Abstract
Rationale: During the coronavirus disease (COVID-19) pandemic, many intensive care units (ICUs) have shifted communication with patients’ families toward chiefly telehealth methods (phone and video) to reduce COVID-19 transmission. Family and clinician perspectives about phone and video communication in the ICU during the COVID-19 pandemic are not yet well understood. Increased knowledge about clinicians’ and families’ experiences with telehealth may help to improve the quality of remote interactions with families during periods of hospital visitor restrictions during COVID-19.
Objectives: To explore experiences, perspectives, and attitudes of family members and ICU clinicians about phone and video interactions during COVID-19 hospital visitor restrictions.
Methods: We conducted a qualitative interviewing study with an intentional sample of 21 family members and 14 treating clinicians of cardiothoracic and neurologic ICU patients at an academic medical center in April 2020. Semistructured qualitative interviews were conducted with each participant. We used content analysis to develop a codebook and analyze interview transcripts. We specifically explored themes of effectiveness, benefits and limitations, communication strategies, and discordant perspectives between families and clinicians related to remote discussions.
Results: Respondents viewed phone and video communication as somewhat effective but inferior to in-person communication. Both clinicians and families believed phone calls were useful for information sharing and brief updates, whereas video calls were preferable for aligning clinician and family perspectives. Clinicians and families expressed discordant views on multiple topics—for example, clinicians worried they were unsuccessful in conveying empathy remotely, whereas families believed empathy was conveyed successfully via phone and video. Communication strategies suggested by families and clinicians for remote interactions include identifying a family point person to receive updates, frequently checking family understanding, positioning the camera on video calls to help family see the patient and their clinical setting, and offering time for the family and patient to interact without clinicians participating.
Conclusions: Telehealth communication between families and clinicians of ICU patients appears to be a somewhat effective alternative when in-person communication is not possible. Use of communication strategies specific to phone and video can improve clinician and family experiences with telehealth.
Keywords: telehealth, COVID-19 pandemic, intensive care, critical care, qualitative research
Over the last decade, there has been a greater focus on family-centered care in intensive care units (ICUs) (1). Families are increasingly encouraged to attend rounds, be present at the bedside, and participate in in-person interdisciplinary family meetings (1, 2). Close communication with families of ICU patients has been shown to improve psychological outcomes in families (3) and lead to higher-quality surrogate decision-making (4).
During the current pandemic of coronavirus disease (COVID-19), hospitals worldwide have imposed visitor restrictions in an effort to reduce transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (5, 6). In many ICUs, clinical communication and visitation have shifted from in-person and bedside discussions toward exclusively remote interactions via telephone or video call (5). These changes have received considerable attention in both the lay press and medical journals, especially regarding families’ inability to be at the bedside with gravely ill loved ones (7–10). Concern has been expressed over the potential dehumanizing and stressful effects on patients, families, and clinicians (7–10). Although institutions have developed remote alternatives to traditional visitation and communication (11), little is known about clinicians’ and families’ perceptions of this approach. We explored experiences, perspectives, and attitudes of family members and ICU clinicians about using phone and video as the primary means of family–clinician communication during COVID-19 visitor restrictions (Figure 1).
Figure 1.
