Abstract
Objective:
To equip clinicians with recommendations specific to concerns related to the novel coronavirus disease 2019 (COVID-19), which impact the physical, emotional, and social health of youth with headache disorders.
Background:
COVID-19 has affected societies on a global scale including children and youth with chronic headache disorders. Many concerns are predicted to arise in the 2020–2021 school year, whether classes are conducted in-person or virtual.
Methods:
Clinical impressions were combined with a review of the literature, although limited due to the recency of this issue.
Results:
We describe recommendations to support caregivers and youth as they face changes expected with the return to school this Fall.
Conclusion:
Although there are significant concerns for caregivers and youth with migraine given the context of changes related to the pandemic, there are many recommendations that can help minimize exacerbations of the physical, emotional and social health of youth with chronic migraine.
Introduction
The World Health Organization (WHO) declared the 2019 Novel Coronavirus Disease (COVID-19) as a global pandemic on March 11, 2020. In an unprecedented response, more than 188 countries imposed school closures, affecting more than 1.5 billion youth1. Many schools implemented distance learning platforms for academic continuity, but the quality and accessibility of distance learning varied greatly.
Under normal circumstances schools play a meaningful role in reducing social and racial inequality2, but the “digital divide” has compounded pre-existing educational inequities. It is estimated that 17% of U.S. students do not have access to a computer in the home and 15% lack access to broadband internet in the home3. Families in which parents and guardians work full time, have limited experience using necessary technology, or do not speak English as their primary language faced additional barriers. Schools faced challenges in serving students with disabilities, learning differences, and complex medical issues through distance learning4.
In our clinical experience as headache specialists, distance learning experiences in children and youth with headache have varied. For some, the increased flexibility with distance learning, the ability to self-pace, and the perceived decreased physical and social demands may have been beneficial in alleviating headache burden. Conversely, for others, factors such as increased screen time and poor ergonomics, stress associated with uncertainty and time management, disruption of routine and sleep schedule, difficulty with time-management, stressful home environment, food insecurity, and increased isolation due to the pandemic may have worsened headache burden. There are not yet published data to support or refute these clinical observations.
For the 2020–2021 school year, the United Nations Educational, Scientific and Cultural Organisation (UNESCO) has recommended that return to school be guided by the best interest of the child and overall education, public health, and socio-economic considerations5. The American Academy of Pediatrics (AAP) has taken the position that “all policy considerations for the coming school year should start with the goal of having students physically present in schools”. However, in many locations there are concerns that the AAP’s recommendations to mitigate risk could not be met2. As a result, schools are choosing from different options: full time in-person learning, hybrid learning that combines in-person and virtual days, and a fully virtual program without any in person instruction. Each option has factors that could exacerbate headache disorders.
In these uncertain times we, as clinicians, have more questions than answers for our patients. We have found that discussions with colleagues have been vital in determining creative solutions for the patients seen in our practices. Realizing that we were all facing the same issues, the authors came together to outline the relevant questions. We assigned topics to coauthors with the most knowledge in that area, each of whom incorporated the available, albeit limited, literature, as well as lessons learned from past patients who have utilized non-traditional school settings (cyberschool, homeschool). We then revised the manuscript together, ensuring consensus. This paper is a compilation of expert opinion on how to best help youth with headache disorders as they return to school in light of the COVID-19 pandemic. In some cases the supporting evidence is drawn from the migraine literature, but these recommendations are not migraine-specific. In fact, though our goal as pediatric headache clinicians is to help this group of patients, these recommendations are relevant to children without headaches as well. We organize topics by the acronym SMART: Sleep, Meals, Activity, Relaxation and Stress Management, Trigger avoidance6.
COVID-19-related school changes that may affect headaches
Sleep:
Sleep disorders are a common comorbidity and sleep disturbances are often reported as a headache trigger by children with migraine7–9. Sleep affects quality of life and mood7, and is foundational to all aspects of health.
Problem – Poor sleep quality:
Poor sleep is associated with increased headache severity and disability in youth8, 9. Decreased daily structure in the context of virtual learning may allow for vastly different bed/wake times compared to during a typical school year. Although virtual school could enable sleep schedules more in line with adolescents’ physiological sleep-timing delay10, virtual school may also promote poor sleep hygiene such as working in bed, napping, or staying up very late, which can disrupt the sleep-wake cycle. Excessive/prolonged screen use has also been associated with shorter and poorer quality of sleep11, with a dose-dependent relationship12.
Solution:
Optimizing sleep during virtual learning may help to enhance improved focus, attention, and mood. This may in turn impact self-directed learning expected during virtual instruction13, 14. On a societal level, high schools should comply with the AAP’s recommendation to start both in person and synchronous virtual classes no earlier than 8:30am10. On the individual level, common clinical recommendations are outlined in Table 1. These are largely based on expert opinion, with citations where possible.
Table 1.
Sleep Recommendations for Virtual Learning for Children with Migraine
| Domain | Encourage patients to: |
|---|---|
| Schedule | Develop and maintain a consistent bedtime routine and avoid daytime napping to prevent disruptions to the sleep-wake cycle89 |
| Environment | (A) Use bed only for sleep to strengthen the sleep-bed connection. Find a separate space for schoolwork to avoid worsening head and neck pain90. (B) Sleep when it is dark to ensure optimal pineal gland function (C) Turn off screens at least 1–2 hours before bed to limit blue light exposure91 |
| Health Behaviors | (A) Avoid caffeine and simple sugars that impair sleep onset, especially in the hours before bed89
(B) Have a healthful snack 2 hours before bedtime (C) Exercise regularly during the day to improve sleep onset and maintenance. |
| Nutraceuticals | Consider use of nutraceuticals such as Melatonin92, 93 and Magnesium94, 95 to optimize sleep and migraine prevention when needed. |
Meals:
Healthy diet15 and adequate hydration16 are important healthy habits for youth to maintain for overall health.
Problem – Inconsistent meal times.
Fasting is a commonly reported headache trigger17. Increased unstructured time at home can make maintaining regular eating habits difficult.
Solution:
Children should be encouraged to eat breakfast and not skip meals throughout the day. Setting mobile phone reminders, and parental encouragement can help maintain good habits.
Problem - Dehydration:
One-third of people with migraine report dehydration as a headache trigger18. Universal facial coverings and physical distancing recommendations may hinder the ability to maintain adequate hydration throughout the day.
