Abstract
Background
Coronary artery disease (CAD) in adults ≤ 35 years of age is rare, but the incidence is on the rise and the risk factors for this age group are largely uncertain. Previous studies have shown that hyperuricemia (HUA) is an independent risk factor for CAD in the general population, whereas the role in adults ≤ 35 years of age with acute coronary syndrome (ACS) is unclear.
Methods
Patients, 18–35 years of age, diagnosed with ACS for the first time at the documented institution between January 2005 and December 2015, were enrolled in the current study. The severity of CAD was assessed by the Gensini score. Patients were divided into two groups according to the definition of HUA. The relationship between HUA and CAD severity was assessed based on multi-variate analysis.
Results
Seven hundred seventy-one participants fulfilling the criteria were included in this study (mean age, 31.6 years; 94.4% male). HUA, which was defined as a serum uric acid level ≥ 7.0 mg/dL (420μmol/L) in males and ≥ 6.0 mg/dL (357 μmol/L) in females, accounted for 37% of the participants. Multivariate analysis identified that HUA is an independent risk factor of CAD severity, as assessed by the Gensini score, in very young adults with ACS (OR 8.28; 95% CI 1.96–14.59; p = 0.01), and the effect of HUA on CAD severity was second only to diabetes mellitus.
Conclusions
Hyperuricemia was shown to be an independent risk factor for CAD severity in young adults with ACS (18–35 years of age).
Keywords: coronary artery disease, hyperuricemia, Gensini score, severity, young adults
Introduction
Young populations, especially the population ≤ 35 years of age, are often overlooked with respect to the diagnoses of acute coronary syndrome (ACS), even in individuals with multiple risk factors; however, studies have demonstrated that the incidence of coronary artery disease (CAD) in young adults is following an ascending trend [1, 2]. Common risk factors for CAD, such as cigarette smoking, elevated body mass index (BMI), and diabetes mellitus (DM), are known to be associated with young patients; however, recent studies have shown that non-traditional risk factors, such as hyperuricemia (HUA), may also play a role in the development of CAD. Considering the increasing incidence of HUA in a young population, this study was conducted to determine the relationship between HUA and CAD severity in very young adults with ACS.
Methods
Study population
In this single center, observational study, young adults, 18–35 years of age, diagnosed with ACS for the first time at Anzhen Hospital between 1 January 2005 and 31 December 2015, were enrolled. The study exclusion criteria were as follows: missing uric acid data; gout, inflammatory diseases, autoimmune diseases, heart failure, and renal impairment (an estimated glomerular filtration rate [eGFR] < 60 mL/min/1.73 m2); history of diuretic or anti-hypertension drug use (losartan potassium and hydrochlorothiazide tablets, compound amiloride hydrochloride tablets, and irbesartan and hydrochlorothiazide tablets), which affect the level of uric acid, before admission; and previous percutaneous coronary intervention or coronary artery bypass grafting, congenital heart disease, cardiomyopathy and valvular heart disease. The study was approved by the Institutional Ethics Committee of Beijing Anzhen Hospital. Written informed consent was obtained from each participant.
Laboratory data collection
Blood samples were obtained from all study subjects by vein puncture after at least 12 h of fasting in the morning on the first day of admission and were analyzed using an automated biochemical analyzer to determine the levels of serum uric acid (SUA) and other laboratory indicators such as total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C).
