Abstract
Objectives:
In this study, we examined use of and interest in using opioids and marijuana, particularly in relation to use motives and perceived barriers to use, among people living with HIV (PLWH).
Methods:
We analyzed online survey data from 304 PLWH in the United States recruited via social media in Summer 2018.
Results:
In this sample (Mage = 30.86, 40.5% male, 64.5% white), 16.1% reported current (past 30-day) use of opioids, 18.1% marijuana, and 15.8% both. Participants reported more use motives and fewer barriers to using marijuana versus opioids (p’s < .001). The most frequently endorsed motive for using either/both drugs were to cope with pain and stress/anxiety. Highest-rated barriers to using either/both drugs were missing symptoms of worsening illness and addiction concerns. Regression analyses indicated that current opioid use correlated with reporting greater opioid use motives; among past-month opioid nonusers, greater interest in using opioids correlated with greater opioid use motives. Current marijuana use correlated with reporting greater marijuana use motives and greater barriers; among past-month marijuana nonusers, greater interest in using marijuana correlated with greater marijuana use motives and fewer barriers.
Conclusions:
Use motives and barriers differentially correlated with use and interest in use across drugs, thereby indicating different intervention approaches to address appropriate use.
Keywords: opioid, marijuana, patient perspectives, symptom management, HIV
Opioids are the most widely prescribed treatment for chronic pain in the United States (US).1–4 Long-term opioid therapy to manage pain has been associated with improvements in quality of life, lower healthcare utilization, and higher productivity.5 However, long-term use of opioids is controversial because of concerns about side effects, long-term efficacy, and functional outcomes, as well as the potential for abuse and addiction.5,6 Nearly 2.5 million people in the US are experiencing opioid addiction, with 75%–83% starting with a prescription drug.7 Moreover, drug overdose is now the leading cause of accidental death in the US,8 opioid overdoses accounting for 61% of overdose deaths.9 Thus, many medical providers are hesitant to prescribe opioids in general as a result,10–12 and patients face multiple barriers to accessing opioids.12
Many patients and providers are turning to marijuana for symptom management.13,14 Currently, 35 states, 4 US territories and the District of Columbia have approved some form of medical marijuana laws.15–17 There is a growing body of evidence that supports the use of prescribed medical to relieve suffering from chronic pain, to reduce morbidity and mortality associated with the use and abuse of pharmaceutical opioids,1,18,19 and to improve quality of life.20 In addition, research suggests that when used in conjunction with opioids, marijuana can lead to a greater cumulative relief of pain, which could reduce patients’ opioid use rates/levels and their adverse side effects.1,20–23 However, this research is still in its infancy and is controversial with regard to its implications for clinical practice.23 Moreover, there are potential negative consequences of marijuana use, including adverse side effects and risk of abuse or addiction.23,24 For patients who do not live in jurisdictions with medical marijuana, obtaining prescription medical marijuana for symptom management is a challenge and can have legal implications.
The controversy regarding the medical use of these drugs has important implications for patient populations, such as people living with HIV (PLWH), a growing population in the US.19,25 PLHWH experience various late and long-term health effects associated with their disease,25,26 and thus, require ongoing management of disease-related health implications.2,27 Particularly relevant to the current study, pain is a common physical symptom among PLWH,2,28 with chronic pain affecting 30%–90% of PLWH.1,2,18,28,29 In addition, PLWH face significant emotional burden related to their respective diseases,30–32 often variable depending on the presence of physical symptoms and elapsed time since diagnosis, which also impact physical health and quality of life.32,33 Given their symptoms and the complexities of opioid and marijuana use to address them, PLWH are left to make difficult decisions about how to best manage their symptoms. However, limited research has examined patient attitudes and ways of navigating these complex issues with regard to medical management of disease-related symptoms.
This study is informed by the Health Belief Model (HBM)34 and the Health Information Seeking Model (HISM; Figure 1).35,36 HBM suggests that one’s beliefs regarding personal threat and/or seriousness of an illness or disease (ie, perceived susceptibility and severity), the effectiveness of the health behavior or treatment (ie, perceived benefits), and the challenges to accessing or using a treatment option (ie, perceived barriers) collectively predict health behaviors.34 HISM35,36 focuses on how individuals access and use information related to health, illness, and related risk factors to make medical decisions or health behavior changes.35–37 Drawing from these frameworks, one’s prior experiences – including their illness, symptoms, medical treatments, and use of medications, and exposure to information about medical options – can shape the perceived utility or benefits (eg, symptom relief) of using different treatment options and the barriers to using them (eg, concerns about addiction, stigma related to use, adverse side effects).23,24 These experiences likely influence their interest in, attitudes about, and the actual use of specific medical options.34
Figure 1.
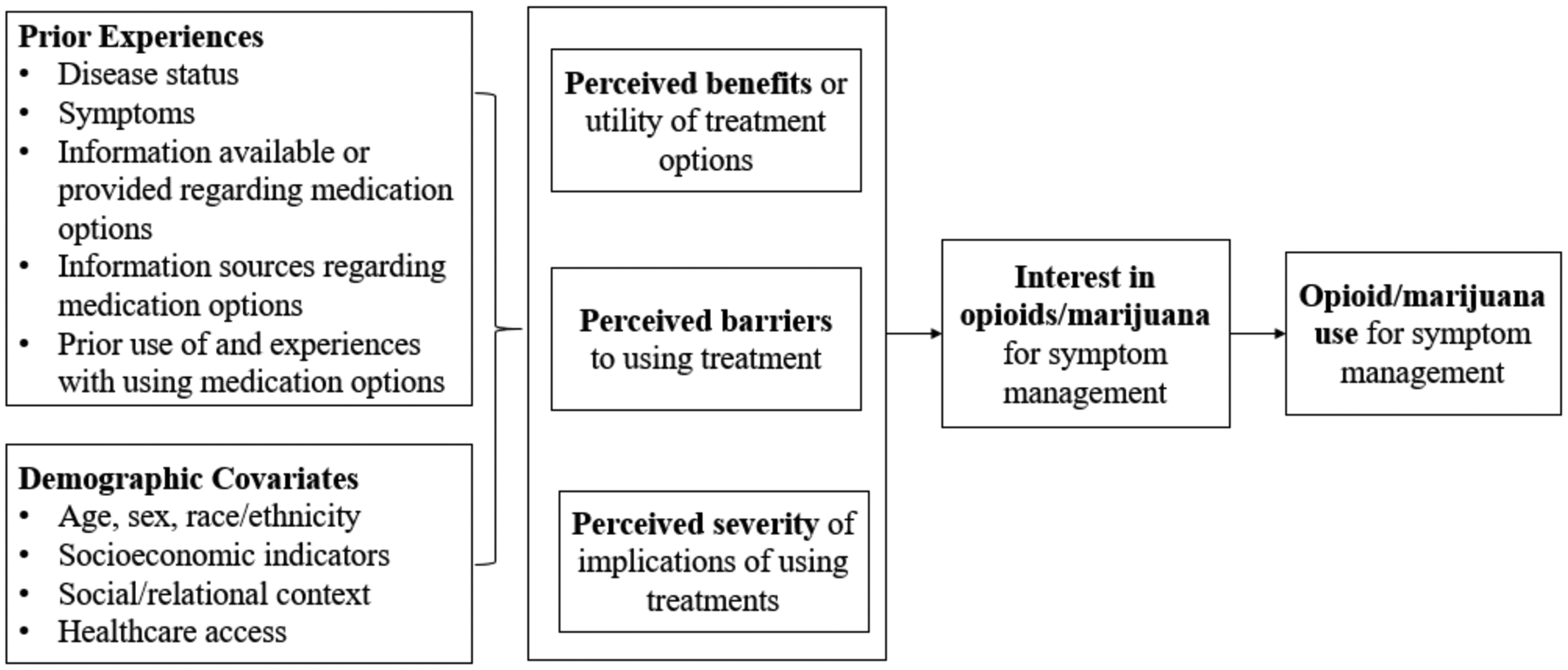
Conceptual Model
Leveraging this overall conceptual framework, we aimed to address a critical gap in the literature, specifically regarding opioid and marijuana use and interest in use for symptom management among PLWH, as well as how motives for use and perceived barriers to use correlate with these outcomes. Moreover, we examined common and preferred information sources regarding these drugs.
