To the Editor:
Percutaneous and surgical tracheostomy is safe in critically ill patients requiring prolonged mechanical ventilation (1–3). However, existing trial data are inconclusive regarding the optimal timing of tracheostomy (4, 5). This uncertainty has grown during the coronavirus disease (COVID-19) pandemic (6). Guidelines have recommended that tracheostomy be delayed later than most “late tracheostomy” arms of recent trials (1, 5, 7–12). This delay arises from uncertainty of patient benefit as well as concern for healthcare workers during aerosol-generating procedures (5, 13). It may be more challenging to sedate or achieve ventilator synchrony in the relatively younger, less comorbid populations with COVID-19 (14). We reviewed our institution’s experience with patients with COVID-19 undergoing tracheostomy placement at the discretion of the attending intensivist, to evaluate whether tracheostomy was associated with a reduction in sedation and analgesia administration.
Methods
Patients were included if they were at least 18 years of age, were positive for COVID-19 on a reverse transcriptase–polymerase chain reaction severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) test, and did not have another indication for deep sedation. The timing of tracheostomy was determined by the attending intensivist. Data were collected for the day of tracheostomy and 5 days before and after the procedure by two independent trained data abstractors blinded to each other’s results; differences were reconciled. Drug dosages were obtained by a pharmacist via electronic data abstraction. Opioids included fentanyl, oxycodone, morphine, and hydromorphone. Opioid doses were converted into intravenous fentanyl equivalents (100 mcg [0.1 mg] i.v. fentanyl = 1.5 mg i.v. hydromorphone = 5 mg oral hydromorphone = 20 mg oxycodone = 30 mg oral morphine = 10 mg i.v. morphine). Statistical analysis was done in Stata 16.1 (Code is in Appendix in the online supplement). Comparisons between before and after tracheostomy were implemented with multilevel regression with daily measurements nested within patient (e.g., using xtreg, fe for continuous outcomes and xtlogit, fe for dichotomous outcomes), with day of procedure omitted. Analyses controlling for change over time before tracheostomy were implemented as marginal spline testing for difference in slope before versus after tracheostomy.
This study was a quality improvement project; retrospective approval was received from the University of Michigan Institutional Review Board (HUM00184067) to disseminate these results.
Results
The first 28 tracheostomies were performed on patients with COVID-19 at the University of Michigan between April 12 and April 28, 2020. During that time, 131 patients received mechanical ventilation and were COVID-19 positive at the same hospital. Twenty-one of the 28 tracheostomies were performed percutaneously, and 7 surgically. Three patients had other indications for deep sedation (one with an intracranial hemorrhage and two with refractory seizures) and were excluded from this analysis; 25 patients were included in the final analysis. Mean age at tracheostomy was 56 (range 26–89), 60% were male, and patients were intubated for a mean of 22 days at the time of tracheostomy (range 8–31). The intensive care unit (ICU) and hospital length of stay median (mean ± standard deviation [SD]) for the cohort were 30 (33.12 ± 9.77) and 51 (54.4 ± 20.4) days, respectively.
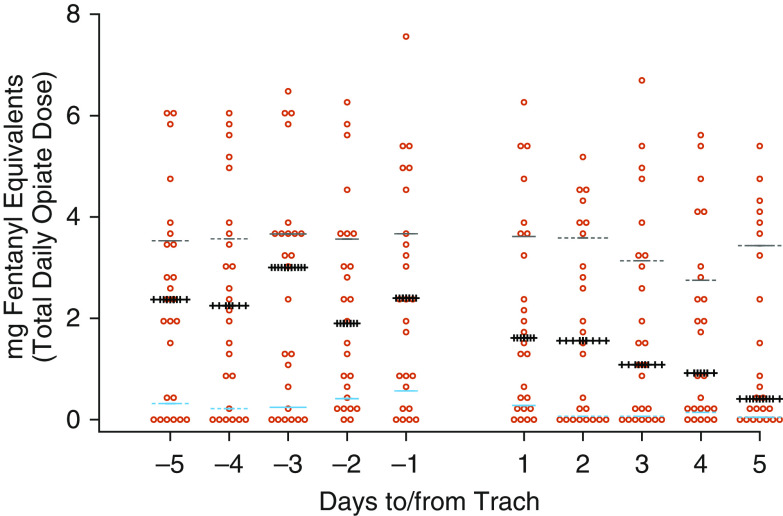
Patients who underwent tracheostomy received a median (mean ± SD) of 3 (3.5 ± 2.0) different classes of sedatives in the 5 days before percutaneous tracheostomy and received a median (mean ± SD) of 2.4 (2.4 ± 2.0) mg of total fentanyl equivalents per day. Following tracheostomy, the median (mean ± SD) fentanyl equivalents administered decreased to 1.1 (1.8 ± 1.9) mg of total fentanyl equivalents per day. (Figure 1 shows individual fentanyl equivalent dosing per day.) The estimated drop of mean fentanyl equivalents was significant in within-person paired testing following tracheostomy (estimated mean drop 0.56 mg fentanyl equivalent per day, 95% confidence interval [95% CI], 0.32–0.81; P < 0.001).
