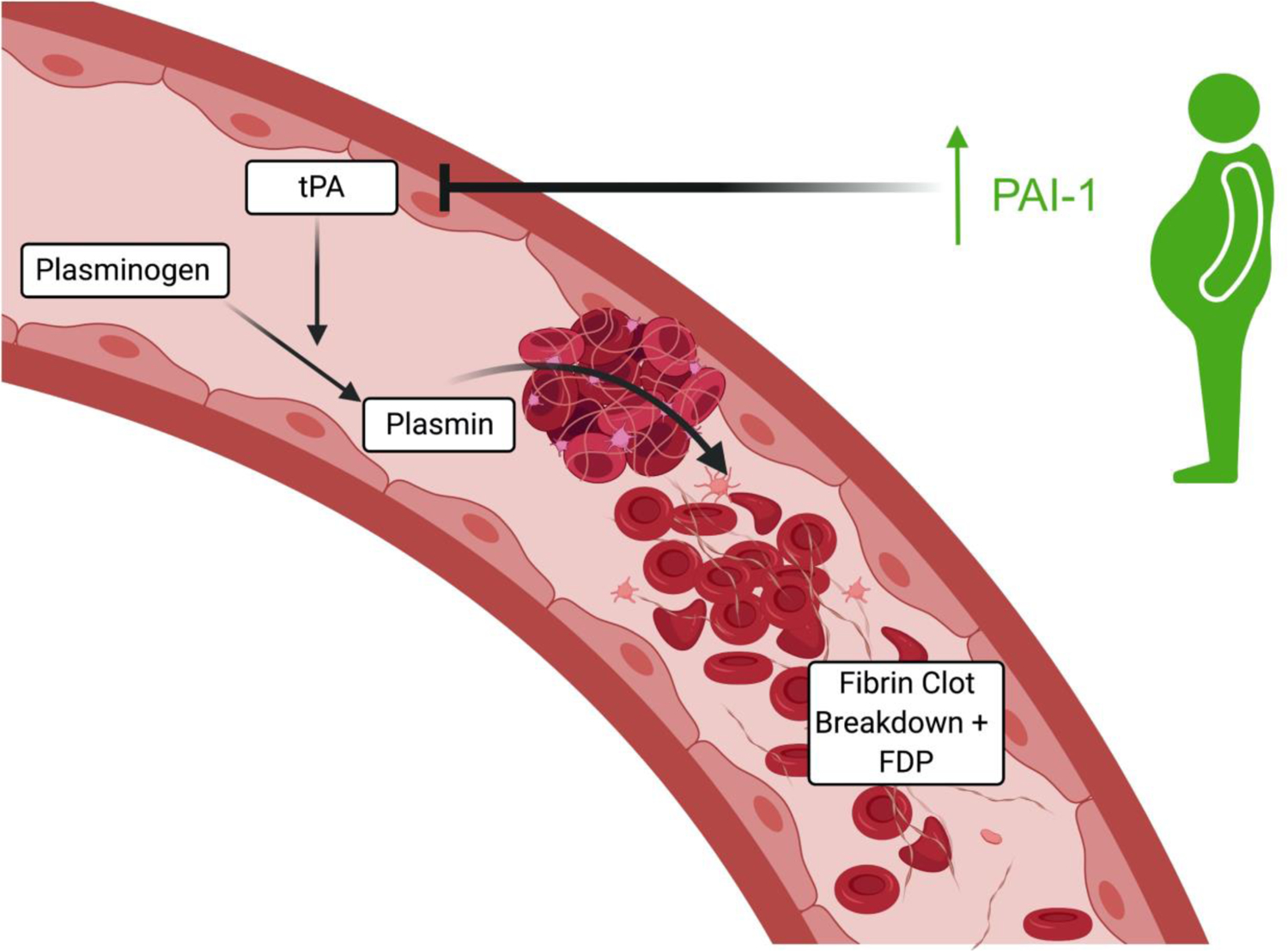
PAI-1, which blocks the activation of fibrinolysis, correlates with BMI and has been shown to be produced in adipose tissue. PAI-1 = Plasminogen activator inhibitor-1; tPA = tissue plasminogen activator; FDP = fibrin degradation products. All figures were created with BioRender.com
Obesity promotes platelet hyperactivity
Platelet activation is also a key component of thrombogenesis and platelet hyperactivity has been noted in obese individuals. Particularly, android obesity (abdominal obesity characterized by increased waist-to-hip ratio) has been found to have higher levels of platelet activation, as reflected by urinary excretion of the major metabolite of TXA2, 11-dehyhdro-TxB2, when compared to gynoid obese (gluteal-femoral obesity) women and non-obese women162. P-selectin expression is a marker of platelet activation, mediating the rolling of platelets on activated endothelial cells and promoting thrombogenesis by stabilizing initial GPIIb/IIIa-fibrinogen connections, permitting the development of large stable platelet aggregates in a venous thrombus. Epidemiological evidence has shown that platelet activation markers such as CD40L and P-selectin are increased in obesity and may reflect persistent in vivo platelet and endothelial activation163, with increased P-selectin expression noted in genetically and diet-induced obese mice164. CRP levels have been shown to increase P-selectin expression and platelet adhesion165. Mean platelet volume, an element of platelet function, is an emerging risk factor for thrombotic disease166,167 and has positively correlated with BMI168. Platelet-derived microparticles are considered an index of platelet activation and have pro-inflammatory and pro-thrombotic effects. These too may be playing a role, as circulating levels of platelet-derived microparticles are elevated in obese subjects in comparison with age-matched non-obese subjects153. Lastly, platelets from obese subjects have been found to retain greater reactivity after suppression by aspirin, compared to non-obese individuals after aspirin therapy169,170. These effects are summarized in Figure 4.