Solution:
Allowing frequent hydration while considering school safety guidelines will be important for reducing risk of dehydration. Some schools are restricting use of water fountains, but permitting children to refill bottles. Hand hygiene stations near water fountains should be implemented. Although less environmentally conscious, disposable water bottles could mitigate the risk of contamination by avoiding the need to refill water at school. Outdoor classroom settings and physical distancing of at least 6 feet would increase safety for students to remove facial coverings and hydrate during class2.
Problem – Food insecurity and risk of weight gain:
Since the onset of the pandemic, issues with food production and distribution have led to increases in food prices19. Simultaneously, widespread increases in unemployment and underemployment have made purchasing healthy food even harder. This has led to a 130% increase in food insecurity in households with children ≤18 years old from 2018 to 202019. Food insecurity can increase further when children cannot receive free or subsidized meals at school19–22. Food insecurity has been linked to risk of weight gain and obesity19–22, and will be compounded by decreased physical activity and increased screen time21, 23–26. Weight gain and obesity are associated with migraine frequency and disability27, 28. African American and Hispanic children may face disproportionate weight gain during school closures 21, 29, putting them at higher risk of worsening migraine.
Solution:
Some schools successfully delivered lunches to students via school bus21. Local food banks are expanding service during the crisis to specifically address food insecurity (additional information can be found at http://feedingamerica.org). Increasing access to local farmers markets and providing free membership to co-op markets with cheaper produce could be an additional way to help youth obtain more healthful food21 As much as possible, children should eat a balanced diet filled with green leafy vegetables, fruit, and protein. Frozen fruit, vegetables, and dry goods like lentil and beans with long shelf lives are more healthful than heavily processed foods and can help limit shopping trips.
Activity:
There is evidence that physical activity reduces migraine frequency, intensity, and duration30. In contrast, prolonged positions and poor posture can trigger and/or exacerbate migraine symptoms31–33.
Problem – Disruption in regular exercise:
Given national requirements of shelter-in-place and social distancing, many youth have experienced a disruption in typical extracurricular activities, sports, access to outdoor space, and daily exercise. This disruption is expected to persist through the upcoming academic school year.
Solution:
Exercising daily can help children and youth maintain structure and good overall mental and physical health15, 34. While exercise has not been studied specifically in pediatric headache, studies in adults have demonstrated benefit of physical activity in headache management30, 35. Consideration of a reward system for daily/weekly activity or encouraging children to work out “with” friends by phone or video can help increase motivation. Involving youth in identifying activities of interest may also increase engagement in physical exercise. Specific suggestions are available:
Problem – Prolonged sitting:
Online classes may result in prolonged sitting and increased time using technology, which have been shown to have negative impacts to posture, neck pain and headaches31–33.
Solution:
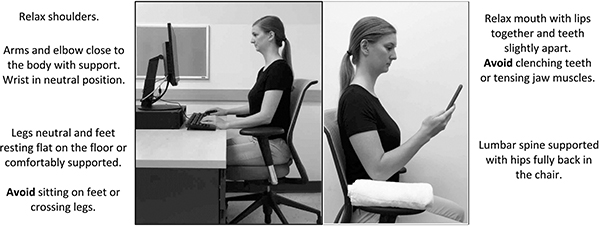
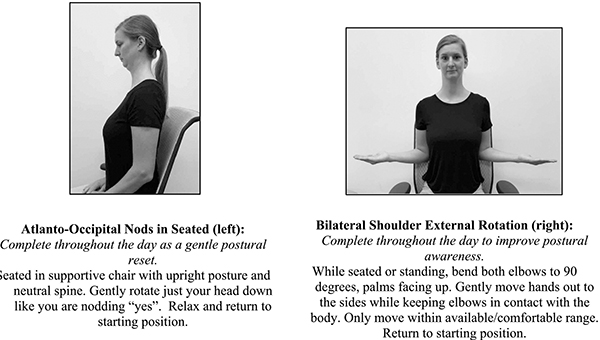
Neutral positioning while completing school work can help improve posture and reduce neck pain31, 32, 36. A simple way to optimize ergonomics is to sit at a table with a chair rather than working on a bed or couch. Computer screen heights can be brought to eye level by elevating the monitor or the child’s seat with books. Holding books or small electronic devices at eye level with elbow support or propping them up is also recommended. Frequent position changes and scheduled movement breaks throughout the day are key. Interventions focused on the cervical spine and shoulder girdle can have a positive effect on headaches37(See Appendix I).
Problem – Carrying a heavy load:
Requirements for individualized school supplies and hybrid learning models may require students to carry increased materials to and from school. Carrying a backpack promotes forward head position and activation of sternocleidomastoid and upper trapezius38 postures known to influence headaches39–43.
Solution:
Students should only carry essential items in their backpacks and place heavier items (such as textbooks) closer to their backs to reduce orthopedic stress44. Students should reduce time carrying backpacks and use assigned lockers or desk space to house supplies, as a recent study found wear time, not relative weight, as the significant contributor of postural pain45.
Relaxation and Stress Management:
Pandemic-related societal changes have had a direct psychosocial impact on the wellbeing of children46, 47 and can exacerbate headache via numerous mechanisms.
Problem – Decreased boundaries between home and school.
Many activities that previously took place outside of the home (e.g., socialization, academics) now take place online. This can create difficulties with identifying and maintaining healthy boundaries and contribute to feelings of burn out.
Solution:
Children and caregivers are recommended to identify a structured day including consistent sleep/wake time, exercise, hydration, meals, and relaxation, as well as class and homework time with specific goals to maintain boundaries throughout weekdays and disconnect more on the weekends. Caregivers are encouraged to identify regular socialization opportunities (e.g., video chat; outdoor socially-distanced peer activities). To create boundaries with social media use, families may set notifications on mobile phones for prolonged time on social media.
Problem – Increased mental health concerns.
Uncertainty, coupled with the influx of constant news and social media, may increase anxiety and worsen headache48, 49. Manifestations of anxiety in youth can present as externalizing behavior (i.e., acting out, arguing), worry, panic and/or increased somatic complaints50. Depressive symptoms are likely to arise with social isolation, uncertainty about the future, concerns for family members’ health, and financial hardships resulting from increases in unemployment and job insecurity due to the pandemic51. Indeed, research in China52, Italy and Spain53 has found higher rates of mental health concerns in children following onset of the pandemic.