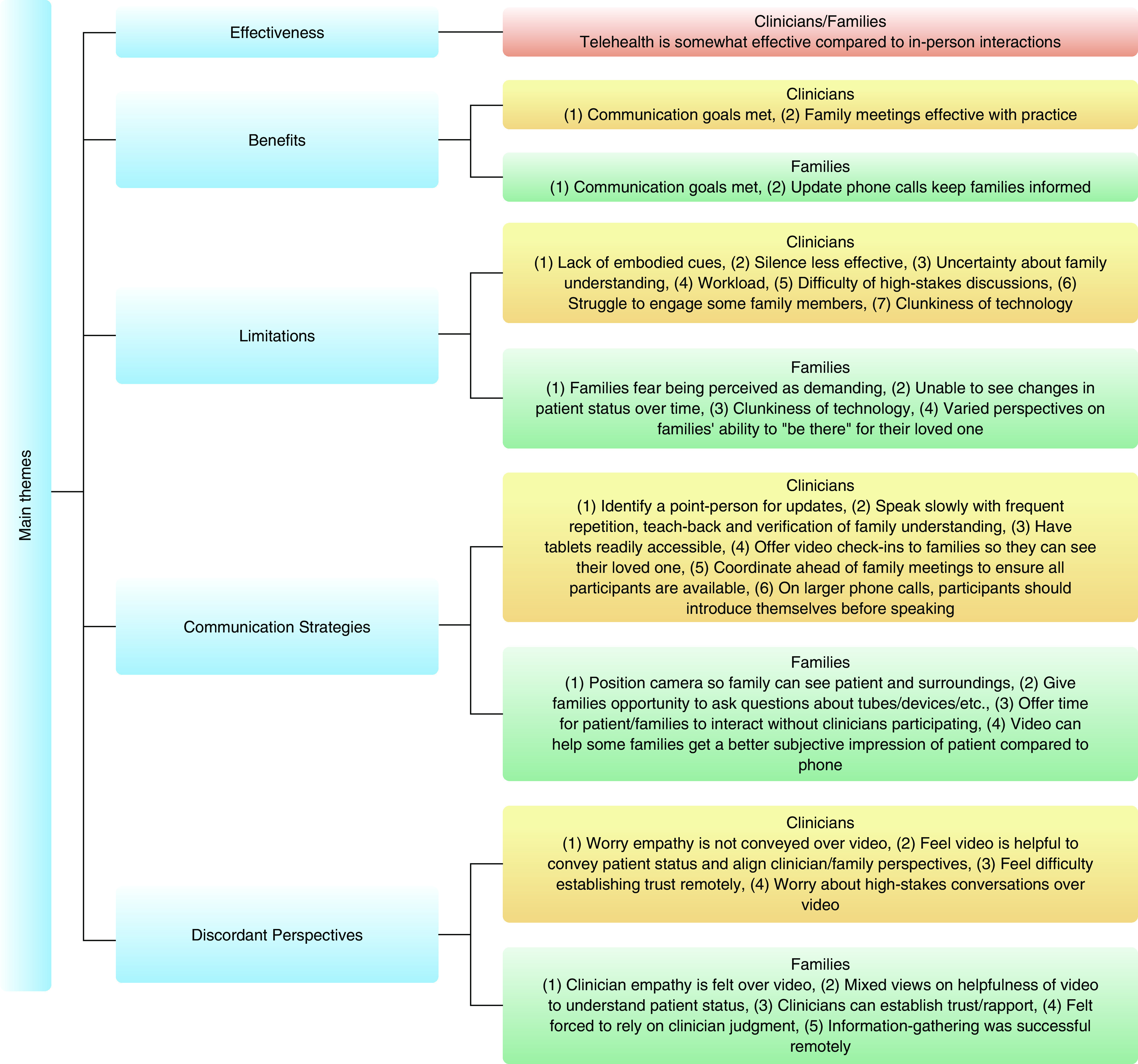
Main perspectives of families and clinicians about the use of remote communication (phone and video) in intensive care units during the coronavirus disease (COVID-19) pandemic.
Methods
Setting
This study was deemed exempt by the University of Pittsburgh Human Research Protection Office. We enrolled participants during April 2020 from three ICUs at a single large academic medical center in southwestern Pennsylvania. These included a 10-bed neurotrauma ICU, a 16-bed neurovascular ICU, and a 20-bed cardiothoracic ICU. During the study period, all three units admitted patients undergoing evaluation for SARS-CoV2 infection, but only the cardiothoracic ICU continued to care for patients with confirmed infection. Each unit is staffed with a separate multidisciplinary critical care team including an attending physician, fellow(s), and residents and a nurse with training in communication and family support (12). During the study period, no family visitation was permitted within the ICU except in the case of actively dying patients receiving only comfort-oriented care, for whom two visitors were permitted. During this time, clinical staff within each participating ICU engaged patients’ families in telehealth communication at their discretion.
Participants
We used an intentional sampling strategy aimed at maximizing the diversity of family experience. We identified target ICUs for recruitment and asked nurses daily for referrals. Specifically, we asked them to identify family members who might be willing to speak with a researcher about their experiences with ICU communication. Nurse specialists identified families of patients who they believed would offer unique or informative perspectives on communication and asked for their willingness to participate in this research. We gave these nurses discretion to approach families based on their gestalt of family members’ emotional states, potential therapeutic benefit to an individual family member of sharing their experience with researchers, recent communications from the care team, and willingness to participate in the study. If a nurse believed that a family member would not be a good candidate for the study at a given time, we did not approach them to participate unless the nurse later indicated that one of these factors had changed. When potential participants were identified, we asked the bedside nurse caring for the patient that day to ask for their willingness to discuss participation in a research study, and then asked the nurse if he or she was willing to participate. We contacted families who agreed to participation by phone and obtained verbal informed consent for participation before conducting interviews. Each participant explicitly gave permission for the interview to be audiotaped. We then identified the clinician counterpart(s) in communication and obtained their assent to participate. We recruited clinicians involved in communication with family participants and interviewed them as well. We enrolled participants until achieving thematic saturation.
Interviews
We conducted semistructured qualitative interviews by telephone. We used an interview guide (Appendix 1) to solicit open-ended answers about family and clinician experiences using phone and video as primary communication methods. The interview guide allows for consistency between interviews while facilitating targeted exploration of participants’ responses and is commonly used in qualitative interviewing (13). In addition, we asked clinicians and family members to rate the effectiveness of their phone and video conversations on a scale of 1–10, in which 1 = “ineffective” and 10 = “equally effective as in-person.” Families who never participated in video calls were only asked questions about phone interactions. Clinicians and families also rated their concerns about the privacy of their remote conversations on a scale of 1–10, in which 1 = “not concerned about privacy” and 10 = “extremely concerned about privacy” (Table E1). Family members rated their comfort with technology on a scale of 1–10, in which 1 = “not comfortable with technology” and 10 = “extremely comfortable with technology” (Table 1).
Table 2.
