Abstract
Objectives
To examine the relationship between mandibular volume and craniofacial morphology in patients with cleft lip and palate using cone beam computed tomography (CBCT) and to compare these findings with control (noncleft) patients undergoing CBCT for other purposes during the deciduous dentition period.
Materials and Methods
Eighty-four patients were categorized into the unilateral cleft lip and alveolus (UCLA) group (n = 25; mean age, 4.60 ± 0.40 years), unilateral cleft lip and palate (UCLP) group (n = 23; mean age, 4.52 ± 0.39 years), bilateral cleft lip and palate (BCLP) group (n = 22; mean age, 4.54 ± 0.37 years), and control group without cleft (n = 14; mean age, 5.19 ± 0.52 years). Mandibular volume and craniofacial cephalometric measurements were obtained using CBCT. All measurements were assessed by analysis of covariance (ANCOVA) using Bonferroni post hoc pairwise comparison tests.
Results
ANCOVA revealed no statistically significant differences in mandibular volume among the groups. SNA° and ANB° were significantly larger in the UCLA and BCLP groups than in the control group. SN-MP° was smallest in the UCLA group. Co-A in the UCLP group was shorter than in the UCLA and BCLP groups. Go-Gn was shortest in the UCLP and BCLP groups compared with the control group.
Conclusions
Three-dimensional evaluation of craniofacial morphology using CBCT can provide valuable information on malocclusion and other dentoskeletal problems among patients with CLP.
Keywords: Mandibular volume, Craniofacial morphology, Cleft lip and palate, Deciduous dentition, Cone beam computed tomography
INTRODUCTION
Cleft lip and palate (CLP) is the most prevalent craniofacial birth anomaly in humans and is closely associated with genetic and environmental factors.1,2 Patients born with these congenital malformations often require surgical intervention to correct problems associated with malocclusion, speech and respiratory difficulties, esthetics and psychosocial concerns.3,4 Patients with CLP usually have a flattened cranial base, midface deficiency with a retruded maxilla and elongated mandible, anterior and/or posterior crossbites, and increased vertical dimension.5 Yet there is some anatomical variation among patients with different types of cleft palate deformities such as unilateral cleft lip and alveolus (UCLA), unilateral cleft lip and palate (UCLP), and bilateral cleft lip and palate (BCLP). Therefore, it is crucial to understand the effect of CLP on bone growth, particularly in the maxilla and mandible, to select the most suitable treatment program.
Predicting mandibular growth can be challenging in growing children with orofacial clefts and may result in a tendency toward Class III malocclusion. It remains unclear whether mandibular growth influences both the mandibular shape (linear and angular variation) and volume during childhood growth. Two previous reports examined mandibular volume changes in patients with CLP6,7; however, these studies explored volumetric changes and differences in the mandibles of very young and adult patients presenting with various cleft types. Thus, the importance of mandibular volume remains incompletely understood. An evaluation of craniofacial morphology, including volumetric differences in the pre–early mixed dentition stage, is vital for the planning of initial orthodontic treatment.
Cone beam computed tomography (CBCT) has dramatically improved imaging within the dental field. CBCT provides accurate visualization of orthodontic problems, aiding in the planning and evaluation of orthodontic treatment. For example, CBCT can be used to identify root resorption caused by impacted teeth, supernumerary teeth, orofacial clefts, craniofacial syndromes, temporomandibular joint abnormalities, soft and hard tissue asymmetries, and nasopharyngeal airway abnormalities. It can also be used for cephalometric analyses and planning of orthognathic surgery.8–10 CBCT has recently been used in studies of craniofacial structure because of its short scanning time, high resolution, and lower radiation (four times) exposure compared with conventional CT.11–13
A previous study showed that adult patients with CLP have reduced maxillary volume and total volume (maxilla + maxillary sinus) compared to subjects without clefts.14 Such maxillary changes may cause compensatory facial growth of the mandible and lead to mandibular volumetric changes. It has been hypothesized that mandibular volume may vary according to the cleft type and degree of maxillary bone defect.6 However, no volumetric evaluations or comparisons among UCLA, UCLP, and BCLP in patients of preschool age have been performed. Few studies have compared differences in craniofacial morphology among patients with various cleft types during the deciduous dentition period.
