Abstract
The National Action Plan to Improve Health Literacy emphasizes the importance of community-based opportunities for education, such as English as a second language (ESL) programs. It recommends collaborations among the adult literacy and ESL communities. However, limited attention has been given to researching the effectiveness of community-based interventions that combine ESL and health literacy. The purpose of this study was to explore the feasibility of using different community settings for improving health literacy among adult Spanish speakers through an English language program. The study used a pre-experimental, single arm pretest–posttest design, and implemented the Health Literacy and ESL Curriculum. A collaborative was established between the community and university researchers. Participants were recruited at three distinctive sites. Health literacy was assessed using the Spanish version of the Test of Functional Health Literacy in Adults (TOFHLA). Analysis included descriptive and paired-group t test. Forty-nine participants completed the intervention and post-tests (92 % retention rate). Overall—all sites—posttest scores significantly improved for total TOFHLA, raw numeracy, and reading comprehension (p < 0.0001). Similarly, all three sites yielded significantly better mean differences for the total TOFHLA score while numeracy and reading comprehension significantly improved in some sites. Results suggest that community sites are viable venues for delivering health literacy/language instruction to Spanish speaking adults. The study also points to community engagement and ESL programs as two essential components of effective health literacy interventions among Spanish speakers.
Keywords: Hispanics, English language, ESL, Collaborative
Introduction
Health literacy is the capacity to “obtain, process, and understand basic health information and services needed to make appropriate health decisions” [1]. Limited health literacy has been negatively associated with healthcare use and health outcomes, including hospital admissions, use of preventative services, management of chronic conditions, and mortality [1–4].
Health literacy has been identified in the literature as a critical factor contributing to health disparities [5–10], and national data confirm that health disparities are exacerbated by the prevalence and severity of limited health literacy. Populations that are most likely to experience limited health literacy include racial and ethnic minority groups, immigrants, people with less than a high school degree, people with incomes at or below the poverty level, and non-native speakers of English [11]. These characteristics are especially predominant among Hispanics, and in fact the 2003 National Assessment of Adult Literacy (NAAL) showed that, overall, Hispanic adults had the lowest health literacy scores of any other race or ethnic group: 41 % were in the “below basic” health literacy range [12].
Despite the fact that disparities in health literacy affecting Hispanics and other minority groups have been identified and reported for more than a decade, limited attention has been given to researching the effectiveness of community-based interventions with these groups. For instance, a 2011 health literacy research review indicated that in the United States there is a lack of data on the health literacy skills of populations with limited or no English language skills [13], including Spanish speakers. This is an issue which must be addressed, as a major contributor to the disparities in health literacy affecting the Hispanic population is language. Studies have shown that language affects how we communicate, understand, and respond to health information, all essential components of health literacy [14]. In fact, the National Action Plan to Improve Health Literacy (NAPIHL) emphasizes the importance of community-based opportunities for education, such as English as a second language (ESL) programs. It recommends collaborations among the adult literacy and ESL communities [14]. The implementation of these recommendations may constitute an effective approach to promote health literacy among Spanish speakers for several reasons. First, according to the most recent census data, more than 37.5 million people in the United States speak Spanish, and about half of these speak English “less than very well” [15]. Additionally, data indicate that Hispanics are overrepresented in ESL instruction [16, 17].
There are educators and health experts who support these recommendations. They recognize the added value of incorporating health into literacy and adult education [18], including ESL, and that students are interested in learning about health issues [19]. Others have suggested that health issues in ESL instruction can develop both language skills and critical thinking [20] and found that the combination results in positive outcomes outside of the classroom, such as “increased activity within the community and learners taking healthful action for themselves” [21, 22]. These added benefits, which go beyond English language learning, are probably due to the fact that a typical ESL curriculum generally has the goals of expanding students’ essential English skills and cultural knowledge. They are generally required not only to study grammar and participate in conversations on familiar topics in social situations to improve their written and oral communication, but also to expand their vocabulary through training on how to use community resources. They are also exposed to interactive learning activities and situations confronted in every-day life.
Despite the advantages of integrating health literacy into ESL and the need for effective health literacy interventions for Spanish speakers, the literature lacks interventions that have used and evaluated this strategy. Most of the reported health literacy interventions with Hispanics and Spanish speakers have been implemented in clinical settings, with the general aim of addressing specific health and/or healthcare issues [23–27]. However, the benefits of using existing community settings that are convenient and not menacing to participants are multilevel: they range from overcoming transportation barriers to providing a relaxed environment that is more conducive to learning.