Figure 4:
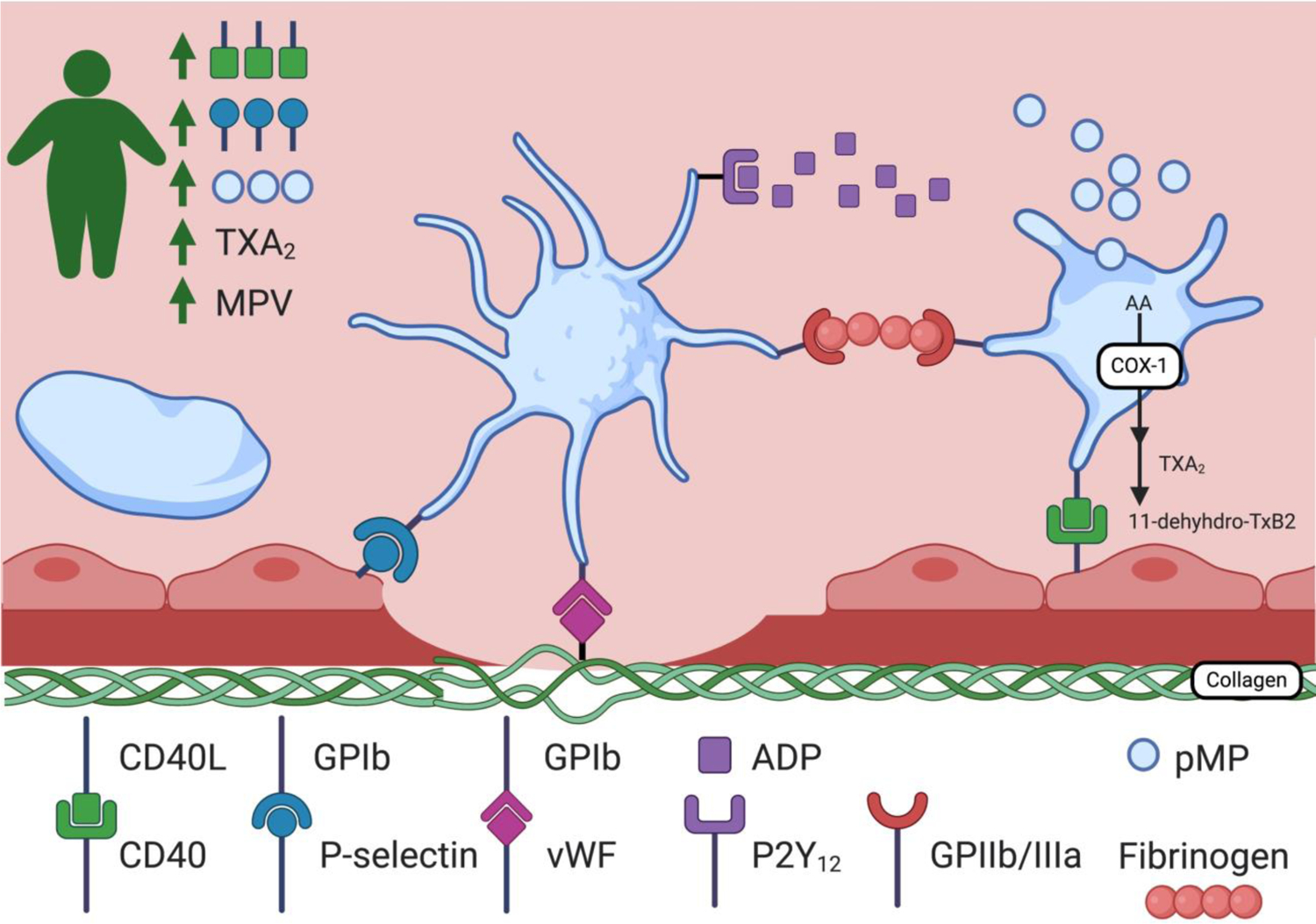
Platelet hyperactivity has been noted in obese individuals, as reflected by urinary excretion of 11-dehyhdro-TxB2, the major metabolite of TXA2. BMI has been associated with increased levels of CD40-L and P-selectin, as well as positively correlated with mean platelet volume, an emerging risk factor for thrombotic disease, and pMPs, markers of platelet activation. GPIb = Glycoprotein Ib; vWF = von Willebrand factor; ADP = Adenosine diphosphate; GPIIB/IIIa = glycoprotein IIb/IIIa; pMP = platelet-derived microparticles; MPV = mean platelet volume; TXA2 = Thromboxane A2; AA = arachidonic acid; COX-1 = Cyclooxygenase-1; 11-dehydro-TXB2 = 11-Dehydrothromboxane B2. All figures were created with BioRender.com
Obesity promotes endothelial dysfunction
Obese individuals exhibit endothelial dysfunction and this is likely induced by the continuous exposure to inflammatory stimuli and oxidative damage. It has been shown that endothelial cells exposed to cytokines secreted by adipose tissue from obese individuals have enhanced expression of endothelial adhesions molecules171. Leptin again may be contributing, promoting oxidative stress; leptin has been shown to increase levels of markers of endothelial cell dysfunction and activation172. Individual components of the metabolic syndrome (i.e. hyperlipidemia) which often accompany obesity, also contribute to activate the endothelial layer by enhancing endothelin-1 production, a vasoconstrictor and pro-inflammatory peptide, and conversely impairing nitric oxide and endothelium-derived hyperpolarizing factor related vasodilation leading to endothelial dysfunction130.
Conclusion
In summary, obesity is associated with increased platelet counts. IL-6 is likely a main contributor to this phenomenon, increasing thrombopoietin and subsequently stimulating megakaryocytopoiesis, resulting in thrombocytosis. There is also substantial evidence that obesity as a proinflammatory condition significantly increases the risk of VTE. The mechanisms underlying this are multifactorial and confounded by lifestyle factors, as well as the individual components of a frequently accompanying metabolic syndrome. However, despite this, there is extensive literature discussing elevated factor levels, impaired fibrinolysis, platelet hyperactivity and endothelial dysfunction, all driven by obesity and its associated inflammatory state; encouragingly, many of these abnormalities improve with weight loss.
Conclusion
There is a sizeable amount of data demonstrating that obesity is a state of chronic low-grade inflammation. Future studies to further understand the underlying mechanisms would be helpful, particularly, future investigations of leptin would be of high interest, given the high suspicion that it is involved in many of the perturbances to hematologic parameters and thrombosis. Also, future studies looking to unmask the underlying mechanisms driving an even higher inflammatory state in women compared to men, would be important in identifying risk factors that could be intervened on. There is an observed relative, and sometimes absolute, leukocytosis driven by this inflammatory state. Recognizing this association may prompt clinicians to avoid unnecessary and extensive work-ups by providing reassurance regarding an unexplained, stable and mild, neutrophilic leukocytosis in obese individuals who have the demographic features present in the above studies (e.g. middle-aged females). The association between obesity, ID and red blood cell counts remains uncertain and future well designed studies are needed to accept or reject this association, as well as to establish if a causal relationship exists. Given the accompanying state of chronic inflammation, identifying abnormalities of iron metabolism is particularly challenging in the obese, but this presents an opportunity to use and validate additional and novel biomarkers of iron status in future investigations and to standardize the methods used to diagnose ID in obese individuals. Also, recognizing that in obesity there is impaired iron absorption via the gut, making oral supplementation insufficient, encourages future studies to further explore and identify underlying mechanisms (e.g. hepcidin) as potential therapeutic targets that could prevent the development of ID in the obese. Lastly, there is sufficient evidence associating obesity with VTE, and some evidence that weight-loss resolves some of the underlying mechanistic abnormalities. Considering that the relative risk of first and recurrent VTE associated with obesity are comparable to those for other established risk factors such as hereditary thrombophilia and estrogen therapy173, and given the high morbidity and mortality that VTE can carry, this presents an additional opportunity for clinicians to more vigorously encourage weight-loss amongst their obese patients. This also further incentivizes future research in the area, particularly with regards to anti-coagulation and anti-inflammatory therapies to prevent thrombosis in obesity.
Summary Statements.
To our knowledge, there is no single review summarizing the effects of obesity on commonly measured hematologic parameters and thrombotic risk, this addresses that.