Solution:
It is important that caregivers provide space for children to share their concerns and worries. Simultaneously, it is recommended families balance the need to stay informed with engagement in non-COVID-19 related thoughts/conversations54. Spending time with family and working on schoolwork was found to be related to lower depressive symptoms in a recent study of adolescents during the COVID-19 crisis55. To facilitate social learning experiences some families plan to supplement virtual learning with in person “learning pods” with a paid tutor. Though this option is likely out of reach for many families, it may be possible to create virtual or distanced in-person study groups or social time.
The use of relaxation strategies (e.g., diaphragmatic breathing, progressive muscle relaxation, guided imagery) are evidenced to be effective for headache prevention and stress management56. Mindfulness strategies have also been found to decrease disability and symptom impact among children with chronic pain57. Children are encouraged integrate these strategies into their day, and can consider accessing various mobile applications for guided exercises and motivation to stay consistent with these practices. Studies have demonstrated patient acceptance of mobile app interventions58, but have not tested efficacy of the publicly available apps. In our clinical practice we have recommended the following - Stop, Breathe and Think, Headspace, Calm, and Relax Melodies – though this list is not exhaustive. Please see the below tables with more specific clinical suggestions on how children with headaches (Table 2) and their caregivers (Table 3) can support emotional health during the transition back to school59. Again, many of these are based on expert opinion, but evidence is cited where available.
Table 2.
Guidance for Children with Headaches to Support Emotional Health and Minimize Stress as a Headache Trigger during COVID-19 Pandemic
| Domain | Encourage Children to: |
|---|---|
| Structure | (A) Maintain a consistent schedule with sleep/wake time, good sleep hygiene, healthy eating habits (not skipping meals), daily exercise and good hydration96 (See Gelfand “Lifestyle Advice” for discussion34). Write this schedule down or design a “reward system” for adherence. (B) When possible, set up a workspace that it is free of clutter or distractions, maximizing focus and concentration97. This could be a desk or a table but not the bed, which should only be used for sleep. (C) Pacing is important. Maintain a daily structure including both activities and academic work that feels manageable irrespective of headache. Take breaks as needed98. |
| Positive Activities | (A) Schedule safe, enjoyable social and/or solo activities daily99. (B) Consider engaging in a new activity or learning a new skill (e.g., an art project, a podcast, an interesting online course, a new language). See also https://ppainsig.weebly.com/clinical.html (C) Stick to plans even if motivation is low. Engaging in enjoyed activities even on a bad day can help boost mood. |
Table 3.
Guidance for Caregivers of Children with Headaches to Support Emotional Health and Minimize Stress as a Headache Trigger during COVID-19 Pandemic
| Domain | Caregivers are encouraged to: |
|---|---|
| Engage in Parental Self Care | Identify the areas in which the caregiver her/himself may be struggling with the pandemic (e.g., anxiety, social isolation). Engage in “coping behaviors” (e.g., exercising, journaling, taking deep breaths) and seek support as needed. Children can be affected by parental stress. |
| Model Emotional and Physical Health Behaviors | (A) Discuss the above coping mechanisms with children to demonstrate the value of self-care. (B) Model social distancing, wearing a mask, and washing hands in a calm and consistent manner. |
| Provide Emotional Support | (A) Normalize and validate the child’s experience while encouraging open communication regarding thoughts, feelings and worries with returning to school50. Pair empathy with encouragement: “I know this is scary, and I know you can do it!” (B) Help the child identify a “menu” of coping skills (e.g., 10 deep breaths, drawing, taking a short mask or water/snack break at school). (C) Explain the specific changes in school (e.g., wearing masks, limiting time in school) and the impact your child has on maintaining safety for her/his peers, staff and their families to create a sense of empowerment. (D) Support the child in gradually engaging in anxiety provoking activities to help them habituate, or become used to, the activities (e.g., wearing masks around the home while engaging in enjoyed activities)100. |
| Create Structure | (A) Consider ways to organize the child’s daily and weekly school responsibilities to remain caught up on schoolwork and minimize the potential of increased stress that could trigger a headache attack and/or interfere with sleep schedule and mood. (B) Discuss details of the school’s current plan (e.g., schedule for online coursework) and secondary plan (e.g., what a planned hybrid model might look like). (C) Create a “COVID Kit” of materials that will help the child at school (e.g., an extra mask, extra pens, hand sanitizer). (D) Develop a plan for quarantine procedures in the event of exposure. Where will your child stay? How will they receive meals and medical care in this time? |
| Advocate with School | (A) Connect with the school community and identify specific school staff that the child can contact should they experience a migraine attack or need extra support. (B) Consider requesting a meeting with identified teachers, school counselor and nurse to discuss a medical plan and supports for your child. (C) For children with existing 504 or IEP plans, place a request to the school in writing to modify accommodations to the current school environment. Special education laws and regulations are not waived during the pandemic101. |
| Seek Support | (A) Remind the child that experiencing anxiety at this time is normal and expected. Worries about exposure to the virus or getting others sick can help motivate protective behaviors (wearing a mask, washing hands). (B) If these behaviors and worries begin to interfere with typical functioning, contact a behavioral health provide for increased support. |
Problem – Social difficulties and worries with returning to in-person school.
Some children have significant social concerns related to school (e.g., bullying, social anxiety), and endorsed increased emotional comfort secondary to shelter-in-place orders. After prolonged absence, these children may experience increased anxiety with the return to in-person school, exacerbating headache. It is also expected that symptoms of anxiety may arise from changes in school environment secondary to COVID-19 (e.g., physically distanced desks, fear of exposure to the virus).
Solution:
Gently but persistently inquire as to these challenges with the child without judgement. Help children identify specific fears about returning to school. Focus on listening, rather than offering advice and trust what the child says. Involve the child in any choices made to address the problem (e.g., informing teachers or school administration). Encourage children and their parents to practice challenging situations they are likely to encounter, create a list of phrases that they can use, and identify an ally at school. Consider using the Pediatric Migraine Action Plan60 for school, and writing in specific accommodations for this year. For children with frequent and very disabling headaches see Appendix II for a suggested 504 request letter template.