Patient demographic and clinical characteristics
| Characteristic | Patients (n = 21) |
|---|---|
| Sex, F, n (%) | 9 (43) |
| Age, mean (SD), yr | 63 (19) |
| Race, n (%) | |
| White | 15 (71) |
| Black | 1 (5) |
| Native American | 1 (5) |
| Declined to answer | 4 (19) |
| Admission diagnosis, n (%) | |
| Neurologic injury | 14 (67) |
| Cardiac arrest | 3 (14) |
| Lung transplant | 1 (5) |
| COVID-19 | 1 (5) |
| Drug overdose | 1 (5) |
| Gastrointestinal bleeding | 1 (5) |
| Clinical condition on day of interview, n (%) | |
| Mechanically ventilated | 15 (71) |
| Multisystem organ failure | 15 (71) |
| Vasopressor dependent | 5 (24) |
| Comatose | 5 (24) |
| Survived to hospital discharge, n (%) | 12 (57) |
| ICU length of stay, mean (SD), d | 9 (6) |
| Day of ICU stay at time of family interview, mean (SD) | 3 (3) |
Definition of abbreviations: COVID-19 = coronavirus disease; ICU = intensive care unit; SD = standard deviation.
Data and Analysis
We collected basic clinical and demographic data using REDCap, an electronic data capture tool hosted at the University of Pittsburgh (14, 15). We summarized these data using descriptive statistics. We used NVivo 12 software (QSR International) to analyze verbatim transcripts of telephone interviews with clinicians and families (16). We used a content analysis approach to develop a codebook to analyze the interviews (17). A single investigator (N.K.) coded all of the interview transcripts, and two other investigators (J.E. and A.S.) independently reviewed the coding for each transcript. Coding disagreements were resolved by discussion until consensus was achieved.
Results
Participant Characteristics
Of 22 family members and 19 clinicians directly contacted by the research team, 21 family members (95%) and 14 clinicians (74%) agreed to participate. We interviewed clinicians involved in communication with 17 of 21 participating family members. All patients about whom communication occurred were critically ill, and 9 of 21 (43%) died in the ICU (Table 2). Most family members were female (76%), were either the spouse (47%) or adult child (33%) of the patient, and were moderately comfortable with technology (mean, 7.1; standard deviation [SD], 2.3) (Table 1). All family members spoke with clinicians over the phone, and 11 of 21 (52%) interacted with the patient and at least one of their treating clinicians using video calls. At the time of the family interview, patients had been in the ICU for a mean of 3 days (SD, 3); the mean ICU stay for patients in the study, including patients who died in the ICU, was 9 days (SD, 6). Participating clinicians were a mix of attending physicians (n = 3 [21%]), residents and fellows (n = 8 [57%]), and nurses (n = 3 [21%]).
Table 1.
Characteristics of participating family members and clinicians
| Characteristic | Count |
|---|---|
| Family members | 21 |
| Sex, F, n (%) | 16 (76) |
| Age, mean (SD) | 56 (13.8) |
| Race, n (%) | |
| White | 20 (95) |
| Black | 1 (5) |
| Relationship to patient, n (%) | |
| Spouse | 10 (47) |
| Child | 7 (33) |
| Parent | 3 (14) |
| Sibling | 1 (5) |
| Education, n (%) | |
| High school graduate or less | 5 (24) |
| Associate’s degree/some college | 7 (33) |
| Bachelor’s degree or advanced degree | 9 (43) |
| Comfort with technology, mean (SD) | 7.1 (2.3) |
| Types of communication, n (%) | |
| Phone with clinicians | 21 (100) |
| Phone with patient | 1 (5) |
| Video with clinicians | 11 (52) |
| Video with patient | 11 (52) |
| Clinicians | 14 |
| Sex, F, n (%) | 5 (36) |
| Years in specialty, mean (range) | 7.4 (1–30) |
| Clinician type, n (%) | |
| Attending physician | 3 (21) |
| Fellow | 5 (36) |
| Resident | 3 (21) |
| Nurse | 3 (21) |
| Medical specialty, n* | |
| Critical care | 6 |
| Neurology | 3 |
| Emergency medicine | 3 |
| Other (anesthesia, medicine, surgery, or neurosurgery) | 4 |
Definition of abbreviation: SD = standard deviation.
The specialty count total for physicians is greater than the total of participating physicians because specialty count includes physicians with training in multiple specialties.
Effectiveness of Phone and Video Communication
Both families and clinicians believed that phone and video were somewhat effective compared with what they believed that an in-person conversation would have achieved (Table E1). Families rated the effectiveness of phone and video a mean of 7.0 (SD, 1.6) and 7.2 (SD, 1.8), respectively; clinicians rated phone and video a mean of 6.2 (SD, 2.2) and 6.6 (SD, 1.2), respectively. Neither group rated privacy as a high concern (mean, 1.1; SD, 0.4 for families and mean, 3.1; SD, 1.9 for clinicians).
Benefits and Limitations of Phone and Video Communication
Phone and video communication with families offers many benefits, including meeting goals of communication and conveying general impressions of the patient (Table 3). Broadly, clinicians believed that their communication goals could be met over phone and video interactions and that family meetings could be effective with practice. Families also reported meeting their communication goals and believed that update phone calls from clinicians were successful in keeping them informed. Video calling may be superior to phone in conveying general impressions of the patient to families and in aligning clinician and family perspectives about patient status. However, although families were all comfortable with phone calls, the opinions of family members about video calling were more mixed.
Table 3.