Obesity is associated with a state of chronic low-grade inflammation and subsequently with an observed relative and sometimes absolute leukocytosis, as well as an increased risk for venous thromboembolism (VTE); its effects on iron deficiency (ID) and red blood cell counts remain unclear.
Recognizing the above associations may provide reassurance regarding otherwise unexplained hematologic abnormalities in obese individuals as well as prompt future studies to identify modifiable risk factors and potential therapeutic targets to prevent the development of probable obesity-associated conditions with significant morbidity and mortality, such as ID and VTE.
Acknowledgment of research support:
J. Shatzel is supported by the National Institutes of Health, National Heart, Lung, and Blood Institute (HL151367)
Footnotes
Conflict-of-interest disclosure: J.J.S. is a consultant for Aronora, Inc. The remaining authors declare no potential conflict of interest.
Data Availability Statement:
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- 1.Centers for Disease Control and Prevention. Adult obesity facts. 2020, February 27; https://www.cdc.gov/obesity/data/adult.html.
- 2.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med. December 19 2019;381(25):2440–2450. [DOI] [PubMed] [Google Scholar]
- 3.Fantuzzi G Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. May 2005;115(5):911–919; quiz 920. [DOI] [PubMed] [Google Scholar]
- 4.Gregor MF, Hotamisligil GS. Inflammatory mechanisms in obesity. Annu Rev Immunol. 2011;29:415–445. [DOI] [PubMed] [Google Scholar]
- 5.Curat CA, Miranville A, Sengenes C, et al. From blood monocytes to adipose tissue-resident macrophages: induction of diapedesis by human mature adipocytes. Diabetes. May 2004;53(5):1285–1292. [DOI] [PubMed] [Google Scholar]
- 6.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. December 2003;112(12):1796–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harman-Boehm I, Bluher M, Redel H, et al. Macrophage infiltration into omental versus subcutaneous fat across different populations: effect of regional adiposity and the comorbidities of obesity. J Clin Endocrinol Metab. June 2007;92(6):2240–2247. [DOI] [PubMed] [Google Scholar]
- 8.Cousin B, Munoz O, Andre M, et al. A role for preadipocytes as macrophage-like cells. FASEB J. February 1999;13(2):305–312. [DOI] [PubMed] [Google Scholar]
- 9.Osborn O, Olefsky JM. The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med. March 6 2012;18(3):363–374. [DOI] [PubMed] [Google Scholar]
- 10.Boutens L, Stienstra R. Adipose tissue macrophages: going off track during obesity. Diabetologia. May 2016;59(5):879–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Banks R, Forbes M, Storr M, et al. The acute phase protein response in patients receiving subcutaneous IL-6. Clinical & Experimental Immunology. 1995;102(1):217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herishanu Y, Rogowski O, Polliack A, Marilus R. Leukocytosis in obese individuals: possible link in patients with unexplained persistent neutrophilia. Eur J Haematol. June 2006;76(6):516–520. [DOI] [PubMed] [Google Scholar]
- 13.Cottam DR, Mattar SG, Barinas-Mitchell E, et al. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: implications and effects of weight loss. Obes Surg. May 2004;14(5):589–600. [DOI] [PubMed] [Google Scholar]
- 14.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. January 1 1993;259(5091):87–91. [DOI] [PubMed] [Google Scholar]
- 15.Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol. April 1999;19(4):972–978. [DOI] [PubMed] [Google Scholar]
- 16.Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis. February 2000;148(2):209–214. [DOI] [PubMed] [Google Scholar]
- 17.Park HS, Park JY, Yu R. Relationship of obesity and visceral adiposity with serum concentrations of CRP, TNF-alpha and IL-6. Diabetes Res Clin Pract. July 2005;69(1):29–35. [DOI] [PubMed] [Google Scholar]
- 18.Roytblat L, Rachinsky M, Fisher A, et al. Raised interleukin-6 levels in obese patients. Obes Res. December 2000;8(9):673–675. [DOI] [PubMed] [Google Scholar]
- 19.Pou KM, Massaro JM, Hoffmann U, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. September 11 2007;116(11):1234–1241. [DOI] [PubMed] [Google Scholar]
- 20.Katsuki A, Sumida Y, Murashima S, et al. Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. March 1998;83(3):859–862. [DOI] [PubMed] [Google Scholar]
- 21.Farhangi MA, Keshavarz SA, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi AA. White blood cell count in women: relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. J Health Popul Nutr. March 2013;31(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohamed-Ali V, Goodrick S, Rawesh A, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab. December 1997;82(12):4196–4200. [DOI] [PubMed] [Google Scholar]
- 23.Bastard JP, Jardel C, Bruckert E, et al. Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss. J Clin Endocrinol Metab. September 2000;85(9):3338–3342. [DOI] [PubMed] [Google Scholar]
- 24.Ziccardi P, Nappo F, Giugliano G, et al. Reduction of inflammatory cytokine concentrations and improvement of endothelial functions in obese women after weight loss over one year. Circulation. February 19 2002;105(7):804–809. [DOI] [PubMed] [Google Scholar]
- 25.Nicklas BJ, Ambrosius W, Messier SP, et al. Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Am J Clin Nutr. April 2004;79(4):544–551. [DOI] [PubMed] [Google Scholar]
- 26.Esposito K, Pontillo A, Di Palo C, et al. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA. April 9 2003;289(14):1799–1804. [DOI] [PubMed] [Google Scholar]
- 27.Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab. August 1998;83(8):2907–2910. [DOI] [PubMed] [Google Scholar]
- 28.Kern PA, Saghizadeh M, Ong JM, Bosch RJ, Deem R, Simsolo RB. The expression of tumor necrosis factor in human adipose tissue. Regulation by obesity, weight loss, and relationship to lipoprotein lipase. J Clin Invest. May 1995;95(5):2111–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swarbrick MM, Stanhope KL, Austrheim-Smith IT, et al. Longitudinal changes in pancreatic and adipocyte hormones following Roux-en-Y gastric bypass surgery. Diabetologia. October 2008;51(10):1901–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin E, Phillips LS, Ziegler TR, et al. Increases in adiponectin predict improved liver, but not peripheral, insulin sensitivity in severely obese women during weight loss. Diabetes. March 2007;56(3):735–742. [DOI] [PubMed] [Google Scholar]