Community settings constitute a viable option that should be considered when planning health literacy interventions with Hispanic immigrants, and this is an area in need of further research. A recent study that explored the feasibility of using ESL instruction in an academic environment to improve health literacy in English among Hispanic adults yielded promising results [28–30]. The purpose of this study was to explore the feasibility of using different community settings for improving health literacy among adult Spanish speakers through an English language program.
Background
This study was conducted in collaboration with Santa Barbara/Martineztown, a small urban community located in Albuquerque, New Mexico. Santa Barbara/Martineztown is a historic community that has overcome economic marginalization and transformed itself through advocacy and civil engagement. However, it continues to experience significant disparities related to adult education and health outcomes. According to recent data, the population of Santa Barbara/Martineztown is 65 % Hispanic/Latino, and almost 50 % speak Spanish at home. More than 34 % fall below the poverty level, and nearly 30 % have not graduated from high school [31]. Regarding health, data indicated that Santa Barbara/Martineztown negatively compared to the larger area of Bernalillo County, where it is located, in most health indicators. These indicators included overall mortality, infant deaths, HIV/AIDS cases, asthma hospitalizations, and hepatitis [32].
The Santa Barbara/Martineztown community was enthusiastic about collaborating with university researchers to address the issue of health literacy because the study related both to education and health. The research team met with community groups during the initial planning phases of the study in order to gain the unique community perspectives on the local impact of low health literacy, and to gain community support and buy-in for the project. These groups included the Santa Barbara/Martineztown Neighborhood Association, Citizens Information Committee of Martineztown, and Martineztown House of Neighborly Service.
A collaborative partnership was established with existing community systems, including a local elementary school (Site 1), a large hotel chain (Site 2), and a community church (Site 3), to implement the various components of the study. The partnership collaborated on all aspects of the study, including the planning, implementation and evaluation of the intervention; identifying study sites; recruiting participants; providing implementation support (e.g. day care for participating parents); contributing to retention (e.g. arranging for transportation and contacting those who missed a session); and facilitating data collection (e.g. allowing space and employee time to complete questionnaires).
Methods
Design
The study used a pre-experimental, single arm pretest–posttest design. The main hypothesis was that participants would demonstrate greater post-test health literacy scores as compared to their baseline scores. Additionally, the study aimed at exploring differences between sites, and comparing results across all intervention sites. The study received human subjects (IRB) approval and all participants were presented with and signed an informed consent.
Participants and Recruitment
Study participants were recruited at the three selected study sites with the assistance of a trained bilingual Health Extension Rural Offices (HEROs) agent. HEROs is a collaborative between the University of New Mexico Health Sciences Center and the Department of Health County Health Councils to link community priority health needs and university resources to achieve measurable improvements in health status. Presentations were made by the HERO agent, who also distributed written information to potential participants at participating sites and other community outlets. Participants were asked to report about whether they met the following inclusion criteria: (a) Hispanic or Latino ethnicity; (b) the ability to read and write in Spanish; and (c) 18 years of age or older. Interested adults were invited to attend an orientation session that was conducted at each selected site. Spanish-speaking members of the research team and the HERO agent facilitated the sessions and presented the program; provided information on participants’ rights and responsibilities; and confirmed inclusion criteria and commitment. Seventy-four individuals showed interest in the program: 30 at site 1, 26 at site 2, and 18 at site 3. Thirteen people could not confirm eligibility and/or availability. A total of 61 adults were invited to participate and attend the first session, which included presenting and obtaining informed consent. All participants who completed the program and tests received a $100 gift certificate as compensation for their time.
Facilitator
One ESL certified teacher was recruited to facilitate the implementation of the intervention. Members of the research team conducted a pre-implementation half-day training session for the facilitator to ensure that she was comfortable guiding participants through the curriculum.
Intervention
This project implemented a health literacy/ESL curriculum that was developed by the research team for a previously funded study. The Health Literacy and ESL Curriculum consists of 12 units (approximately 45 h) intended to be implemented in 6 weeks (although the number and duration of the weekly sessions were determined depending on availability of the participants and convenience). It combines health literacy content and English language instruction, and is specifically designed for Spanish-speaking Hispanic adults. The content focuses on improving participants’ English language proficiency in listening, speaking, reading, and writing. In addition, it is designed to enhance essential health literacy skills, including reading comprehension of different types of documents, numeracy skills, familiarity with clinical and preventive practices, and navigation of the health care system. Information on the development, content, and evaluation of the curriculum has been previously reported [28–30], and the curriculum is publically available [33].