Figure 1.
Fentanyl equivalents before and after tracheostomy placement. The median is indicated by the crosses; the dashed lines indicate the 25th and 75th percentiles. Trach = tracheostomy.
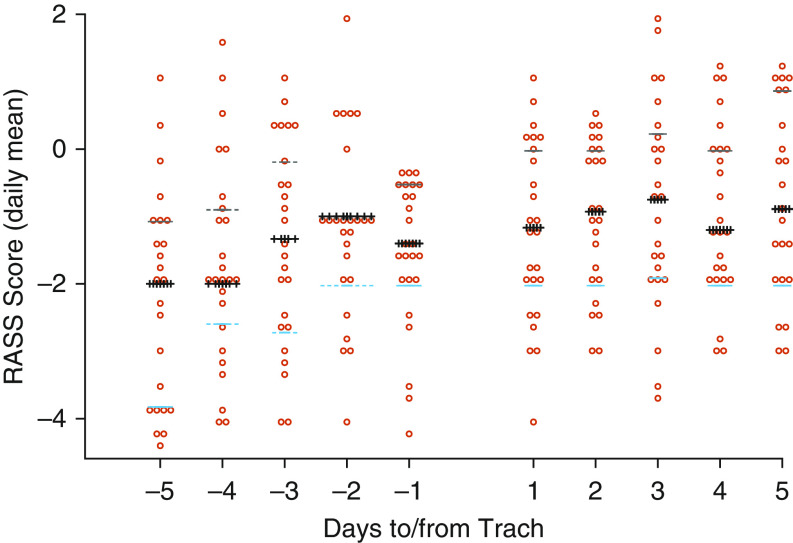
During the 5 days before tracheostomy placement, bedside nurses evaluated the median (mean ± SD) Richmond Agitation-Sedation Scale (RASS) score as −1.5 (−1.6 ± 1.4) (Figure 2). Sixty-seven percent of patient-days had no recorded levels of “coma” (−4 or below), and 6% had at least one recorded “agitated” level (+4 or above). Three percent of patient-days included a physical therapy session. Spontaneous breathing trials were attempted in 22% of patient-days before tracheostomy.
Figure 2.
RASS scores before and after tracheostomy placement. The median is indicated by the crosses; the dashed lines indicate the 25th and 75th percentiles. RASS = Richmond Agitation-Sedation Score; Trach = tracheostomy.
In contrast, during the 5 days after tracheostomy, the median (mean ± SD) RASS score rose to −1.0 (−1.0 ± 1.3), and 92% of patient-days had no recorded levels of coma. Fourteen percent of patient-days after tracheostomy had periods without delirium, and 1% had a recorded agitated level. In within-person paired analyses, mean RASS scores rose 0.61 (95% CI, 0.32–0.90; P < 0.001), as did the odds of being coma-free (odds ratio [OR], 3.4; 95% CI, 1.9–6.0) and of receiving physical therapy (OR, 7.2; 95% CI, 2.1–24.2; P = 0.002), but not days without agitation defined as RASS score of +4 or +5 (OR, 0.72; 95% CI, 0.32–1.60; P = 0.42). Fifteen percent of patient-days included a physical therapy session, and 43% of patient-days included a spontaneous breathing trial.
In regression analyses controlled for linear trend across the 5 days before tracheostomy, there were no statistically significant differences following tracheostomy in fentanyl equivalents or RASS score. However, estimates were imprecisely estimated so differences cannot be ruled out (Table 1).
Table 1.
Multivariable fixed effects regression
| Outcomes | Immediate Change |
Change in Slope (per Day) |
||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI Lower | 95% CI Upper | P Value | Estimate | 95% CI Lower | 95% CI Upper | P Value | |
| Fentanyl equivalents | −0.27 | −0.85 | 0.31 | 0.359 | −0.10 | −0.28 | 0.07 | 0.246 |
| RASS | −0.25 | −0.92 | 0.42 | 0.460 | −0.09 | −0.29 | 0.11 | 0.395 |
| Odds Ratio | 95% CI Lower | 95% CI Upper | P Value | Odds Ratio | 95% CI Lower | 95% CI Upper | P Value | |
|---|---|---|---|---|---|---|---|---|
| No coma | 1.11 | 0.30 | 4.07 | 0.878 | 1.35 | 0.91 | 2.02 | 0.139 |
| Participation in physical therapy | 17.50 | 0.53 | 575.46 | 0.108 | 1.90 | 0.75 | 4.80 | 0.173 |
Definition of abbreviations: CI = confidence interval; RASS = Richmond Agitation-Sedation Score.