Benefits and limitations of telehealth-only communications with families of ICU patients
| Benefits and Limitations | Representative Quote |
|---|---|
| Benefits | |
| Goals of communications are often met | Patient’s husband: “I thought they answered all of our questions [on the phone] in a pretty concise manner that we were able to understand.” |
| Physician: “The end result [over the phone] I think was essentially as effective.” | |
| “Update” phone calls keep families informed | Patient’s daughter: “They've actually been calling me at shift change, saying ‘Hey, I'm your mom’s new nurse,’ giving me a little bit of updates.” |
| Larger family meetings can be effective with sufficient planning, practice, and effort to identify who is speaking | Patient’s wife: “When we did group meetings when the doctors would round. . .everybody would stay together, do the conversation together and be on the same page. I thought it was really helpful to have all those people involved.” |
| Nurse: “A lot of people were trying to talk and then they would stop. But everybody was like, those people were trying to talk at the same time and stuff together. . . .I feel like practice makes perfect.” | |
| Mixed | |
| Families’ self-perceived ability to “be there” for their loved one varies by family member and level of consciousness of patient | Patient’s son: “[Video] gave us the opportunity and whether he heard us or not, just kind of express how we feel and share our love for him. . .[but] you can't ever replace the sense of being there. . .absolutely we miss something.” |
| Patient’s daughter: “Seeing it just over a screen, I think would just be just much more horrible. And there is no comfort I can give her, that's just going to be etched in my mind.” | |
| Challenges | |
| Embodied cues are lacking | Physician: “I think the ability to read people’s emotions and faces, and do things like therapeutic touch, are things we still lose a little bit to video.” |
| Silence cannot be used as effectively | Physician: “Silence is harder to deal with over the phone. . .Silence in person often leads the conversation along and you get to more interesting places, but silence over the phone just begets more silence.” |
| Clinicians are uncertain about family understanding | Physician: “It was difficult to pick up on family cues, like to get a real sense of understanding or to see where there was a real emotional response as opposed to a cognitive response.” |
| High-stakes discussions are difficult | Physician: “The family meetings, where you're like, ‘things are going poorly and we may need to change our strategy,’ like the bad news delivery meetings are much harder over the phone. You can't see somebody to tell if they're ready for you to keep going yet.” |
| Some clinicians felt telehealth added to their workload | Physician: “[In the ICU], it's added [work] in some ways in that you're calling everyone after seeing everyone when they're on rounds. . .” |
| Families fear they may be perceived as demanding | Patient’s husband: “I asked them how many times a day I could call for updates. I didn't want to be a pest…” |
| Clinicians feel they struggle to engage some family members | Physician: “. . .it's easy for one family member to take a back seat in a passive role and not really say anything. And it's difficult to probe them as much as if they were sitting there in front of me.” |
| Family is unable to see changes in patient status over time | Patient’s daughter: “[On FaceTime] we just had that little snippet of time, and that's a 5-min window out of a 24-h day. . . we're not seeing any little changes because we're not there to physically be with mother.” |
| “Clunkiness” and technical difficulties are uncomfortable and can interfere with communication | Patient’s wife: “I find that [phone] was. . .harder. Sometimes I didn't catch something. . .And sometimes the voice would go lower or higher. I think in person is a lot better than over the phone.” |
| Patient’s daughter: “[Sometimes] it was a little shaky [over video], but nothing that was distracting.” |
Definition of abbreviation: ICU = intensive care unit.
Both clinicians and families reported that communicating exclusively through telehealth had a number of drawbacks. The main limitations from the clinician perspective involved difficulties inherent to the phone and video media; for example, a dearth of embodied cues over the phone may result in trouble using silence effectively, uncertainty about family understanding of information shared, and difficulty having high-stakes discussions. Though video calls provide more information about facial expressions, there is still a comparative lack of nonverbal information and an inability to use body language to amplify messaging when compared with in-person conversations. Other common issues with telehealth can be ameliorated through active planning by the care team. For example, setting expectations at the beginning of an ICU stay for the frequency of check-ins can mitigate family concerns about being perceived as demanding. For their part, families expressed a number of concerns about exclusively communicating through phone and video, including fears of being seen as demanding, having limited ability to see changes in their loved one’s status and “be there” for their loved one, and concerns about the “clunkiness” of technology.
Suggested Communication Strategies
Most clinicians believed that conversations over phone and video calls took longer and required extra steps (Table 4). Before telehealth family meetings, ensuring technology availability and effectively coordinating with families and consulting clinicians facilitated successful interactions. Making minor changes in conversational mechanics (i.e., reintroducing clinicians before speaking on large calls and positioning the video to see the patient’s room) improved conversations.
Table 4.
