Summary
Background:
Emotional eating is associated with obesity, though less is known regarding factors that predict emotional eating episodes in children and adolescents.
Objectives:
To investigate whether moderate to vigorous physical activity (MVPA) or total activity counts 60 minutes prior to psychological stress predicted stress-related eating and positive emotional eating (ie, eating while happy), and whether adiposity (z-BMI) moderated these associations.
Methods:
Participants were drawn from a prior study of siblings (N = 77; mean age = 15.4 ± 1.4 years) discordant for weight status (39 non-overweight siblings, 38 siblings with overweight/obesity) who completed an ecological momentary assessment protocol with accelerometer-based assessment of physical activity.
Results:
Greater MVPA was associated with lower stress-related eating across the sample. Lower total activity (between-person effects) and lower MVPA (within-person effects) were associated with greater stress-related eating for siblings with greater z-BMI. Greater total activity was associated with lower positive emotional eating for siblings with lower z-BMI (between- and within-person).
Conclusions:
Findings demonstrate potential regulating effects of prior physical activity on emotional eating at the individual and momentary level, though there are nuances depending on z-BMI. Future work is needed to examine underlying mechanisms and timescale of effects, and particularly the extent to which enhancing MVPA time among youth with z-BMI may mitigate momentary risk of stress-related eating episodes.
Keywords: adolescents, ecological momentary assessment, emotional eating, physical activity, stress
1 |. INTRODUCTION
Excess adiposity during childhood and adolescence represents a serious and growing global health problem. It is estimated that over 330 million children worldwide have overweight or obesity, with obesity affecting approximately one in five children and adolescents in the United States.1,2 This is concerning given that obesity during childhood and adolescence increases risk of developing psychiatric disorders, physical health problems and non-communicable diseases, as well as the likelihood of maintaining excess weight into adulthood.1 While prevention and intervention efforts require multifaceted, systemic approaches, at the individual-level, it is imperative to understand and effectively target energy-balance behaviours in the daily lives of youth. In particular, considerable evidence suggests emotional eating tendencies are important contributors to obesity,3,4 and prior research has shown associations between eating psychopathology and negative affectivity among children with overweight and obesity.5 However, less is known regarding factors that may influence episodes of emotional eating among youth in naturalistic settings.
Emotional eating behaviour (typically defined as eating in response to negative emotions or stress) tends to emerge during adolescence and has been consistently associated with greater energy intake (particularly in the form of fat and sugar) and obesity.3,4 Data from twin research also suggest emotional eating is a learned behaviour that is more strongly shaped by environmental compared to genetic factors.6 This is consistent with the broader literature implicating psychological stress and stress reactivity as important determinants of excess energy intake and adiposity, as well as research in children and adolescents showing associations between emotional eating tendencies, stress, and poorer food choice and diet quality.7–12 In addition, while historically most studies have conceptualized emotional eating as eating in the context of negative emotions, there has been increasing research on the role of positive emotional eating (ie, eating in the context of positive emotions) and its relevance for eating and weight disorders. For instance, positive emotional eating in adults is associated with greater food intake, binge eating, and overeating in community samples.13–15 Together this research underscores the need to further understand individual and momentary factors that potentiate or mitigate emotional eating in order to advance obesity prevention and intervention approaches.
Physical activity may be one such factor that is important to consider in the context of eating regulation. That is, alongside its direct influence on adiposity via energy balance, physical activity may exert an important regulating effect on psychological stress, eating, and emotional functioning. Extant evidence shows that greater amounts of physical activity are correlated with better mental health (eg, lower negative and greater positive affect), as well as better appetite regulation, reduced food cue responsivity, and less binge eating.16–19 The effects of physical activity on increased positive and decreased negative affect, eating, and appetite may also unfold over relatively short timescales (eg, a few hours).20–22 Thus, physical activity could further impact weight regulation via influences on emotional eating behaviour, both at the individual and momentary levels.
However, there may be paradoxical effects of physical activity across the weight spectrum. The potential beneficial effects of physical activity on emotional eating behaviour may differ between youth with and without overweight/obesity given that individuals with overweight/obesity engage in less physical activity and have more variable affective responses to physical activity.23–25 Youth with overweight or obesity could find exercise less enjoyable, perhaps in part due to appearance concerns, weight stigma, and/or physical discomfort.26 Therefore, physical activity may not exert a regulatory or stress-reducing function in these children. Furthermore, greater weight (ie, measured in terms of body mass index percentile or z-score [z-BMI]) has been associated with greater food enjoyment, emotional eating, and lower satiety among children and adolescents.27–29 This suggests youth with overweight and obesity may experience greater reinforcement from food and be more likely to engage in eating behaviours as means of regulating states of high negative and/or low positive affect.9,10,30 Consequently, their amount of physical activity may not be potent enough to exert regulating effects on these processes and behaviours.
Together, evidence suggests that engaging in greater amounts of physical activity could buffer against psychological stress and emotional eating in children and adolescents. However, the effect of physical activity on psychological stress and emotional eating may not be the same for youth with overweight/obesity given that they may experience less affect regulation from physical activity,25 as well as increased food-related reward responsiveness.30 In addition, it is not clear whether such relationships may be specific to more intense physical activity (ie, moderate to vigorous physical activity [MVPA]) as opposed to overall lifestyle activity, given that research in youth has tended to focus on MVPA or sedentary behaviour.31 To address these questions, this study utilized naturalistic assessment methods (ie, ecological momentary assessment [EMA] paired with accelerometers) in a sample of weight-discordant siblings to assess (a) relationships between physical activity (MVPA and total activity counts) and subsequent emotional eating, and (b) the extent to which weight status (ie, BMI z-score [z-BMI]) moderated these associations. A sample of weight-discordant siblings was used to systematically investigate moderating effects of z-BMI across the weight spectrum, adjusting for shared environmental influences of family. Given that emotional eating is shaped by environmental factors, this design is particularly useful to examine experiences that are not shared among discordant siblings raised in the same family.
Emotional eating was operationalized in the present study as (a) psychological stress-related eating given the relevance of psychological stress for eating behaviours in obesity7 and (b) positive emotional eating (eg, eating while happy) given the increasing recognition of its relevance for obesogenic eating behaviours.15 It was hypothesized that when individuals engaged in greater amounts of physical activity (ie, greater MVPA minutes and total physical activity counts) in the hour preceding EMA recordings, relative to their own average level of MVPA and activity counts, they would be less likely to report psychological stress-related eating (ie, eating while feeling stressed compared to eating while not feeling stressed) at the next EMA recording. A second hypothesis was that these momentary associations would be statistically weaker among siblings with overweight/obesity, such that the associations between physical activity (ie, MVPA minutes and activity counts) and emotional eating would be weaker among siblings with lower z-BMI. While primary hypotheses were momentary (ie, within-person) in nature, the independent and interactive effects of physical activity and z-BMI were also examined at the individual (ie, between-person) level.