Problem – Adverse Childhood Experiences (ACEs):
In times of stress and uncertainty, parent-child relationships can face strain due to increased proximity and conflict or experiences of caregiving fatigue61. Increases in harsh parenting tend to accompany times of economic distress62 and increased time at home may further exacerbate the issue, leading to increased violence in the home. Simultaneously, in-person access to mandated reporters (schools and medical offices) is decreased63 which in turn can lead to prolonged exposure to adverse childhood experiences (ACEs; physical/emotional/sexual abuse and neglect, exposure to mental illness in household, witnessing domestic violence, divorce, substance-abuse). ACE exposure has been found to contribute to frequent headache64 and learning difficulties65. Increased ACEs and their negative effects on neurological outcomes also contribute to disparities in health, as communities of color often carry disproportionately higher burdens of ACE exposure and trauma66.
Solution:
Ensure appropriate questions are asked during medical visits to help screen for ACEs and provide resources to families. The Centers for Disease Control and Prevention (CDC) provides resources for both children and parents on the Coronavirus Disease 2019 website67 and the American Academy of Pediatrics released guidance on effective parenting while dealing with stress of the pandemic68. Multiple ACE screeners are also available online69,70. One simple question to incorporate in every medical appointment is, “Do you feel safe in the home?” Discussing methods of maintaining confidentiality at the start of a telehealth appointment (e.g., using headphones, ensuring doors are closed) may reduce fears of honest disclosure.
Trigger Avoidance:
Many common triggers such as dehydration, fasting, sleep problems, and stressors were discussed above. Here we highlight screen use and mask wearing as potential additional school-related triggers.
Screen Use:
Virtual learning has increased reliance on computer screens, which can create visual discomfort and is thought to trigger or exacerbate headaches due to prolonged screen exposure. While evidence for this is limited, increased exposure to screens (including smartphones, tablets, computers, and television) has been associated with higher risk of migraine in adolescents and young adults69. This presents potential challenges to managing headache and promoting healthy sleep habits.
Problem – Screens cause eye strain and dry eyes:
Frequent computer use can cause eye strain, eye fatigue, irritation, redness, blurry vision, and double vision70. Dry eye appears to be the most significant contributor to these symptoms70, and is particularly prevalent in individuals with chronic migraine71, 72.
Solution:
The use of artificial tears can be used to combat dry eye. In addition, regular practice of yoga has been associated with reduced visual discomfort from computer screens73.
Problem – Brightness from screens:
Computer screens are thought to both trigger and exacerbate migraine attacks, though there is only limited evidence showing correlation between increased screen time and risk of migraine69.
Solutions:
We recommend striking a balance between reducing visual triggers and gradual exposure to make viewing more tolerable over time.
Planned exposure to screens may increase tolerance over time. Bright flickering light causes visual disturbance and head pain in individuals with regular headaches. However, these symptoms were reduced with prolonged exposure (>30 minutes) to the same bright flickering light74. Indeed, strategies that involve learning to cope with triggers (including visual triggers) have shown promise in reducing headache frequency75. One approach includes taking breaks from screen exposure just before headache usually starts to develop, and gradually increasing the amount of time spent continuously at the computer76. Focusing on an object greater than 20 feet away about every 30 minutes is thought to reduce eye strain by taking a break from viewing close objects like a computer screen77. Additionally, providing paper options for reading or assignments when possible may be beneficial.
Work area lighting: Having a similar level of brightness across visual space may improve visual comfort. This includes reducing exposure to intense florescent lights, and excessive window lighting70.
Monitor refresh rate: Certain flicker frequencies especially in the 10–30 Hz range can be particularly uncomfortable to individuals with migraine78. While evidence is quite limited, selecting a monitor with a higher refresh rate when possible may be helpful.
- Light filtering glasses and computer screen covers: When prolonged screen use is unavoidable, methods that reduce exposure to certain wavelengths of light may be helpful. Options to filter light from computer screens include tinted glasses, physical filters that cover computer screens, and altering the display. While the evidence is mixed, it is reasonable to use these filters if they are perceived to be helpful.
- Blue light blocking filters have a positive impact on sleep and counteract the melatonin suppression triggered by LED screens, especially when used 2 hours before bed79, 80, and can improve eye-fatigue and dryness79. However, at least one study did not find a reduction in migraine attack frequency81.
- It has been reported that exposure to green light can be less exacerbating to individuals experiencing migraine86.
Mask-related headaches:
Can wearing a mask cause headaches? Theoretically, the answer is “yes”, but in practice, it is unlikely to do so.
Problem: Pressure created by the mask or its straps against various contact points on the face or scalp could trigger headache.
This issue was highlighted in a recent study of health care workers in Singapore who were required to wear N95 masks for approximately 6 hours a day. Over one month, 81% had experienced new headaches87. The location of their pain closely mirrored the mask’s contact points at the nasal bridge and cheeks as well as strap’s contact against the temples and the back of the head. Those wearing masks for longer than 4 hours a day and those with pre-existing primary headache disorders were more likely to experience mask-related headache than their peers.
Solution:
The cloth or surgical masks most commonly worn are looser-fitting than N95 masks and typically secured behind the ears, which should not produce the same degree of pressure against the face and scalp, and are therefore less likely to trigger headaches. Youth who find ear loops uncomfortable could try wearing a mask extender or a cloth headband with a button around which to fasten the ear loops. Alternately, try a mask which can be tied at the back of the head at a higher or lower position for comfort.
Hopeful Prospects of the COVID-19 Pandemic
The COVID-19 pandemic has transformed the world and touched every aspect of daily life. As highlighted in this article, there are countless domains in which the novel virus has negatively impacted schools and children, including those with headache disorders. However, the impact on students varies widely depending on a number of external and internal factors, and there may be some “silver linings.”
At a societal level, the COVID-19 pandemic has drawn attention to disparities in education for children and adolescents based on race, geography, and socioeconomic status that have been left unaddressed for far too long. At a family unit level, with caregivers taking on the role of teacher, appreciation of the strengths and weaknesses of their child’s scholastic achievement, socialization and resiliency may be more apparent. On an individual level, for youth who excelled or experienced a reduction in headache during this time, it will be a matter of understanding what changes fostered positive outcomes88. For example, some schools may learn to tailor the school environment and educational format to better suit that child’s needs (e.g., provide more flexibility to allow for breaks, meals, hydration, sleep; more one-on-one learning, self-paced learning) and some students and families may advocate for access to needed supports (e.g., school counselors to help intervene with bullying or teach strategies to manage social anxiety and school stress).
As many crises have done before, perhaps the difficulties and struggles central to families’ current experiences will build resilience in youth, and highlight paths to long-term, positive change.