Measures
Health literacy was assessed using the Spanish version of the Test of Functional Health Literacy in Adults (TOFHLA) (Peppercorn Books and Press, MI), which has shown to be a valid and reliable instrument [34]. The TOFHLA consists of a 17-item numerical ability test and a 50-item reading test, and requires up to 22 min to administer. It measures adult functional health literacy, both numeracy and reading comprehension, using actual health-related materials such as prescription bottle labels and appointment slips. The total score is calculated based on the number of correct answers, with a range from 0 to 100 (the 17-item numeracy test raw score is weighted to up to 50 points to balance the total TOFHLA score). Further, the test score is categorized into three levels: inadequate functional health literacy (0–59), unable to read and interpret health texts; marginal functional health literacy (60–74), difficulty reading and interpreting texts, and adequate functional health literacy (75–100), can read and interpret most texts. For this study, the TOFHLA was adapted so that it could be administered in a group setting, rather than one-on-one. Participants were provided with a hard copy of the test, and general completion instructions were read out loud to the group. Each item in the numeracy section included the prompt and related questions, and a blank space. Participants were asked to read the prompts and write the answer to the questions in the space provided. For each section, the time allotted was consistent with the test’s instructions: 10 and 12 min respectively.
Participants also completed a brief demographics questionnaire (pre-test only) that included questions on age, gender, whether they were born in the United States, years living in the United States, years of formal education, and education level (see Table 1).
Table 1.
Demographics by site (n = 49)
| Site 1 (n = 19) | Site 2 (n = 16) | Site 3 (n = 14) | |
|---|---|---|---|
| Sex | |||
| Male | 10 (53 %) | 2 (13 %) | 8 (58 %) |
| Female | 9 (47 %) | 14 (87 %) | 6 (42 %) |
| Age (years) | |||
| 20–29 | 7 (37 %) | 1 (6 %) | 3 (22 %) |
| 30–39 | 4 (21 %) | 2 (12 %) | 6 (42 %) |
| 40–49 | 4 (21 %) | 6 (38 %) | 3 (22 %) |
| 50 or more | 4 (21 %) | 7 (44 %) | 2 (14 %) |
| U.S. Born | |||
| No | 19 (100 %) | 15 (94 %) | 13 (93 %) |
| Yes | 1 (6 %) | 1 (7 %) | |
| Years living in US | |||
| <5 | 2 (10 %) | 2 (13 %) | 3 (22 %) |
| >5 | 15 (80 %) | 14 (87 %) | 9 (64 %) |
| Missing | 2 (10 %) | 2 (14 %) | |
| Education level | |||
| <High school | 9 (47 %) | 10 (62 %) | 9 (65 %) |
| Finished high school | 6 (32 %) | 3 (19 %) | 2 (14 %) |
| >High school | 4 (21 %) | 3 (19 %) | 1 (7 %) |
| Not sure | 2 (14 %) | ||
| English proficiency | |||
| Low | 9 (47 %) | 12 (75 %) | 9 (64 %) |
| Intermediate | 8 (42 %) | 4 (25 %) | 5 (36 %) |
| Good | 2 (11 %) | ||
| Language spoken at home | |||
| Spanish | 18 (95 %) | 14 (87 %) | 12 (86 %) |
| Both (Spanish and English) | 1 (5 %) | 2 (13 %) | 2 (14 %) |
Data Collection and Analysis
Trained Spanish-speaking members of the research team administered the pre-test immediately prior to the first session. Each participant was assigned a unique ID number, and the questionnaire did not include participants’ names. A list of names and ID numbers was kept separately from the data, and used to distribute the post-tests at the end of the last session. All participants who attended the last session completed the post-test. Only participants who completed more than 75 % of the sessions were included in the final analysis. Demographics and survey responses were entered into IBM SPSS Statistics 19.0 software program (SPSS Inc., Chicago, Ill).
Data analysis procedures included descriptive demographics and TOFHLA score averages, and paired-group t test to determine pretest and posttest changes across sites and groups by domain: total combined TOFHLA score (range 0–100), numeracy raw score (range 0–17), and reading comprehension score (range 0–50). Fisher’s exact test was used to compare functional health literacy level change across sites. For the categorical analyses, a change in health literacy level index was developed as follows: 0 = failed to improve (e.g. those participants who were at the inadequate or marginal health literacy level and who did not improve their level at post-test); 1 = improved (e.g. those who improved by one or more levels); 2 = maintained adequate level (e.g. those with adequate level at both pre-test and post-test).