- 31.Kopp CW, Kopp HP, Steiner S, et al. Weight loss reduces tissue factor in morbidly obese patients. Obes Res. August 2003;11(8):950–956. [DOI] [PubMed] [Google Scholar]
- 32.Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J Clin Endocrinol Metab. March 1998;83(3):847–850. [DOI] [PubMed] [Google Scholar]
- 33.Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology. May 2004;145(5):2273–2282. [DOI] [PubMed] [Google Scholar]
- 34.Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-Reactive Protein Levels in Overweight and Obese Adults. JAMA. 1999;282(22):2131–2135. [DOI] [PubMed] [Google Scholar]
- 35.Festa A, D’Agostino R Jr., Williams K, et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord. October 2001;25(10):1407–1415. [DOI] [PubMed] [Google Scholar]
- 36.Ford ES. Body mass index, diabetes, and C-reactive protein among U.S. adults. Diabetes Care. December 1999;22(12):1971–1977. [DOI] [PubMed] [Google Scholar]
- 37.Tchernof A, Nolan A, Sites CK, Ades PA, Poehlman ET. Weight loss reduces C-reactive protein levels in obese postmenopausal women. Circulation. February 5 2002;105(5):564–569. [DOI] [PubMed] [Google Scholar]
- 38.Vazquez LA, Pazos F, Berrazueta JR, et al. Effects of changes in body weight and insulin resistance on inflammation and endothelial function in morbid obesity after bariatric surgery. J Clin Endocrinol Metab. January 2005;90(1):316–322. [DOI] [PubMed] [Google Scholar]
- 39.Calabro P, Chang DW, Willerson JT, Yeh ET. Release of C-reactive protein in response to inflammatory cytokines by human adipocytes: linking obesity to vascular inflammation. J Am Coll Cardiol. September 20 2005;46(6):1112–1113. [DOI] [PubMed] [Google Scholar]
- 40.Raghavan V, Gunasekar D, Rao KR. Relevance of Haematologic Parameters in Obese Women with or without Metabolic Syndrome. J Clin Diagn Res. May 2016;10(5):EC11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soehnlein O, Steffens S, Hidalgo A, Weber C. Neutrophils as protagonists and targets in chronic inflammation. Nat Rev Immunol. April 2017;17(4):248–261. [DOI] [PubMed] [Google Scholar]
- 42.do Carmo LS, Rogero MM, Paredes-Gamero EJ, et al. A high-fat diet increases interleukin-3 and granulocyte colony-stimulating factor production by bone marrow cells and triggers bone marrow hyperplasia and neutrophilia in Wistar rats. Exp Biol Med (Maywood). April 2013;238(4):375–384. [DOI] [PubMed] [Google Scholar]
- 43.Julius S, Egan BM, Kaciroti NA, Nesbitt SD, Chen AK, investigators T. In prehypertension leukocytosis is associated with body mass index but not with blood pressure or incident hypertension. J Hypertens. February 2014;32(2):251–259. [DOI] [PubMed] [Google Scholar]
- 44.Pratley RE, Wilson C, Bogardus C. Relation of the white blood cell count to obesity and insulin resistance: effect of race and gender. Obes Res. November 1995;3(6):563–571. [DOI] [PubMed] [Google Scholar]
- 45.Nanji AA, Freeman JB. Relationship between body weight and total leukocyte count in morbid obesity. Am J Clin Pathol. September 1985;84(3):346–347. [DOI] [PubMed] [Google Scholar]
- 46.Ulich TR, del Castillo J, Guo KZ. In vivo hematologic effects of recombinant interleukin-6 on hematopoiesis and circulating numbers of RBCs and WBCs. Blood. January 1989;73(1):108–110. [PubMed] [Google Scholar]
- 47.Suwa T, Hogg JC, English D, Van Eeden SF. Interleukin-6 induces demargination of intravascular neutrophils and shortens their transit in marrow. Am J Physiol Heart Circ Physiol. December 2000;279(6):H2954–2960. [DOI] [PubMed] [Google Scholar]
- 48.Witko-Sarsat V, Rieu P, Descamps-Latscha B, Lesavre P, Halbwachs-Mecarelli L. Neutrophils: molecules, functions and pathophysiological aspects. Lab Invest. May 2000;80(5):617–653. [DOI] [PubMed] [Google Scholar]
- 49.van Eeden SF, Terashima T. Interleukin 8 (IL-8) and the release of leukocytes from the bone marrow. Leuk Lymphoma. April 2000;37(3–4):259–271. [DOI] [PubMed] [Google Scholar]
- 50.Pini M, Rhodes DH, Fantuzzi G. Hematological and acute-phase responses to diet-induced obesity in IL-6 KO mice. Cytokine. December 2011;56(3):708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson CA, Bekele G, Nicolson M, Ravussin E, Pratley RE. Relationship of the white blood cell count to body fat: role of leptin. Br J Haematol. November 1997;99(2):447–451. [DOI] [PubMed] [Google Scholar]
- 52.Laharrague P, Oppert JM, Brousset P, et al. High concentration of leptin stimulates myeloid differentiation from human bone marrow CD34+ progenitors: potential involvement in leukocytosis of obese subjects. Int J Obes Relat Metab Disord. September 2000;24(9):1212–1216. [DOI] [PubMed] [Google Scholar]
- 53.Severe N, Karabacak NM, Gustafsson K, et al. Stress-Induced Changes in Bone Marrow Stromal Cell Populations Revealed through Single-Cell Protein Expression Mapping. Cell Stem Cell. October 3 2019;25(4):570–583 e577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dias CC, Nogueira-Pedro A, Barbosa CM, et al. Hematopoietic stem cell expansion caused by a synthetic fragment of leptin. Peptides. December 2013;50:24–27. [DOI] [PubMed] [Google Scholar]
- 55.Zhou BO, Yue R, Murphy MM, Peyer JG, Morrison SJ. Leptin-receptor-expressing mesenchymal stromal cells represent the main source of bone formed by adult bone marrow. Cell Stem Cell. August 7 2014;15(2):154–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sugiyama T, Omatsu Y, Nagasawa T. Niches for hematopoietic stem cells and immune cell progenitors. Int Immunol. February 6 2019;31(1):5–11. [DOI] [PubMed] [Google Scholar]
- 57.Tarkun I, Cetinarslan B, Turemen E, Canturk Z, Biyikli M. Association between Circulating Tumor Necrosis Factor-Alpha, Interleukin-6, and Insulin Resistance in Normal-Weight Women with Polycystic Ovary Syndrome. Metab Syndr Relat Disord. Summer 2006;4(2):122–128. [DOI] [PubMed] [Google Scholar]
- 58.Phelan N, O’Connor A, Kyaw Tun T, et al. Leucocytosis in women with polycystic ovary syndrome (PCOS) is incompletely explained by obesity and insulin resistance. Clin Endocrinol (Oxf). January 2013;78(1):107–113. [DOI] [PubMed] [Google Scholar]