Acknowledgments
Funding: Dr. Szperka is supported by NINDS K23 NS102521
Disclosures:
Dr VanderPluym consults for Teva and has a research grant from Amgen. Dr. Patterson Gentile has received grant support from the American Academy of Neurology and the American Headache Society. Dr. Szperka has received grant support from Pfizer, NINDS, and FDA. She has consulted for Teva and Lundbeck. All other authors report no disclosures.
Appendix I
Illustration demonstrating an ergonomic student workspace at home with neutral spine.
When using smaller electronic devices limit prolonged cervical flexion by raising the objects up closer to eye level while maintaining a neutral spine.
Appendix II:
Accommodations Letter (adapted from UCSF Child & Adolescent Headache Program)
To Whom It May Concern:
[Patient Name] is a patient at [Institution/Primary Care Practice] and is under our care for [Headache Diagnosis].
[Headache Diagnosis] can be debilitating, interfering with academics, socialization, mood, and overall functioning. The interactive effect of impairments associated with headache and disruptions in typical socialization, enjoyed activities, and academics due to the COVID-19 pandemic may contribute to difficulties with adjustment, mood, and overall coping.
We understand that children will be engaging in different models of education this year and encourage consideration of specific accommodations to help support our patients with headaches as they return to school. We continue to encourage our patients to maintain a healthy lifestyle with good hydration, sleep, exercise, regular meals and coping strategies for stress/headache management and emphasize the importance of continued functioning despite symptoms.
We recommend a 504 plan to establish appropriate accommodations to maximize learning opportunities for [Patient Name]:
-
School Accommodations Point Person: We recommend that [Patient Name] have a point person at school to support [her/him] in refining [her/his] school accommodation plan and communicating with teachers and school staff members throughout the year.
[Patient Name] would benefit from regular check-ins with this point person to help [her/him] stay on-task with required assignments and problem solve any barriers to the below plan.
Breaks: Please allow [Patient Name] to take breaks as needed both for optimal management of [her/his] headache disorder.
Absences: We encourage daily school attendance. However, please excuse rare absences due to headaches. Similarly, if [Patient Name] is unable to attend for the full day due to headache, please excuse late arrival or early dismissal. We have instructed [Patient Name] to contact our office if [she/he] misses school frequently.
Assignments: Please allow extra time to complete assignments and exams, as productivity can be greatly reduced during headache. When possible, please give [Patient Name] assignments one week beforehand so that [she/he] can work on them when headaches are less disabling.
- Schedule: For [her/his] age group, 8–10 hours a night of sleep are recommended. The American Academy of Pediatrics recommends that high schools begin no earlier than 8:30 AM, in recognition of adolescents’ physiologic tendency to go to bed later and wake later than younger children. I recommend scheduling [her/his] first period class as either an empty slot, or a course that can be flexibly attended (such as an art class). Adequate sleep is essential to headache management.Sleep duration recommendations from the American Academy of Sleep Medicine (2016):Children 3 to 5 years old: 10–13 hoursChildren 6 to 12 years old: 9–12 hoursTeenagers 13–18 years old: 8–10 hours
Privacy: While [Patient Name]’s family is comfortable with teachers and relevant school personnel knowing about [her/his] condition, we appreciate your keeping [her/his] medical information confidential.
-
Accommodations Specific to Remote Learning: Prolonged screen time can provoke or worsen a migraine headache. In general, we recommend limiting the time [Patient Name] is required to be on [her/his] screen to the greatest extent possible.
Alternate assignments: When possible, please provide materials that can be shifted to a paper format as opposed to electronically. For example, completing homework assignments on paper that can then be sent via pdf (if the student has access to a printer) or provided in workbook form. Additional we recommend considering alternative mechanisms to earn course credit to minimize screen time.
Recording lessons: As concentration may be challenging during headache, consider recording live lessons or allowing [Patient Name] to record the lesson so [she/he] can go back to watch what [she/he] may have missed at a later time.
-
Breaks from screens: Please allow frequent breaks from screens.
Please allow [Patient Name] to turn the screen off, if desired, and allow for audio only.
Please allow [Patient Name] to turn off the camera, if desired, to allow [her/him] to dim [her/his] lights or not look at the screen as needed.
Allow use of audiobooks or text-to-speech technology to help minimize time on the screen.
Communication: As communicating while distance learning can be challenging, please support [Patient Name] in developing a system to help ease regular communication (e.g. regular email to check-in, chat function to ask questions, ‘office hours’ for students to ask questions).
-
Accommodations Specific to In-Person Classroom Learning
Hydration: Please allow [Patient Name] to keep a water bottle with [her/him] in the classroom or set up a plan where [she/he] can easily step away from [her/his] classmates to drink water at an appropriate distance. Please also allow trips to the bathroom as needed, without restriction.
Snacks: Please allow [Patient Name] access to snacks at school. Please support [Patient Name] in setting up a plan where [she/he] can easily step away from [her/his] classmates to have a snack at an appropriate distance.
Medication: At onset or worsening of headache- please allow [Patient Name] to take [her/his] acute medications and rest in a safe and quiet area at the nurse’s office, or a supervised equivalent.
-
Environment: Headaches can be exacerbated by movement, overheating, dehydration, light, sounds, and smell.
[Patient Name] should exercise regularly, but may need modifications to Physical Education class to avoid headache flares during the school day. Please allow [her/him] to participate in physical activities as [she/he] is able, and allow rest/hydration as needed.
Please allow [her/him] to be in settings/conditions as needed that can minimize bright lights, sounds, and smells. Please allow [her/him] to take breaks as needed in such a location.
Other accommodations to be discussed by [Patient Name], [her/his] family, and the school.
We sincerely appreciate your understanding and assistance in optimizing [Patient Name]’s attendance and performance in school related activities with an appropriate regard for [Patient Name]’s diagnosis, especially during this challenging time.
Ongoing communication between the school, family, and medical team is vital to ensuring [Patient Name]’s success in these efforts. Please feel free to reach out to our office with any questions you may have.
Sincerely,
[Treating Clinician]
[Institution/Primary Care Practice]
References:
- 1.dashboard UM-atUE. COVID-19 and Children [online] [online]. [Google Scholar]
- 2.Pediatrics AAo. COVID-19 Planning Considerations: Guidance for School Re-entry [online]. [online]. Available at: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/.