Acute coronary syndromes refers to a group of clinical conditions generated by myocardial ischemia, including unstable angina, non-ST-segment elevation myocardial infarction and ST-segment elevation myocardial infarction [3]. ACS was diagnosed based on elevated cardiac biomarkers with classic symptoms of acute myocardial ischemia and new onset ischemic electrocardiographic abnormalities. Patients without elevated cardiac biomarkers were qualified to participate if symptoms of acute myocardial ischemia were accompanied by a new onset electrocardiographic changes [4]. Hypertension (HTN) was defined as a blood pressure ≥ 140/90 mmHg or using anti-HTN medications according to the 2010 Hypertension Prevention and Treatment Guideline [5]. DM was defined according to the 1999 World Health Organization diabetes diagnostic criteria [6]. A LDL-C level ≥ 130 mg/dL (3.4 mmol/L) was considered elevated, hypertriglyceridemia was defined as a TG ≥ 150 mg/dL (1.7 mmol/L), a HDL-C < 40 mg/dL (1.0 mmol/L) was considered low, and hypercholesterolemia was defined as a TC ≥ 200 mg/dL (5.2 mmol/L). All of the above values were defined according to the 2016 Guidelines for the Prevention and Treatment of Dyslipidemia in Chinese Adults [7]. The National Cholesterol Education Program Adult Treatment Panel III criteria [8] for the metabolic syndrome were used to diagnose study participants with metabolic syndrome. Based on published clinical guidelines, SUA levels ≥ 7.0 mg/dL (420 μmol/L) in males and ≥ 6.0 mg/dL (357 μmol/L) in females were defined as HUA [9]. A personal history of HTN and DM, a family history of CAD, cigarette smoking, and alcohol consumption were collected from electronic medical records.
Gensini score and angiographic analysis
Coronary angiography (CAG) was performed using a standard technique. Coronary angiograms were analyzed by two experienced interventional cardiologists blinded to patient clinical information. CAD was defined as a luminal diameter stenosis ≥ 50% in any of the major epicardial coronary arteries, including the left main, left anterior descending, left circumflex, and right coronary arteries and the main branches of these arteries. Patients with acute myocardial infarction were also considered to have CAD. The severity of CAD was evaluated by the Gensini score. Based on the baseline diagnostic angiogram, the Gensini score was computed by assigning a severity score to each coronary stenosis according to the degree of luminal narrowing. This number was then multiplied by a factor that took into account the geographic importance of the lesion location in the coronary arteries. The Gensini score was then expressed as the sum of scores of all coronary arteries [10].
Statistical analyses
Continuous variables are presented as the mean ± standard deviation (normal distribution) or as the median with interquartile range (non-normal distribution). Categorical variables are presented as frequencies or percentages. Comparisons of normal distribution variables between two groups were achieved using unpaired t-tests. Comparisons of non-normal distribution variables between two groups were performed using the Mann-Whitney U test. For comparisons of categorical variables, χ2 tests were used. The significant variables in the univariate analysis were brought into a multivariate linear regression model to identify predictors of CAD. The relationship between HUA and the severity of CAD was assessed with multi-variate linear regression analysis. A p value ≤ 0.05 (two-sided) was considered statistically significant. All analyses were performed with the statistical software package R and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA, USA) [11].
Results
Patient demographics
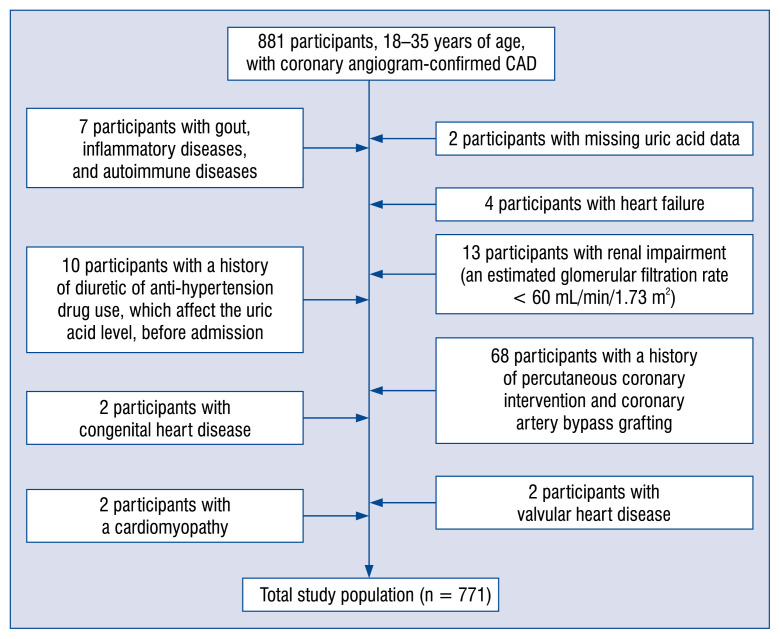
A total of 771 participants fulfilling the criteria were included in this observational study (mean age, 31.6 years; 94.4% males). Figure 1 shows the study flow chart. Two hundred eighty-five participants were included in the HUA group, and the remaining 486 participants were included in the normouricemia group. The baseline characteristics are shown in Table 1. Male gender, HTN, and metabolic syndrome were more prevalent in the HUA group than the normouricemic group (p < 0.05). The HUA group also had a decreased HDL-C level (p < 0.001). Moreover, the serum creatinine and TG levels, and BMI were increased in the HUA group (p < 0.001). The other factors which were analyzed (LDL-C, DM, family history of CAD, and alcohol consumption) were not associated with HUA.