METHODS
Procedures and Participants
Recruitment for this study was done parallel to recruitment for a study focused on cancer survivors, with the broad scope of research focused on symptom management and quality of life among patient populations. Participant recruitment was done via advertisements on 2 social networking websites, specifically Facebook and Reddit, modeled after other published research methods.38 To provide greater detail, we targeted PLWH, cancer survivors, and symptom management by integrating 2 approaches. First, to identify those likely to have a history of cancer or HIV, algorithms within each social media site were used to increase ad exposure among (or target) individuals following certain topics (eg, HIV, cancer survivorship, medical marijuana). Second, study advertisements targeting these groups used taglines such as “Help researchers learn more about your experience using [opioids/marijuana] to address [cancer symptoms]” and “We want to know how those with [HIV manage their pain. Let us know by participating in this research study!” Advertisement images included pink/red awareness ribbons, individuals diverse in age and ethnicity, and nature scenes such as lakes and mountains.
Individuals who clicked on the advertisements were directed to the online survey, administered via www.surveygizmo.com. The landing page provided a brief description of the study and a link to the informed consent form along with a more detailed description of the study. Once participants provided their consent to participate, they were screened for eligibility. To be eligible for the larger study, participants needed to: (1) reside in the US, (2) be at least 18 years old, and either have been (3a) diagnosed with HIV/AIDS or (3b) diagnosed with cancer and completed cancer treatment within the past 6 months. Those eligible for the current study met criteria 1, 2 and 3a. The eligibility screener also assessed sex and race/ethnicity. Those who consented and met eligibility criteria then completed the online survey. To limit duplicate responses, one response per IP address was permitted. Purposive sampling was used to ensure recruitment of roughly equal numbers of men and women, at least one-third of the sample was non-white, and at least one-third of the sample was comprised of cancer survivors and PLWH, respectively, thus declining further enrollment among subgroups that met recruitment targets (based on eligibility screener responses). The survey took approximately 30 minutes to complete. Each participant was compensated with a $5 gift card.
Recruitment occurred over between June 29, 2018 and July 4, 2018. Of the 702 individuals who clicked on the advertisements, 20 did not provide consent (4 did not respond to the consent form and 16 declined consent). Of the 682 who provided consent, 66 were deemed ineligible at the screening stage (ie, 12 resided outside of the US, 6 were outside the eligible age range, 38 were HIV negative and had no prior cancer diagnosis, 10 cancer survivors were more than 6 months from treatment completion). In addition, we discontinued enrollment of women once our target enrollment was reached (ie, 25 women who were eligible were not enrolled). Of the 591 who consented and were deemed eligible, 88 provided incomplete survey data, and 5 were deemed to have invalid data (eg, illogical response patterns). Thus, 498 had complete and valid responses (Figure 2), 304 of whom were PLWH who were included in these analyses.
Figure 2.