The objective of this study was to examine the relationship between mandibular volume and craniofacial morphology in patients with various cleft types using CBCT and to compare these findings with noncleft control subjects during the deciduous dentition period.
MATERIALS AND METHODS
This study sample included 84 patients (mean age, 4.66 ± 0.47 years; 46 boys, 38 girls) who visited the Department of Orthodontics, Showa University Dental Hospital. Patient demographics and skeletal classification are shown in Tables 1 and 2, respectively. The patients were divided into four groups: UCLA group, UCLP group, BCLP group, and control group without cleft. Noncleft control subjects were classified into skeletal Classes I, II, or III based on the anteroposterior relationship between the maxillary and mandibular bases (ANB angle): Class I, −1° ≤ ANB < 4°; Class II, ANB ≥ 4°, and Class III, ANB < −1°.15,16 Patients were not categorized by side (left and right). All patients were nonsyndromic and had no systemic disease or history of previous orthodontic treatment. Written informed consent was obtained from the parents of all patients. This study was approved by the Ethics Committee at Showa University.
Table 1.
Patient Demographicsa
| Cleft Type |
Number of Patients (Male, Female) |
Age in Years (mean ± SD) |
| UCLA | 25 (8, 17) | 4.60 ± 0.40 |
| UCLP | 23 (13, 10) | 4.52 ± 0.39 |
| BCLP | 22 (16, 6) | 4.54 ± 0.37 |
| Control | 14 (9, 5) | 5.19 ± 0.52 |
BCLP indicates bilateral cleft lip and palate; control, without cleft; UCLA, unilateral cleft lip and alveolus, UCLP, unilateral cleft lip and palate.
Table 2.
Skeletal Classification of Noncleft Control Subjects
| Male |
Female |
Total |
|
| Skeletal Class I | 6 | 3 | 9 |
| Skeletal Class II | 2 | 1 | 3 |
| Skeletal Class III | 1 | 1 | 2 |
CBCT examination was performed for patients with and without clefts scheduled to undergo one of several procedures or evaluations: alveolar bone grafting, orthodontic treatment, or removal of impacted teeth; evaluation of skeletal Class III malocclusion; or evaluation of anterior open bite and lateral crossbite. All CBCT images were obtained using a KaVo 3D eXam (KaVo Dental, Biberach, Germany). The scanning conditions were set at 120 kV and 5 mA, with a voxel size of 0.4 mm, and a scanning time of 8.9 s. Patients were seated comfortably in a chair, with the chin rest adjusted to allow for a natural head position. Patients were then asked to bite down on the film but not to move or swallow during the scan. CBCT images were converted to DICOM (Digital Imaging and Communications in Medicine) format.
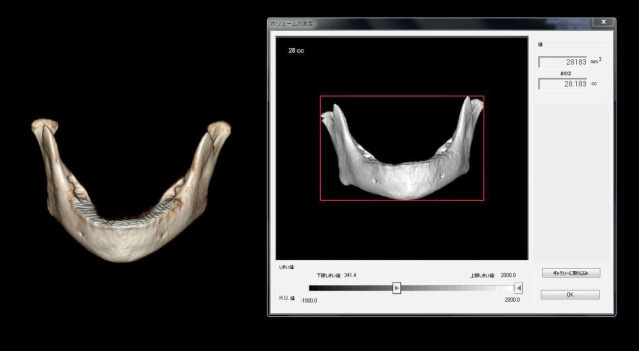
Data for the mandible were extracted from the CBCT image data and analyzed using dental software (Invivo 5; Anatomage, San Jose, CA). The mandibular volume was measured as reported by Deguchi et al.,17 extracting the crowns of the teeth but including the condyles. The outer border of the cortical bone and tooth crown was drawn freehand (Figure 1). The angular and linear measurements were performed as reported by Celikoglu et al.7 (Figure 2).
Figure 1.
Automated volume measurement of the mandible, including the condyle and roots of the mandibular teeth and excluding crowns, using Invivo 5 dental software.