2 |. METHODS
2.1 |. Participants
Participants were drawn from a larger study of 40 same-sex biological sibling pairs (N = 80; age 13–17, no more than 4 years apart) who were discordant on weight status (ie, one sibling was above the 85th BMI percentile and the other sibling was below the 70th BMI percentile). The aim of the larger study was to evaluate putative factors contributing to differences in energy-balance behaviours and adiposity among weight discordant siblings. A discordant sibling design allows for controlling for approximately 50% of the genetic variability between siblings, as well as a portion of variance associated with shared environmental factors (ie, environmental factors that make the siblings similar to one another; eg, same parents, neighbourhood, etc.).
Recruitment for this parent study was conducted using newspaper advertisement, as well as a database of families who had inquired about previous studies. Phone screens were used to collect children’s height, weight, a brief medical history, and ethnic background. Exclusion criteria included families with children below the 10th BMI percentile, current psychopathology or developmental disability, and/or if either child was on medications or had conditions that could influence their mobility or activity level. Initially, 930 families were contacted by study staff regarding the study; 234 of these families did not reply to study staff after initial contact and 652 of these families were not eligible for the study. The most common reason for ineligibility was that siblings within families were not discordant for weight. There were also families that did not have same gender children, had children who fell outside of the age range, had children who were adopted, had twins, had conditions that made it so they could not be in the study (eg, food allergies, developmental delay, or medical issues that could affect their ability to be physically active), or one or both children did not like the study foods used in the parent study. Some families also could not schedule appointments, or scheduled and did not show up. In total, 44 families were enrolled in the study, however, four dropped out before completion. Social and Behavioral Sciences Institutional Review Board at the University of Buffalo approved all study procedures. Parents provided written informed consent and adolescents provided assent for study participation. The present study excluded three participants due to missing data (see Results section below), resulting in a final analytic sample of 77 (mean age = 15.36 ± 1.4 years; 41.6% female; 92.5% Caucasian).
2.2 |. Procedures
Siblings and parents attended a study visit during which they completed a series of measures and laboratory assessments, which have been previously described in detail.32–34 Following the study visit, participants’ momentary affect and eating were captured using EMA for seven consecutive days (five weekdays, two weekend days). EMA was administered using a study-provided cell phone that delivered text messages to participants during the study. Participants received text messages approximately every 2 hours between 3:00 PM and 9:00 PM on weekdays and between 10:00 AM and 10:00 PM on weekend days. During the EMA protocol, participants also wore a waist-worn accelerometer (MTI Actigraph; Pensacola, Florida) and received instructions on use, including appropriate care and placement. Participants were asked to wear the Actigraph at least 10 hours each day. Research staff kept a record of participants’ EMA responses and followed up the next working day if there was a lack of clarity regarding responses.
2.3 |. Measures
2.3.1 |. BMI z-score
Participants’ height and weight were measured with an electronic scale (Model BWB-800S, Tanita, Portage, Michigan) and digital stadiometer (Model PE-AIM-101, Perspective Enterprises). Participants removed their shoes, outer wear, belts, and emptied their pockets prior to being weighed. Weight was measured to the nearest 0.01 kg. Height was measured three times (to the nearest 0.1 cm), unless the first two measurements matched exactly. Means of these height measurements and measured weight were used to calculate BMI (kg/m2) percentiles and z-scores using the Center for Disease Control and Prevention growth charts.35
2.3.2 |. EMA-measured affect and eating
During the EMA protocol participants were asked to report on their current behaviours and affective states. The text message asked participants to indicate their current activity (What were you doing?), to which they could respond eating, physical activity, screen time, or other sedentary behaviour. Participants also reported on their current affective states (eg, Are you happy? and Are you stressed?) with a yes or no response format. The present study used EMA responses in which participants reported they were currently eating. These episodes were then coded as stress-related eating if participants reported currently feeling stressed, and positive emotional eating episodes if participants reported currently feeling happy.
2.3.3 |. Physical activity
Physical activity was assessed by the MTI Actigraph (Pensacola, Florida) and operationalized as total activity counts and minutes of MVPA. The Actigraph is a well-validated measure of objective physical activity in adolescents.36–38 The Actigraph was initialized for 15-seconds epochs, and thresholds for activity were consistent with national surveillance data.39,40 Age-specific thresholds for children’s activity were adjusted by applying the Freedson prediction equation.41,42 Downloaded data were further processed using R to create time windows of Actigraph activity counts (ie, an index of average total physical activity) and MVPA minutes before EMA prompts. Accumulated minutes of MVPA and activity counts were derived from 60-minute time windows before all EMA prompts; only windows with at least two-thirds valid wear time (40 minutes) were included in analyses. Non-wear time (>60 continuous minutes of zero activity counts) and non-valid days (<10 hours of wear time) were identified; all non-wear time and non-valid days were removed from analyses. The selection of 60-minute windows was based on recent EMA research in youth that has found effects of activity on affect and eating behaviours using similar length time windows.31,43
2.4 |. Statistical analyses
EMA recordings were time-matched to Actigraph-measured activity counts and MVPA minutes in the 60 minutes before each recording. Separate generalized estimating equations (GEEs) were used to examine hypotheses. In each model, siblings were nested within family, and the effects of physical activity variables (ie, activity counts or MVPA minutes) were separated into within-person (ie, person-mean centred) and between-person (ie, grand-mean centred) components. That is, within-person associations indicate the degree to which changes in the physical activity variable (ie, total activity counts or MVPA minutes during the 60 minutes prior to EMA recordings), relative to an individual’s own mean, are related to the dependent variable (ie, likelihood of reporting stress-related or positive emotional eating), whereas between-person associations reflect the degree to which an individual’s average amount of physical activity across the EMA protocol, relative to other individuals, is associated with stress-related or positive emotional eating.
In each GEE, the between- and within-person effects of physical activity amounts were included as predictors of stress-related and positive emotional eating reported at EMA recordings to examine the first hypothesis. To examine the second hypothesis, each GEE also included the main effect of z-BMI (continuous variable) and the two-way interactions of z-BMI and between- and within-person physical activity (ie, total activity counts or MVPA minutes). The outcomes examined were the likelihood of psychological stress-related eating and positive emotional eating. Psychological stress-related eating was operationalized as the likelihood of reporting feeling stressed while eating (compared to not reporting feeling stressed while eating), while positive emotional eating was operationalized as the likelihood of reporting feeling happy while eating (compared to not reporting feeling happy while eating).
Age and gender were included as covariates in all models. All GEEs specified an AR1 serial autocorrelation to account for dependence within the nested data, and a binary logistic function was given the dichotomous nature of dependent variables. GEEs were conducted using SPSS version 25.