- 59.Herlihy AC, Kelly RE, Hogan JL, O’Connor N, Farah N, Turner MJ. Polycystic ovary syndrome and the peripheral blood white cell count. J Obstet Gynaecol. 2011;31(3):242–244. [DOI] [PubMed] [Google Scholar]
- 60.Kahal H, Kyrou I, Tahrani AA, Randeva HS. Obstructive sleep apnoea and polycystic ovary syndrome: A comprehensive review of clinical interactions and underlying pathophysiology. Clin Endocrinol (Oxf). October 2017;87(4):313–319. [DOI] [PubMed] [Google Scholar]
- 61.Kahal H, Kyrou I, Uthman OA, et al. The prevalence of obstructive sleep apnoea in women with polycystic ovary syndrome: a systematic review and meta-analysis. Sleep Breath. May 20 2019. [DOI] [PMC free article] [PubMed]
- 62.Bozkus F, Dikmen N, Samur A, Bilal N, Atilla N, Arpag H. Does the neutrophil-to-lymphocyte ratio have any importance between subjects with obstructive sleep apnea syndrome with obesity and without obesity? Tuberk Toraks. March 2018;66(1):8–15. [DOI] [PubMed] [Google Scholar]
- 63.Sunbul M, Sunbul EA, Kanar B, et al. The association of neutrophil to lymphocyte ratio with presence and severity of obstructive sleep apnea. Bratisl Lek Listy. 2015;116(11):654–658. [DOI] [PubMed] [Google Scholar]
- 64.Altintas N, Cetinoglu E, Yuceege M, et al. Neutrophil-to-lymphocyte ratio in obstructive sleep apnea; a multi center, retrospective study. Eur Rev Med Pharmacol Sci. September 2015;19(17):3234–3240. [PubMed] [Google Scholar]
- 65.Oyama J, Nagatomo D, Yoshioka G, et al. The relationship between neutrophil to lymphocyte ratio, endothelial function, and severity in patients with obstructive sleep apnea. J Cardiol. March 2016;67(3):295–302. [DOI] [PubMed] [Google Scholar]
- 66.Geovanini GR, Wang R, Weng J, et al. Elevations in neutrophils with obstructive sleep apnea: The Multi-Ethnic Study of Atherosclerosis (MESA). Int J Cardiol. April 15 2018;257:318–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nadeem R, Molnar J, Madbouly EM, et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med. October 15 2013;9(10):1003–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mansukhani MP, Kara T, Caples SM, Somers VK. Chemoreflexes, sleep apnea, and sympathetic dysregulation. Curr Hypertens Rep. September 2014;16(9):476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wenzel BJ, Stults HB, Mayer J. Hypoferraemia in obese adolescents. Lancet. August 18 1962;2(7251):327–328. [DOI] [PubMed] [Google Scholar]
- 70.Zhao L, Zhang X, Shen Y, Fang X, Wang Y, Wang F. Obesity and iron deficiency: a quantitative meta-analysis. Obes Rev. December 2015;16(12):1081–1093. [DOI] [PubMed] [Google Scholar]
- 71.Khan A, Khan WM, Ayub M, Humayun M, Haroon M. Ferritin Is a Marker of Inflammation rather than Iron Deficiency in Overweight and Obese People. J Obes. 2016;2016:1937320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aigner E, Feldman A, Datz C. Obesity as an emerging risk factor for iron deficiency. Nutrients. September 11 2014;6(9):3587–3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cheng HL, Bryant C, Cook R, O’Connor H, Rooney K, Steinbeck K. The relationship between obesity and hypoferraemia in adults: a systematic review. Obes Rev. February 2012;13(2):150–161. [DOI] [PubMed] [Google Scholar]
- 74.Monteiro AM, Fernandes V, Matta-Coelho C, et al. Iron Deficiency and Obesity - Are we Diagnosing with Appropriate Indicators? Acta Med Port. September 28 2018;31(9):478–482. [DOI] [PubMed] [Google Scholar]
- 75.Shekarriz R, Vaziri MM. Iron Profile and Inflammatory Status of Overweight and Obese Women in Sari, North of Iran. Int J Hematol Oncol Stem Cell Res. April 1 2017;11(2):108–113. [PMC free article] [PubMed] [Google Scholar]
- 76.Herter-Aeberli I, Thankachan P, Bose B, Kurpad AV. Increased risk of iron deficiency and reduced iron absorption but no difference in zinc, vitamin A or B-vitamin status in obese women in India. Eur J Nutr. December 2016;55(8):2411–2421. [DOI] [PubMed] [Google Scholar]
- 77.Asghari G, Khalaj A, Ghadimi M, et al. Prevalence of Micronutrient Deficiencies Prior to Bariatric Surgery: Tehran Obesity Treatment Study (TOTS). Obes Surg. August 2018;28(8):2465–2472. [DOI] [PubMed] [Google Scholar]
- 78.Neymotin F, Sen U. Iron and obesity in females in the United States. Obesity (Silver Spring). January 2011;19(1):191–199. [DOI] [PubMed] [Google Scholar]
- 79.Adib Rad H, Sefidgar SAA, Tamadoni A, et al. Obesity and iron-deficiency anemia in women of reproductive age in northern Iran. J Educ Health Promot. 2019;8:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Arshad M, Jaberian S, Pazouki A, Riazi S, Rangraz MA, Mokhber S. Iron deficiency anemia and megaloblastic anemia in obese patients. Rom J Intern Med. March 1 2017;55(1):3–7. [DOI] [PubMed] [Google Scholar]
- 81.Wang C, Guan B, Yang W, Yang J, Cao G, Lee S. Prevalence of electrolyte and nutritional deficiencies in Chinese bariatric surgery candidates. Surg Obes Relat Dis. Mar-Apr 2016;12(3):629–634. [DOI] [PubMed] [Google Scholar]
- 82.Lefebvre P, Letois F, Sultan A, Nocca D, Mura T, Galtier F. Nutrient deficiencies in patients with obesity considering bariatric surgery: a cross-sectional study. Surg Obes Relat Dis. May-Jun 2014;10(3):540–546. [DOI] [PubMed] [Google Scholar]
- 83.Ghose B, Yaya S, Tang S. Anemia Status in Relation to Body Mass Index Among Women of Childbearing Age in Bangladesh. Asia Pac J Public Health. October 2016;28(7):611–619. [DOI] [PubMed] [Google Scholar]
- 84.Qin Y, Melse-Boonstra A, Pan X, et al. Anemia in relation to body mass index and waist circumference among Chinese women. Nutr J. January 11 2013;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dallman PR, Siimes MA, Stekel A. Iron deficiency in infancy and childhood. Am J Clin Nutr. January 1980;33(1):86–118. [DOI] [PubMed] [Google Scholar]
- 86.Farhat G, Lees E, Macdonald-Clarke C, Amirabdollahian F. Inadequacies of micronutrient intake in normal weight and overweight young adults aged 18–25 years: a cross-sectional study. Public Health. February 2019;167:70–77. [DOI] [PubMed] [Google Scholar]
- 87.Sanchez A, Rojas P, Basfi-Fer K, et al. Micronutrient Deficiencies in Morbidly Obese Women Prior to Bariatric Surgery. Obes Surg. February 2016;26(2):361–368. [DOI] [PubMed] [Google Scholar]