Suggested communication strategies for clinicians using exclusively telehealth to communicate with families of ICU patients
| Communication Strategy | Representative Quote |
|---|---|
| General strategies | |
| Identify a point person who will receive clinical updates | Nurse: “[When you tell] one family member one thing in the morning, and then in the afternoon another family member calls, and something happened in that timeframe. . .there can be miscommunication. We've been trying to make sure that families have either one or two designated people that are calling to get updates to talk to us. . .because we don't want there to be a lot of confusion.” |
| Speak slowly and repeat what was previously discussed | Physician: “In terms of style . . . just taking it a lot slower. Leaving more time for pauses, questions . . . I think you have to be cognizant of the fact that these family discussions are probably going to take longer than they have in the past if you want to do them well. . . .” |
| Frequently check families’ understanding | Physician: “We definitely took extra steps to ask and re-ask if they understood what we were saying and have them say it back to us. . .more than when in person, when it's a little bit clearer to kind of judge looking at someone if they're really grasping what you're saying.” |
| Physician: “[There’s] much more deliberate checking in, hammering the point home, making sure that we're on the same page, that everything was understood.” | |
| Video calling | |
| Have tablet devices readily accessible | Physician: “I think the one thing that's helped is having iPads in the units. Initially we were using nurses' or physicians’ cell phones frequently. And now having iPads available, we can have folks join using the unit-based site that has worked better.” |
| Position camera so that family can see the patient and what is in the room | Patient’s daughter: “What I do like about what [the nurse] does. . .he’ll usually do an up-close shot of my mother's face so that we can see her and try and chat with her. But then he also kind of pulls back and kind of lets you kind of see how she’s situated in the room. Today was the first day they actually had her sitting up and so he kind of pulled back to show us that she was in a sitting position rather than laying down. . . .I thought that was pretty clever of him to not only just let us see her face, but then also to see the situation that she’s in and how they had her positioned. . . .” |
| Give family opportunity to ask questions about what they see (i.e., tubes and devices) | Patient’s son: “It’s always good to see the person [on video]. . .[the nurse] did a phenomenal job kind of explaining everything, showing tubes and all that sort of stuff.” |
| Offer time for patient/family member to interact without clinicians participating | Patient’s daughter: “I kind of liked that [the nurses] did not interact with us much because it was kind of like we were just in a room with [dad] and not other people like, ‘look at him do this, look at him do that. . . .’ We knew that they were there, but they didn't make it all obvious that they were there.” |
| Consider using video instead of phone calls for sharing subjective patient impressions and improving alignment between clinicians and families | Patient’s wife: “[To understand how her husband is] doing mood-wise. . .It's kind of hard, because the nurses don't necessarily know him as well as I do . . .to have them try to relay that information over the phone when he's not able to verbally communicate is hard. But, I feel like that was a little better this morning when I was able to FaceTime.” |
| Nurse: “If she really didn’t want aggressive care and that she sees her mom's getting all this aggressive care, maybe she’d be less likely to continue all this. . .versus over the phone where she can't see how much maybe all these things that we're doing for her mom is not what she wanted. . .using a video would help break that gap a little bit.” | |
| Offer a daily video check-in to families | Physician: “. . .have the nurses do a daily video chat where the family member can talk with a nurse over video, see the patient over video, ask questions about what they're seeing in the ICU room and that sort of thing. I think that added substantially to understanding when we have that element as well.” |
| Phone conferences | |
| Coordinate ahead of time to ensure that all participants are available | Physician: “Having a nurse to coordinate the timing of the conference is extremely important, especially when the family is not by the bedside. . . .[The nurse] made sure that everybody who needed to be in on the conversation was in on the conversation. . .it helped us maximize the recommendations we would give. . .and the prognostication we could do.” |
| To avoid confusion, each participant should introduce themselves at the start of the call and each time before speaking | Nurse: “When we first started doing it, we forgot to introduce everybody. . .[or] we introduced everybody, but then didn’t be like, ‘Hey, this is [name], again. . . .’ So, they just had this random voice talking at them, and sometimes it’s helpful to know, I think, if you're getting a nurse perspective, a doctor perspective, or an APP perspective, because they’re different.” |
Definition of abbreviations: APP = advanced practice provider; ICU = intensive care unit.
A number of clinicians expressed that telehealth conversations did not require entirely new communication strategies but rather the modification or additional emphasis of communication strategies they used regularly during in-person conversations. For example, one physician focused more deliberately on using teach-back methods, whereas another made a concerted effort to extend phone silences until a family member spoke.
Families’ main suggestions to improve communication during video and phone communication involved using technology to more closely approximate the experience of families’ being present at bedside. These suggestions included positioning the camera so that the family can see the patient and their surroundings, offering families the opportunity to ask questions about tubes and devices, and offering time for patients and families to interact without clinician participation.
Discordant Perspectives between Families and Clinicians
Family members and clinicians held a number of discordant opinions (Table 5). Many clinicians expressed worry about conveying empathy and establishing trust with families using telehealth. Families, however, typically felt that clinicians’ empathy was readily apparent and reported that they trusted the clinicians even without the ability to meet the clinicians in person. Not all participants held these views; one nurse believed that mistrust was fairly common in the ICU and not purely a telehealth problem, and a small number of family members expressed trepidation about not knowing whether their loved one was receiving the “best” care without meeting clinicians in person. Clinicians generally believed that video calling helped families understand their loved one’s clinical status, whereas families had varying opinions about the usefulness and acceptability of video to interact with their loved ones and physicians.
Table 5.