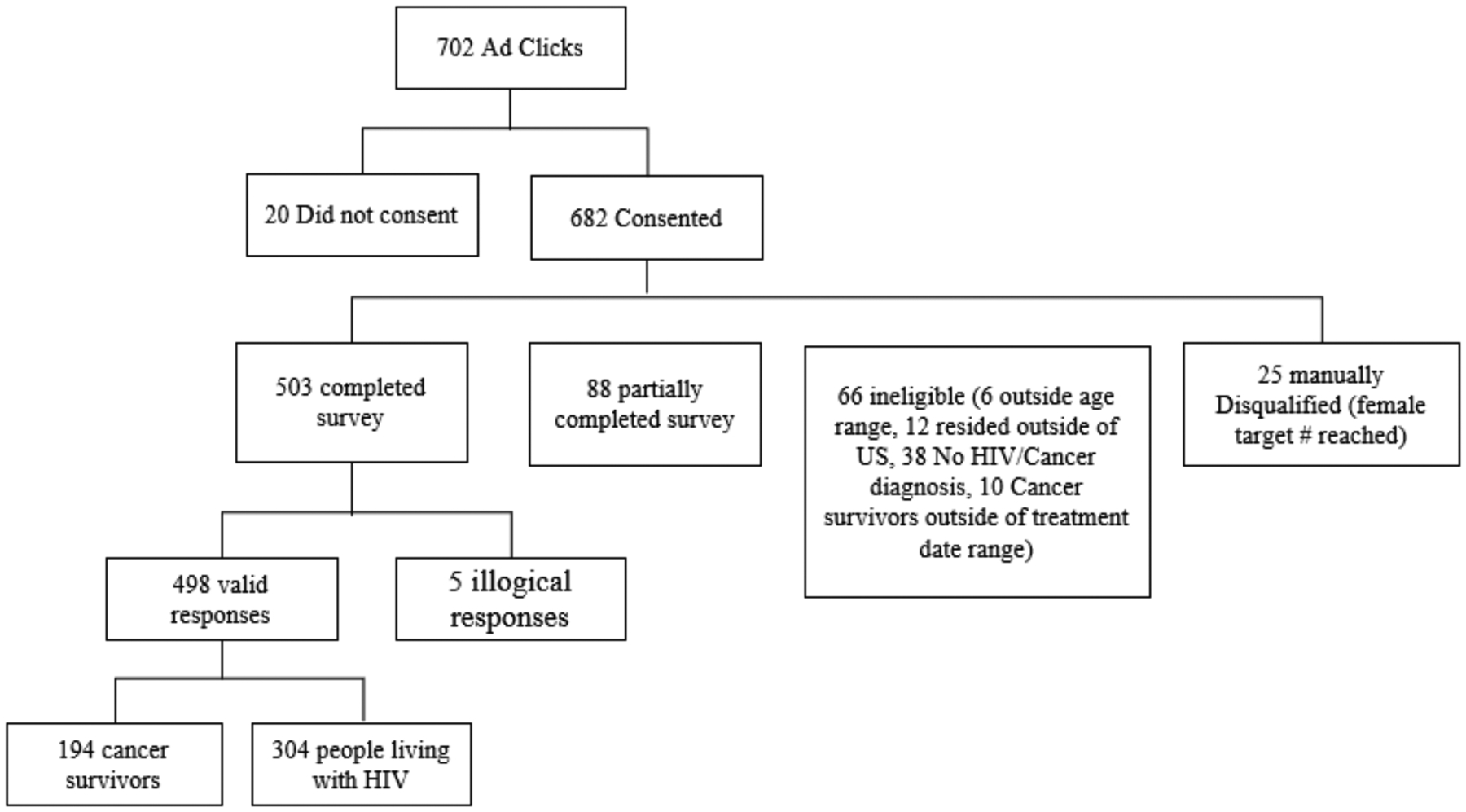
Recruitment and Eligibility Flowchart
Measures
Potential covariates.
Sociodemographics included age, sex, race/ethnicity, marital status, children in the home, employment status, educational background, pre-tax monthly household income, and insurance coverage.
Descriptive factors.
Self-reported medical information was obtained, including if participants had ever been diagnosed with HIV/AIDS, and if so, their HIV status (asymptomatic, symptomatic, or AIDS converted) and viral load status (detectable, undetectable, or don’t know).
Common and preferred information sources regarding drugs were assessed among all participants by asking: “From what sources do you get information on the use of [opioids and marijuana/cannabis] as it relates to your medical condition? (Check all that apply.)” Response options included: doctor/nurse, another patient, websites/blogs, naturopath/herbalist, [medicinal marijuana store for marijuana], friend/family member, pamphlet/handout, nutritionist, newspaper/magazine article, social media (Facebook, Twitter, etc), TV/Radio advertisement, literature/research, other, or I haven’t received this information.39 Participants’ preferred information source about opioids or marijuana use was assessed by asking: “From what sources would you prefer to get information on [opioid or marijuana/cannabis] use as it relates to your medical condition? (Check all that apply.)” with the same response options.39
Primary predictors of interest.
Potential motives for use were assessed among all participants by asking: “For which of the following reasons would you use [opioids or marijuana/cannabis]? (Check all that apply.)” Response options included: for pain related to your medical condition, for another type of pain not caused by these conditions (such as back pain or arthritis), for nausea/upset stomach, to improve appetite, for depression/to improve mood, to help cope with illness, to help deal with stress/anxiety, to sleep, for recreational use/enjoyment, to treat your medical condition, none of these conditions, other, or refuse to answer.40 Among past 12-month users, motives for actually using the respective drugs was assessed (within a separate section via a skip pattern) by asking parallel questions for opioids and marijuana, reframing the stem to indicate: “For which of the following reasons do you use [opioids or marijuana/cannabis]? (Check all that apply.)” with the same response options.40 Index scores for use motives and potential use motives for each drug, respectively, were created by summing the number of responses endorsed.
Perceived barriers to using opioids and marijuana were assessed using the Barriers Questionnaire – 13 item.41 We asked: “For each of the items below, please indicate the number (0 = Do not agree at all to 5 = Agree very much) that comes closest to how much you agree with that item.” Example items include: “Drowsiness from [opioids or marijuana/cannabis] is or could be really a bother” and “People get addicted to [opioids or marijuana/cannabis] easily” (all items listed in Table 3). Total scores were computed by averaging scores across opioid items and marijuana items, respectively. Cronbach’s alphas in the current study were .86 for opioids and .79 for marijuana.
Table 3.
Bivariate Analyses Regarding Motives/Potential Motives for and Barriers to Using Opioids or Marijuana
| Opioids | Marijuana | P | |
|---|---|---|---|
| Potential motives to use [med] in all participants (N, %) a | |||
| For pain related to your medical condition | 42 (13.8) | 149 (49.0) | < .001 |
| For another type of pain not caused by these conditions | 217 (71.4) | 199 (65.5) | .116 |
| For nausea/upset stomach | 17 (5.6) | 23 (7.6) | .326 |
| To improve appetite | 118 (38.8) | 135 (44.4) | .162 |
| For depression/to improve mood | 25 (8.2) | 28 (9.2) | .666 |
| To help cope with illness | 22 (7.2) | 34 (11.2) | .092 |
| To help deal with stress/anxiety | 18 (5.9) | 25 (8.2) | .224 |
| To sleep | 7 (2.3) | 16 (5.3) | .056 |
| For recreational use/enjoyment | 4 (1.3) | 8 (2.6) | .244 |
| To treat medical condition | 11 (3.6) | 14 (4.6) | .540 |
| None of these conditions | 15 (4.9) | 14 (4.6) | .849 |
| Motives for use (in past 12-month users) (N, %) a | N=49 | N=57 | |
| For pain related to your medical condition | 11 (22.4) | 18 (31.6) | .293 |
| For another type of pain not caused by these conditions | 10 (20.4) | 15 (26.3) | .475 |
| For nausea/upset stomach | 15 (30.6) | 22 (38.6) | .390 |
| To improve appetite | 26 (53.1) | 22 (38.6) | .136 |
| For depression/to improve mood | 12 (24.5) | 15 (26.3) | .830 |
| To help cope with illness | 15 (30.6) | 19 (33.3) | .765 |
| To help deal with stress/anxiety | 14 (28.6) | 20 (35.1) | .474 |
| To sleep | 10 (20.4) | 10 (17.5) | .707 |
| For recreational use/enjoyment | 2 (4.1) | 7 (12.3) | .131 |
| To treat medical condition | 7 (14.3) | 8 (14.0) | .971 |
| None of the conditions above | 0 (0.0) | 0 (0.0) | |
| Barriers (M, SD) b | |||
| Drowsiness | 3.55 (0.95) | 2.40 (1.63) | < .001 |
| Symptoms signal worsening disease | 3.92 (1.45) | 2.59 (1.44) | < .001 |
| Confusion | 3.01 (1.16) | 2.54 (1.48) | < .001 |
| Do/would not like | 2.68 (1.06) | 2.46 (1.56) | < .001 |
| Cannot control my symptoms/pain | 3.25 (1.13) | 2.66 (1.55) | .042 |
| Concern of addiction | 3.60 (1.00) | 2.45 (1.49) | < .001 |
| Nausea | 3.66 (1.19) | 2.37 (1.47) | < .001 |
| Important to be strong by not talking about symptoms | 2.85 (0.99) | 2.51 (1.51) | .001 |
| Doctors should focus on cure, not symptoms | 3.19 (1.50) | 2.49 (1.59) | < .001 |
| Could cause embarrassing behavior | 3.26 (0.95) | 2.37 (1.56) | < .001 |
| Concern about habituating to medication | 3.53 (1.07) | 2.52 (1.50) | < .001 |
| Constipation | 3.40 (1.43) | 2.53 (1.54) | < .001 |
| Medication side effects | 2.98 (0.96) | 2.34 (1.43) | < .001 |
Note.