3 |. RESULTS
Three participants were excluded due to insufficient wear time, resulting in a final analytic sample of 77 siblings. The mean age gap between siblings within the same family was 2.2 ± .9 years. Descriptive information for the final analytic sample is shown in Table 1. Each participant reported an average of 32.3 ± 4.1 of 34 EMA recordings during the study; feeling stressed was endorsed at 9.7% of recordings made while eating, while feeling happy was reported at 92.9% of recordings made while eating. Resemblance within sibling pairs in the independent and dependent variables was examined using intraclass correlation coefficients (ICCs). Consistent with prior research,34 ICC values were interpreted as no family similarity for values ranging .00 to .10, slight similarity for scores ranging .11 to .40, fair amounts of similarity for scores ranging .41 to .60, moderate similarity for scores ranging .61 to .80, and high similarity for amounts exceeding .81. ICC values revealed was little familial resemblance for total stress-related eating episodes (ICC = .12), total positive emotional eating episodes (ICC = .04), mean MVPA minutes prior to EMA prompts (ICC = .04), and mean activity counts prior to EMA prompts (ICC = .11). When siblings with and without overweight/obesity were compared as separate groups, they did not differ with respect to the proportion of EMA recordings made while eating, or the proportion of endorsements of feeling stressed or happy while eating (ps = .09–.521). They were also not different with respect to average daily Actigraph wear time, average daily MVPA minutes, average daily activity counts, MVPA minutes or activity counts prior to EMA recordings, total number of EMA recordings completed EMA (ps = .333-.973). Similarly, there were no gender differences for these variables (ps = .058–.864). Age was not associated with average daily Actigraph wear time, total number of EMA recordings completed (Spearman ρ = −.01–.04, P = .726–.922), or average daily activity counts (ρ = −.22, P = .066). However, age was negatively associated with average daily MVPA minutes (ρ = −.37, P = .001), as well as MVPA minutes (ρ = −.37, P = .001) and activity counts (ρ = −.29, P = .010) measured within 60 minutes prior to EMA recordings. Participant z-BMI was not associated with any of these variables (ρ = .01–.15, P = .203–.944), except for a positive association with activity counts prior to EMA recordings (ρ = −23, P = .047).
TABLE 1.
Descriptive statistics
| Total sample (N = 77) | Siblings within normal weight (N = 39) | Siblings with overweight/obesity (N = 38) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | Minimum | Maximum | M | SD | Minimum | Maximum | M | SD | Minimum | Maximum | |
| z-BMI | 0.78 | 0.89 | −1.45 | 2.42 | 0.03 | 0.52 | −1.45 | 0.65 | 1.56 | 0.35 | 1.05 | 2.42 |
| Age | 15.36 | 1.43 | 13.01 | 17.84 | 15.64 | 1.42 | 13.01 | 17.84 | 15.06 | 1.39 | 13.10 | 17.75 |
| Daily wear time (hours) | 13.79 | 1.31 | 10.68 | 19.90 | 13.78 | 1.00 | 11.94 | 15.67 | 13.80 | 1.60 | 10.68 | 19.90 |
| Daily MVPA time (minutes) | 23.38 | 18.34 | 0.00 | 75.50 | 24.59 | 20.49 | 2.67 | 75.50 | 22.07 | 15.88 | 0.00 | 73.75 |
| MVPA minutes before EMA | 1.42 | 1.33 | 0.00 | 6.42 | 1.28 | 1.30 | 0.04 | 5.56 | 1.58 | 1.37 | 0.00 | 6.42 |
| Activity counts before EMA | 20 231.65 | 8504.27 | 6730.15 | 46 770.53 | 19 305.28 | 9378.46 | 6730.15 | 46 770.53 | 21 208.11 | 7478.01 | 8584.93 | 43 103.21 |
| Completed EMA prompts | 32.75 | 5.76 | 7.00 | 68.00 | 33.38 | 6.58 | 18.00 | 68.00 | 32.11 | 4.76 | 7.00 | 34.00 |
Abbreviations: EMA, ecological momentary assessment; MVPA, moderate to vigorous physical activity; z-BMI, body mass index z-score.
GEE results are displayed in Table 2. There were no significant main effects of gender, age, z-BMI, within-person MVPA minutes, or the interaction of z-BMI and between-person MVPA minutes predicting stress-related eating. There was a between-person effect of total MVPA time (B = −1.55, SE = .56, P = .006) predicting psychological stress-related eating, indicating participants who evidenced greater total MVPA minutes across the study reported lower stress-related eating. At the momentary level, there was a significant interaction of within-person MVPA minutes and z-BMI predicting episodes of stress-related eating (B = −.50, SE = .17, P = .003). As shown in Figure 1, when participants with greater z-BMI engaged in less MVPA in the hour before EMA recordings (relative to their average amount), they were more likely to report eating while stressed compared to eating without feeling stressed. Conversely, participants with lower z-BMI were more likely to report eating while stressed when they reported increased MVPA (relative to their average amount) prior to EMA recordings.
TABLE 2.
Generalized estimating equation results predicting the occurrence of stress-related and positive emotional eating
| DV: Stress-related eating | DV: Positive emotional eating | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||||||
| MVPA models | B | SE | Lower | Upper | Wald χ2 | P | B | SE | Lower | Upper | Wald χ2 | P |
| Intercept | −3.01 | 0.58 | −4.14 | −1.89 | 27.44 | <.001 | 2.14 | 0.50 | 1.16 | 3.11 | 18.43 | <.001 |
| Gender | −1.58 | 0.90 | −3.35 | 0.18 | 3.09 | .079 | 1.06 | 0.83 | −0.57 | 2.70 | 1.63 | .202 |
| Age | 0.20 | 0.25 | −0.30 | 0.69 | 0.61 | .433 | −0.09 | 0.26 | −0.59 | 0.42 | 0.11 | .741 |
| z-BMI | 0.59 | 0.55 | −0.49 | 1.67 | 1.15 | .283 | 0.13 | 0.57 | −0.98 | 1.24 | 0.05 | .821 |
| MVPA (between) | −1.55 | 0.56 | −2.64 | −0.45 | 7.68 | .006 | 0.14 | 0.50 | −0.85 | 1.12 | 0.08 | .784 |
| MVPA (within) | −0.04 | 0.18 | −0.39 | 0.32 | 0.04 | .835 | −0.09 | 0.13 | −0.35 | 0.17 | 0.44 | .506 |
| z-BMI x MVPA (between) | 0.02 | 0.45 | −0.86 | 0.91 | <0.01 | .957 | 0.97 | 0.83 | −0.65 | 2.59 | 1.38 | .239 |
| z-BMI x MVPA (within) | −0.50 | 0.17 | −0.82 | −0.17 | 8.98 | .003 | 0.36 | 0.33 | −0.28 | 1.01 | 1.23 | .268 |
| Activity count models | ||||||||||||
| Intercept | −2.37 | 0.55 | −3.45 | −1.29 | 18.45 | <.001 | 2.16 | 0.41 | 1.35 | 2.97 | 27.57 | <.001 |
| Gender | −1.75 | 0.98 | −3.67 | 0.17 | 3.20 | .073 | 1.09 | 0.76 | −0.41 | 2.59 | 2.03 | .154 |
| Age | 0.16 | 0.23 | −0.29 | 0.62 | 0.49 | .483 | 0.01 | 0.24 | −0.46 | 0.48 | <0.01 | .962 |
| z-BMI | −0.13 | 0.55 | −1.20 | 0.94 | 0.06 | .808 | −0.08 | 0.31 | −0.69 | 0.54 | 0.06 | .802 |
| Activity (between) | <−0.01 | <0.01 | <−0.01 | <−0.01 | 5.16 | .023 | <0.01 | <0.01 | <−0.01 | <0.01 | 0.19 | .659 |
| Activity (within) | <0.01 | <0.01 | <−0.01 | <0.01 | 1.09 | .297 | <−0.01 | <0.01 | <−0.01 | <−0.01 | 9.37 | .002 |
| z-BMI x Activity (between) | <−0.01 | <0.01 | <−0.01 | <−0.01 | 5.22 | .022 | <0.01 | <0.01 | <0.01 | <0.01 | 4.69 | .030 |
| z-BMI x Activity (within) | <−0.01 | <0.01 | <−0.01 | <0.01 | 0.87 | .351 | <0.01 | <0.01 | <0.01 | <0.01 | 7.22 | .007 |
Abbreviations: CI, confidence interval; DV, dependent variable; EMA, ecological momentary assessment; MVPA, moderate to vigorous physical activity; z-BMI, body mass index z-score.