- 88.Tussing-Humphreys LM, Liang H, Nemeth E, Freels S, Braunschweig CA. Excess adiposity, inflammation, and iron-deficiency in female adolescents. J Am Diet Assoc. February 2009;109(2):297–302. [DOI] [PubMed] [Google Scholar]
- 89.Aeberli I, Hurrell RF, Zimmermann MB. Overweight children have higher circulating hepcidin concentrations and lower iron status but have dietary iron intakes and bioavailability comparable with normal weight children. Int J Obes (Lond). October 2009;33(10):1111–1117. [DOI] [PubMed] [Google Scholar]
- 90.Menzie CM, Yanoff LB, Denkinger BI, et al. Obesity-related hypoferremia is not explained by differences in reported intake of heme and nonheme iron or intake of dietary factors that can affect iron absorption. J Am Diet Assoc. January 2008;108(1):145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cepeda-Lopez AC, Osendarp SJ, Melse-Boonstra A, et al. Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity-related inflammation rather than by differences in dietary iron intake. Am J Clin Nutr. May 2011;93(5):975–983. [DOI] [PubMed] [Google Scholar]
- 92.Failla ML, Kennedy ML, Chen ML. Iron metabolism in genetically obese (ob/ob) mice. J Nutr. January 1988;118(1):46–51. [DOI] [PubMed] [Google Scholar]
- 93.Cepeda-Lopez AC, Zimmermann MB, Wussler S, et al. Greater blood volume and Hb mass in obese women quantified by the carbon monoxide-rebreathing method affects interpretation of iron biomarkers and iron requirements. Int J Obes (Lond). May 2019;43(5):999–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nemeth E, Ganz T. The role of hepcidin in iron metabolism. Acta Haematol. 2009;122(2–3):78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chung B, Chaston T, Marks J, Srai SK, Sharp PA. Hepcidin decreases iron transporter expression in vivo in mouse duodenum and spleen and in vitro in THP-1 macrophages and intestinal Caco-2 cells. J Nutr. August 2009;139(8):1457–1462. [DOI] [PubMed] [Google Scholar]
- 96.Mujica-Coopman MF, Brito A, Lopez de Romana D, Pizarro F, Olivares M. Body mass index, iron absorption and iron status in childbearing age women. J Trace Elem Med Biol. April 2015;30:215–219. [DOI] [PubMed] [Google Scholar]
- 97.Zimmermann MB, Zeder C, Muthayya S, et al. Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification. Int J Obes (Lond). July 2008;32(7):1098–1104. [DOI] [PubMed] [Google Scholar]
- 98.Cepeda-Lopez AC, Melse-Boonstra A, Zimmermann MB, Herter-Aeberli I. In overweight and obese women, dietary iron absorption is reduced and the enhancement of iron absorption by ascorbic acid is one-half that in normal-weight women. Am J Clin Nutr. December 2015;102(6):1389–1397. [DOI] [PubMed] [Google Scholar]
- 99.Nemeth E, Valore EV, Territo M, Schiller G, Lichtenstein A, Ganz T. Hepcidin, a putative mediator of anemia of inflammation, is a type II acute-phase protein. Blood. April 1 2003;101(7):2461–2463. [DOI] [PubMed] [Google Scholar]
- 100.del Giudice EM, Santoro N, Amato A, et al. Hepcidin in obese children as a potential mediator of the association between obesity and iron deficiency. J Clin Endocrinol Metab. December 2009;94(12):5102–5107. [DOI] [PubMed] [Google Scholar]
- 101.Nemeth E, Rivera S, Gabayan V, et al. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest. May 2004;113(9):1271–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bekri S, Gual P, Anty R, et al. Increased adipose tissue expression of hepcidin in severe obesity is independent from diabetes and NASH. Gastroenterology. September 2006;131(3):788–796. [DOI] [PubMed] [Google Scholar]
- 103.Wrighting DM, Andrews NC. Interleukin-6 induces hepcidin expression through STAT3. Blood. November 1 2006;108(9):3204–3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chung B, Matak P, McKie AT, Sharp P. Leptin increases the expression of the iron regulatory hormone hepcidin in HuH7 human hepatoma cells. J Nutr. November 2007;137(11):2366–2370. [DOI] [PubMed] [Google Scholar]
- 105.Tussing-Humphreys L, Frayn KN, Smith SR, et al. Subcutaneous adipose tissue from obese and lean adults does not release hepcidin in vivo. Scientific World Journal. 2011;11:2197–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sal E, Yenicesu I, Celik N, et al. Relationship between obesity and iron deficiency anemia: is there a role of hepcidin? Hematology. September 2018;23(8):542–548. [DOI] [PubMed] [Google Scholar]
- 107.Hernandez Vera R, Vilahur G, Badimon L. Obesity with insulin resistance increase thrombosis in wild-type and bone marrow-transplanted Zucker Fatty rats. Thromb Haemost. February 2013;109(2):319–327. [DOI] [PubMed] [Google Scholar]
- 108.Samocha-Bonet D, Justo D, Rogowski O, et al. Platelet counts and platelet activation markers in obese subjects. Mediators Inflamm. 2008;2008:834153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Raoux L, Moszkowicz D, Vychnevskaia K, et al. Effect of Bariatric Surgery-Induced Weight Loss on Platelet Count and Mean Platelet Volume: a 12-Month Follow-Up Study. Obes Surg. February 2017;27(2):387–393. [DOI] [PubMed] [Google Scholar]
- 110.Williams JL, Pipia GG, Datta NS, Long MW. Thrombopoietin requires additional megakaryocyte-active cytokines for optimal ex vivo expansion of megakaryocyte precursor cells. Blood. June 1 1998;91(11):4118–4126. [PubMed] [Google Scholar]
- 111.Lazzari L, Henschler R, Lecchi L, Rebulla P, Mertelsmann R, Sirchia G. Interleukin-6 and interleukin-11 act synergistically with thrombopoietin and stem cell factor to modulate ex vivo expansion of human CD41+ and CD61+ megakaryocytic cells. Haematologica. January 2000;85(1):25–30. [PubMed] [Google Scholar]
- 112.Kaser A, Brandacher G, Steurer W, et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood. November 1 2001;98(9):2720–2725. [DOI] [PubMed] [Google Scholar]
- 113.Baatout S Interleukin-6 and megakaryocytopoiesis: an update. Ann Hematol. October 1996;73(4):157–162. [DOI] [PubMed] [Google Scholar]
- 114.Sui X, Tsuji K, Ebihara Y, et al. Soluble interleukin-6 (IL-6) receptor with IL-6 stimulates megakaryopoiesis from human CD34(+) cells through glycoprotein (gp)130 signaling. Blood. April 15 1999;93(8):2525–2532. [PubMed] [Google Scholar]