Figure 2.

Angular and linear measurements performed using cone beam computed tomography images. The following cephalographic measurements were made: SNA°, SNB°, ANB°, SN-MP°, Co-A (mm), Go-Gn (mm), ANS-Me (mm), Co-Gn (mm), and Co-Go (mm).
Statistical analyses were performed using SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, NY). Shapiro-Wilk and Levene tests were used to confirm normality and equality of variances in the measurements. Analysis of covariance (ANCOVA) was performed with Bonferroni post hoc pairwise comparison for corrected means to compare the mandibular volume and craniofacial measurements among the groups and between individuals, with sex and age as covariates. Statistical significance was defined at P < .05.
A power analysis was performed using G*Power version 3.1.9.2 (Franz Faul, Universitat Kiel, Germany). The F test, using a fixed effects one-way analysis of variance, was used to calculate the effect size and power based on the mean difference and the recruited number of patients, with an alpha error level of .05. The F test was used to determine the result of the hypothesis test, in which the null hypothesis states that all means are equal and the alternative hypothesis, that at least one is different.
To assess operator error, 10 CBCT images were randomly selected, and volumes and craniofacial measurements were remeasured at 2-week intervals in separate sessions under identical conditions using Dahlberg's formula.18
RESULTS
The mandibular volume and craniofacial measurements obtained from the CBCT images in each group are summarized in Table 3. There was no statistically significant difference in the mean mandibular volume among the four groups using ANCOVA and controlling for age and sex (Table 4). However, statistically significant differences were found in the angular measurements for SNA°, ANB°, and SN-MP° and the linear measurements for Co-A and Go-Gn. Table 5 shows the effect size and power calculated using a significance level of α = .05 and sample size, average value, and standard deviation as parameters in each measurement. Table 6 shows the mean and statistically significant differences in the mandibular volume and craniofacial measurements among the four groups using Bonferroni post hoc pairwise comparison tests for the corrected means. There was no significant difference in the volumetric measurements among the groups. However, there were statistically significant differences in the mean SNA°, ANB°, and Co-A between the UCLA and UCLP groups. Likewise, statistically significant differences were found in SNA° between the UCLP and BCLP groups, in ANB° between the UCLA and control groups and between the BCLP and control groups, in SN-MP° between the UCLA and BCLP groups, and in Go-Gn between the BCLP and control groups.
Table 3.
Descriptive Statistics and Comparison of Measurements Among All Groupsa
| UCLA |
UCLP |
BCLP |
Control |
|
| Volume (mm3) | 24,507.04 ± 512.18 | 23,593.96 ± 706.89 | 22,967.36 ± 649.08 | 26,459.21 ± 795.53 |
| Angular measurements, ° | ||||
| SNA | 84.66 ± 0.70 | 79.69 ± 0.81 | 84.02 ± 0.81 | 81.36 ± 0.76 |
| SNB | 76.72 ± 0.59 | 76.48 ± 0.62 | 77.10 ± 0.62 | 79.30 ± 0.80 |
| ANB | 7.94 ± 0.59 | 3.21 ± 0.68 | 6.92 ± 0.74 | 2.05 ± 0.78 |
| SN-MP | 36.60 ± 0.71 | 39.59 ± 0.85 | 40.55 ± 0.89 | 39.69 ± 1.33 |
| Linear measurements, mm | ||||
| ANS-Me | 51.75 ± 0.72 | 52.52 ± 0.71 | 54.47 ± 0.65 | 54.43 ± 1.51 |
| Co-A | 68.81 ± 0.74 | 65.79 ± 0.65 | 68.57 ± 0.64 | 67.98 ± 1.12 |
| Go-Gn | 53.04 ± 0.59 | 52.44 ± 0.54 | 51.03 ± 0.66 | 55.71 ± 1.01 |
| Co-Go | 39.65 ± 0.41 | 39.23 ± 0.56 | 39.19 ± 0.65 | 40.15 ± 0.62 |
| Co-Gn | 81.72 ± 0.61 | 81.78 ± 0.79 | 81.57 ± 0.94 | 86.29 ± 1.52 |
Data are presented as mean ± standard error. BCLP indicates bilateral cleft lip and palate; control, without cleft; UCLA, unilateral cleft lip and alveolus; UCLP, unilateral cleft lip and palate.