Number of participants endorsing each item.
On a scale of 0 = Do not agree at all to 5 = Agree very much.
Primary outcomes.
Opioid and marijuana use were assessed by asking about lifetime use and, among ever users of the respective drugs, age at first use and past 12-month use.40 Among past 12-month users, we assessed number of days of opioid and marijuana use in the past 30 days; response options included 0 through 30 and refuse.40
Interest in opioids and marijuana for symptom management was assessed by asking: “On a scale of 1 to 10, with 1 being “not at all interested” and 10 being “extremely interested,” how interested are you in learning more about [opioids/marijuana/cannabis] to treat symptoms related to HIV?”39 Average scores among participants were calculated to determine reported interest in opioids and marijuana, respectively.
Data Analysis
Participant characteristics and factors related to medical condition, information sources, motives for use, use barriers, drug use, and interest in using these drugs for symptom management were summarized using descriptive statistics. Multivariable binary logistic regressions were then conducted examining correlates of the outcome of current (past 30-day) use, and multivariable linear regressions were conducted examining the outcome of interest in use, entering the primary predictors of interest (ie, use motives, perceived barriers) and controlling for sociodemographics. Using multivariable linear regressions, we also explored the outcomes of potential use motives and barriers to use among current users and nonusers of the respective drugs.
In preliminary analyses, we conducted bivariate analyses, as well as examined instances of collinearity among variables and cell sizes for some variables, to inform our inclusion of sociodemographic covariates in regression models. Given small cell sizes for education, employment, and insurance status and the associations of income with these 3 variables, income was selected for entry into the multivariable models; given the small cell sizes for children in the home and the association between marital status and children in the home, marital status was selected for entry into the multivariable models. SPSS 25.0 was used for all data analyses. Statistical significance was set at α = .05 for all tests.
RESULTS
Participant Characteristics
Participants in this study represented 42 states. Participants were on average 30.86 years old (SD = 8.07); 40.5% were male, 64.5% white, 20.1% black, 80.6% married/cohabitating, 95.7% employed, and 84.9% with more than a high school education (Table 1). In this sample, 118 (38.8%) reported being asymptomatic, 109 (35.9%) symptomatic, and 77 (25.3%) AIDS converted. Additionally, 119 (39.1%) reported a detectable viral load, 92 (30.3%) undetectable viral loads, and the remainder (N = 93, 30.6%) were not aware of their current status.
Table 1.
Participant Characteristics, N = 304
| PLWH | |
|---|---|
| Age (M, SD) | 30.86 (8.07) |
| Sex (N, %) | |
| Male | 123 (40.5) |
| Female | 181 (59.5) |
| Race (N, %) | |
| White | 196 (64.5) |
| Black | 61 (20.1) |
| Other | 47 (15.5) |
| Relationship Status (N, %) | |
| Married/cohabitating | 245 (80.6) |
| Other | 59 (19.4) |
| Employed (N, %) | |
| Full-/part-time | 291 (95.7) |
| Other | 13 (4.3) |
| Education (N, %) | |
| ≤HS | 46 (15.1) |
| >HS | 258 (84.9) |
| Children in Home (N, %) | |
| No | 289 (95.1) |
| Yes | 15 (4.9) |
| Income (N, %) | |
| ≤$1799/month | 63 (20.7) |
| >$1799/month | 241 (79.3) |
| Insurance (N, %) | |
| Private | 219 (72.0) |
| Government | 77 (25.3) |
| None | 8 (2.6) |
Overall, 49 participants (16.1%) reported past 12-month use of opioids, 57 (18.8%) marijuana, and 48 (15.8%) both; 49 (16.1%) reported current (past 30-day) use of opioids, 55 (18.1%) marijuana, and 48 (15.8%) both (Table 2). In general, there was greater interest in learning more about marijuana than opioids (M = 6.60, SD = 2.31 vs M = 5.97, SD = 2.27, p < .001); this held true comparing past-year nonusers of the respective drugs (opioids: M = 7.55, SD = 1.63 vs marijuana: M = 9.50, SD = 1.68, p < .001; not shown in tables).
Table 2.