Results
Of the 61 adults who were invited to participate, 53 attended the first session and completed the pre-tests. Of those, 49 completed the post-tests (92 % retention rate). Only complete cases are reported below. Sample size by site and demographic data are included in Table 1. A majority of the participants were female and had less than a high school education (although 17 % had received some type of college degree). Demographics across sites were balanced for certain variables, more than 93 % were foreign born, nearly 67 % lived in the country for more than 5 years, most self-assessed their English language level as low or intermediate, and 90 % spoke only Spanish at home. Females were overrepresented in site 2; and education level and English proficiency were higher in site 1.
The baseline overall TOFHLA mean score was 73.9, and post-test mean score was 83.4. Site 1 had the highest baseline total TOFHLA mean score (79.1), as well as raw numeracy (12.0) and reading comprehension (43.2) scores. Overall and domain specific pre and post-test TOFHLA mean scores are included in Table 2.
Table 2.
Overall and domain-specific pretest and posttest TOFHLA scores (n = 49)
| Mean | SD | |
|---|---|---|
| Total TOFHLA pretest score | 73.96 | 19.516 |
| Total TOFHLA posttest score | 83.41 | 12.057 |
| Numeracy pretest raw score | 10.86 | 4.481 |
| Numeracy posttest raw score | 12.94 | 3.185 |
| Reading comprehension pretest score | 41.51 | 7.982 |
| Reading comprehension posttest score | 44.71 | 4.183 |
The paired t test comparing overall—all sites—baseline and post-test mean scores yielded a difference of 9.4 (p value <0.0001) for the combined total TOFHLA score; a 2.1 (p value <0.0001) for the raw numeracy score; and a 3.2 (p value <0.001) for the reading comprehension score. Baseline and post-test differences by site are included in Table 3. All three sites yielded significantly better mean differences for the total TOFHLA score (site 1 p values <0.05; site 2 p value = 0.02; site 3 p value = 0.0003); numeracy scores significantly improved in sites 2 (p value = 0.02) and 3 (p = 0.003); while reading comprehension significantly improved in site 3 (p = 0.006).
Table 3.
Overall and domain specific pre-test and post-test TOFHLA mean score and difference by site (n = 49)
| Difference | SD | Std. Error mean | |
|---|---|---|---|
| Site 1 (n = 19) | |||
| Total TOFHLA mean score | 7.47 | 15.49 | 3.55 |
| Numeracy raw mean score | 1.47 | 3.38 | 0.77 |
| Reading comprehension mean score | 2.89 | 6.46 | 1.48 |
| Site 2 (n = 16) | |||
| Total TOFHLA score | 10.18 | 16.07 | 4.01 |
| Numeracy raw score | 2.43 | 3.74 | 0.93 |
| Reading comprehension score | 3.0 | 7.91 | 1.97 |
| Site 3 (n = 14) | |||
| Total TOFHLA score | 11.28 | 8.73 | 2.33 |
| Numeracy raw score | 2.5 | 2.56 | 0.68 |
| Reading comprehension score | 3.85 | 4.34 | 1.16 |
Categorical results are included in Fig. 1. The percentage of participants who scored at the “adequate level of functional health literacy” increased at post-test by 22.5 %. Participants at site 3 showed the highest improvement (28 % difference between baseline and post-test). Similarly, there was a 16 % reduction of the percentage of participants who scored at the “inadequate level of functional health literacy”; only 4 % of the participants scored at this level at post-test (vs. 20 % at baseline). The results of the Fisher’s exact test based on the proposed level change index yielded a non-statistically significant association between site and a change in health literacy level (χ2 = 2.30; p = 0.705).
Fig. 1.