Figure 1.
Flow chart of the study shows participant selection based on the inclusion and exclusion criteria among young adults 18–35 years of age with the diagnosis of acute coronary syndrome for the first time at this institution. A total of 771 participants were included in the analysis; CAD — coronary artery disease.
Table 1.
Baseline clinical characteristics in normouricemic and hyperuricemic patients.
| Normouricemic patient group (n = 486) | Hyperuricemic patient group (n = 285) | P | |
|---|---|---|---|
| Baseline characteristics | |||
| Age [years] | 31.6 ± 3.4 | 31.7 ± 3.5 | 0.973 |
| Male | 452 (93.0%) | 276 (96.8%) | 0.025 |
| Alcohol consumption | 115 (23.7%) | 79 (27.7%) | 0.210 |
| BUN [mg/dL] | 12.12 ± 4.85 | 12.75 ± 4.71 | 0.080 |
| Serum creatinine [mg/dL] | 0.86 ± 0.17 | 0.93 ± 0.19 | < 0.001 |
| Triglycerides [mg/dL] | 156.82 (110.75–220.61%) | 200.24 (140.87–300.35%) | < 0.001 |
| HDL-C [mg/dL] | 35.71 ± 8.15 | 33.87 ± 7.72 | 0.002 |
| LDL-C [mg/dL] | 113.96 ± 46.35 | 115.87 ± 47.75 | 0.587 |
| Total cholesterol [mg/dL] | 176.60 ± 53.79 | 183.68 ± 58.10 | 0.089 |
| Fasting glucose [mg/dL] | 104.88 ± 34.24 | 103.29 ± 30.84 | 0.519 |
| BMI [kg/m2] | 27.31 ± 3.97 | 28.86 ± 4.20 | < 0.001 |
| Traditional coronary risk factors | |||
| Current smokers | 323 (66.5%) | 203 (71.2%) | 0.170 |
| Family history of CAD | 70 (14.4%) | 43 (15.1%) | 0.795 |
| Hypertension | 186 (38.3%) | 136 (47.7%) | 0.010 |
| Diabetes mellitus | 81 (16.7%) | 43 (15.1%) | 0.565 |
| Metabolic syndrome | 257 (53.1%) | 193 (68.9%) | < 0.001 |
Values are given as the mean ± standard deviation, median with interquartile range, or number (%).
BUN — blood urea nitrogen; HDL-C — high-density lipoprotein cholesterol; LDL-C — low-density lipoprotein cholesterol; BMI — body mass index; CAD — coronary artery disease
Analysis of CAG
Analysis of the coronary angiographic findings demonstrated that multi-vessel disease was more prevalent in the HUA group (47.5% vs. 38.1%; p = 0.01). Moreover, the single-vessel disease rate was decreased and the triple-vessel disease rate was increased in the HUA group (p = 0.036). Five hundred four (54.1%) patients underwent coronary stent implantation in the current study. In addition, patients undergoing stenting whose number of stents were between 4 and 7 were more common in the HUA group (p = 0.026; Table 2).