Bivariate Results: Opioid and Marijuana Use History, Interest in Use, and Information Sources, N = 304
| Opioids | Marijuana | P | |
|---|---|---|---|
| Lifetime use (N, %) | 54 (17.8) | 61 (20.1) | .468 |
| Age at first use (M, SD) a | 21.19 (7.40) | 19.57 (5.80) | .003 |
| Used in past 12 months (N, %) | 49 (16.1) | 57 (18.8) | .392 |
| Used in past 30 days (N, %) | 49 (16.1) | 55 (18.1) | .518 |
| Number of days of use, past 30 days (M, SD) | 6.24 (4.96) | 7.14 (5.78) | .040 |
| Interest in learning about [med] (M, SD) a | 5.97 (2.27) | 6.60 (2.31) | .001 |
| Sources of information on [med] (N, %) b | |||
| Doctor/nurse | 29 (9.5) | 18 (5.9) | .095 |
| Another patient | 15 (4.9) | 11 (5.7) | .422 |
| Websites/blogs | 234 (77.0) | 35 (11.5) | < .001 |
| Naturopath/herbalist | 17 (5.6) | 219 (72.0) | < .001 |
| Friend/family member | 219 (72.0) | 216 (71.1) | .787 |
| Pamphlet/handout | 16 (5.3) | 8 (2.6) | .096 |
| Nutritionist | 9 (3.0) | 12 (3.9) | .505 |
| Newspaper/magazine article | 13 (4.3) | 21 (6.9) | .158 |
| Social media (Facebook, Twitter, etc.) | 22 (7.1) | 25 (8.2) | .648 |
| TV/Radio advertisement | 9 (3.0) | 5 (1.6) | .279 |
| Literature/research | 4 (1.3) | 2 (1.0) | .412 |
| Doctor/nurse outside of the health center | 110 (36.2) | -- | -- |
| Medicinal marijuana store | -- | 25 (8.2) | -- |
| Preferred sources of information on [med] (N, %) b | |||
| Doctor/nurse | 29 (9.5) | 127 (41.8) | < .001 |
| Another patient | 109 (35.9) | 116 (38.2) | .557 |
| Websites/blogs | 130 (42.8) | 134 (44.1) | .743 |
| Naturopath/herbalist | 115 (37.8) | 13 (4.3) | .743 |
| Friend/family member | 14 (4.6) | 26 (8.6) | .047 |
| Pamphlet/handout | 19 (6.3) | 16 (5.3) | .601 |
| Nutritionist | 7 (2.3) | 11 (3.6) | .339 |
| Newspaper/magazine article | 13 (4.3) | 16 (5.3) | .568 |
| Social media (Facebook, Twitter, etc.) | 10 (3.3) | 112 (36.8) | < .001 |
| TV/Radio advertisement | 109 (35.9) | 6 (2.0) | < .001 |
| Literature/research | 3 (1.0) | 5 (1.6) | .477 |
| Doctor/nurse outside of the health center | 0 (0.0) | -- | -- |
| Medicinal marijuana store | -- | 216 (71.1) | -- |
Note.
On a scale of 1 = not at all to 10 = extremely interested.
Number of participants endorsing each item.
Sources of Information Regarding Opioids and Marijuana
Among all participants, friends/family were the most frequently endorsed sources of information regarding opioid and marijuana use (72.0% and 71.1%, respectively; Table 2). Other frequently endorsed information sources regarding opioids included websites/blogs (77.0%) and doctors/nurses outside of the health center (36.2%). Other frequently endorsed information sources regarding marijuana included naturopaths/herbalists (72.0%). The most frequently endorsed preferred sources of information regarding opioid and marijuana use were websites/blogs (42.8% and 44.1%, respectively) and other patients (35.9% and 38.2%, respectively). Other frequently endorsed preferred sources of information regarding marijuana use were healthcare providers (41.8%), social media (36.8%) and marijuana dispensaries (71.1%).
Use Motives and Potential Use Motives
Among all participants, there was a greater number of motives for potentially using marijuana versus opioids (M = 2.08, SD = 1.47 vs M = 1.58, SD = 1.07, respectively, p < .001). Among all participants, the most frequently endorsed motives for potentially using opioids and marijuana, respectively, were to manage pain not caused by their medical condition (71.4% and 65.5%, respectively) and to improve appetite (38.8% and 44.4% respectively; Table 3). Additionally, a frequently endorsed motive for potentially using marijuana was for pain related to their medical condition (49.0%).
Table 3 also presents data regarding actual use motives among past 12-month users. Among past 12-month opioid users (N = 49, 16.1%) and past 12-month marijuana users (N = 57, 18.8%), common use motives for using opioids and marijuana were to improve appetite (53.1% and 38.6% respectively), for nausea (30.6% and 38.6%, respectively), to help cope with illness (30.6% and 33.3%, respectively), and to cope with stress/anxiety (28.6% and 35.1%, respectively).
Multivariable linear regression analyses examining correlates of number of motives for using the respective drugs (not shown in tables) included sociodemographics (ie, age, sex, race/ethnicity, marital status, and income). Reporting more potential motives for using opioids among past-year opioid nonusers was associated with being unmarried/ not cohabitating (B = −.050, CI: −0.74, −0.23, p < .001) and lower income (B = −0.45, CI: −0.64, −0.25, p < .001; Adjusted R-square = .182). Reporting more actual motives for using opioids among past-year opioid users was associated with being black (vs white, B = 1.82, CI: 0.60, 3.04, p = .004) and lower income (B = −1.41, CI: −2.45, −0.38, p = .009; Adjusted R-square = .278).
Reporting more potential motives for using marijuana among past-year marijuana nonusers was associated with being unmarried/not cohabitating (B = −0.90, CI: −1.33, −0.47, p < .001) and higher income (B = 0.89, CI: 0.59, 1.20, p < .001; Adjusted R-square = .278). Reporting more actual motives for using marijuana among past-year marijuana users was associated with lower income (B = −1.59, CI: −2.77, −0.41, p = .009; Adjusted R-square = .265).
Perceived Barriers to Use
Table 3 presents data regarding perceived barriers for opioid and marijuana use among all participants. Overall, participants reported fewer barriers to using marijuana versus opioids (M = 32.23, SD = 11.36 vs M = 42.88, SD = 8.06, p < .001). On average, among the highest-rated perceived barriers to using opioids and marijuana were because “having symptoms means the disease is getting worse” (M = 3.92, SD = 1.45 and M = 2.59, SD = 1.44, respectively) and concerns of addiction (M = 3.60, SD = 1.00 and M = 2.45, SD = 1.44, respectively).
Among past-year opioid nonusers, multivariable linear regression analyses (examining sociodemographic correlates; not shown in tables) indicated that greater perceived barriers for using opioids was associated with being unmarried/not cohabitating (B = 3.71, CI: 0.32, 7.10, p = .032) and lower income (B = −3.62, CI: −6.08, −1.16, p = .004; Adjusted R-square = .068). Among past-year opioid users, greater perceived barriers for using opioids was associated with higher income (B = 6.34, CI: 1.43, 11.25, p = .013; Adjusted R-square = .240).
Among past-year marijuana nonusers, greater perceived barriers for using marijuana was associated with being diagnosed with being male (B = −3.25, CI: −6.02, −0.47, p = .022), married/cohabitating (B = 17.46, CI: 14.18, 20.74, p < .001), and higher income (B = 2.55, CI: 0.23, 4.87, p = .032; Adjusted R-square = .536; not shown in tables). Among past-year marijuana users, greater perceived barriers for using marijuana was associated with being unmarried/not cohabitating (B = −15.15, CI: −21.21, −9.08, p < .001; Adjusted R-square = .331).