- 3.Anderson MP, Andrew. Nearly one-in-five teens can’t always finish their homework because of the digital divide: Pew Research Center, 2018 October 26, 2018.
- 4.United Nations oAa. Policy Brief: The Impact of COVID-19 on children [online]. Available at: https://www.un.org/sites/un2.un.org/files/policy_brief_on_covid_impact_on_children_16_april_2020.pdf. Accessed August 6.
- 5.UNESCO. Framework for School Reopening [online]. Available at: https://en.unesco.org/news/framework-school-reopening. Accessed August 6.
- 6.Blume HK, Szperka CL. Secondary causes of headaches in children: when it isn’t a migraine. Pediatric annals 2010;39:431–439. [DOI] [PubMed] [Google Scholar]
- 7.Zeitlhofer J, Schmeiser-Rieder A, Tribl G, et al. Sleep and quality of life in the Austrian population. Acta Neurologica Scandinavica 2000;102:249–257. [DOI] [PubMed] [Google Scholar]
- 8.Clementi MA, Chang YH, Gambhir R, Lebel A, Logan DE. The Impact of Sleep on Disability and School Functioning: Results From a Tertiary Pediatric Headache Center. Journal of child neurology 2020;35:221–227. [DOI] [PubMed] [Google Scholar]
- 9.Gilman DK, Palermo TM, Kabbouche MA, Hershey AD, Powers SW. Primary headache and sleep disturbances in adolescents. Headache 2007;47:1189–1194. [DOI] [PubMed] [Google Scholar]
- 10.Gelfand AA, Pavitt S, Greene K, et al. High School Start Time and Migraine Frequency in High School Students. Headache 2019;59:1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kenney EL, Gortmaker SL. United States adolescents’ television, computer, videogame, smartphone, and tablet use: associations with sugary drinks, sleep, physical activity, and obesity. The Journal of pediatrics 2017;182:144–149. [DOI] [PubMed] [Google Scholar]
- 12.Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, Sivertsen B. Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 2015;5:e006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langdon R, DiSabella M, Strelzik J, Fletcher A. Pediatric Migraine and Academics. Curr Pain Headache Rep 2020;24:40. [DOI] [PubMed] [Google Scholar]
- 14.Genizi J, Gordon S, Kerem NC, Srugo I, Shahar E, Ravid S. Primary headaches, attention deficit disorder and learning disabilities in children and adolescents. J Headache Pain 2013;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics 2003;112:424–430. [DOI] [PubMed] [Google Scholar]
- 16.Medicine Io. Dietary Reference Intakes for Water, Potassium, Sodium Chloride, and Sulfate. Available at 10.17226/109252005. [DOI]
- 17.Peris F, Donoghue S, Torres F, Mian A, Wober C. Towards improved migraine management: Determining potential trigger factors in individual patients. Cephalalgia : an international journal of headache 2017;37:452–463. [DOI] [PubMed] [Google Scholar]
- 18.Top 10 Migraine Triggers and How to Deal with Them [online]. Available at: https://americanmigrainefoundation.org/resource-library/top-10-migraine-triggers/. Accessed August 3.
- 19.Paslakis G, Dimitropoulos G, Katzman DK. A call to action to address COVID-19-induced global food insecurity to prevent hunger, malnutrition, and eating pathology. Nutr Rev 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinsey EW, Hammer J, Dupuis R, Feuerstein-Simon R, Cannuscio CC. Planning for Food Access During Emergencies: Missed Meals in Philadelphia. Am J Public Health 2019;109:781–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity (Silver Spring) 2020;28:1008–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet 2012;112:1949–1958. [DOI] [PubMed] [Google Scholar]
- 23.von Hippel PT, Workman J. From Kindergarten Through Second Grade, U.S. Children’s Obesity Prevalence Grows Only During Summer Vacations. Obesity (Silver Spring) 2016;24:2296–2300. [DOI] [PubMed] [Google Scholar]
- 24.Wang YC, Vine S, Hsiao A, Rundle A, Goldsmith J. Weight-related behaviors when children are in school versus on summer breaks: does income matter? J Sch Health 2015;85:458–466. [DOI] [PubMed] [Google Scholar]
- 25.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis 2014;11:E101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calcaterra V, Vandoni M, Pellino VC, Cena H. Special Attention to Diet and Physical Activity in Children and Adolescents With Obesity During the Coronavirus Disease-2019 Pandemic. Front Pediatr 2020;8:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oakley CB, Scher AI, Recober A, Peterlin BL. Headache and obesity in the pediatric population. Current pain and headache reports 2014;18:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hershey AD, Powers SW, Nelson TD, et al. Obesity in the pediatric headache population: a multicenter study. Headache 2009;49:170–177. [DOI] [PubMed] [Google Scholar]
- 29.An R Projecting the impact of the coronavirus disease-19 pandemic on childhood obesity in the United States: A microsimulation model. J Sport Health Sci 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krøll LS, Hammarlund CS, Linde M, Gard G, Jensen RH. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia : an international journal of headache 2018;38:1805–1816. [DOI] [PubMed] [Google Scholar]
- 31.Park S-y, Yoo W-g. Effects of the sustained computer work on upper cervical flexion motion. Journal of physical therapy science 2014;26:441–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith L, Louw Q, Crous L, Grimmer-Somers K. Prevalence of neck pain and headaches: impact of computer use and other associative factors. Cephalalgia 2009;29:250–257. [DOI] [PubMed] [Google Scholar]
- 33.Uttarwar P, Vibha D, Prasad K, Srivastava AK, Pandit AK, Dwivedi SN. Smartphone use and primary headache: A cross-sectional hospital-based study. Neurology: Clinical Practice 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gelfand AA, Irwin SL. Lifestyle Advice for Pediatric Migraine: Blaming the Patient, or Evidence Based? Seminars in neurology 2020;40:277–285. [DOI] [PubMed] [Google Scholar]