- 115.Burmester H, Wolber EM, Freitag P, Fandrey J, Jelkmann W. Thrombopoietin production in wild-type and interleukin-6 knockout mice with acute inflammation. J Interferon Cytokine Res. July 2005;25(7):407–413. [DOI] [PubMed] [Google Scholar]
- 116.Maury E, Ehala-Aleksejev K, Guiot Y, Detry R, Vandenhooft A, Brichard SM. Adipokines oversecreted by omental adipose tissue in human obesity. Am J Physiol Endocrinol Metab. September 2007;293(3):E656–665. [DOI] [PubMed] [Google Scholar]
- 117.Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. January 1 2008;117(1):93–102. [DOI] [PubMed] [Google Scholar]
- 118.Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med. May 27 2002;162(10):1182–1189. [DOI] [PubMed] [Google Scholar]
- 119.Di Minno G, Mannucci PM, Tufano A, et al. The first ambulatory screening on thromboembolism: a multicentre, cross-sectional, observational study on risk factors for venous thromboembolism. J Thromb Haemost. July 2005;3(7):1459–1466. [DOI] [PubMed] [Google Scholar]
- 120.Abdollahi M, Cushman M, Rosendaal FR. Obesity: risk of venous thrombosis and the interaction with coagulation factor levels and oral contraceptive use. Thromb Haemost. March 2003;89(3):493–498. [PubMed] [Google Scholar]
- 121.Holst AG, Jensen G, Prescott E. Risk factors for venous thromboembolism: results from the Copenhagen City Heart Study. Circulation. May 4 2010;121(17):1896–1903. [DOI] [PubMed] [Google Scholar]
- 122.Samama MM. An epidemiologic study of risk factors for deep vein thrombosis in medical outpatients: the Sirius study. Arch Intern Med. December 11–25 2000;160(22):3415–3420. [DOI] [PubMed] [Google Scholar]
- 123.Stein PD, Beemath A, Olson RE. Obesity as a risk factor in venous thromboembolism. Am J Med. September 2005;118(9):978–980. [DOI] [PubMed] [Google Scholar]
- 124.Borch KH, Braekkan SK, Mathiesen EB, et al. Anthropometric measures of obesity and risk of venous thromboembolism: the Tromso study. Arterioscler Thromb Vasc Biol. January 2010;30(1):121–127. [DOI] [PubMed] [Google Scholar]
- 125.Hansson PO, Eriksson H, Welin L, Svardsudd K, Wilhelmsen L. Smoking and abdominal obesity: risk factors for venous thromboembolism among middle-aged men: “the study of men born in 1913”. Arch Intern Med. September 13 1999;159(16):1886–1890. [DOI] [PubMed] [Google Scholar]
- 126.Eichinger S, Hron G, Bialonczyk C, et al. Overweight, obesity, and the risk of recurrent venous thromboembolism. Arch Intern Med. August 11 2008;168(15):1678–1683. [DOI] [PubMed] [Google Scholar]
- 127.Rodger MA, Kahn SR, Wells PS, et al. Identifying unprovoked thromboembolism patients at low risk for recurrence who can discontinue anticoagulant therapy. CMAJ. August 26 2008;179(5):417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Writing Group M, Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. January 26 2016;133(4):e38–360. [DOI] [PubMed] [Google Scholar]
- 129.Regitz-Zagrosek V, Kararigas G. Mechanistic Pathways of Sex Differences in Cardiovascular Disease. Physiol Rev. January 2017;97(1):1–37. [DOI] [PubMed] [Google Scholar]
- 130.Vilahur G, Ben-Aicha S, Badimon L. New insights into the role of adipose tissue in thrombosis. Cardiovasc Res. July 1 2017;113(9):1046–1054. [DOI] [PubMed] [Google Scholar]
- 131.Schafer K, Konstantinides S. Adipokines and thrombosis. Clin Exp Pharmacol Physiol. December 2011;38(12):864–871. [DOI] [PubMed] [Google Scholar]
- 132.Wilkerson WR, Sane DC. Aging and thrombosis. Semin Thromb Hemost. December 2002;28(6):555–568. [DOI] [PubMed] [Google Scholar]
- 133.Allman-Farinelli MA. Obesity and venous thrombosis: a review. Semin Thromb Hemost. November 2011;37(8):903–907. [DOI] [PubMed] [Google Scholar]
- 134.Dellas C, Schafer K, Rohm I, et al. Absence of leptin resistance in platelets from morbidly obese individuals may contribute to the increased thrombosis risk in obesity. Thromb Haemost. December 2008;100(6):1123–1129. [PubMed] [Google Scholar]
- 135.Nakata M, Yada T, Soejima N, Maruyama I. Leptin promotes aggregation of human platelets via the long form of its receptor. Diabetes. February 1999;48(2):426–429. [DOI] [PubMed] [Google Scholar]
- 136.Konstantinides S, Schafer K, Koschnick S, Loskutoff DJ. Leptin-dependent platelet aggregation and arterial thrombosis suggests a mechanism for atherothrombotic disease in obesity. J Clin Invest. November 2001;108(10):1533–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Corsonello A, Malara A, Ientile R, Corica F. Leptin enhances adenosine diphosphate-induced platelet aggregation in healthy subjects. Obes Res. April 2002;10(4):306. [DOI] [PubMed] [Google Scholar]
- 138.Konstantinides S, Schafer K, Neels JG, Dellas C, Loskutoff DJ. Inhibition of endogenous leptin protects mice from arterial and venous thrombosis. Arterioscler Thromb Vasc Biol. November 2004;24(11):2196–2201. [DOI] [PubMed] [Google Scholar]
- 139.Ozata M, Avcu F, Durmus O, Yilmaz I, Ozdemir IC, Yalcin A. Leptin does not play a major role in platelet aggregation in obesity and leptin deficiency. Obes Res. October 2001;9(10):627–630. [DOI] [PubMed] [Google Scholar]
- 140.Corsonello A, Perticone F, Malara A, et al. Leptin-dependent platelet aggregation in healthy, overweight and obese subjects. Int J Obes Relat Metab Disord. May 2003;27(5):566–573. [DOI] [PubMed] [Google Scholar]
- 141.Corica F, Corsonello A, Perticone F. Effects of leptin on platelet function in obese patients. JAMA. July 17 2002;288(3):313–314; author reply 314. [DOI] [PubMed] [Google Scholar]
- 142.Wallaschofski H, Kobsar A, Sokolova O, et al. Differences in platelet activation by prolactin and leptin. Horm Metab Res. July 2004;36(7):453–457. [DOI] [PubMed] [Google Scholar]
- 143.Chu NF, Spiegelman D, Hotamisligil GS, Rifai N, Stampfer M, Rimm EB. Plasma insulin, leptin, and soluble TNF receptors levels in relation to obesity-related atherogenic and thrombogenic cardiovascular disease risk factors among men. Atherosclerosis. August 2001;157(2):495–503. [DOI] [PubMed] [Google Scholar]
- 144.Singh P, Peterson TE, Barber KR, et al. Leptin upregulates the expression of plasminogen activator inhibitor-1 in human vascular endothelial cells. Biochem Biophys Res Commun. January 29 2010;392(1):47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Cushman M, Yanez D, Psaty BM, et al. Association of fibrinogen and coagulation factors VII and VIII with cardiovascular risk factors in the elderly: the Cardiovascular Health Study. Cardiovascular Health Study Investigators. Am J Epidemiol. April 1 1996;143(7):665–676. [DOI] [PubMed] [Google Scholar]