Opioid and Marijuana Use and Interest in Use
Binary logistic regression indicated that current opioid use was associated with reporting greater motives for opioid use (OR = 2.96, CI: 1.84, 4.78, p < .001), as well as being female (OR = 0.02, CI: 0.01, 0.07, p < .001; Nagelkerke R-square = .638; not shown in tables). Multivariable linear regression (Table 4) indicated that, among past-month opioid nonusers, greater interest in using opioids was associated with reporting greater motives for opioid use (B = 0.75, p < .001), as well as being female (B = 1.08, p < .001), and married/cohabitating (B = −4.08, p < .001; Adjusted R-square = .742).
Table 4.
Multivariable Results from Multivariable Regression Regarding Interest in Use Among Nonusers
| Interest in opioid use among nonusers N = 255 | Interest in marijuana use among nonusers N = 249 | |||||
|---|---|---|---|---|---|---|
| B | CI | P | B | CI | P | |
| Age | 0.02 | −0.01, 0.04 | .140 | 0.02 | 0.00, 0.04 | .038 |
| Sex | ||||||
| Male | Ref | -- | -- | Ref | -- | -- |
| Female | 1.08 | 0.64, 1.53 | <.001 | 0.88 | 0.44, 1.33 | <.001 |
| Race | ||||||
| White | Ref | -- | -- | Ref | -- | -- |
| Black | 0.17 | −0.26, 0.60 | .429 | 0.16 | −0.26, 0.57 | .455 |
| Other | −0.32 | −0.75, 0.12 | .152 | −0.46 | −0.89, −0.04 | .031 |
| Relationship Status | ||||||
| Married/cohabitating | Ref | -- | -- | Ref | -- | -- |
| Other | −3.53 | −4.08, −2.98 | <.001 | −2.47 | −3.09, −1.85 | <.001 |
| Income | ||||||
| ≤1799/month | Ref | -- | -- | Ref | -- | -- |
| >$1799/month | 0.21 | −0.19, 0.61 | .299 | −0.90 | −1.29, −0.50 | <.001 |
| Potential use motives | 0.75 | 0.50, 1.00 | <.001 | 0.76 | 0.62, 0.90 | <.001 |
| Perceived barriers to use | −0.01 | −0.03, 0.01 | .248 | −0.04 | −0.06, −0.02 | <.001 |
| Adjusted R-square | .742 | .773 | ||||
Binary logistic regression indicated that current marijuana use was associated with reporting greater motives for marijuana use (OR = 2.63, CI: 1.80, 3.86, p < .001) and greater barriers to use (OR = 1.15, CI: 1.09, 1.21, p < .001), as well as being female (OR = 0.03, CI: 0.01, 0.13, p < .001), black (vs white, OR = 0.26, CI: 0.07, 0.91, p = .036), and unmarried/not cohabitating (OR = 0.27, CI: 0.09, 0.84, p = 0.024; Nagelkerke R-square = .688; not shown in tables). Multivariable linear regression (Table 4) indicated that, among past-month marijuana nonusers, greater interest in using marijuana was associated with reporting greater motives for marijuana use (B = 0.76, p < .001) and fewer barriers to using marijuana (B = −0.04, p < .001), as well as being older (B = 0.02, p = .038), female (B = 0.88, p < .001), white (vs other race, B = −0.46, p = .031), married/cohabitating (B = −2.47, p < .001), and having lower income (B = −0.90, p < .001; Adjusted R-square = .773).
DISCUSSION
The controversy regarding the medical use of opioids and marijuana has important implications for patient populations, such as PLWH. Given the chronicity of this condition and its health implications, it is important to understand patient perceptions of these treatments and the barriers to effectively managing their HIV-related symptoms. This study provides information on PLWH perceptions and barriers to using opioids and marijuana for symptom management. It is important to note that, in this sample, there was significant overlap in using opioids and marijuana, with 16.1% reporting current use of opioids, 18.1% marijuana, and 15.1% both. Thus, examining motives for use and perceived barriers to use among both users and nonusers provided insights regarding various perceptions of both medical options.
More than half of the overall sample reported that a critical motive for using both drugs was pain. Other motives for use among the overall sample and subsample of past 12-month users was to improve appetite. Among past 12-month users, a common motive for use was to help cope with stress and anxiety. Whereas both opioids and medical marijuana can be effective for pain management,1,2,42 using opioids and/or marijuana to treat anxiety is much more concerning. One qualitative study of adults with evidence of opioid dependence diagnoses43 indicated 5 pathways to opioid addiction, 3 of which were related to pain management (eg, ineffective chronic pain management, use for acute pain episodes, use among those with substance use disorders), one of which related to recreational/non-medical opioid use, and the fifth involving opioid use to cope with emotional distress or mental health issues.43 Along these lines, among the highest-rated perceived barriers to using both drugs were addiction concerns. Thus, there is significant need both to promote appropriate use of these drugs and other medical options to manage pain effectively and to encourage appropriate medical and behavioral management of emotional distress. Also noteworthy is that a highly endorsed barrier to using both drugs was missing symptoms that signal worsening illness. Thus, ongoing surveillance of patient use of opioids or marijuana is critical in managing both their medical conditions and their mental health.
There was one main distinction regarding use motives for the 2 drugs. Nearly 60% of the sample reported potentially using marijuana for pain related to their medical condition, whereas less than 15% of the sample reported this as a motive for using opioids. This distinction may be due to several states with medical marijuana legislation including mental health (eg, anxiety, post-traumatic stress disorder) as conditions for which medical marijuana may be used.16
Greater motives for use correlated with current opioid and marijuana use and with interest in use among nonusers of the respective drugs, consistent with the HBM.34 However, findings regarding barriers to use were less straightforward. Although perceiving fewer barriers to use was associated with interest in using marijuana among nonusers, as theory might suggest,34 perceived barriers to use was not associated with opioid use or interest in opioid use among nonusers, and perceiving greater barriers was associated with reporting current marijuana use. The reasons for these findings are unclear. It is possible that some concerns about using these drugs are more salient when one is considering their use or has had to navigate challenges in order to use these drugs.