Note: Between = grand-mean centred variable; within = person-mean centred variable. MVPA and activity counts were assessed within 60 minutes before EMA ratings. Gender was coded such that girls were the reference category. Bolded values indicate significant effects at p <.05.
FIGURE 1.
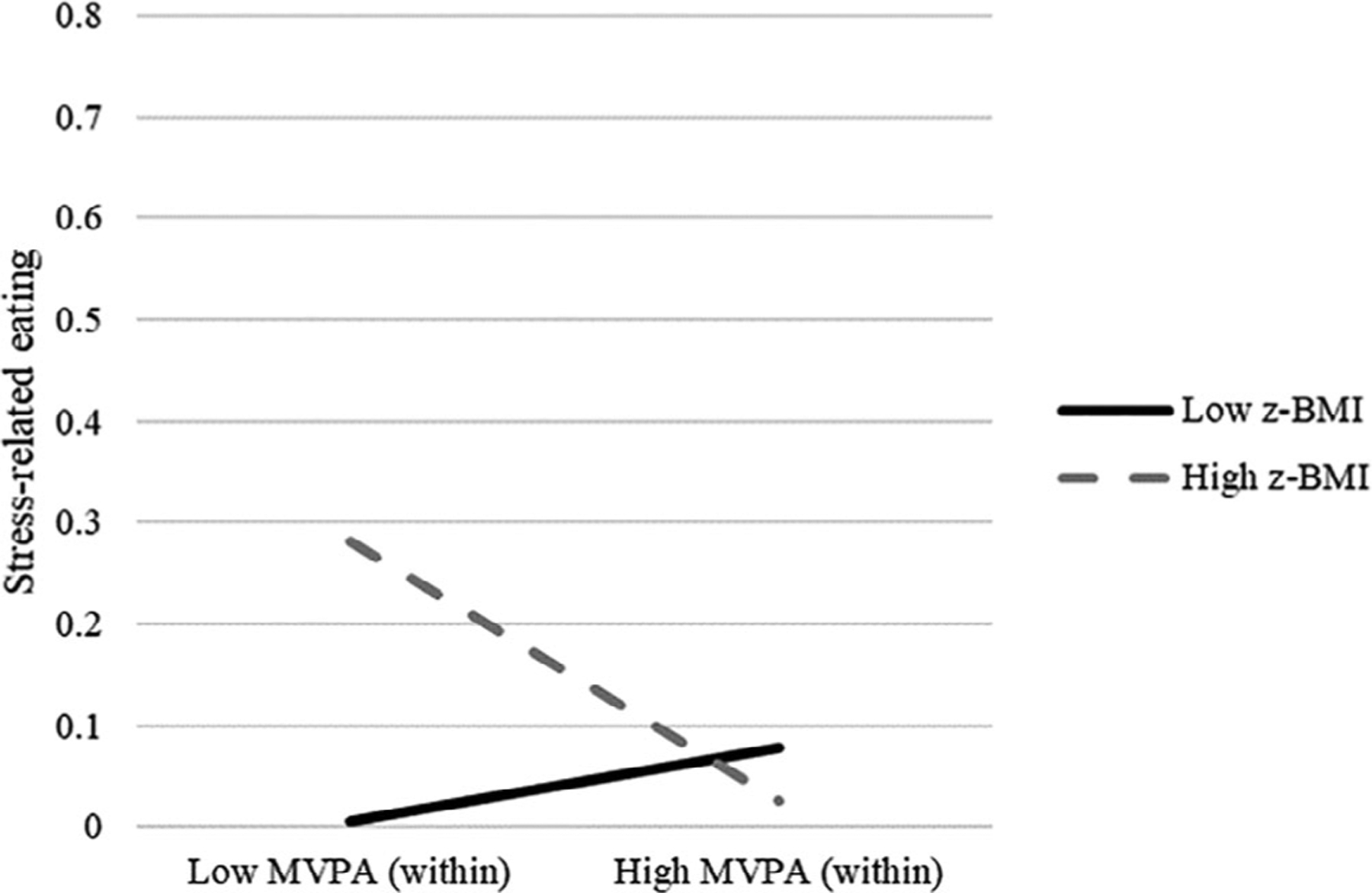
Interaction of body mass index z-score and within-person moderate to vigorous physical activity time in the hour before ecological momentary assessment recordings (relative to their own average amount) predicting likelihood of stress-related eating. High and low values reflect 1 SD above and below individual/sample means, respectively
Regarding activity counts in relation to stress-related eating, there were no significant main effects of gender, age, z-BMI, within-person activity counts, or the interaction of z-BMI and within-person activity counts predicting stress-related eating. However, there was a main effect of between-person activity counts (B = <−.01, SE < .01, P = .023) and an interaction of between-person activity counts and z-BMI predicting stress-related eating (B = <−.01, SE < .01, P = .023), such that participants with greater z-BMI and lower total activity reported the greatest stress-related eating across the EMA protocol (Figure 2).
FIGURE 2.