Table 2.
Clinical features, angiographic findings, and medical treatment based on the definition of hyperuricemia in coronary artery disease patients.
| Baseline characteristics | Normouricemic patients (n = 486) | Hyperuricemic patients (n = 285) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Unstable angina | 184 (37.9%) | 132 (46.3%) | 0.021 |
| NSTEMI | 75 (15.4%) | 34 (11.9%) | 0.178 |
| STEMI | 227 (46.7%) | 119 (41.7%) | 0.182 |
| Angiographic findings of vessel involvement | 0.036 | ||
| None | 41 (8.7%) | 16 (5.6%) | |
| Single vessel | 252 (53.3%) | 133 (46.8%) | |
| Double vessel | 93(19.7%) | 62 (21.8%) | |
| Triple vessel | 87 (18.4%) | 73 (25.7%) | |
| Left main disease | 29 (6.0%) | 23(8.1%) | 0.261 |
| Multi-vessel | 180 (38.1%) | 135 (47.5%) | 0.01 |
| Treatment | 0.421 | ||
| Drug | 111 (22.8%) | 56 (19.6%) | |
| Intervention | 324 (66.7%) | 203 (71.2%) | |
| Coronary artery bypass grafting | 51 (10.5%) | 26 (9.1%) | |
| Number of stents per patient: | 0.026 | ||
| 0 | 111 (26.4%) | 56 (22.5%) | |
| 1 | 184 (43.7%) | 109 (43.8%) | |
| 2 | 80 (19.0%) | 44 (17.7%) | |
| 3 | 33 (7.8%) | 18 (7.2%) | |
| 4~7 | 13 (3.1%) | 22 (8.8%) | |
Values are given as the number (%).
NSTEMI — non-ST-segment elevation myocardial infarction; STEMI — ST-segment elevation myocardial infarction
Univariate analysis of traditional CAD risk factors
Univariate analysis showed that the traditional CAD risk factors, such as DM, LDL-C and BUN levels, were significantly associated with the severity of CAD (p < 0.05). Univariate analysis also showed that HUA plays a prominent role in the severity of CAD (odds ratio [OR] 6.85; 95% confidence interval [CI] 1.00–12.72; p = 0.022). In contrast, risk factors, such as current smokers, a family history of CAD, TG, HTN and metabolic syndrome were not significantly related to the severity of CAD (Table 3).
Table 3.
Univariate analysis of coronary artery disease risk factors.
| Variables | Statistics | Crude HR (95% CI) | P |
|---|---|---|---|
| Age | 31.64 ± 3.43 | 0.67 (−0.17, 1.50) | 0.117 |
| Gender: | |||
| Female | 43 (5.56) | 2.41 (−10.02, 14.84) | 0.7039 |
| Male | 730 (94.44) | 1.0 | |
| Hyperuricemia | 285 (36.96) | 6.85 (1.00, 12.72) | 0.022 |
| 486 (63.04) | 1.0 | ||
| BUN | 12.35 ± 4.81 | 0.78 (0.19, 1.37) | 0.0098 |
| Serum creatinine | 0.89 ± 0.18 | −7.92 (−23.65, 7.81) | 0.324 |
| BMI | 27.9 ± 4.12 | 0.07 (−0.65, 0.80) | 0.841 |
| Alcohol consumption: | |||
| Yes | 194 (25.1) | −5.54 (−12.11, 1.02) | 0.0983 |
| No | 579 (74.9) | 1.0 | |
| Current smokers: | |||
| Yes | 527 (68.18) | 4.37 (−1.74, 10.48) | 0.162 |
| No | 246 (31.82) | 1.0 | |
| Family history of CAD: | |||
| Yes | 113 (14.62) | 5.17 (−2.82, 13.15) | 0.205 |
| No | 660 (85.38) | 1.0 | |
| Hypertension: | |||
| Yes | 324 (41.91) | −4.11 (−9.85, 1.63) | 0.161 |
| No | 449 (58.09) | 1.0 | |
| Diabetes mellitus: | |||
| Yes | 124 (16.04) | 15.48 (7.77, 23.19) | < 0.001 |
| No | 649 (83.96) | 1.0 | |
| Metabolic syndrome: | |||
| Yes | 450 (58.9) | 3.25 (−2.57, 9.07) | 0.274 |
| No | 314 (41.1) | 1.0 | |
| Total cholesterol | 179.2 ± 55.48 | 0.12 (0.07, 0.17) | < 0.0001 |
| Triglycerides | 214.54 ±174.49 | 0.02 (0.00, 0.03) | 0.0532 |
| LDL-C | 114.66 ± 46.84 | 0.13 (0.07, 0.19) | < 0.0001 |
| HDL-C | 35.04 ± 8.04 | −0.37 (−0.73, −0.01) | 0.0427 |
Values are given as mean ± standard deviation or number (%).