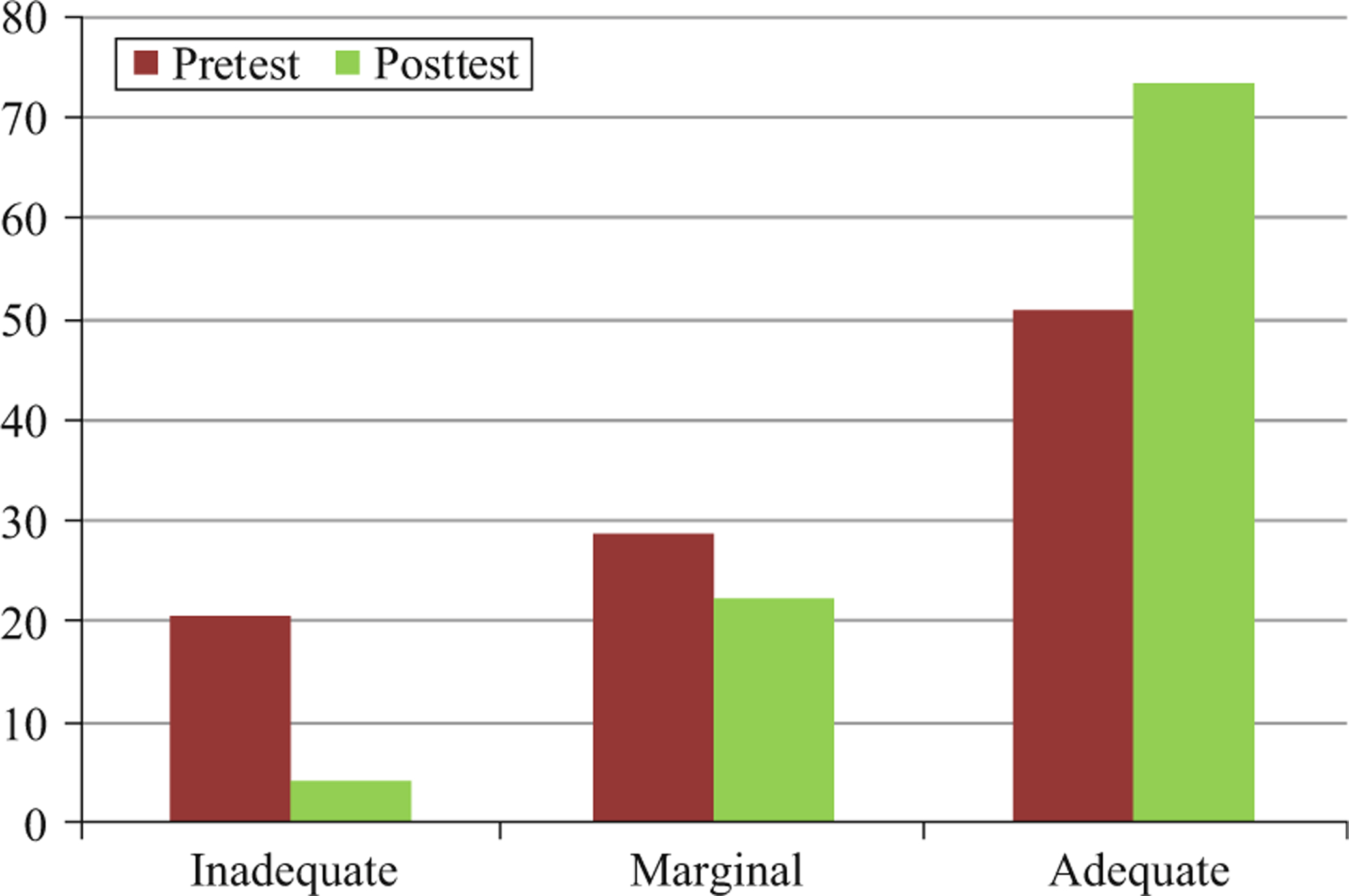
Percent of participants at each health literacy level, pretest and posttest (n = 49)
Discussion
The main purpose of this study was to explore the feasibility of using a variety of community settings to improve health literacy among adult Spanish speakers. The study implemented a curriculum that combines both health literacy and language content. Although the curriculum had been piloted and evaluated previously in an academic environment [28–30], the results of this study support its use and effectiveness in different community contexts.
First, it is important to mention the importance of the community-academia collaborative partnership that was established. The collaborative was successful because the study addressed issues that were already of concern to the community (e.g. low education/literacy and prominent health issues). The partnership was instrumental in identifying community settings and facilitated the recruitment of a diverse population; provided a supportive and familiar environment for the implementation of the Health Literacy and ESL Curriculum; increased participants’ trust, and added perceived confidence in its potential benefits. Although the research team made it very clear at each site that participation was voluntary and that the study was the initiative of a university-community partnership, support from administrators and employers was instrumental in achieving the study’s goals and objectives. Site 1 (school) reached out to adult education programs in nearby academic institutions whose students were interested in ESL programs. The employer in site 2 (hotel) realized the advantage of improved health and English language training to valued employees. Also, given that employees perceived the opportunity as an added benefit, there was the potential for improved job satisfaction and performance. The church pastor in site 3 supported the program because of the opportunity to contribute to the community and provide a needed service to its members. The community support and partnership greatly contributed to recruitment and retention (92 %). The ESL teacher also proved to be an important motivator to keeping participants engaged in the project.