Table 4.
ANCOVA Resultsa
| UCLA | UCLP | BCLP | Control | ||||
| Mean ± SE |
Mean ± SE |
Mean ± SE |
Mean ± SE |
F |
P |
Covariates |
|
| Volume, mm3 | 25,091.21 ± 536.29 | 23,987.51 ± 548.91 | 23,013.36 ± 569.89 | 24,697.00 ± 784.19 | 2.42 | .07 | Age*, Sex, Age × Sex |
| Angular measurements, ° | |||||||
| SNA | 84.49 ± 0.75 | 79.60 ± 0.77 | 84.04 ± 0.80 | 81.78 ± 1.10 | 8.84 | .00 | Age, Sex, Age × Sex |
| SNB | 76.72 ± 0.62 | 76.50 ± 0.63 | 77.13 ± 0.66 | 79.22 ± 0.91 | 2.10 | .11 | Age, Sex, Age × Sex |
| ANB | 7.77 ± 0.66 | 3.10 ± 0.68 | 6.91 ± 0.70 | 2.55 ± 0.97 | 12.96 | .00 | Age, Sex, Age × Sex |
| SN-MP | 36.68 ± 0.86 | 39.50 ± 0.88 | 40.38 ± 0.92 | 39.97 ± 1.26 | 3.37 | .02 | Age, Sex, Age × Sex |
| Linear measurements, mm | |||||||
| ANS-Me | 52.29 ± 0.77 | 52.54 ± 0.79 | 54.11 ± 0.82 | 54.00 ± 1.12 | 1.23 | .31 | Age, Sex, Age × Sex |
| Co-A | 69.38 ± 0.68 | 66.00 ± 0.69 | 68.42 ± 0.72 | 66.86 ± 0.99 | 4.79 | .00 | Age, Sex, Age × Sex |
| Go-Gn | 53.66 ± 0.57 | 52.70 ± 0.58 | 50.91 ± 0.60 | 54.37 ± 0.83 | 4.99 | .00 | Age*, Sex, Age × Sex |
| Co-Go | 40.03 ± 0.50 | 39.47 ± 0.51 | 39.21 ± 0.53 | 39.07 ± 0.73 | 0.57 | .63 | Age*, Sex, Age × Sex |
| Co-Gn | 82.68 ± 0.74 | 82.17 ± 0.76 | 81.35 ± 0.78 | 84.27 ± 1.08 | 1.56 | .21 | Age*, Sex, Age × Sex |
ANCOVA indicates analysis of covariance; control, without cleft; BCLP, bilateral cleft lip and palate; UCLA, unilateral cleft lip cleft and alveolus; UCLP, unilateral lip and palate. Means are the estimated marginal means after adjusting for covariates.
Significantly associated covariates (P < .05).
Table 5.
Effect Size and Power of Each Measurementa
| Measured Parameter |
ANCOVA Results (P Value) |
Calculated Effect Size |
Calculated Power, % |
| Volume | .07 | 0.29 | 57.62 |
| SNA | .00 | 0.48 | 96.12 |
| SNB | .11 | 0.29 | 58.31 |
| ANB | .00 | 0.56 | 99.39 |
| SN-MP | .02 | 0.34 | 72.10 |
| ANS-Me | .31 | 0.21 | 32.44 |
| Co-A | .00 | 0.38 | 82.60 |
| Go-Gn | .00 | 0.40 | 87.24 |
| Co-Go | .63 | 0.15 | 17.24 |
| Co-Gn | .21 | 0.25 | 44.22 |
ANCOVA indicates analysis of covariance.
Table 6.