BUN — blood urea nitrogen; CI — confidence interval; HDL-C — high-density lipoprotein cholesterol; HR — hazard ratio; LDL-C — low-density lipoprotein cholesterol; BMI — body mass index; CAD — coronary artery disease
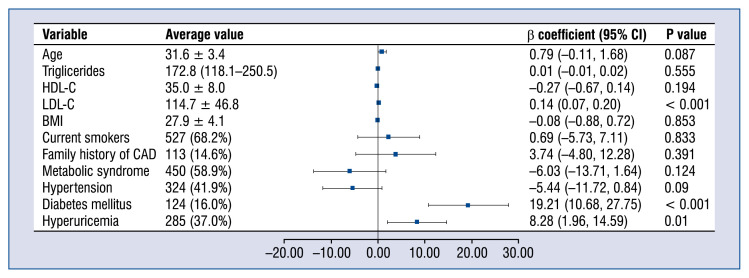
Multi-variate linear regression analysis model of different CAD risk factors
A multi-variate linear regression analysis model further showed that traditional CAD risk factors (DM [OR 19.21; 95% CI 10.68–27.75; p < 0.001] and LDL-C [OR 0.14; 95% CI 0.07–0.20; p < 0.001]) and a non-traditional CAD risk factor (HUA [OR 8.28; 95% CI 1.96–14.59; p = 0.01]) were significant risk factors for the severity of CAD after adjusting for confounding factors (Fig. 2).
Figure 2.
Forest plot of multi-variate linear regression analysis model of different coronary artery disease (CAD) risk factors. HDL-C — high-density lipoprotein cholesterol; LDL-C — low-density lipoprotein cholesterol; BMI — body mass index; CI — confidence interval.
Discussion
This is the largest study to date investigating the relationship between HUA and severity of CAD in adults ≤ 35 years of age. The most relevant finding of the current study was that HUA is an independent risk factor for CAD severity. Furthermore, the effect of HUA was shown to be only second to DM on CAD severity in this specific population of young adults.