Discordant perspectives between clinicians and families about telehealth
| Clinician Perspectives | Family Perspectives |
|---|---|
| Communicating empathy over telehealth | |
| Clinicians worry about conveying empathy. | Empathy comes across regardless of medium. |
| Physician: “When the patient’s daughter broke down and cried and when it was harder. . .in real life I probably would’ve given a box of tissues. I would have given a pat on the shoulder. I would have demonstrated with probably my body language that I'm concerned. I could not do any of that.” | Patient’s daughter: “I feel like people who have more of a bedside manner, that still comes across well on the phone.” |
| Using video to convey an understanding of patient’s clinical status | |
| Clinicians felt video communication might help families to understand severity of illness. | Family preferences about using video to understand the patient’s status are mixed. |
| Nurse: “When she got to see him [over video], I think it helped her comprehension. . .she started to understand why he was having so much trouble breathing and getting out of the ICU. . . .Without the video she wouldn't have been able to do that.” | Patient’s daughter: “I think in person would be. . .I mean, it would be tragic and horrible in itself, but just seeing her through a screen like that would just be....You don’t Google horrid pictures of people. I definitely wouldn’t want to see that through a phone or computer screen.” |
| Nurse: “She thought we were neglecting him. . .or not telling her the full truth. So, when she got to see him [over video]. . .she started to understand why he was having so much trouble breathing and getting out of the ICU.” | Patient’s husband: “Her reactions to us [over FaceTime] were a definite sign that she has some abilities. Whereas the way they were describing that over the phone. . .the nurses said there was no response to their command....I surmised from their conversation it was worse than what it is.” |
| Trust and rapport between clinician and family | |
| Trust can be difficult to establish. | Clinicians can establish trust and rapport. |
| Physician: “[Over the phone], a lot of this came down to trust. There was a lot of questioning, concern....[The family] said some pretty rude things that implied that we didn’t care about the patient....Those things kind of seemed to go away once we met them in person.” | Patient’s husband: “Honestly I think it was better over the phone for some reason....It seemed like they felt bad they couldn't talk to us in person, so they really listened and they really, they never rushed us off the phone....The doctor was really, really good.” |
| Some clinicians feel awkward when there is no in-person relationship. | Families are generally less concerned about the impact of remote interactions with physicians. |
| Nurse: “I still interact with families on the phone every day, but it still feels weird and I think it’s because I have no personal interaction with them.” | Patient’s mother: “I don't think [meeting in-person] would've changed the physician interaction. . .because I was still able to receive the information that they had [over the phone], and ask questions and have those questions, and they've been answered.” |
| Physician: “I'm glad that we had the conversation. . .but I overall didn't like it. I don't like that I couldn't see her, so I couldn't see what her body language was or what her voice was like or if she was fearful. I couldn't read her to see if she really understood what I was saying.” | Some families may trust clinicians less without meeting them in-person. |
| Patient’s husband: “If you’re talking to a strange doctor that you’ve never met in person, what kind of confidence [do] you have in their abilities? I know they’re all doctors, but all doctors aren’t born equal. Yes. If you can meet face to face, it is a lot better.” | |
| Aligning clinician and family perspectives | |
| Telehealth-only (especially phone-only) interactions can result in families being less aligned with clinicians about their loved one’s condition. | Families felt forced to rely on clinician judgment. |
| Physician: “I think it's easier to talk with families when they have either seen no change, or a change, whether it's for better or for worse, to frame the discussion. And to check in with family and be like, ‘Hey, what we’re seeing is they're getting worse.’ And the family's often like, ‘Yeah, we’re seeing that too.’. . .So it's easier to align ourselves with the family [in person].” | Patient’s husband: “With the coronavirus thing, there’s no visitation. We have to rely on their interpretation of what’s going on. They’re experts.” |
| Physician: “Aligning our points of view was more difficult over the phone. Despite every time they said, ‘We're just trying to advocate for our mom.’ We’re like, ‘Absolutely.’ It just—there seemed to be a little bit of a disconnect. And I can't help but imagine that telecoms, teleconferencing as opposed to in-person, contributed....” | Patient’s daughter: “I had no other choice but to trust them. We can't come into the hospital now to visit with patients because of the coronavirus so we have to trust the administrators and doctors that are taking care of our families.” |
| Perceptions of amount and type of information shared over telehealth | |
| Some clinicians worry about high-stakes conversations. | Most families feel they would have received the same information in person that they did remotely. |
| Physician: “I think I’m more reluctant to address goals of care, and I’ve been doing more like information sharing. Because it’s just harder to read, like, families and where they are and how they’re receiving bad news.” | Patient’s wife: “I don’t think that we could have gotten different information if we were there. Because pretty much, we can ask anything we want to them on the Zoom.” |
Definition of abbreviation: ICU = intensive care unit.
Discussion
Both clinicians and families found that telehealth interactions (phone and video) were somewhat effective for communicating during visitor restrictions. However, it is important to note that, consistent with previous literature (18), both groups believed that communicating over phone or video was inferior to in-person interactions. Telehealth interactions were perceived more favorably for low-stakes communications, such as informational updates, and were viewed less favorably for high-stakes discussions, such as goals-of-care conversations. In the absence of the typical embodied conversational cues over phone and video, clinicians found it more challenging to interpret patients’ comprehension of the information shared and to communicate with families during complicated discussions.
Though remote communication between clinicians and families was common in ICUs even before COVID-19, the pandemic milieu presented unique challenges. In the pre–COVID-19 era, phone and video calls with families of ICU patients were most often used to supplement in-person interactions between clinicians and families. However, during this period of strict visitor restrictions in hospitals because of COVID-19, phone and video interactions acted as the only methods of communication between clinicians and families of ICU patients. A much higher proportion of families never met the clinicians caring for their loved ones, and families who wished to see their loved one in person were, with rare exceptions, unable to do so. In this context, communicating effectively with families over phone and video calls is especially critical.