- 146.Rosito GA, D’Agostino RB, Massaro J, et al. Association between obesity and a prothrombotic state: the Framingham Offspring Study. Thromb Haemost. April 2004;91(4):683–689. [DOI] [PubMed] [Google Scholar]
- 147.Ay L, Kopp HP, Brix JM, et al. Thrombin generation in morbid obesity: significant reduction after weight loss. J Thromb Haemost. April 2010;8(4):759–765. [DOI] [PubMed] [Google Scholar]
- 148.Samad F, Pandey M, Loskutoff DJ. Regulation of tissue factor gene expression in obesity. Blood. December 1 2001;98(12):3353–3358. [DOI] [PubMed] [Google Scholar]
- 149.Napoleone E, DIS A, Amore C, et al. Leptin induces tissue factor expression in human peripheral blood mononuclear cells: a possible link between obesity and cardiovascular risk? J Thromb Haemost. July 2007;5(7):1462–1468. [DOI] [PubMed] [Google Scholar]
- 150.Rafail S, Ritis K, Schaefer K, et al. Leptin induces the expression of functional tissue factor in human neutrophils and peripheral blood mononuclear cells through JAK2-dependent mechanisms and TNFalpha involvement. Thromb Res. 2008;122(3):366–375. [DOI] [PubMed] [Google Scholar]
- 151.Mertens I, Van Gaal LF. Obesity, haemostasis and the fibrinolytic system. Obes Rev. May 2002;3(2):85–101. [DOI] [PubMed] [Google Scholar]
- 152.Pandolfi A, Iacoviello L, Capani F, Vitacolonna E, Donati MB, Consoli A. Glucose and insulin independently reduce the fibrinolytic potential of human vascular smooth muscle cells in culture. Diabetologia. December 1996;39(12):1425–1431. [DOI] [PubMed] [Google Scholar]
- 153.Murakami T, Horigome H, Tanaka K, et al. Impact of weight reduction on production of platelet-derived microparticles and fibrinolytic parameters in obesity. Thromb Res. 2007;119(1):45–53. [DOI] [PubMed] [Google Scholar]
- 154.Shimomura I, Funahashi T, Takahashi M, et al. Enhanced expression of PAI-1 in visceral fat: possible contributor to vascular disease in obesity. Nat Med. July 1996;2(7):800–803. [DOI] [PubMed] [Google Scholar]
- 155.Samad F, Loskutoff DJ. Tissue distribution and regulation of plasminogen activator inhibitor-1 in obese mice. Mol Med. September 1996;2(5):568–582. [PMC free article] [PubMed] [Google Scholar]
- 156.Folsom AR, Qamhieh HT, Wing RR, et al. Impact of weight loss on plasminogen activator inhibitor (PAI-1), factor VII, and other hemostatic factors in moderately overweight adults. Arterioscler Thromb. February 1993;13(2):162–169. [DOI] [PubMed] [Google Scholar]
- 157.Marckmann P, Toubro S, Astrup A. Sustained improvement in blood lipids, coagulation, and fibrinolysis after major weight loss in obese subjects. Eur J Clin Nutr. May 1998;52(5):329–333. [DOI] [PubMed] [Google Scholar]
- 158.Molins B, Pena E, Vilahur G, Mendieta C, Slevin M, Badimon L. C-reactive protein isoforms differ in their effects on thrombus growth. Arterioscler Thromb Vasc Biol. December 2008;28(12):2239–2246. [DOI] [PubMed] [Google Scholar]
- 159.Danenberg HD, Szalai AJ, Swaminathan RV, et al. Increased thrombosis after arterial injury in human C-reactive protein-transgenic mice. Circulation. August 5 2003;108(5):512–515. [DOI] [PubMed] [Google Scholar]
- 160.Grad E, Danenberg HD. C-reactive protein and atherothrombosis: Cause or effect? Blood Rev. January 2013;27(1):23–29. [DOI] [PubMed] [Google Scholar]
- 161.Hankey CR, Rumley A, Lowe GD, Woodward M, Lean ME. Moderate weight reduction improves red cell aggregation and factor VII activity in overweight subjects. Int J Obes Relat Metab Disord. August 1997;21(8):644–650. [DOI] [PubMed] [Google Scholar]
- 162.Davi G, Guagnano MT, Ciabattoni G, et al. Platelet activation in obese women: role of inflammation and oxidant stress. JAMA. October 23–30 2002;288(16):2008–2014. [DOI] [PubMed] [Google Scholar]
- 163.De Pergola G, Pannacciulli N, Coviello M, et al. sP-selectin plasma levels in obesity: association with insulin resistance and related metabolic and prothrombotic factors. Nutr Metab Cardiovasc Dis. March 2008;18(3):227–232. [DOI] [PubMed] [Google Scholar]
- 164.Nishimura S, Manabe I, Nagasaki M, et al. In vivo imaging in mice reveals local cell dynamics and inflammation in obese adipose tissue. J Clin Invest. February 2008;118(2):710–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yaron G, Brill A, Dashevsky O, et al. C-reactive protein promotes platelet adhesion to endothelial cells: a potential pathway in atherothrombosis. Br J Haematol. August 2006;134(4):426–431. [DOI] [PubMed] [Google Scholar]
- 166.Gulcan M, Varol E, Etli M, Aksoy F, Kayan M. Mean platelet volume is increased in patients with deep vein thrombosis. Clin Appl Thromb Hemost. July 2012;18(4):427–430. [DOI] [PubMed] [Google Scholar]
- 167.Cil H, Yavuz C, Islamoglu Y, et al. Platelet count and mean platelet volume in patients with in-hospital deep venous thrombosis. Clin Appl Thromb Hemost. November 2012;18(6):650–653. [DOI] [PubMed] [Google Scholar]
- 168.Coban E, Ozdogan M, Yazicioglu G, Akcit F. The mean platelet volume in patients with obesity. Int J Clin Pract. August 2005;59(8):981–982. [DOI] [PubMed] [Google Scholar]
- 169.Bordeaux BC, Qayyum R, Yanek LR, et al. Effect of obesity on platelet reactivity and response to low-dose aspirin. Prev Cardiol. Spring 2010;13(2):56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tamminen M, Lassila R, Westerbacka J, Vehkavaara S, Yki-Jarvinen H. Obesity is associated with impaired platelet-inhibitory effect of acetylsalicylic acid in nondiabetic subjects. Int J Obes Relat Metab Disord. August 2003;27(8):907–911. [DOI] [PubMed] [Google Scholar]
- 171.Hanzu FA, Palomo M, Kalko SG, et al. Translational evidence of endothelial damage in obese individuals: inflammatory and prothrombotic responses. J Thromb Haemost. June 2011;9(6):1236–1245. [DOI] [PubMed] [Google Scholar]
- 172.Marseglia L, Manti S, D’Angelo G, et al. Oxidative stress in obesity: a critical component in human diseases. Int J Mol Sci. December 26 2014;16(1):378–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lentz SR. Thrombosis in the setting of obesity or inflammatory bowel disease. Blood. November 17 2016;128(20):2388–2394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