Regarding results, considerable improvements in posttest health literacy scores and functional health literacy levels were observed in all three sites. Overall TOFHLA mean score increased by 11.3 points at post-test; numeracy by 2.4 points, and reading comprehension by 4.2 points. Only 2 participants scored at the “inadequate level of functional health literacy” at post-test, compared to 13 at baseline. These results support federal recommendations for improving health literacy, which specifically include community-based opportunities for ESL programs [14]. Results are also consistent with a previous study that used the Health Literacy and ESL Curriculum with a similar population in an academic environment [28–30]. While the previous study assessed health literacy in English, the present study used the Spanish version of the same instrument (TOFHLA). This may be of relevance, as it may indicate that the approach constitutes a viable option for improving both English and Spanish health literacy. Although health literacy has been defined as the ability to understand English health information [4, 12, 35] and studies have found that limited English proficiency (LEP) constitutes a barrier to health care [36], whether or not it is appropriate to measure health literacy in other than the primary language of the participant is a debated issue and in need of further research. Health literacy research must address the role of language in the assessment of health literacy level among Hispanics, and also the role of other factors such as health beliefs and practices [37].
Ii is also important to emphasize that a significant improvement was observed not only in overall total TOFHLA score, but also in numeracy and reading comprehension (Table 2). These are relevant findings considering that both numeracy and reading skills are essential domains within health literacy. Researchers have suggested that these domains, both together and individually, are correlated with utilization of health care services, health outcomes, and have a mediating effect on health disparities [13]. Although it would be premature to suggest that these results were produced by the intervention/curriculum, considering that the study was exploratory and non-experimental, the results are encouraging: they suggest that the Health Literacy and ESL Curriculum may have a positive effect on two key health literacy domains as measured in Spanish. This finding constitutes areas for future research: First, the study should be replicated using an experimental design. More importantly, considering that the Health Literacy and ESL Curriculum combines health and language content and is delivered in English, it would be essential to identify the specific features that contribute to improve Spanish health literacy. For instance, it would be important to discern whether the positive effect in Spanish health literacy is mediated by English proficiency, health knowledge/skills, numeracy, reading skills, or more than one factor. The changes could also be related to improvements in critical thinking skills. Previous research has suggested that the combination of health content and ESL instruction can contribute to the development of critical thinking [20]. In any case, further researcher would inform the development of effective interventions that positively affect health outcomes among Spanish speakers.
Regarding differences across sites, it seems that participants in site 2 and site 3 benefited the most from the program as they showed greater increases in TOFHLA scores (See Table 3). Participants in site 1 may have received less benefit from the program, as their overall baseline TOFHLA scores were already high. This may be due to the fact that these participants had a higher level of education and English proficiency compared to other sites (see Table 1). These results are consistent with the literature, and previous studies with Hispanics that found a positive association between education, English proficiency, and health literacy [37, 38], and that Hispanic college students had higher health literacy than the general Hispanic adult population [39]. Finally, although the categorical comparison did not result in significant differences in health literacy level across sites, it is important to remember that the TOFHLA score range for each category is very wide. Therefore, a significant improvement in absolute score may not translate into a categorical change.
Limitations
This was a non-experimental single-arm study designed for the collection of preliminary data with a relatively small sample. Therefore, generalizations should be made cautiously. Results may only apply to Spanish-speaking Hispanic adults with the same characteristics as those of the study’s population. Similarly, the curriculum was specifically developed for adults with a low to intermediate level of English, and may only be appropriate for this population group. The sample size was small and homogeneous, which did not allow for comparative analyses between subgroups. The study did not conduct subsequent follow-up assessments after the post-test, and it is not known whether observed changes persisted over time. Since an identical version of the S-TOFHLA was used in the pre-test and post-test, there may be a threat to internal validity. Specifically, there is a chance that the participants remembered certain items from the pre-test, which could influence results on the post-test.
Conclusion
Community engagement and ESL programs may constitute two essential components of effective health literacy interventions among Spanish speakers. The results of this exploratory study suggest ESL instruction as a recommended approach for improving health literacy among Spanish speaking adults. The study also points to community sites as viable venues for delivering health literacy/language instruction to Spanish speaking adults. Further research is recommended.
Acknowledgments
This project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health through Grant Number 8UL1TR000041. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors thank the University of New Mexico Office of Community Health for its contribution to the project. Many thanks to Mr. Frank Martinez and the Citizens Information Committee of Martineztown. We also thank the Martineztown House of Neighborly Service and Santa Barbara/Martineztown Neighborhood Association.