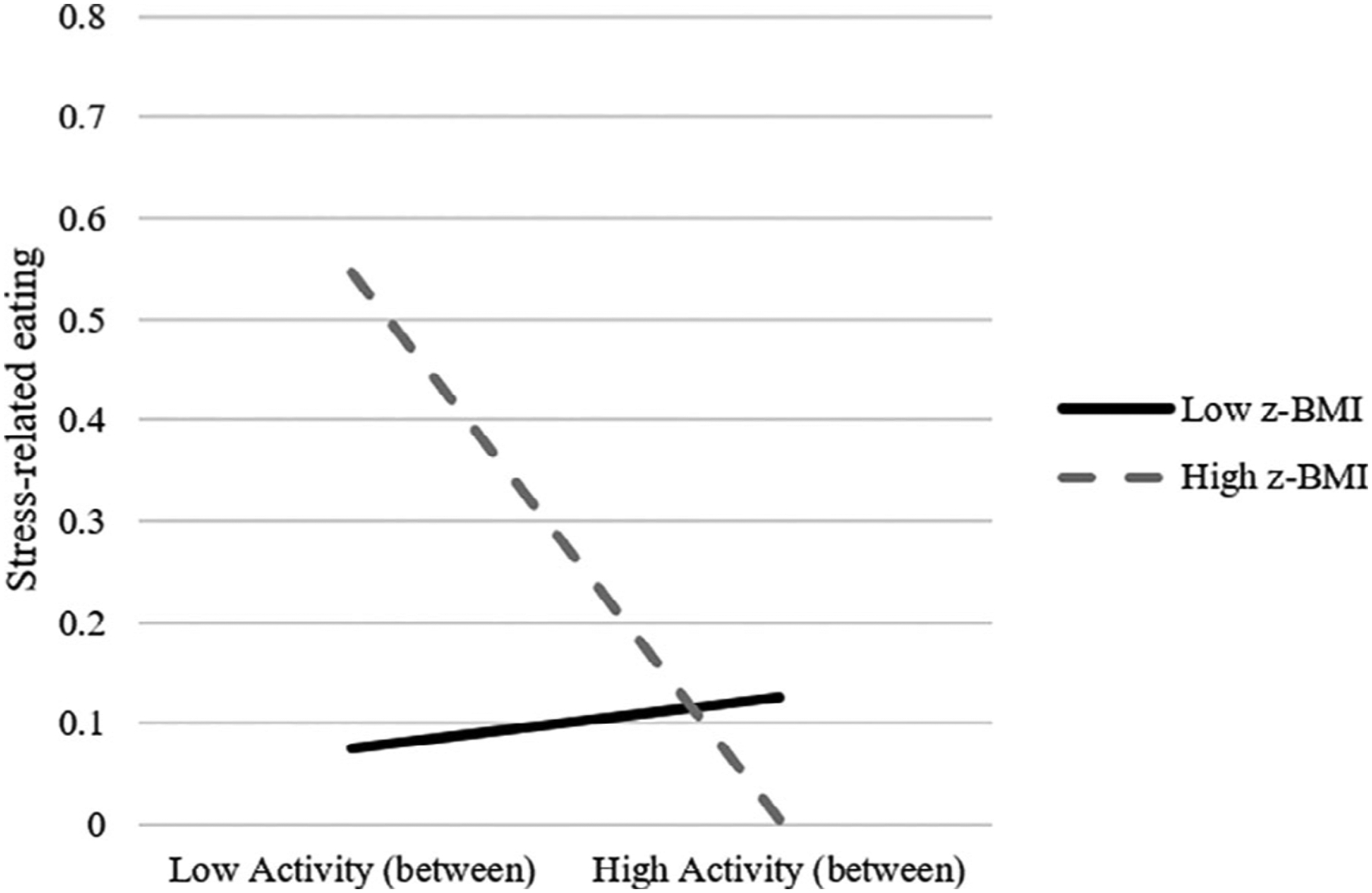
Interactions of between-person activity counts (relative to other individuals) and body mass index z-score predicting likelihood of stress-related eating. High and low values reflect 1 SD above and below sample means, respectively
With respect to positive emotional eating, there were no significant main effects of gender, age, z-BMI, MVPA (within- or between-person), or interactions between z-BMI and MVPA predicting positive emotional eating. In the GEE examining activity counts in association with positive emotional eating, there were also no significant main effects of gender, age, z-BMI, or between-person activity counts. However, there was a main effect of within-person activity counts (B = <−01, SE < .01, P = .002), an interaction of between-person activity counts and z-BMI (B = <01, SE < .01, P = .030), and an interaction of within-person activity and z-BMI (B = <01, SE < .01, P = .007) predicting positive emotional eating. At the individual (between-person) level, Figure 3 shows that among participants with greater z-BMI, lower total physical activity (total counts) was associated with less positive emotional eating across the EMA protocol. However, for participants with lower z-BMI, greater total activity (total counts) was associated with lower positive emotional eating across the EMA protocol. At the momentary (within-person) level, participants with lower z-BMI were less likely to report positive emotional eating after engaging in more activity in the hour prior to EMA recordings (relative to their own average amounts), whereas activity amounts prior to EMA prompts were not related to the likelihood of reporting positive emotional eating among participants with greater z-BMI (See Figure 4).
FIGURE 3.
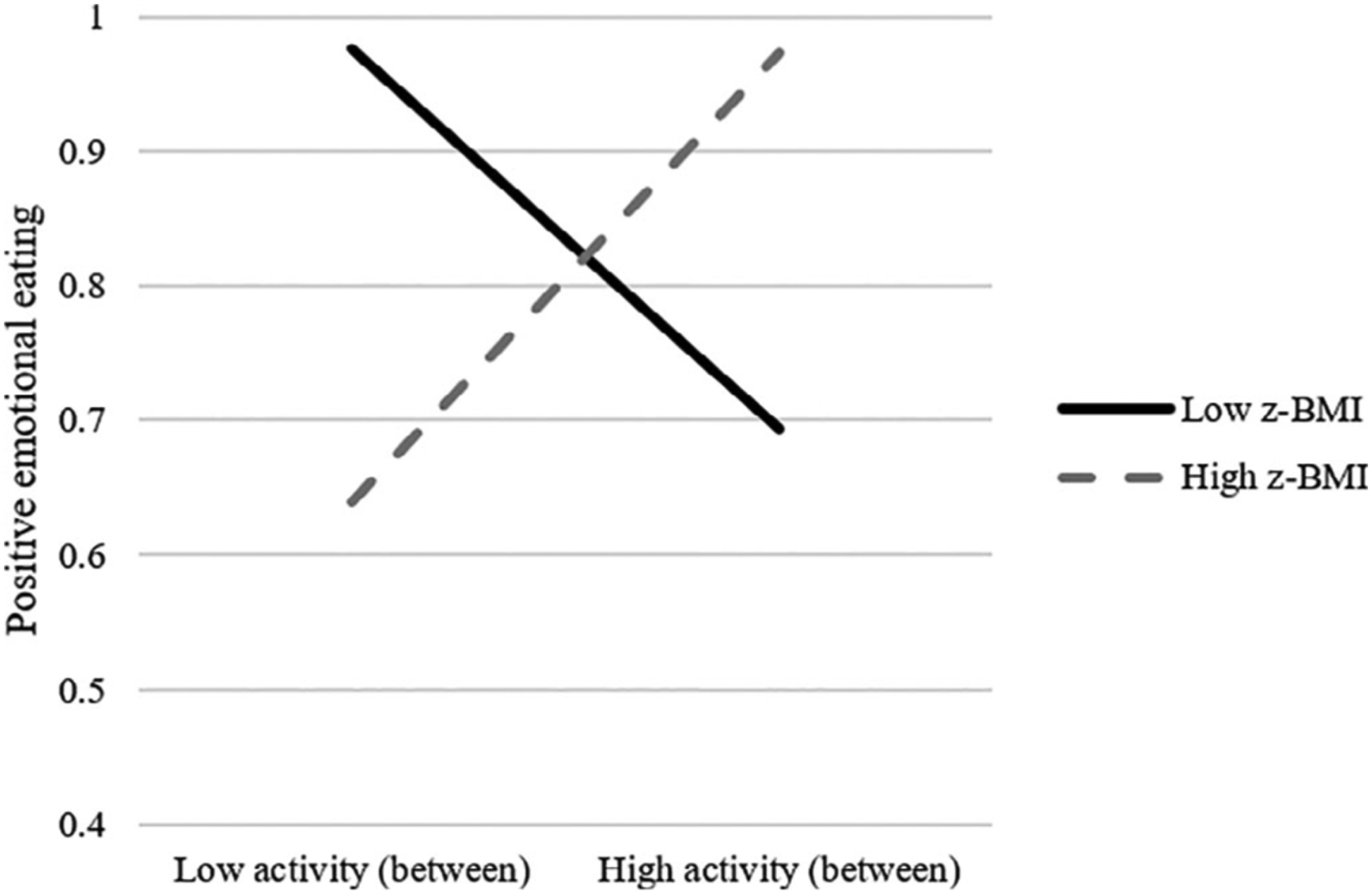
Interactions of between-person activity counts (relative to other individuals) and body mass index z-score predicting likelihood of positive emotional eating. High and low values reflect 1 SD above and below sample means, respectively
FIGURE 4.