- 35.Hanssen H, Minghetti A, Magon S, et al. Effects of different endurance exercise modalities on migraine days and cerebrovascular health in episodic migraineurs: A randomized controlled trial. Scandinavian journal of medicine & science in sports 2018;28:1103–1112. [DOI] [PubMed] [Google Scholar]
- 36.Fabrizio P Ergonomic intervention in the treatment of a patient with upper extremity and neck pain. Physical therapy 2009;89:351–360. [DOI] [PubMed] [Google Scholar]
- 37.Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy 2017;47:A1–A83. [DOI] [PubMed] [Google Scholar]
- 38.Kim M, Yi C, Kwon O, Cho S, Yoo W. Changes in neck muscle electromyography and forward head posture of children when carrying schoolbags. Ergonomics 2008;51:890–901. [DOI] [PubMed] [Google Scholar]
- 39.Bevilaqua-Grossi D, Gonçalves MC, Carvalho GF, et al. Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2016;97:866–874. [DOI] [PubMed] [Google Scholar]
- 40.Blaschek A, Milde-Busch A, Straube A, et al. Self-reported muscle pain in adolescents with migraine and tension-type headache. Cephalalgia : an international journal of headache 2012;32:241–249. [DOI] [PubMed] [Google Scholar]
- 41.Luedtke K, Starke W, May A. Musculoskeletal dysfunction in migraine patients. Cephalalgia 2018;38:865–875. [DOI] [PubMed] [Google Scholar]
- 42.Szikszay TM, Hoenick S, von Korn K, et al. Which examination tests detect differences in cervical musculoskeletal impairments in people with migraine? A systematic review and meta-analysis. Physical therapy 2019;99:549–569. [DOI] [PubMed] [Google Scholar]
- 43.Kellis E, Emmanouilidou M. The effects of age and gender on the weight and use of schoolbags. Pediatric Physical Therapy 2010;22:17–25. [DOI] [PubMed] [Google Scholar]
- 44.Chow D, Ou Z, Wang X, Lai A. Short-term effects of backpack load placement on spine deformation and repositioning error in schoolchildren. Ergonomics 2010;53:56–64. [DOI] [PubMed] [Google Scholar]
- 45.MacCabe A, Berg-Poppe P, Arnott M. Adolescent Back Pain and Associated Backpack Loading, Locker Use, and Online Textbook Alternatives. International Journal of School Health 2017;4:1–7. [Google Scholar]
- 46.Gifford-Smith ME, Brownell CA. Childhood peer relationships: Social acceptance, friendships, and peer networks. Journal of school psychology 2003;41:235–284. [Google Scholar]
- 47.Oberle E, Schonert-Reichl KA, Thomson KC. Understanding the link between social and emotional well-being and peer relations in early adolescence: Gender-specific predictors of peer acceptance. Journal of Youth and Adolescence 2010;39:1330–1342. [DOI] [PubMed] [Google Scholar]
- 48.Barthorpe A, Winstone L, Mars B, Moran P. Is social media screen time really associated with poor adolescent mental health? A time use diary study. Journal of Affective Disorders 2020;274:864–870. [DOI] [PubMed] [Google Scholar]
- 49.Twenge JM, Farley E. Not all screen time is created equal: associations with mental health vary by activity and gender. Social Psychiatry and Psychiatric Epidemiology 2020. [DOI] [PubMed] [Google Scholar]
- 50.Dalton L, Rapa E, Stein A. Protecting the psychological health of children through effective communication about COVID-19. The Lancet Child & Adolescent Health 2020;4:346–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and adolescent psychiatry and mental health 2020;14:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liang L, Ren H, Cao R, et al. The effect of COVID-19 on youth mental health. Psychiatric Quarterly 2020:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Orgilés M, Morales A, Delvecchio E, Mazzeschi C, Espada JP. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. 2020. [DOI] [PMC free article] [PubMed]
- 54.Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ellis WE, Dumas TM, Forbes LM. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement 2020;52:177–187. [Google Scholar]
- 56.Holden EW, Deichmann MM, Levy JD. Empirically supported treatments in pediatric psychology: recurrent pediatric headache. Journal of pediatric psychology 1999;24:91–109. [DOI] [PubMed] [Google Scholar]
- 57.Ali A, Weiss TR, Dutton A, et al. Mindfulness-Based Stress Reduction for Adolescents with Functional Somatic Syndromes: A Pilot Cohort Study. The Journal of pediatrics 2017;183:184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Minen MT, Torous J, Raynowska J, et al. Electronic behavioral interventions for headache: a systematic review. The journal of headache and pain 2016;17:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.O’Rourke S, Williams S, Goya Arce A, Swanger-Gagne M, Allen J, & Boerner K. Anxiety with Return to Modified School. [online]. Available at: https://ppainsig.weebly.com/clinical.html. [Google Scholar]
- 60.Turner SB, Rende EK, Pezzuto T, et al. Pediatric Migraine Action Plan (PedMAP). Headache 2019;59:1871–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist 2020. [DOI] [PubMed] [Google Scholar]
- 62.Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Children and youth services review 2017;72:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thomas EY, Anurudran A, Robb K, Burke TF. Spotlight on child abuse and neglect response in the time of COVID-19. The Lancet Public Health 2020;5:e371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache 2010;50:1473–1481. [DOI] [PubMed] [Google Scholar]
- 65.Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child abuse & neglect 2011;35:408–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Crouch E, Probst JC, Radcliff E, Bennett KJ, McKinney SH. Prevalence of adverse childhood experiences (ACEs) among US children. Child abuse & neglect 2019;92:209–218. [DOI] [PubMed] [Google Scholar]
- 67.Prevention CfDCa. Coronavirus (COVID-19) [online]. Available at: https://www.cdc.gov/coronavirus/2019-ncov/index.html.