Mean Differences and Statistical Significance of Mandibular Volume and Angular and the Bonferroni Post Hoc Pairwise Comparison Test for Corrected Meansa
| Group (a) |
Group (b) |
Mean Difference (a − b) |
P Value (Approximate) |
|
| Volume | UCLA | UCLP | 1103.70 | N.S. |
| BCLP | 2077.85 | N.S. | ||
| Control | 393.98 | N.S. | ||
| UCLP | BCLP | 974.15 | N.S. | |
| Control | 974.15 | N.S. | ||
| BCLP | Control | −1683.87 | N.S. | |
| SNA | UCLA | UCLP | 4.89 | .00* |
| BCLP | 0.44 | N.S. | ||
| Control | 2.71 | N.S. | ||
| UCLP | BCLP | −4.44 | .00* | |
| Control | −2.18 | N.S. | ||
| BCLP | Control | 2.27 | N.S. | |
| SNB | UCLA | UCLP | 0.22 | N.S. |
| BCLP | −0.41 | N.S. | ||
| Control | −2.50 | N.S. | ||
| UCLP | BCLP | −0.63 | N.S. | |
| Control | −2.72 | N.S. | ||
| BCLP | Control | −2.10 | N.S. | |
| ANB | UCLA | UCLP | 4.67 | .00* |
| BCLP | 0.85 | N.S. | ||
| Control | 5.21 | .00* | ||
| UCLP | BCLP | −3.82 | N.S. | |
| Control | 0.55 | N.S. | ||
| BCLP | Control | 4.36 | .00* | |
| SN-MP | UCLA | UCLP | −2.81 | N.S. |
| BCLP | −3.69 | .03* | ||
| Control | −3.29 | N.S. | ||
| UCLP | BCLP | 2.81 | N.S. | |
| Control | −0.48 | N.S. | ||
| BCLP | Control | 0.41 | N.S. | |
| Co-A | UCLA | UCLP | 3.38 | .01* |
| BCLP | 0.96 | N.S. | ||
| Control | 2.52 | N.S. | ||
| UCLP | BCLP | −2.42 | N.S. | |
| Control | −0.86 | N.S. | ||
| BCLP | Control | 1.57 | N.S. | |
| ANS-Me | UCLA | UCLP | −0.24 | N.S. |
| BCLP | −1.81 | N.S. | ||
| Control | −1.71 | N.S. | ||
| UCLP | BCLP | −1.57 | N.S. | |
| Control | −1.47 | N.S. | ||
| BCLP | Control | 0.10 | N.S. | |
| Go-Gn | UCLA | UCLP | 0.95 | N.S. |
| BCLP | 2.75 | N.S. | ||
| Control | −0.72 | N.S. | ||
| UCLP | BCLP | 1.80 | N.S. | |
| Control | −1.67 | N.S. | ||
| BCLP | Control | −3.46 | .01* | |
| Co-Go | UCLA | UCLP | 0.56 | N.S. |
| BCLP | 0.82 | N.S. | ||
| Control | 0.95 | N.S. | ||
| UCLP | BCLP | 0.26 | N.S. | |
| Control | 0.40 | N.S. | ||
| BCLP | Control | 0.13 | N.S. | |
| Co-Gn | UCLA | UCLP | 0.51 | N.S. |
| BCLP | 1.33 | N.S. | ||
| Control | −1.59 | N.S. | ||
| UCLP | BCLP | 0.82 | N.S. | |
| Control | −2.10 | N.S. | ||
| BCLP | Control | −2.92 | N.S. |
BCLP indicates bilateral cleft lip and palate; control, without cleft; N.S., not significant; UCLA, unilateral cleft lip and alveolus; UCLP, unilateral cleft lip and palate.
Statistical significance at the .05 level.
The random measurement errors ranged from 0.00% to 0.08% and 0.00% to 1.98% for the mandibular volume and craniofacial measurements, respectively, and were within the acceptable range.