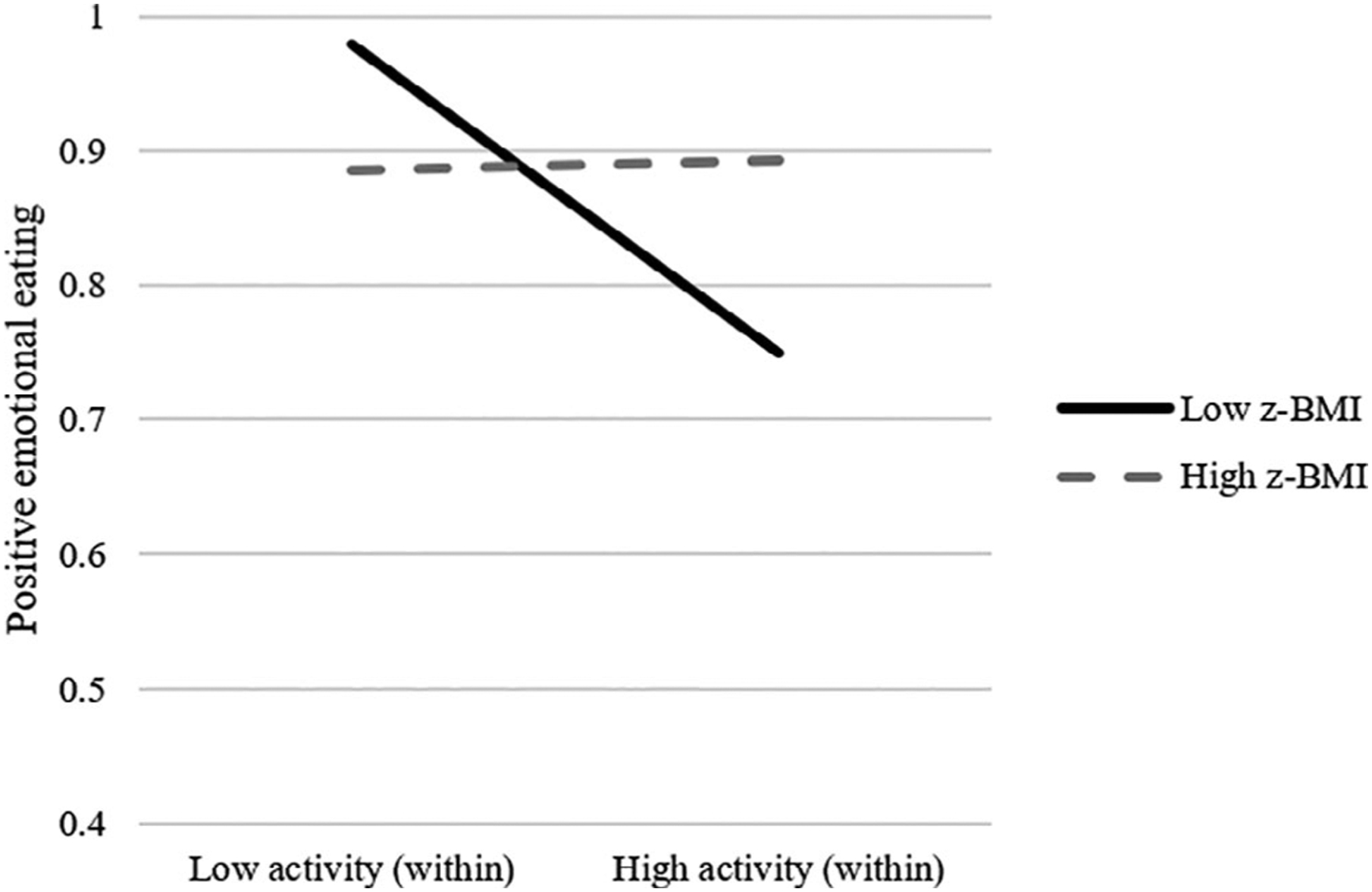
Interactions of within-person activity and body mass index z-score predicting likelihood of positive emotional eating. High and low values reflect 1 SD above and below individual/sample means, respectively
4 |. DISCUSSION
The present study was the first to investigate physical activity as a predictor of emotional eating behaviour in youth, as well as the extent to which adiposity influences these associations. Further, physical activity was as assessed at differing intensity levels, including overall lifestyle activity (ie, indexed by total activity counts) as well as MVPA time. The pattern of findings partially supported hypotheses, such that participants who engaged in greater total MVPA across the study reported lower stress-related eating, and weight status moderated both individual-level and momentary relationships of MVPA time and total activity counts with emotional eating. With respect to individual-level (ie, between-person) moderation effects, among siblings with greater z-BMI, lower total activity was related with greater stress-related eating, yet lower positive emotional eating. Conversely, among siblings with lower z-BMI, greater total activity was related with lower positive emotional eating but was not associated with their degree of stress-related eating. Regarding the momentary (ie, within-person) moderation effects, greater total physical activity in the hour before EMA recordings was associated with reduced likelihood of positive emotional eating among siblings with lower, but not greater z-BMI. Lastly, lower MVPA time in the hour before EMA recordings was related to increased likelihood of stress-related eating among siblings with greater, but not lower z-BMI.