Interest in these drugs among nonusers was associated with being female, married/cohabitating, and higher income. The sample of PLWH in this study could have been diagnosed at any time and thus may be outside this critical window. Females may be more likely to engage in health information-seeking,44,45 which may be an indicator of openness to learning about different medical options. Findings regarding marital status and income level are much more difficult to interpret, particularly given the inconsistent findings across regression analyses regarding correlates of motives for use and barriers to use. More specifically, lower income was associated with reporting greater motives across drugs and for both nonusers and users but was only correlated with barriers to using opioids among opioid nonusers, while higher income was associated with greater perceived barriers to using opioids among past-year opioid users. This latter point highlights the need to distinguish users from nonusers when examining motives for use and barriers to use. Whereas motives and barriers were similar across drugs, the correlates of number of motives and the magnitude of the barriers were distinct, which warrants further examination.
With regard to information sources, distinctions between individuals’ actual sources of information about these treatment options versus their preferred information sources also were interesting to note from a theoretical perspective.35,36 The most frequently endorsed information source for opioids or marijuana was a friend or a family member. One major distinction between drugs was that over 75% of the sample reported using websites or blogs for information on opioids whereas only about 10% reported this as an information source for marijuana. In this study, we found that patients’ most preferred source of information regarding opioids and marijuana were websites and blogs. There were 2 major distinctions among preferred information sources between drugs. Over 35% of the sample reported a naturopath or herbalist as a preferred source of information whereas less than 5% reported it as a preferred information source for marijuana. Over 35% of the sample reported social media as a preferred source of information for marijuana, whereas less than 5% reported it as a preferred information source for opioids. A prior study45 indicated that there is an age, socio-economic, and ethnic divide among US adults’ health information-seeking behaviors with regard to active seeking and sources of information. For example, being younger, more educated, and higher income predicted using the Internet for health information-seeking, whereas being older, having low internet skill, and being Hispanic were associated with using healthcare providers or traditional media (eg, print, magazines) as information sources.45 The online/social media recruitment strategy used in this study may have resulted in a sample particularly receptive to using these online sources for health information.
Our study has implications for research and practice. With regard to research, advances are needed with respect to how information is provided about use of opioids and marijuana for symptom management. Moreover, research is needed to inform best practices regarding medical management of symptoms using opioids and marijuana and how to predict negative consequences (eg, addiction potential). In terms of practice, healthcare providers need to be cognizant of the use motives and barriers to use to have effective conversations about drug use with patients and to make appropriate recommendations.
Despite the strengths of our study, its generalizability is limited given that the sample was recruited via social networking sites. In addition, the wording of the advertisements and strategies used for social media recruitment may have led to the recruitment of a disproportionate number of opioid and marijuana users. We also had a relatively low response rate and used self-report assessments, which may lead to bias. In addition, some measures were adapted to assess perceptions (eg, use motives and barriers) across drugs, with some of these items potentially being irrelevant for one of the drugs (eg, constipation as a barrier to marijuana use). Moreover, the use motives and barriers included in the assessments were not exhaustive. For example, we did not assess social stigma of taking opioids or marijuana and whether this hindered patients from using these medical options. This is significant, given that research has documented that social stigma is among the most common reasons patients refuse to take opioids for the treatment of pain10,11 and also is an important concern with regard to medical marijuana use.46,47 Additionally, some differences in measures pertaining to opioids versus marijuana (eg, index scores for motives) were small, highlighting the need to consider whether such differences are clinically meaningful. Additionally, we did not assess all potential factors that could impact opioid or marijuana use, including where participants actually accessed the drug they used. This is, in part, why we did not include state policies regarding opioid and medical marijuana use in these analyses. Finally, the cross-sectional nature of this study limits the ability to make causal attributions.
In conclusion, findings suggest that PLWH show greater interest in marijuana versus opioids, generally indicate more motives they may use marijuana versus opioids, and perceive fewer barriers to using marijuana compared to opioids. Understanding patients’ perceptions about prescription analgesics is an essential component for managing symptoms and improving quality of life for PLWH. Thus, clinicians must attend to patients differentially using and perceiving these drugs to ensure appropriate use. Moreover, accurate and effective sources of information are needed to educate and support patients in making decisions about how to treat their symptoms.
Acknowledgements
This research was supported by the Atlanta Clinical & Translational Science Institute Research Seed Grant Program (now the Georgia Clinical and Translational Science Alliance) (PHS Grant UL1TR000454 from the National Center for Advancing Translational Sciences, National Institute of Health). Dr. Berg is also supported by other NCI funding (R01CA215155-01A1, PI: Berg; R01CA179422-01, PI: Berg; R01CA239178-01A1, MPIs: Berg, Levine; P30CA138292, PI: Curran) and the US Fogarty International Center / National Cancer Institute (1R01TW010664-01, MPIs: Berg, Kegler), and the NIEHS/Fogarty (D43ES030927-01, MPIs: Berg, Marsit, Sturua). Ms. Vu. is supported by the National Cancer Institute (F31 CA243220-01, PI: Vu).
Footnotes
Conflict of Interest Disclosure Statement
The authors declare no conflicts of interest.
References
- 1.Lucas P. Cannabis as an adjunct to or substitute for opiates in the treatment of chronic pain. J Psychoactive Drugs. 2012;44(2):125–133. [DOI] [PubMed] [Google Scholar]
- 2.Krashin DL, Merrill JO, Trescot AM. Opioids in the management of HIV-related pain. Pain Physician. 2012;15(3 Suppl):ES157–ES168. [PubMed] [Google Scholar]
- 3.Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 4.Paice JA, Portenoy R, Lacchetti C, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(27):3325–3345. [DOI] [PubMed] [Google Scholar]
- 5.Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett DS, Carr DB. Opiophobia as a barrier to the treatment of pain. J Pain Palliat Care Pharmacother. 2002;16(1):105–109. [PubMed] [Google Scholar]
- 7.National Institute on Drug Abuse. Drugs of Abuse: Opioids. Bethesda, MD: National Institute on Drug Abuse. 2015. http://www.drugabuse.gov/drugs-abuse/opioids. Accessed September 4, 2020. [Google Scholar]
- 8.Straus MM, Ghitza UE, Tai B. Preventing deaths from rising opioid overdose in the US – the promise of naloxone antidote in community-based naloxone take-home programs. Subst Abuse Rehabil. 2013;2013(4):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths – United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51):1378–1382. [DOI] [PubMed] [Google Scholar]
- 10.Shah S, Diwan S. Methadone: does stigma play a role as a barrier to treatment of chronic pain? Pain Physician. 2010;13(3):289–293. [PubMed] [Google Scholar]
- 11.Carr DB. Patients with pain need less stigma, not more. Pain Med. 2016;17(8):1391–1393. [DOI] [PubMed] [Google Scholar]
- 12.Page R, Blanchard E. Opioids and cancer pain: patients’ needs and access challenges. J Oncol Pract. 2019;15(5):229–231. [DOI] [PubMed] [Google Scholar]
- 13.Boehnke KF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain. 2016;17(6):739–744. [DOI] [PubMed] [Google Scholar]
- 14.Vyas MB, LeBaron VT, Gilson AM. The use of cannabis in response to the opioid crisis: a review of the literature. Nurs Outlook. 2018;66(1):56–65. [DOI] [PubMed] [Google Scholar]
- 15.Bradford AC, Bradford WD. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Aff (Millwood). 2016;35(7):1230–1236. [DOI] [PubMed] [Google Scholar]
- 16.National Conference on State Legislatures. State Medical Marijuana Laws. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Published August 1, 2019. Accessed September 4, 2020.