DISCUSSION
This study examined mandibular volume and craniofacial measurements in patients with various types of clefts using CBCT and compared these measurements with noncleft control subjects who underwent CBCT for other reasons during the deciduous dentition period. Many recent studies used CBCT to evaluate mandibular volume in normal patients15,16,18,19 as well as in patients with CLP.6,7 Katayama et al.15 evaluated mandibular volume based on vertical and sagittal skeletal dimensions in adults and found significant correlations between mandibular volume and some parameters related to mandibular morphology. Deguchi et al.17 reported that adult female patients with skeletal Class III malocclusion tended to have a larger mandibular volume than those with skeletal Class II malocclusion. Nakawaki et al.16 found a significant difference in mandibular volume between hypodivergent (mandibular plane angle [MP] <23°) and hyperdivergent (MP >30°) adult subjects. Therefore, it was suspected that the mandibular volume might be affected by the presence of CLP and that it might vary according to cleft type. In the present study, craniofacial morphology and mandibular volume were assessed in 84 children during the pre–early mixed dentition stage. Patients were categorized according to cleft type using CBCT and compared against noncleft control subjects. Although the findings of the present study supported the hypothesis for differences in mandibular volume, these differences were not statistically significant.
Only two studies previously measured mandibular volume in patients with CLP. The age ranges of the patients in those studies (2.7–4.0 months and 10–23 years)6,7 differed from the ages of the children in the present study. Lo et al.6 demonstrated significant mandibular asymmetry and deformity in infants with UCLP, which affected the mandibular volume on the deformed side. They suggested that the cleft-related maxillary dysmorphology affected early mandibular development. Celikoglu et al.7 examined mandibular volume in children and young adult patients with UCLP and BCLP and compared measurements with those in normal subjects. In this older cohort, they found the mandibular volume to be smaller in patients with clefts compared with those without clefts, but the difference did not reach significance.
The mandible is a component of the facial buttresses, which consists of the upper transverse section (mandibular alveolar process and extension from its posterior border through the ramus to the posterior cortical border of the mandible) and the lower transverse section (inferior border of the mandible).20 Structurally, it is a cortical bone that thickens when subjected to a heavy load and undergoes a remodeling process to withstand mechanical forces in accordance with stress. Forces from the muscles of mastication can modify cortical bone mineralization, increasing bone density within the growing mandible.21 Therefore, the mandibular bone volume will continue to increase regardless of the presence of an alveolar and/or palatal cleft in the maxilla due to occlusal forces and a constant remodeling process. Taking these factors into account, the lack of a difference in the mandibular volume among the different cleft groups and the control group was a reasonable finding.
Most patients with CLP have malocclusion related to the dentofacial anomalies of that particular cleft type.22 In the present study, CBCT was used to evaluate the craniofacial morphology of patients with CLP through measurements of angles and linear parameters. There were statistically significant differences in some of the angular (SNA°, ANB°, and SN-MP°) and linear (Co-A and Go-Gn) measurements between the groups. The significant differences in SNA°, ANB°, and Co-A might be explained by the abnormal growth pattern of the maxilla in patients with CLP, which greatly affects the final shape of the maxilla.23 Co-A is a marker of growth deficiency caused by palatoplasty and scar formation on the palate in patients with UCLP.5 Most patients with CLP exhibit oral breathing due to nasal airway abnormalities. Oral breathing increases the lower face height and causes subsequent posterior rotation of the mandible, which can affect the position of the B point and, therefore, the ANB°.23,24 The present study showed a larger SNA° in the UCLA and BCLP groups than in the UCLP and control groups. In addition, the ANB° was larger in the UCLA and BCLP groups than in the UCLP and control groups. Co-A was shortest in the UCLP group. There was a significant difference in Go-Gn, indicating a shorter mandible in the cleft groups than in the control group. Patients with CLP are characterized by a shorter and retrognathic mandible; this difference is particularly noticeable in younger individuals because the mandible undergoes adaptation with age. A short and retrognathic mandible is due to a primary anomaly in infants born with a cleft of the secondary palate with or without a cleft of the primary palate.24