The finding that greater MVPA was associated with lower stress-related eating across the sample is generally consistent with the literature indicating that greater physical activity is related with reduced negative affectivity.16 Further, for youth with greater z-BMI, there may be particularly detrimental effects of physical inactivity on eating regulation, given that lower total activity in this group was related to greater stress-related eating relative to youth of lower weight, and lower momentary MVPA was predictive of increased likelihood of subsequent stress-related eating. It may be that lower physical activity corresponds to more engagement in sedentary behaviour (eg, screen time), which has been linked to lower momentary positive affect and poorer mental health in children and adolescents.16,31 Consequently, this may increase risk for trait-level and momentary emotional eating, potentially as a means of affect regulation. Given that physical activity can also exert beneficial effects on executive functioning,18 which is centrally important to the development of emotion regulation capacity,44 it would be helpful for future studies to explore the extent to which low levels of physical activity may impede cognitive regulation of negative affective states, thereby contributing to stress-related eating.
Although no significant relationships were observed between MVPA and positive emotional eating, it is notable that interactions emerged between total activity and z-BMI at the individual and momentary level, suggesting physical activity may have regulating effects on eating even at lower intensities. The findings that greater total physical activity, as well as greater momentary activity prior to EMA prompts, were associated with lower positive emotional eating among youth with lower z-BMI suggests that physical activity may have a buffering effect on reward-related or hedonic eating in this group. Additional research examining the role of appetite-related hormones may be useful to understand these associations given that prior literature has shown acute exercise decreases ghrelin (an appetite stimulating hormone) and increases appetite suppressing hormones (ie, peptide YY [PYY], glucagon-like peptide 1 [GLP-1], and pancreatic polypeptide [PP]).22 Moreover, recent neuroimaging research showed that greater MVPA was associated with reduced activation in brain regions involved in emotion and reward processing when individuals viewed energy dense food images.19 This may suggest that at the neural level, physical activity can attenuate food cue reactivity contributing to reward-related eating.19 Lastly, it was somewhat unexpected that for youth with greater z-BMI, lower total activity was associated with lower positive emotional eating across the EMA protocol. It could be that physical inactivity has a more potent effect on eating in the context of lower positive affect/greater negative affect for youth with overweight/obesity, especially in light of the associations between momentary MVPA, total activity, and stress-related eating in this group.
Despite the strengths of the study (eg, naturalistic assessment methodology and objective measurement of physical activity), there are important limitations to note. Affect and eating behaviours were assessed concurrently (ie, at the same EMA signal), and thus micro-temporal relationships between these constructs could not be elucidated. That is, it is not clear whether affective states were proximal triggers, concurrent experiences, or consequences of eating behaviour. The only positive affective state assessed at EMA signals was happy; and thus, other facets of positive affect were not possible to examine. There was also a relatively high proportion of instances of positive emotional eating relative to stress-related eating, and furthermore, the EMA protocol used a signal-contingent assessment schedule that only randomly assessed experiences throughout the day. That is, they were not asked to complete surveys at every eating episode of the day (ie, event-contingent recordings). Consequently, the schedule of EMA signals may have missed some eating occasions (eg, late night, weekday mornings). Together these factors may have limited the ability to capture all eating episodes and relevant affective states. In addition, subjective experiences of loss of control eating or objective measures of overeating/dietary intake were not assessed at EMA prompts, which would be important to investigate in future EMA studies of emotional eating in relationship to eating disorder psychopathology and obesity in youth. The sample was also relatively homogenous with respect to race/ethnicity, and all participants were age 13 or older; thus, it is not clear the extent to which findings may generalize to other demographic groups or younger children.
In conclusion, these results suggest that physical activity not only impacts energy balance directly, but also may exert regulating effects on obesogenic eating behaviours among youth. Importantly, associations were observed at both at lower and higher levels of physical activity intensity, indicating even modest increases could have beneficial effects on eating. Further, the moderating effects of weight highlight the importance of considering individual differences in the extent to which physical activity may exacerbate or mitigate pediatric obesity risk via influences on eating behaviours. In addition, these results may have important implications for future prevention and intervention efforts. Specifically, our findings indicate that enhancing overall lifestyle activity in addition to MVPA among youth with greater z-BMI may generally reduce likelihood of stress-related eating. While directionality cannot be inferred from these between-person relationships, the within-person effects in this study lend further nuance in identifying the particular moments of risk of stress-related eating. That is, increasing MVPA time throughout the day, even in modest amounts, may have meaningful effects on obesogenic eating behaviours in this group. Doing so will likely require further exploration of factors that facilitate and/or impede MVPA among adolescents with greater z-BMI (eg, self-efficacy, body image, and contextual factors such as activity type, location, and presence of others).26,45
Moving forward, additional research is warranted to (a) explore biobehavioral mechanisms (eg, appetite regulation, executive functioning) by which physical activity may influence emotional eating behaviours, (b) elucidate micro-temporal associations between activity, affect, and eating, (c) examine characteristics of emotional eating episodes (ie, objective dietary intake, subjective ratings loss of control and overeating, consumption of meals vs snacks) following physical activity, and (d) prospectively examine the extent to which changes in physical activity amounts may predict disordered eating behaviours across development.
ACKNOWLEDGMENTS
This work was funded by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD064958) to James N. Roemmich and the United States Department of Agriculture, Agricultural Research Service, 3062-51000-51-00D. Author Shannon O’Connor was supported by the National Institute of Mental Health (T32MH082761).
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest. Author Ross D. Crosby is a paid statistical consultant for Health Outcomes Solutions, Winter Park, Florida, USA.
REFERENCES
- 1.Di Cesare M, Soric M, Bovet P, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 2019;17(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prevention CfDCa. Childhood Obesity Facts. 2019. https://www.cdc.gov/obesity/data/childhood.html (Accessed 2020).