Discussion
Our study shows an association between placement of tracheostomy and decrease in opioid use, as well as improvement in mental status as measured by RASS score, increased participation in physical therapy, and an increase in days with attempted spontaneous breathing trials. This aligns with theoretical benefits of tracheostomy over translaryngeal intubation, such as decreased pulmonary infections, sedation requirements, days of mechanical ventilation, and total ICU days (15, 16).
Timing of tracheostomy has been complicated during COVID-19, when ICU beds and supplies have been limited. It has also been noted that younger, healthier patients with COVID-19 pneumonia have received higher doses and multiple agents to achieve sedation and synchrony (14). Owing to personal protective equipment requirements and increased time and effort to enter isolation rooms, providers may less frequently titrate sedative infusions. Efforts should be made to minimize sedation requirements despite the challenges of COVID-19, as that remains best practice. Tracheostomy may facilitate this but should be considered with multiple other strategies.
Supplementary Material
Footnotes
Supported by U.S. National Institutes of Health T32 HL007749 and K12 HL138039. This material is the result of work supported with resources and use of facilities at the Ann Arbor Veterans Affairs Medical Center. This work does not necessarily represent the views of the U.S. Government or Department of Veterans Affairs.
This letter has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Hess DR, Altobelli NP. Tracheostomy tubes. Respir Care. 2014;59:956–971. doi: 10.4187/respcare.02920. [Discussion, pp. 971–973.] [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM. Early tracheostomy for primary airway management in the surgical critical care setting. Surgery. 1990;108:655–659. [PubMed] [Google Scholar]
- 3.Stock MC, Woodward CG, Shapiro BA, Cane RD, Lewis V, Pecaro B. Perioperative complications of elective tracheostomy in critically ill patients. Crit Care Med. 1986;14:861–863. doi: 10.1097/00003246-198610000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Marsh HM, Gillespie DJ, Baumgartner AE. Timing of tracheostomy in the critically ill patient. Chest. 1989;96:190–193. doi: 10.1378/chest.96.1.190. [DOI] [PubMed] [Google Scholar]
- 5.Wang F, Wu Y, Bo L, Lou J, Zhu J, Chen F, et al. The timing of tracheotomy in critically ill patients undergoing mechanical ventilation: a systematic review and meta-analysis of randomized controlled trials. Chest. 2011;140:1456–1465. doi: 10.1378/chest.11-2024. [DOI] [PubMed] [Google Scholar]
- 6.Lamb CR, Desai NR, Angel L, Chaddha U, Sachdeva A, Sethi S, et al. Use of tracheostomy during the COVID-19 pandemic: American College of Chest Physicians/American Association for Bronchology and Interventional Pulmonology/Association of Interventional Pulmonology Program Directors Expert Panel Report. Chest. 2020;158:1499–1514. doi: 10.1016/j.chest.2020.05.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Academy of Otolaryngology and Head and Neck Surgery. AAO position statement: tracheotomy recommendations during the COVID-19 pandemic. 2020 [accessed 2020 Jul 3]. Available from: https://www.entnet.org/ content/aao-position-statement-tracheotomy-recommendations -during-covid-19-pandemic.
- 8.Canadian Society of Otolaryngology-Head and Neck Surgery. Recommendations from the CSO-HNS Taskforce on performance of tracheotomy during the COVID-19 pandemic. 2020 doi: 10.1186/s40463-020-00414-9. [accessed 2020 Jul 3]. Available from: https://www.entcanada.org/wp-content/uploads/COVID-19-Guidelines -CSOHNS-Task-Force-Mar-23–2020.pdf. [DOI] [PMC free article] [PubMed]
- 9.Bittner EA, Schmidt UH. The ventilator liberation process: update on technique, timing, and termination of tracheostomy. Respir Care. 2012;57:1626–1634. doi: 10.4187/respcare.01914. [DOI] [PubMed] [Google Scholar]
- 10.Terragni PP, Antonelli M, Fumagalli R, Faggiano C, Berardino M, Pallavicini FB, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA. 2010;303:1483–1489. doi: 10.1001/jama.2010.447. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330:1243. doi: 10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275:679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 13.McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717–725. doi: 10.1016/S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanidziar D, Bittner EA. Sedation of mechanically ventilated COVID-19 patients: challenges and special considerations. Anesth Analg. 2020;131:e40–e41. doi: 10.1213/ANE.0000000000004887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trouillet J-L, Luyt C-E, Guiguet M, Ouattara A, Vaissier E, Makri R, et al. Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: a randomized trial. Ann Intern Med. 2011;154:373–383. doi: 10.7326/0003-4819-154-6-201103150-00002. [DOI] [PubMed] [Google Scholar]
- 16.Breckenridge SJ, Chlan L, Savik K. Impact of tracheostomy placement on anxiety in mechanically ventilated adult ICU patients. Heart Lung. 2014;43:392–398. doi: 10.1016/j.hrtlng.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.