Contributor Information
F. Soto Mas, Public Health Program, Department of Family and Community Medicine, MSC09 5060, 1 University of New Mexico, Albuquerque, NM 87131-0001, USA
H. E. Jacobson, Department of Linguistics, MSC 03 2130, 1 University of New Mexico, Albuquerque, NM 87131-0001, USA
F. Ronquillo, Office of Community Health, University of New Mexico Health Sciences Center, MSC09 5065, 1 University of New Mexico, Albuquerque, NM 87131, USA
D. Helitzer, Department of Family and Community Medicine, School of Medicine, MSC09 5040, 1 University of New Mexico, Albuquerque, NM 87131-0001, USA
References
- 1.Ratzan SC, & Parker RM (2000). Introduction. In Selden CR, Zorn M, Ratzan SC, & Parker RM (Eds.), National library of medicine current bibliographies in medicine: Health literacy. Vol. NLM Pub. No. CBM 2000–1 Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services. [Google Scholar]
- 2.Baker DW, Wolf MS, Feinglass J, & Thompson JA (2008). Health literacy, cognitive abilities, and mortality among elderly persons. Journal of General Internal Medicine, 23(6), 723–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berkman ND, DeWalt DA, Pignone MP, et al. (2004). Literacy and health outcomes (AHRQ Publication No. 04-E007–2) Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- 4.Nielsen-Bohlman L, Panzer AM, & Kindig DA (Eds.). (2004). Health literacy: A prescription to end confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 5.Cheng TL, Dreyer BP, & Jenkins RR (2009). Introduction: Child health disparities and health literacy. Pediatrics, 124(Suppl 3), S161–S162. [DOI] [PubMed] [Google Scholar]
- 6.Hasnain-Wynia R, & Wolf MS (2010). Promoting health care equity: Is health literacy a missing link? Health Services Research, 45(4), 897–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelly PA, & Haidet P (2007). Physician overestimation of patient literacy: A potential source of health care disparities. Patient Education and Counseling, 66(1), 119–122. [DOI] [PubMed] [Google Scholar]
- 8.Horowitz AM, & Kleinman DV (2012). Oral health literacy: A pathway to reducing oral health disparities in Maryland. Journal of Public Health Dentistry, 72(Suppl 1), S26–S30. [DOI] [PubMed] [Google Scholar]
- 9.Paasche-Orlow MK, & Wolf MS (2010). Promoting health literacy research to reduce health disparities. Journal of Health Communication, 15(Suppl 2), S34–S41. [DOI] [PubMed] [Google Scholar]
- 10.Sentell TL, & Halpin HA (2006). Importance of adult literacy in understanding health disparities. Journal of General Internal Medicine, 21(8), 862–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Education US. (2006). National assessment of adult literacy (NAAL): A first look at the literacy of America’s adults in the 21st century (NCES Publication No. 2006–470) Washington, DC: Institute of Education Sciences. [Google Scholar]
- 12.Kutner M, Greenberg E, Jin Y, & Paulsen C (2006). The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006–483). U.S. Department of Education Washington, DC: National Center for Education Statistics. [Google Scholar]
- 13.Berkman ND, DeWalt DA, Pignone MP, et al. (2004). Literacy and health outcomes (AHRQ Publication No. 04-E007–2) Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- 14.U.S. Department of Health and Human Services. (2010). National Action Plan to Improve Health Literacy. DHHS, Office of Disease Prevention and Health Promotion. Washington, DC: Author. [Google Scholar]
- 15.Ryan C (2013). Language use in the United States: 2011. American Community Survey Reports. U.S. Department of Commerce, Economics and Statistics Administration, U.S. CENSUS BUREAU, August. [Google Scholar]
- 16.Creighton S, & Hudson L (2002). Participation trends and patterns in adult education: 1991 to 1999 (NCES Technical Report No. 2002–119) Washington DC: U.S. Department of Education, Office of Educational Research and Improvement. [Google Scholar]
- 17.Singleton K (2002). Health literacy and adult English language learner. Washington, DC: National Center for ESL Literacy Education, Center for Applied Linguistics. [Google Scholar]
- 18.Rudd RE, Zahner L, & Banh M (1999). Findings from a national survey of state directors of adult education. Harvard School of Public Health, The National Center for the Study of Adult Learning and Literacy (NCSALL) Reports #9, Cambridge, MA, January. [Google Scholar]
- 19.Povenmire AV, & Hohn M (2001). Why teach health. Field Notes 10(4), Spring. [Google Scholar]