Previous studies [12, 13] have investigated the relationship between HUA and the severity of CAD; however, the current study is the only study investigating HUA in a young ACS population. Duran et al. [14] studied 246 middle-aged and elderly non-diabetic and non-hypertensive patients with ACS and reported a positive association between HUA and angiographic severity of ischemic heart disease (Gensini score). The results of the Duran et al. study [14] are in agreement with our data; however, the Duran et al. [14] study had a smaller sample size and the participants were older. In young adults, the relationship between HUA and the progression of CAD has also been reported. A study published in 2011 [15] involving a non-CAD population 40 ± 4 years of age (CARDIA database) suggested that SUA levels are directly related to the occurrence and severity of coronary calcifications (subclinical coronary atherosclerosis indicators) independent of traditional risk factors. The study showed that a strong correlation exists between high uric acid levels and atherosclerosis, which in turn suggested that HUA may also be associated with the formation and severity of CAD in young adults; however, this conclusion was derived from non-CAD participants. An observational study [16], which included 607 premenopausal women, showed that patients with higher levels of SUA had an increased rate of multi-vessel disease. Another study involving SUA levels and premature CAD (< 45 years of age) in 2015 [17] showed that SUA levels > 8 mg/dL are predictive of an increased risk of three-vessel disease (OR 2.345; 95% CI 1.335–4.119) independent of traditional cardiovascular risk factors. The definition of HUA in this study [17] was the same as the current study and the findings are consistent with the present study regarding the relationship between HUA and the number of diseased vessels, the participants, however, were older than the participants in the current study. Moreover, we concluded that the correlation between HUA and the Gensini score was more clinically meaningful than the number of diseased vessels in describing the angiographic severity of CAD. Thus, the current study has great value compared with previous studies [17] confirming the significance of HUA with CAD in a very young population.
The current study showed that HUA may be related to patients with HTN, metabolic syndrome and an increased TG level, however, after multivariate regression analysis to eliminate the impact of other CAD risk factors, HUA still plays an independent role in the development of CAD. Current studies have drawn many different conclusions on the pathologic mechanism of uric acid in the development of CAD [12, 13, 18–21]. Uric acid can crystallize into the formation of monosodium urate crystals, which can result in tissue damage through an inflammatory response process, and thus participate in the occurrence of CAD [22]. In addition to the effect of monosodium urate crystals, there is agreement on the notion that even asymptomatic HUA can induce tissue injury, particularly at the level of coronary vessels [23, 24]. Studies have shown that HUA can lead to CAD through a number of mechanisms, such as stimulating vasoconstriction involving an inflammatory process, causing oxidative stress and impairing endothelial function [25–28]. These mechanisms are probably related to the incidence and progression of CAD in young adults.
Patient groups < 35 years of age are identified as very young in the literature [29, 30]. In the current study, the age range of participants was narrowed to 18–35 years in an effort to determine the correlation between HUA and the severity of CAD (a predictor of adverse outcomes in CAD) in a specific group (very young adults). Although traditional factors are vital for the prognosis of CAD, HUA was also shown to be an independent risk factor for CAD severity in the current study. Thus, the clinical significance of the current study involves increasing awareness of the importance of the uric acid level in patients ≤ 35 years of age. Clinicians should further instruct patients with asymptomatic HUA to pay more attention to eating habits, including a low purine diet and consuming less alcohol to control uric acid levels to within the normal range. More importantly, HUA was shown to be associated with the prognosis of CAD in young patients in the current study, as evidenced by an increased number of implanted stents associated with poor prognosis of CAD in the HUA group. Thus, the intention was to carry out an indepth study in the future to determine whether or not HUA is correlated with the prognosis of young patients after percutaneous coronary intervention and whether or not reducing HUA can decrease the severity of CAD.
Limitations of the study
There were several limitations to this study. First, this was not a randomized trial, but an observational study. Second, to define a risk factor with certainty, one has to demonstrate that reducing the factor can improve prognosis. Large randomized trials should be carried out to determine whether or not urate-lowering therapy has beneficial effects for reducing CAD mortality, thus potentially providing new therapeutic methods for the prevention and treatment of CAD. Third, in this study the Gensini score was used rather than the Syntax score to assess CAD severity. Because some patients were treated 10 years ago, and severity was assessed by CAG reports instead of reading the coronary angiogram, the Syntax score was not calculated, however, previous studies have verified the relevance and equivalence, with none inferior to the other [31].
Conclusions
In young adults with ACS (≤ 35 years of age), HUA is an independent risk factor for the severity of CAD after adjusting for potential confounding variables.
Acknowledgements
This work was supported by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of special funding support (code: ZYLX201303 grant number: ¥5000), the National Key Clinical Specialty Construction Project (2013–2014 grant number: ¥5000), and the Beijing Municipal Administration of Hospitals ascent plan (code: DFL20150601 grant number: ¥5000).