- 17.Goyal S, Kubendran S, Kogan M, Rao YJ. High expectations: the landscape of clinical trials of medical marijuana in oncology. Complement Ther Med. 2020;49:102336. [DOI] [PubMed] [Google Scholar]
- 18.Bruce RD, Merlin J, Lum PJ, et al. 2017 HIVMA of IDSA Clinical practice guidelines for the management of chronic pain in patients living with HIV. Clin Infect Dis. 2017;65(10):e1–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taddei TH, Lo Re V 3rd, Justice AC. HIV, aging, and viral coinfections: taking the long view. Curr HIV/AIDS Rep. 2016;13(5):269–278. [DOI] [PubMed] [Google Scholar]
- 20.Boehnke KF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. J Pain. 2016;17(6):739–744. [DOI] [PubMed] [Google Scholar]
- 21.Abrams DI, Couey P, Shade SB, et al. Cannabinoid-opioid interaction in chronic pain. Clin Pharmacol Ther. 2011;90(6):844–851. [DOI] [PubMed] [Google Scholar]
- 22.Haroutounian S, Ratz Y, Ginosar Y, et al. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: a prospective open-label study. Clin J Pain. 2016;32(12):1036–1043. [DOI] [PubMed] [Google Scholar]
- 23.Bennett M, Paice JA, Wallace M. Pain and opioids in cancer care: benefits, risks, and alternatives. Am Soc Clin Oncol Educ Book. 2017(37):705–713. [DOI] [PubMed] [Google Scholar]
- 24.Elikkottil J, Gupta P, Gupta K. The analgesic potential of cannabinoids. J Opioid Manag. 2009;5(6):341–357. [PMC free article] [PubMed] [Google Scholar]
- 25.Ball SC. Increased longevity in HIV: caring for older HIV-infected adults. Care Manag J. 2014;15(2):76–82. [DOI] [PubMed] [Google Scholar]
- 26.Lewis-Patterson P, Palos GR, Dains J, Jackson TL. Cancer prevention in the survivorship setting. Semin Oncol Nurs. 2016;32(3):291–305. [DOI] [PubMed] [Google Scholar]
- 27.Farquhar-Smith P, Brown MRD. Persistent pain in cancer survivors: pathogenesis and treatment options. Pain Clin Updates. 2016;24(4):1–8. [Google Scholar]
- 28.Glare PA, Davies PS, Finlay E, et al. Pain in cancer survivors. J Clin Oncol. 2014;32(16):1739–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, et al. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag. 2016;51(6):1070–1090, e1079. [DOI] [PubMed] [Google Scholar]
- 30.American Cancer Society. Managing Cancer as a Chronic Illness. https://www.cancer.org/content/dam/CRC/PDF/Public/7871.00.pdf. Published January 14, 2019. Accessed September 3, 2020.
- 31.Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol. 2006;24(32):5132–5137. [DOI] [PubMed] [Google Scholar]
- 32.Bhatia R, Hartman C, Kallen MA, et al. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: results from the Steps Study. AIDS Behav. 2011;15(6):1161–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Althoff KN, Smit M, Reiss P, Justice AC. HIV and ageing: improving quantity and quality of life. Curr Opin HIV AIDS. 2016;11(5):527–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. [DOI] [PubMed] [Google Scholar]
- 35.Lalazaryan A, Zare-Farashbandi F. A review of models and theories of health information seeking behavior. Int J Health Syst Disaster Manag. 2014;2(4):193–203. [Google Scholar]
- 36.Wilson TD. Human information behavior. Inf Sci. 2000;3(2):49–56. [Google Scholar]
- 37.Cutilli CC. Seeking health information: what sources do your patients use? Orthop Nurs. 2010;29(3):214–219. [DOI] [PubMed] [Google Scholar]
- 38.Ramo DE, Prochaska JJ. Broad reach and targeted recruitment using Facebook for an online survey of young adult substance use. J Med Internet Res. 2012;14(1):e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lankenau SE, Kioumarsi A, Reed M, et al. Becoming a medical marijuana user. Int J Drug Policy. 2018;52:62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pergam SA, Woodfield MC, Lee CM, et al. Cannabis use among patients at a comprehensive cancer center in a state with legalized medicinal and recreational use. Cancer. 2017;123(22):4488–4497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyd-Seale D, Wilkie DJ, Kim YO, et al. Pain barriers: psychometrics of a 13-item questionnaire. Nurs Res. 2010;59(2):93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park J-Y, Wu L-T. Prevalence, reasons, perceived effects, and correlates of medical marijuana use: a review. Drug Alcohol Depen. 2017;177:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stumbo SP, Yarborough BJ, McCarty D, et al. Patient-reported pathways to opioid use disorders and pain-related barriers to treatment engagement. J Subst Abuse Treat. 2017;73:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ren C, Deng Z, Hong Z, Zhang W. Health information in the digital age: an empirical study of the perceived benefits and costs of seeking and using health information from online sources. Health Info Libr J. 2019;36(2):153–167. [DOI] [PubMed] [Google Scholar]
- 45.Jacobs W, Amuta AO, Alvares C. Health information seeking in the digital age: an analysis of health information seeking behavior among US adults. Cogent Soc Sci. 2017;3(1):1302785. [Google Scholar]
- 46.Satterlund TD, Lee JP, Moore RS. Stigma among California’s medical marijuana patients. J Psychoactive Drugs. 2015;47(1):10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bottorff JL, Bissell LJ, Balneaves LG, et al. Perceptions of cannabis as a stigmatized medicine: a qualitative descriptive study. Harm Reduct J. 2013;10:2. [DOI] [PMC free article] [PubMed] [Google Scholar]