The SN-MP° measurement indicates the vertical dimensions of the mandible in relation to the cranial base. The SN-MP° was larger in the BCLP group than in the UCLA, UCLP, and control groups. Hermann et al.24 obtained similar findings and assumed that this was caused by primary factors, such as cleft malformation, or secondary factors, such as growth and functional adaptations. Increased inclination of the mandible in relation to the anterior cranial base is a form of vertical compensatory mandibular growth in response to the horizontal and vertical changes seen in the midfacial region in patients with UCLP and BCLP.24
According to the hospital's treatment protocol, alveolar bone grafting is performed for almost all patients with CLP at age 5 to 7 years. Early correction of the bone defect in the maxilla allows for stabilization and the provision of bone continuity to the maxillary arch. In addition, early alveolar bone grafting allows for orthodontic forces to be applied to the upper anterior teeth as soon as the teeth erupt, thus facilitating correction of the malalignment of the anterior teeth. Early alveolar bone grafting leads to more efficient application of orthopedic therapy in patients with clefts and concurrent maxillary hypoplasia.25 However, treatment outcomes are invariably affected by patient responses to surgical intervention and treatment, as well as the reference points chosen by different investigators for angular and linear measurements. There is still no consensus on how the mandible will be affected long term by surgical, orthopedic, and orthodontic treatment in patients with CLP. In addition, the growth patterns of craniofacial structures in patients with CLP are debatable. These factors could be considered limitations of the present study. Furthermore, the sample comprised 84 patients, which is relatively low. Although there was no significant difference in the mandibular volume between patients with and without CLP, the findings are still clinically noteworthy, as comparisons of craniofacial morphology with three-dimensional analysis tools, such as mandibular volume measurements over several generations, might be useful in predicting craniofacial growth in CLP. Evaluating mandibular volume as part of orthodontic examination provides useful information about mandibular growth with respect to craniofacial anatomy.
CONCLUSIONS
There was no significant difference in mandibular volume among patients with various cleft types and those without clefts.
Significant differences were found in some angular and linear measurements of the craniofacial complex among the cleft groups examined using CBCT analysis.
ACKNOWLEDGMENTS
The authors would like to thank all the participants of this study for their valuable time. This work was supported by JSPS KAKENHI (16K20654; Grant-in-Aid for Young Scientists [B]). The authors also thank Rebecca Jackson, PhD, and Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this article.
REFERENCES
- 1.Schutte BC, Murray JC. The many faces and factors of orofacial clefts. Hum Mol Genet. 1999;8:1853–1859. doi: 10.1093/hmg/8.10.1853. [DOI] [PubMed] [Google Scholar]
- 2.Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12:167–178. doi: 10.1038/nrg2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colbert SD, Green B, Brennan PA, Mercer N. Contemporary management of cleft lip and palate in the United Kingdom. Have we reached the turning point? Br J Oral Maxillofac Surg. 2015;53:594–598. doi: 10.1016/j.bjoms.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Warren DW, Drake AF, Davis JU. Nasal airway in breathing and speech. Cleft Palate Craniofac J. 1992;29:511–519. doi: 10.1597/1545-1569_1992_029_0511_naibas_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 5.Abuhijleh E, Aydemir H, Toygar-Memikoğlu U. Three-dimensional craniofacial morphology in unilateral cleft lip and palate. J Oral Sci. 2014;56:165–172. doi: 10.2334/josnusd.56.165. [DOI] [PubMed] [Google Scholar]
- 6.Lo LJ, Wong FH, Chen YR, Wong HF. Mandibular dysmorphology in patients with unilateral cleft lip and cleft palate. Chang Gung Med J. 2002;25:502–508. [PubMed] [Google Scholar]