Footnotes
Conflict of interest: None declared
References
- 1.Maroszyńska-Dmoch EM, Wożakowska-Kapłon B. Clinical and angiographic characteristics of coronary artery disease in young adults: a single centre study. Kardiol Pol. 2016;74(4):314–321. doi: 10.5603/KP.a2015.0178. [DOI] [PubMed] [Google Scholar]
- 2.Bhardwaj R, Kandoria A, Sharma R. Myocardial infarction in young adults-risk factors and pattern of coronary artery involvement. Niger Med J. 2014;55(1):44–47. doi: 10.4103/0300-1652.128161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalra S, Duggal S, Valdez G, et al. Review of acute coronary syndrome diagnosis and management. Postgrad Med. 2008;120(1):18–27. doi: 10.3810/pgm.2008.04.1756. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz GG, Olsson AG, Abt M, et al. dal-OUTCOMES Investigators. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–2099. doi: 10.1056/NEJMoa1206797. [DOI] [PubMed] [Google Scholar]
- 5.Liu LS. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39(7):579–615. [PubMed] [Google Scholar]
- 6.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J, Zhou Q, Wang DP, et al. Joint committee issued Chinese guideline for the management of dyslipidemia in adults. [ST-segment elevation myocardial infarction in the eastern urban China: from 2001 to 2011]. Zhonghua Xin Xue Guan Bing Za Zhi. 2016;44(4):303–308. doi: 10.3760/cma.j.issn.0253-3758.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Thomas GN, Ho SY, Janus ED, et al. Hong Kong Cardiovascular Risk Factor Prevalence Study Steering Committee. The US National Cholesterol Education Programme Adult Treatment Panel III (NCEP ATP III) prevalence of the metabolic syndrome in a Chinese population. Diabetes Res Clin Pract. 2005;67(3):251–257. doi: 10.1016/j.diabres.2004.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Kanbay M, Solak Y, Dogan E, et al. Uric acid in hypertension and renal disease: the chicken or the egg? Blood Purif. 2010;30(4):288–295. doi: 10.1159/000321074. [DOI] [PubMed] [Google Scholar]
- 10.Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51(3):606. doi: 10.1016/s0002-9149(83)80105-2. [DOI] [PubMed] [Google Scholar]
- 11.Liu J, Zuo SW, Li Y, et al. Hyperhomocysteinaemia is an independent risk factor of abdominal aortic aneurysm in a Chinese Han population. Sci Rep. 2016;6:17966. doi: 10.1038/srep17966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SY, Guevara JP, Kim KMi, et al. Hyperuricemia and coronary heart disease: a systematic review and meta-analysis. Arthritis Care Res (Hoboken) 2010;62(2):170–180. doi: 10.1002/acr.20065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braga F, Pasqualetti S, Ferraro S, et al. Hyperuricemia as risk factor for coronary heart disease incidence and mortality in the general population: a systematic review and meta-analysis. Clin Chem Lab Med. 2016;54(1):7–15. doi: 10.1515/cclm-2015-0523. [DOI] [PubMed] [Google Scholar]
- 14.Duran M, Kalay N, Akpek M, et al. High levels of serum uric acid predict severity of coronary artery disease in patients with acute coronary syndrome. Angiology. 2012;63(6):448–452. doi: 10.1177/0003319711426868. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan E, Pandya BJ, Chung L, et al. Hyperuricemia and the risk for subclinical coronary atherosclerosis--data from a prospective observational cohort study. Arthritis Res Ther. 2011;13(2):R66. doi: 10.1186/ar3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Jw, He Lj, Cao Sj, et al. Association of serum uric acid and coronary artery disease in premenopausal women. PLoS One. 2014;9(9):e106130. doi: 10.1371/journal.pone.0106130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dai XM, Wei L, Ma LL, et al. Serum uric acid and its relationship with cardiovascular risk profile in Chinese patients with earlyonset coronary artery disease. Clin Rheumatol. 2015;34(9):1605–1611. doi: 10.1007/s10067-015-2878-1. [DOI] [PubMed] [Google Scholar]