- 20.LaMachia J, & Morris E (2001). Teachers’ concerns about incorporating health into adult education. Field Notes, 10(4), Spring. [Google Scholar]
- 21.Rudd RE, Zacharai C, & Daube K (1998). Integrating health and literacy: Adult educators’ experiences. National Center for the Study of Adult Learning and Literacy. NCSALL Reports #5. Cambridge, MA, August. [Google Scholar]
- 22.Rudd RE, Moeykens BA, & Colton TC (1999). Health and literacy: A review of medical and public health literature. In Comins J, Garners B, & Smith C (Eds.), Annual review of adult learning and literacy. New York: Jossey-Bass. [Google Scholar]
- 23.Brice JH, Travers D, Cowden CS, Young MD, Sanhueza A, & Dunston Y (2008). Health literacy among Spanish-speaking patients in the emergency department. Journal of the National Medical Association, 100(11), 1326–1332. [DOI] [PubMed] [Google Scholar]
- 24.Garbers S, Schmitt K, Rappa AM, & Chiasson MA (2010). Functional health literacy in Spanish-speaking Latinas seeking breast cancer screening through the National Breast and Cervical Cancer Screening Program. International Journal of Women’s Health, 9(1), 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koskan A, Friedman DB, & Messias DKH (2010). Health literacy among Hispanics: A systematic research review (1992–2008). Hispanic Health Care International, 8(2), 65–76. [Google Scholar]
- 26.Penaranda E, Diaz M, Noriega O, & Shokar N (2012). Evaluation of health literacy among Spanish-speaking primary care patients along the US–Mexico border. Southern Medical Journal, 105(7), 334–338. [DOI] [PubMed] [Google Scholar]
- 27.Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, & Schillinger D (2009). Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Education and Counseling, 75(3), 398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fuentes B, Soto Mas F, Mein E, & Jacobson H (2011). Un currículo interdisciplinario de base teórica para enseñar inglés como segunda lengua (An interdisciplinary theory-based ESL curriculum). Colombian Journal of Applied Linguistics, 13(2), 60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soto Mas F, Ji M, Fuentes B, & Tinajero J (2014). The health literacy & ESL study: A community-based intervention for Spanish speaking adults. Journal of Health Communication. doi: 10.1080/10810730.2014.965368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soto Mas F, Mein E, Fuentes B, Thatcher B, & Balcázar H (2013). Integrating health literacy and ESL: An interdisciplinary curriculum for Hispanic immigrants. Health Promotion Practice, 14(2), 263–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau, (n.d.). Community Facts. 2008–2012 American Community Survey 5-Year Estimates. Retrieved September 15, 2014, from http://factfinder2.census.gov/faces/nav/jsf/pages/community_facts.xhtml. [Google Scholar]
- 32.Khanlian S, & Scharmen T (2005). Albuquerque and Bernalillo County zip code maps. Health and social indicators. New Mexico: Department of Health, Public Health Division, District 1. Office of Community Assessment, Planning and Evaluation. [Google Scholar]
- 33.Soto Mas F, Fuentes BO, Arnal P, Mein E, & Tinajero J (2013). Health literacy & ESL curriculum. MedEdPORTAL. Retrieved September 15, 2014, from https://www.mededportal.org/publication/9420. [Google Scholar]
- 34.Parker RM, Baker DW, Williams MV, & Nurss JR (1995). The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine, 10(10), 537–541. [DOI] [PubMed] [Google Scholar]
- 35.Kirsch I, Jungeblut A, Jenkins L, & Kolstad A (Eds.). (1993). Adult literacy in America: A first look at the National Adult Literacy Survey (NALS). Washington, DC: U.S. Department of Education. [Google Scholar]
- 36.Pippins JR, Alegría M, & Haas JS (2007). Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Medical Care, 45(11), 1020–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyas JF (2013). Correlates of health literacy among Latinos in Arkansas. Social Work in Public Health, 28(1), 32–43. [DOI] [PubMed] [Google Scholar]
- 38.Sentell T, & Braun KL (2012). Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. Journal of Health Communication, 17(Suppl 3), S82–S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mas FS, Jacobson HE, & Dong Y (2014). Health literacy level of Hispanic college students. Southern Medical Journal, 107(2), 61–65. doi: 10.1097/SMJ.0000000000000050. [DOI] [PubMed] [Google Scholar]