Clinicians reported developing effective telehealth communication strategies through a trial-and-error process during COVID-19. Small changes in planning and communication—such as frequently checking for family understanding and ensuring that patients can visualize their loved one’s room—substantially improved the perceived quality of telehealth conversations. As other telehealth studies have noted (19, 20), there is a clear role for administrative and institutional support in improving the efficacy of telehealth communications. For example, having tablet devices with video capability readily available in units ameliorates clinician concerns about privacy when using their own personal devices and improves the ease of conducting group video communications in the ICU. A number of clinicians believed that “practice makes perfect” and that if the coronavirus continues to necessitate visitor restrictions in hospitals, clinicians will become more familiar and facile with communicating through telehealth. Some of the problems with telehealth reported in our study and others—such as technical difficulties (21) and the impact of telehealth on clinician workload (18)—may improve over time as technology develops and if health systems are forced to rely on telehealth-only interactions for longer periods.
Telehealth communication was perceived as somewhat effective by both clinicians and families. This may reflect the need for these stakeholders to “make do” under the suboptimal circumstances rather than either clinicians or families feeling that remote and in-person communication are interchangeable during normal circumstances. Both clinicians and families believed that telecommunication functioned well for information sharing but had concerns about noninformational aspects of telehealth communication, such as the ability for families to “be there” for the patient and fully grasp how sick the patient was. As a group, clinicians were fairly concerned about the drawbacks of telehealth communication with families, whereas families expressed fewer worries about telehealth communication with physicians. This disconnect may be attributable to differences in perception and spheres of influence surrounding a patient’s care in the ICU. From the standpoint of a clinician in a hospital with few COVID cases, telehealth communication with families is one of the few major changes in patient care—the rest of the ICU experience has remained largely consistent, so clinicians may focus more on communication. For families, the entire experience of having a loved one in the hospital is often devastating and unprecedented, and telehealth communication may be a minor concern relative to others: families are unable to be at bedside, offer in-person emotional support to their loved one, or form opinions with their own eyes about the patient’s care and clinical status.
Clinicians also have a greater ability to influence telecommunication in the ICU because it is under their purview that video and phone calls with families are offered during visitor restrictions. As such, clinicians likely feel more responsible for stewarding telehealth interactions and therefore express greater concern about the limitations. By contrast, families may have less control over their communication with clinicians; though they can decide how often to call the unit to ask for updates, they are often in the dark about what kinds of communication they can reasonably request and depend largely on clinicians to explain their options. In addition, families’ ability to influence and advocate for their loved one’s care is reduced when they are not at the bedside. It follows that many families may be more focused on acquiring information and understanding their loved one’s clinical status and less concerned about how that information is being conveyed. Of course, how information is delivered likely influences a great deal of families’ perception of their loved one’s situation in ways that are difficult to parse out from the content of the information shared.
Over the last several months of the COVID-19 pandemic, the use of telemedicine services has expanded significantly across the globe (22, 23). Perspectives on the ongoing use of telehealth services in medicine have continued to evolve as the pandemic progresses. Though small studies such as ours have found that various stakeholders (including patients) have felt that remote communication with clinicians is satisfactory in some contexts in the setting of the COVID-19 pandemic, it remains difficult to ascertain how much of this satisfaction is borne of patients and families being more accepting of telemedicine during a pandemic, and it is still too soon to tell whether clinical outcomes are meaningfully changed as a result of telehealth use (24, 25). In the context of an ongoing pandemic without a clear end date and an increasing reliance on telemedicine, it is important for clinicians to continue to develop remote communication skills and improve our understanding of family experiences with phone and video communication in the ICU setting.
Our study has a number of limitations. First, we interviewed clinicians and families of patients at one hospital during its initial response to the coronavirus in a city that was not an epicenter of COVID-19. The perspectives of both clinicians and families about telehealth may evolve as the COVID-19 pandemic progresses, and our results may not be generalizable beyond the initial COVID-19 response in a relatively COVID-19–spared city. The majority of patients enrolled in our study did not have COVID-19; the specific concerns of families of patients with COVID-19 (e.g., personal safety and reasons not to be present on the hospital) are not well represented in our sample. In addition, our sampling strategy, which aimed to select respondents with unique views on communication rather than on achieving demographic balance, further limits generalizability. The majority of our families were white and well educated, and these interviews therefore may not represent the experiences of all family members. Second, our suggestions for communication strategies are grounded in firsthand reports of clinicians’ experiences and have not yet been tested in the context of a behavioral study. The nurses we included in our study were all trained in communication; although this likely improved the quality of their suggestions about communication strategies, these perspectives may not be representative of bedside nurses more generally. Given the relatively small sample and heterogeneity of the clinician group, this study may not have fully captured the perspectives of individual disciplines or clinicians with different levels of experiences. Finally, participant recruitment was dependent on physicians and nurses, who asked families of critically ill patients whether they would be willing to talk to the study team; this may have introduced some selection bias into the family reports of acceptability of telehealth.
Conclusions
Although both clinicians and families of ICU patients viewed telehealth communication as moderately effective, we identified a number of discordant perspectives between clinicians and family members as well as benefits and challenges of telehealth-only interactions in the ICU. We propose strategies for effective telehealth communications with families of critically ill patients based on the experiential knowledge of family members and treating clinicians. Further research should specifically evaluate the effectiveness of telehealth communication strategies in the ICU setting.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank the families who participated in this study and the clinicians who volunteered their time to be interviewed.