- 18.Kanbay M, Segal M, Afsar B, et al. The role of uric acid in the pathogenesis of human cardiovascular disease. Heart. 2013;99(11):759–766. doi: 10.1136/heartjnl-2012-302535. [DOI] [PubMed] [Google Scholar]
- 19.Volterrani M, Iellamo F, Sposato B, et al. Uric acid lowering therapy in cardiovascular diseases. Int J Cardiol. 2016;213:20–22. doi: 10.1016/j.ijcard.2015.08.088. [DOI] [PubMed] [Google Scholar]
- 20.Zuo T, Liu X, Jiang Lu, et al. Hyperuricemia and coronary heart disease mortality: a meta-analysis of prospective cohort studies. BMC Cardiovasc Disord. 2016;16(1):207. doi: 10.1186/s12872-016-0379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borghi C, Tykarski A, Widecka K, et al. Expert consensus for the diagnosis and treatment of patient with hyperuricemia and high cardiovascular risk. Cardiol J. 2018;25(5):545–563. doi: 10.5603/CJ.2018.0116. [DOI] [PubMed] [Google Scholar]
- 22.Grassi D, Ferri L, Desideri G, et al. Chronic hyperuricemia, uric acid deposit and cardiovascular risk. Curr Pharm Des. 2013;19(13):2432–2438. doi: 10.2174/1381612811319130011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klinenberg JR, Kippen I, Bluestone R. Hyperuricemic nephropathy: pathologic features and factors influencing urate deposition. Nephron. 1975;14(1):88–98. doi: 10.1159/000180438. [DOI] [PubMed] [Google Scholar]
- 24.Wu L, Yang LJ, Meng XY, et al. Association between hyperuricemia and outcomes in patients undergoing percutaneous coronary intervention. Int J Cardiol. 2016;204:152–153. doi: 10.1016/j.ijcard.2015.11.184. [DOI] [PubMed] [Google Scholar]
- 25.Biscaglia S, Ceconi C, Malagù M, et al. Uric acid and coronary artery disease: An elusive link deserving further attention. Int J Cardiol. 2016;213:28–32. doi: 10.1016/j.ijcard.2015.08.086. [DOI] [PubMed] [Google Scholar]
- 26.Puddu P, Puddu GM, Cravero E, et al. Relationships among hyperuricemia, endothelial dysfunction and cardiovascular disease: molecular mechanisms and clinical implications. J Cardiol. 2012;59(3):235–242. doi: 10.1016/j.jjcc.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Li M, Hu X, Fan Y, et al. Hyperuricemia and the risk for coronary heart disease morbidity and mortality a systematic review and dose-response meta-analysis. Sci Rep. 2016;6:19520. doi: 10.1038/srep19520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.pmhdev. Xanthine oxidase inhibition for the treatment of cardiovascular disease: a systematic review and meta-analysis — National Library of Medicine- PubMed Health. Centre for Reviews & Dissemination; 2012. [Google Scholar]
- 29.Wolfe C, Vacek J. Myocardial Infarction in the Young. Chest. 1988;94(5):926–930. doi: 10.1378/chest.94.5.926.. [DOI] [PubMed] [Google Scholar]
- 30.Christus T, Shukkur AM, Rashdan I, et al. Coronary Artery Disease in Patients Aged 35 or less - A Different Beast? Heart Views. 2011;12(1):7–11. doi: 10.4103/1995-705X.81550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sinning C, Lillpopp L, Appelbaum S, et al. Angiographic score assessment improves cardiovascular risk prediction: the clinical value of SYNTAX and Gensini application. Clin Res Cardiol. 2013;102(7):495–503. doi: 10.1007/s00392-013-0555-4. [DOI] [PubMed] [Google Scholar]