- 3.Frayn M, Knauper B. Emotional eating and weight in adults: a review. Curr Psychol. 2018;37(4):924–933. [Google Scholar]
- 4.van Strien T Causes of emotional eating and matched treatment of obesity. Curr Diab Rep. 2018;18(6):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheinbein DH, Stein RI, Hayes JF, et al. Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: a social-ecological approach. Pediatr Obes. 2019;14(8):e12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herle M, Fildes A, Llewellyn CH. Emotional eating is learned not inherited in children, regardless of obesity risk. Pediatr Obes. 2018;13(10):628–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tomiyama AJ. Stress and obesity. Annu Rev Psychol. 2019;70:703–718. [DOI] [PubMed] [Google Scholar]
- 8.Roemmich JN, Smith JR, Epstein LH, Lambiase M. Stress reactivity and adiposity of youth. Obesity (Silver Spring). 2007;15(9):2303–2310. [DOI] [PubMed] [Google Scholar]
- 9.Roemmich JN, Lambiase MJ, Lobarinas CL, Balantekin KN. Interactive effects of dietary restraint and adiposity on stress-induced eating and the food choice of children. Eat Behav. 2011;12(4):309–312. [DOI] [PubMed] [Google Scholar]
- 10.Roemmich JN, Wright SM, Epstein LH. Dietary restraint and stress-induced snacking in youth. Obes Res. 2002;10(11):1120–1126. [DOI] [PubMed] [Google Scholar]
- 11.Michels N, Sioen I, Braet C, et al. Stress, emotional eating behaviour and dietary patterns in children. Appetite. 2012;59(3):762–769. [DOI] [PubMed] [Google Scholar]
- 12.Nguyen-Rodriguez ST, Unger JB, Spruijt-Metz D. Psychological determinants of emotional eating in adolescence. Eat Disord. 2009;17(3):211–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnhart WR, Braden AL, Jordan AK. Positive emotional eating and increased ease of activation and intensity of positive emotional reactivity interact to predict increased binge eating. Appetite. 2020. https://www.sciencedirect.com/science/article/abs/pii/S0195666319313558. [DOI] [PubMed] [Google Scholar]
- 14.Bongers P, Jansen A, Houben K, Roefs A. Happy eating: the single target implicit association test predicts overeating after positive emotions. Eat Behav. 2013;14(3):348–355. [DOI] [PubMed] [Google Scholar]
- 15.Sultson H, Kukk K, Akkermann K. Positive and negative emotional eating have different associations with overeating and binge eating: construction and validation of the positive-negative emotional eating scale. Appetite. 2017;116:423–430. [DOI] [PubMed] [Google Scholar]
- 16.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45(11):886–895. [DOI] [PubMed] [Google Scholar]
- 17.Blanchet C, Mathieu ME, St-Laurent A, Fecteau S, St-Amour N, Drapeau V. A systematic review of physical activity interventions in individuals with binge eating disorders. Curr Obes Rep. 2018;7(1):76–88. [DOI] [PubMed] [Google Scholar]
- 18.Joseph RJ, Alonso-Alonso M, Bond DS, Pascual-Leone A, Blackburn GL. The neurocognitive connection between physical activity and eating behaviour. Obes Rev. 2011;12(10):800–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo S, O’Connor SG, Belcher BR, Page KA. Effects of physical activity and sedentary behavior on brain response to high-calorie food cues in young adults. Obesity (Silver Spring). 2018;26(3):540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liao Y, Shonkoff ET, Dunton GF. The acute relationships between affect, physical feeling states, and physical activity in daily life: a review of current evidence. Front Psychol. 2015;6:1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schubert MM, Desbrow B, Sabapathy S, Leveritt M. Acute exercise and subsequent energy intake. A meta-analysis. Appetite. 2013;63:92–104. [DOI] [PubMed] [Google Scholar]
- 22.Schubert MM, Sabapathy S, Leveritt M, Desbrow B. Acute exercise and hormones related to appetite regulation: a meta-analysis. Sports Med. 2014;44(3):387–403. [DOI] [PubMed] [Google Scholar]
- 23.Janssen I, Katzmarzyk PT, Boyce WF, King MA, Pickett W. Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. 2004;35(5):360–367. [DOI] [PubMed] [Google Scholar]
- 24.Unick JL, Strohacker K, Papandonatos GD, et al. Examination of the consistency in affective response to acute exercise in overweight and obese women. J Sport Exerc Psychol. 2015;37(5):534–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Unick JL, Michael JC, Jakicic JM. Affective responses to exercise in overweight women: initial insight and possible influence on energy intake. Psychol Sport Exerc. 2012;13(5):528–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gayes LA, Steele RG. Comparison of two measures of weight criticism in youth: associations with physical activity engagement and attitudes, weight status, and health-related quality of life. J Pediatr Psychol. 2015;40(2):228–237. [DOI] [PubMed] [Google Scholar]
- 27.Berge JM, Tate AD, Trofholz A, Conger K, Neumark-Sztainer D. Sibling eating behaviours and parental feeding practices with siblings: similar or different? Public Health Nutr. 2016;19(13):2415–2423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roemmich JN, White TM, Paluch R, Epstein LH. Energy intake, parental control of children’s eating, and physical activity in siblings discordant for adiposity. Appetite. 2010;55(2):325–331. [DOI] [PubMed] [Google Scholar]
- 29.Stojek MMK, Tanofsky-Kraff M, Shomaker LB, et al. Associations of adolescent emotional and loss of control eating with 1-year changes in disordered eating, weight, and adiposity. Int J Eat Disord. 2017;50(5):551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van den Berg L, Pieterse K, Malik JA, et al. Association between impulsivity, reward responsiveness and body mass index in children. Int J Obes. 2011;35(10):1301–1307. [DOI] [PubMed] [Google Scholar]
- 31.Wen CKF, Liao Y, Maher JP, et al. Relationships among affective states, physical activity, and sedentary behavior in children: moderation by perceived stress. Health Psychol. 2018;37(10):904–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salvy SJ, Feda DM, Epstein LH, Roemmich JN. The social context moderates the relationship between neighborhood safety and adolescents’ activities. Prev Med Rep. 2017;6:355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salvy SJ, Feda DM, Epstein LH, Roemmich JN. Friends and social contexts as unshared environments: a discordant sibling analysis of obesity- and health-related behaviors in young adolescents. Int J Obes. 2017;41(4):569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ufholz K, Salvy SJ, Feda DM, Epstein LH, Roemmich JN. Eating responses to external food cues in weight discordant siblings. J Adolesc Health. 2019;65(1):155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- 36.Robusto KM, Trost SG. Comparison of three generations of ActiGraph activity monitors in children and adolescents. J Sports Sci. 2012;30(13):1429–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Romanzini M, Petroski EL, Ohara D, Dourado AC, Reichert FF. Calibration of ActiGraph GT3X, Actical and RT3 accelerometers in adolescents. Eur J Sport Sci. 2014;14(1):91–99. [DOI] [PubMed] [Google Scholar]
- 38.Vanhelst J, Beghin L, Turck D, Gottrand F. New validated thresholds for various intensities of physical activity in adolescents using the Actigraph accelerometer. Int J Rehabil Res. 2011;34(2):175–177. [DOI] [PubMed] [Google Scholar]
- 39.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc. 2010;42(12):2211–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 41.Freedson P, Pober D, Janz KF. Calibration of accelerometer output for children. Med Sci Sports Exerc. 2005;37(11 Suppl):S523–S530. [DOI] [PubMed] [Google Scholar]
- 42.Harrell JS, McMurray RG, Baggett CD, Pennell ML, Pearce PF, Bangdiwala SI. Energy costs of physical activities in children and adolescents. Med Sci Sports Exerc. 2005;37(2):329–336. [DOI] [PubMed] [Google Scholar]
- 43.Smith KE, Haedt-Matt A, Mason TB, et al. Associations between naturalistically assessed physical activity patterns, affect, and eating in youth with overweight and obesity. J Behav Med. 2020. https://link.springer.com/content/pdf/10.1007/s10865-020-00152-3.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmed SP, Bittencourt-Hewitt A, Sebastian CL. Neurocognitive bases of emotion regulation development in adolescence. Dev Cogn Neurosci. 2015;15:11–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dunton GF, Liao Y, Intille S, Huh J, Leventhal A. Momentary assessment of contextual influences on affective response during physical activity. Health Psychol. 2015;34(12):1145–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]