Footnotes
Supported by the U.S. National Institutes of Health (NIH) through grant 5K23NS097629 (J.E.). D.B.W.’s research time is supported by the NIH through grant NIH-National Heart, Lung, and Blood Institute K24 HL148314. The authors report no conflicts of interest and have no other relevant declarations. The views expressed in this article do not communicate an official position of the University of Pittsburgh, UPMC, or NIH.
Author Contributions: N.R.K., A.S., A.A.D., and J.E. contributed to conception and design of the study. N.R.K., A.S., A.A.D., W.D., K.N., and J.E. contributed to acquisition of data. N.R.K., A.S., and J.E. contributed to data analysis and interpretation. All authors contributed to drafting the article, revising it for critically important intellectual content, and approving the version being submitted.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 2.Kleinpell R, Zimmerman J, Vermoch KL, Harmon LA, Vondracek H, Hamilton R, et al. Promoting family engagement in the ICU: experience from a national collaborative of 63 ICUs. Crit Care Med. 2019;47:1692–1698. doi: 10.1097/CCM.0000000000004009. [DOI] [PubMed] [Google Scholar]
- 3.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356:469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 4.White DB, Cua SM, Walk R, Pollice L, Weissfeld L, Hong S, et al. Nurse-led intervention to improve surrogate decision making for patients with advanced critical illness. Am J Crit Care. 2012;21:396–409. doi: 10.4037/ajcc2012223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Atlanta, GA: Centers for Disease Control and Prevention; 2019. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. [Google Scholar]
- 6.Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med. 2020;27:taaa039. doi: 10.1093/jtm/taaa039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamas DJ. New York Times; 2020. I’m on the front lines: I have no plan for this. March 25. Available from: https://www.nytimes.com/2020/03/24/opinion/coronavirus-hospital-visits.html. [Google Scholar]
- 8.Hafner K.‘A heart-wrenching thing’: hospital bans on visits devastate families New York Times; 2020. March 30Available from: https://www.nytimes.com/2020/03/29/health/coronavirus-hospital-visit-ban.html [Google Scholar]
- 9.Zauzmer J.In life’s last moments, U.S. clergy minister to the sick and dying via FaceTime and Zoom The Washington Post; 2020. April 2Available from: https://www.washingtonpost.com/religion/2020/04/02/last-rites-coronavirus-sick-facetime-clergy/ [Google Scholar]
- 10.Wakam GK, Montgomery JR, Biesterveld BE, Brown CS. Not dying alone - modern compassionate care in the covid-19 pandemic. N Engl J Med. 2020;382:e88. doi: 10.1056/NEJMp2007781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollander JE, Carr BG. Virtually perfect? Telemedicine for covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 12.White DB, Angus DC, Shields AM, Buddadhumaruk P, Pidro C, Paner C, et al. PARTNER Investigators. A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018;378:2365–2375. doi: 10.1056/NEJMoa1802637. [DOI] [PubMed] [Google Scholar]
- 13.Ruddy KJ, Greaney ML, Sprunck-Harrild K, Meyer ME, Emmons KM, Partridge AH. Young women with breast cancer: a focus group study of unmet needs. J Adolesc Young Adult Oncol. 2013;2:153–160. doi: 10.1089/jayao.2013.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.QSR International NVivo qualitative data analysis software Doncaster, Australia: QSR International; 2018[2020 Apr 14]. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home [Google Scholar]
- 17.Weber RP. Basic content analysis. 2nd ed. Newbury Park, CA: Sage Publications; 1990. p. 96. [Google Scholar]
- 18.Stelson EA, Carr BG, Golden KE, Martin N, Richmond TS, Delgado MK, et al. Perceptions of family participation in intensive care unit rounds and telemedicine: a qualitative assessment. Am J Crit Care. 2016;25:440–447. doi: 10.4037/ajcc2016465. [DOI] [PubMed] [Google Scholar]
- 19.Thorp SR, Fidler J, Moreno L, Floto E, Agha Z. Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychol Serv. 2012;9:197–199. doi: 10.1037/a0027057. [DOI] [PubMed] [Google Scholar]
- 20.Jarvis-Selinger S, Chan E, Payne R, Plohman K, Ho K. Clinical telehealth across the disciplines: lessons learned. Telemed J E Health. 2008;14:720–725. doi: 10.1089/tmj.2007.0108. [DOI] [PubMed] [Google Scholar]
- 21.Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15:225–229. doi: 10.1370/afm.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1193. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox B, Sizemore O. Verona, WI: Epic Health Research Network; 2020. Telehealth: fad or the future. Available from: https://ehrn.org/articles/telehealth-fad-or-the-future. [Google Scholar]
- 24.Mustafa SS, Yang L, Mortezavi M, Vadamalai K, Ramsey A. Patient satisfaction with telemedicine encounters in an allergy and immunology practice during the coronavirus disease 2019 pandemic. Ann Allergy Asthma Immunol. 2020;125:478–479. doi: 10.1016/j.anai.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serper M, Nunes F, Ahmad N, Roberts D, Metz DC, Mehta SJ. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology. 2020;159:1589–1591, e4. doi: 10.1053/j.gastro.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