- 68.Pediatrics AAo. Press Release for Parents Experiencing Stress Over COVID-19. . 2020. [Google Scholar]
- 69.Montagni I, Guichard E, Carpenet C, Tzourio C, Kurth T. Screen time exposure and reporting of headaches in young adults: A cross-sectional study. Cephalalgia : an international journal of headache 2016;36:1020–1027. [DOI] [PubMed] [Google Scholar]
- 70.Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol 2005;50:253–262. [DOI] [PubMed] [Google Scholar]
- 71.Kinard KI, Smith AG, Singleton JR, et al. Chronic migraine is associated with reduced corneal nerve fiber density and symptoms of dry eye. Headache 2015;55:543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koktekir BE, Celik G, Karalezli A, Kal A. Dry eyes and migraines: is there really a correlation? Cornea 2012;31:1414–1416. [DOI] [PubMed] [Google Scholar]
- 73.Vincent AJ, Spierings EL, Messinger HB. A controlled study of visual symptoms and eye strain factors in chronic headache. Headache 1989;29:523–527. [DOI] [PubMed] [Google Scholar]
- 74.Martin PR. How do trigger factors acquire the capacity to precipitate headaches? Behaviour research and therapy 2001;39:545–554. [DOI] [PubMed] [Google Scholar]
- 75.Martin PR, Reece J, Callan M, et al. Behavioral management of the triggers of recurrent headache: a randomized controlled trial. Behaviour research and therapy 2014;61:1–11. [DOI] [PubMed] [Google Scholar]
- 76.Martin PR. Behavioral management of migraine headache triggers: learning to cope with triggers. Current pain and headache reports 2010;14:221–227. [DOI] [PubMed] [Google Scholar]
- 77.Cheu R Good vision at work. Occupational health and safety 1998;67:20–24. [PubMed] [Google Scholar]
- 78.Karanovic O, Thabet M, Wilson HR, Wilkinson F. Detection and discrimination of flicker contrast in migraine. Cephalalgia : an international journal of headache 2011;31:723–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ayaki M, Hattori A, Maruyama Y, Tsubota K, Negishi K, Bahler J. Large-scale integration in tablet screens for blue-light reduction with optimized color: The effects on sleep, sleepiness, and ocular parameters. Cogent Biology 2017;3. [Google Scholar]
- 80.van der Lely S, Frey S, Garbazza C, et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J Adolesc Health 2015;56:113–119. [DOI] [PubMed] [Google Scholar]
- 81.Suzuki A, Tatsumoto M, Suzuki T, Hirata K. Are blue-light blocking eyeglasses beneficial to migraine patients? CEPHALALGIA; 2015: SAGE PUBLICATIONS LTD 1 OLIVERS YARD, 55 CITY ROAD, LONDON EC1Y 1SP, ENGLAND: 36–36.24812036 [Google Scholar]
- 82.Harle DE, Shepherd AJ, Evans BJ. Visual stimuli are common triggers of migraine and are associated with pattern glare. Headache: The Journal of Head and Face Pain 2006;46:1431–1440. [DOI] [PubMed] [Google Scholar]
- 83.Evans BJ, Patel R, Wilkins AJ. Optometric function in visually sensitive migraine before and after treatment with tinted spectacles. Ophthalmic Physiol Opt 2002;22:130–142. [DOI] [PubMed] [Google Scholar]
- 84.Huang J, Zong X, Wilkins A, Jenkins B, Bozoki A, Cao Y. fMRI evidence that precision ophthalmic tints reduce cortical hyperactivation in migraine. Cephalalgia : an international journal of headache 2011;31:925–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Good PA, Taylor RH, Mortimer MJ. The use of tinted glasses in childhood migraine. Headache 1991;31:533–536. [DOI] [PubMed] [Google Scholar]
- 86.Noseda R, Reuven-Nir R, Bernstein C, Borsook D, Buettner C, Burstein R. Green light alleviates migraine photophobia (S47. 005). AAN Enterprises, 2017. [Google Scholar]
- 87.Ong JJ, Bharatendu C, Goh Y, et al. Headaches associated with personal protective equipment–A cross-sectional study among frontline healthcare workers during COVID-19. Headache: The Journal of Head and Face Pain 2020;60:864–877. [DOI] [PubMed] [Google Scholar]
- 88.Schroeder J What if Some Kids Are Better Off at Home? [Opinion]. The New York Times 2020, August 10. [Google Scholar]
- 89.Allen SL, Howlett MD, Coulombe JA, Corkum PV . ABCs of SLEEPING: A review of the evidence behind pediatric sleep practice recommendations. Sleep medicine reviews 2016;29:1–14. [DOI] [PubMed] [Google Scholar]
- 90.Meltzer LJ, Mindell JA. Systematic review and meta-analysis of behavioral interventions for pediatric insomnia. Journal of pediatric psychology 2014;39:932–948. [DOI] [PubMed] [Google Scholar]
- 91.Perrault AA, Bayer L, Peuvrier M, et al. Reducing the use of screen electronic devices in the evening is associated with improved sleep and daytime vigilance in adolescents. Sleep 2019;42. [DOI] [PubMed] [Google Scholar]
- 92.Fallah R, Shoroki FF, Ferdosian F. Safety and efficacy of melatonin in pediatric migraine prophylaxis. Current drug safety 2015;10:132–135. [DOI] [PubMed] [Google Scholar]
- 93.Miano S, Parisi P, Pelliccia A, Luchetti A, Paolino MC, Villa MP. Melatonin to prevent migraine or tension-type headache in children. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology 2008;29:285–287. [DOI] [PubMed] [Google Scholar]
- 94.Wang F, Van Den Eeden SK, Ackerson LM, Salk SE, Reince RH, Elin RJ. Oral magnesium oxide prophylaxis of frequent migrainous headache in children: a randomized, double-blind, placebo-controlled trial. Headache 2003;43:601–610. [DOI] [PubMed] [Google Scholar]
- 95.Gallelli L, Avenoso T, Falcone D, et al. Effects of acetaminophen and ibuprofen in children with migraine receiving preventive treatment with magnesium. Headache 2014;54:313–324. [DOI] [PubMed] [Google Scholar]
- 96.Bektas O, Ugur C, Gencturk ZB, Aysev A, Sireli O, Deda G. Relationship of childhood headaches with preferences in leisure time activities, depression, anxiety and eating habits: A population-based, cross-sectional study. Cephalalgia : an international journal of headache 2015;35:527–537. [DOI] [PubMed] [Google Scholar]
- 97.RH L, CS T. Provide Structure for Children With Learning and Behavior Problems. Intervention in School and Clinic 2005;40:182–187. [Google Scholar]
- 98.Sieberg CB, Huguet A, von Baeyer CL, Seshia S. Psychological interventions for headache in children and adolescents. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques 2012;39:26–34. [DOI] [PubMed] [Google Scholar]
- 99.Martin F, Oliver T. Behavioral activation for children and adolescents: a systematic review of progress and promise. European child & adolescent psychiatry 2019;28:427–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Whiteside SPH, Sim LA, Morrow AS, et al. A Meta-analysis to Guide the Enhancement of CBT for Childhood Anxiety: Exposure Over Anxiety Management. Clinical child and family psychology review 2020;23:102–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.COVID-19 Guidance Memo: Special Education Rights During School Closure Due to Covid-19 [online]. Available at: https://caseadvocacy.org/covid-19-guidance-memo/.