- 7.Celikoglu M, Ucar FI, Buyuk SK, Celik S, Sekerci AE, Akin M. Evaluation of the mandibular volume and correlating variables in patients affected by unilateral and bilateral cleft lip and palate: a cone-beam computed tomography study. Clin Oral Invest. 2016;20:1741–1746. doi: 10.1007/s00784-015-1651-9. [DOI] [PubMed] [Google Scholar]
- 8.Machado GL. CBCT imaging—a boon to orthodontics. Saudi Dent J. 2015;27:12–21. doi: 10.1016/j.sdentj.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapila SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dentmaxillofac Radiol. 2015;44:20140282. doi: 10.1259/dmfr.20140282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buyuk SK, Celikoglu M, Benkli YA, Sekerci AE. Evaluation of the transverse craniofacial morphology of adolescents with repaired unilateral cleft lip and palate using cone-beam computed tomography. J Craniofac Surg. 2016;27:1870–1874. doi: 10.1097/SCS.0000000000003065. [DOI] [PubMed] [Google Scholar]
- 11.Maki K, Inou N, Takanishi A, Miller AJ. Computer-assisted simulations in orthodontic diagnosis and the application of a new cone beam X-ray computed tomography. Orthod Craniofac Res. 2003;6:95–101. doi: 10.1034/j.1600-0544.2003.241.x. [DOI] [PubMed] [Google Scholar]
- 12.Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:106–114. doi: 10.1016/j.tripleo.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 13.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol. 2004;33:83–86. doi: 10.1259/dmfr/28403350. [DOI] [PubMed] [Google Scholar]
- 14.Jiang C, Yin N, Zheng Y, Song T. Characteristics of maxillary morphology in unilateral cleft lip and palate patients compared to normal subjects and skeletal class III patients. J Craniofac Surg. 2015;26:e517–523. doi: 10.1097/SCS.0000000000002028. [DOI] [PubMed] [Google Scholar]
- 15.Katayama K, Yamaguchi T, Sugiura M, Haga S, Maki K. Evaluation of mandibular volume using cone-beam computed tomography and correlation with cephalometric values. Angle Orthod. 2014;84:337–342. doi: 10.2319/012913-87.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakawaki T, Yamaguchi T, Tomita D, et al. Evaluation of mandibular volume classified by vertical skeletal dimensions with cone-beam computed tomography. Angle Orthod. 2016;86:949–954. doi: 10.2319/103015-732.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deguchi T, Sr, Katashiba S, Inami T, Foong KW, Huak CY. Morphologic quantification of the maxilla and mandible with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:218–222. doi: 10.1016/j.ajodo.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 18.Dahlberg G. Statistical methods for medical and biological students. Br Med J. 1940;2:358–359. [Google Scholar]
- 19.Nair R, Deguchi T, Sr, Li X, Katashiba S, Chan YH. Quantitative analysis of maxilla and mandible in hyper- and hypodivergent skeletal class II pattern. Orthod Craniofac Res. 2009;12:9–13. doi: 10.1111/j.1601-6343.2008.01431.x. [DOI] [PubMed] [Google Scholar]
- 20.Winegar BA, Murillo H, Tantiwongkosi B. Spectrum of critical imaging findings in complex facial skeletal trauma. 2018 doi: 10.1148/rg.331125080. Available at: http://radiographics.rna.org Accessed December 24. [DOI] [PubMed]
- 21.Maki K, Miller A, Okano T, Shibasaki Y. Changes in cortical bone mineralization in the developing mandible: a three-dimensional quantitative computed tomography study. J Bone Miner Res. 2000;15:700–709. doi: 10.1359/jbmr.2000.15.4.700. [DOI] [PubMed] [Google Scholar]
- 22.Vettore MV, Sousa Campos AE. Malocclusion characteristics of patients with cleft lip and/or palate. Euro J Orthod. 2011;33:311–317. doi: 10.1093/ejo/cjq078. [DOI] [PubMed] [Google Scholar]
- 23.van den Dungen GM, Ongkosuwito EM, Aartman IH, Prahl-Andersen B. Craniofacial morphology of Dutch patients with bilateral cleft lip and palate and noncleft controls at the age of 15 years. Cleft Palate Craniofac J. 2008;45:661–666. doi: 10.1597/07-166.1. [DOI] [PubMed] [Google Scholar]
- 24.Hermann NV, Darvann TA, Jensen BL, Dahl E, Bolund S, Kreiborg S. Early craniofacial morphology and growth in children with bilateral complete cleft lip and palate. Cleft Palate Craniofac J. 2004;41:424–438. doi: 10.1597/03-056.1. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Jia H, Fu Z, Huang Y, Wang Z, Guo R. Dentoskeletal effects of facemask therapy in skeletal class III cleft patients with or without bone graft. Am J Orthod Dentofacial Orthop. 2018;153:542–549. doi: 10.1016/j.ajodo.2017.07.024. [DOI] [PubMed] [Google Scholar]