Abstract
Objectives
To investigate the hypothesis that there is difference in the treatment outcomes of milder skeletal Class III malocclusion between facemask and facemask in combination with a miniscrew in growing patients.
Materials and Methods
Patients were randomly divided into two groups. In one group, the patients were treated with facemask therapy (FM group: 12 males, eight females, average age: 10 years, 5 months ± 1 year, 8 months). In the other group, patients were treated with facemask therapy along with a miniscrew (FM+MS group: 12 males, seven females, average age: 11 years, 1 month ± 1 year, 3 months). A lingual arch with hooks was fixed to the maxillary arch in both groups and a protractive force of 500 g was applied from the facemask to the hooks. The patients were instructed to use the facemask for 12 hours per day. In the FM+MS group, a miniscrew was inserted into the palate and fixed to the lingual arch.
Results
Mobility and loosening of the miniscrew were not observed during treatment. Lateral cephalometric analysis showed that SNA, SN-ANS, and ANB values were significantly increased in the FM+MS group compared with those for the FM group (SNA, 1.1° SN-ANS, 1.3° ANB, 0.8°). Increase in proclination of maxillary incisors was significantly greater in the FM group than in the FM+MS group (U1-SN, 5.0°).
Conclusions
During treatment of milder skeletal Class III malocclusion, facemask therapy along with a miniscrew exhibits fewer negative side effects and delivers orthopedic forces more efficiently to the maxillary complex than facemask therapy alone.
Keywords: Class III malocclusion, Maxillary protraction, Facemask therapy, Miniscrew, Absolute anchorage
INTRODUCTION
Young patients with skeletal Class III malocclusions are treated primarily with facemask therapy to promote maxillary forward growth or to restrain mandibular growth.1,2 A major feature of this treatment is that orthopedic force is applied to the maxillary teeth as the anchorage through which the force is delivered to the maxillary complex. This results in stimulation of maxillary forward growth, restraint of mandibular growth, and posterior changes in the direction of mandibular growth and mandibular position.1,2 However, negative side effects, such as proclination of the maxillary incisors and mesial movement of the maxillary molars, often become problematic.3
Miniscrews have been reported as being effective anchorage in orthodontic treatment and they have been used as a practical application for improving various types of malocclusions that are difficult to cure with conventional orthodontic treatment.4–8 Because miniscrews are reportedly highly stable in the young jawbone,9 the application of orthopedic force directly to the jaw by using miniscrews to control its growth and development is expected to be successful.
Nienkemper et al.10,11 evaluated the effect of the Hybrid Hyrax bone-anchored rapid palatal expansion (RPE) appliance as a part of facemask treatment. Their report was useful for understanding the effect of this appliance; however, the effect of the miniscrew itself was not apparent. Ngan et al.12 reported that the Hybrid Hyrax RPE appliance significantly minimized the side effects encountered by tooth-borne RPE appliances during treatment with a facemask. However, the amount of maxillary protraction of the Hybrid Hyrax bone-anchored RPE appliance was almost the same as that observed with the tooth-borne RPE appliance.
The purpose of the present study was to compare the effect of treatment with facemask therapy and a miniscrew with that of facemask therapy alone in a randomized controlled study.
MATERIALS AND METHODS
Trial Design
This study was a single-center, prospective randomized clinical trial. No changes occurred during the trial.
Participants, Eligibility Criteria, and Settings
This study protocol was reviewed and approved by the institutional board of Tohoku University (approval number: 20-2). Forty-one young patients who visited the Tohoku University Hospital orthodontic clinic were recruited from April 2008 to March 2013 and satisfied the following criteria:
Skeletal Class III (ANB ≤ 2.5°), measured by inspection of initial lateral cephalograms.
Overjet ≥0, measured during initial cast analysis.
Undergoing circumpubertal phase of skeletal development (CVMS II–IV).
No congenital or systemic disease.
No skeletal asymmetry.
No missing teeth.
No temporomandibular joint disorder.
The cervical vertebral maturation stage (CVMS) was used for patient selection. CVMS II, III, and IV stages, which correspond with the circumpubertal growth period, were defined by lateral cephalometric radiographs.13 In this study, 28 patients were at CVMS II; 8 at CVMS III; and 3 at CVMS IV. The minimum age was 7 years, 5 months and the maximum, 13 years, 8 months. The patients and guardians provided informed consent for participation in this study. The CONSORT flowchart is shown in Figure 1. The final number of subjects was 39 (two refused to participate). No patients terminated participation in this study during treatment.
Figure 1.
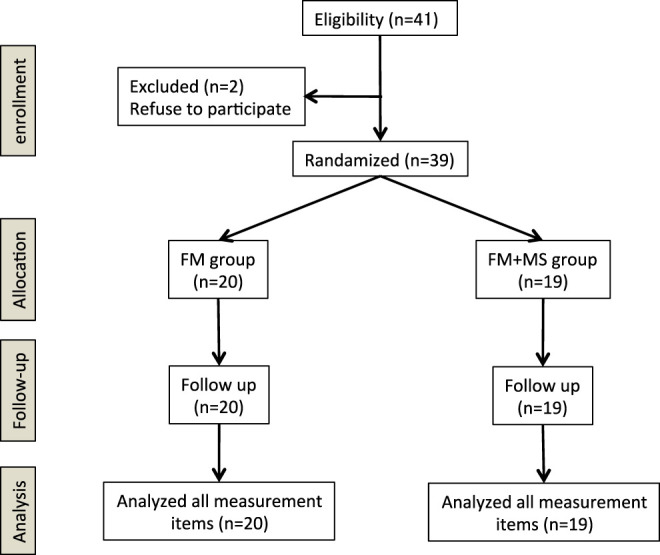
CONSORT flowchart.
Sample Size Calculation
Calculation of sample size was based on the evaluation of protocols for maxillary protraction previously performed by Cevidanes et al.14 They compared the treatment effects for maxillary protraction induced by bone-anchored maxillary protraction (BAMP) and facemask in association with rapid maxillary expansion (RME/FM). The BAMP protocol produced significantly greater (1.8 times greater) maxillary protraction than the RME/ FM therapy (BAMP; 5.2 ± 1.9 mm, RME/ FM; 2.9 ± 1.3 mm). In the current study, a 1.5 times increase was assumed in maxillary forward growth due to treatment with facemask therapy with a miniscrew, a test power of 80%, a significance level of 5%, and an effect size of 0.98. The calculation was carried out using the software G*power (Universität Düsseldorf, Germany). The recommended sample size was 18 patients for each group.
Randomization
Simple randomization was computer generated by use of a software program (R version 3.0.3, R Foundation for Statistical Computing, Vienna, Austria) in a 1:1 ratio by someone not involved in the study. The patients were randomly allocated into two groups using sequentially numbered, opaque, and sealed envelopes.
The FM group (10 years, 5 months ± 1 year, 8 months) consisted of 12 males and eight females and were treated with facemask therapy alone. The FM+MS group (11 years, 1 month ± 1 year, 3 months) included 12 males and seven females and were given facemask therapy with a miniscrew.
Interventions
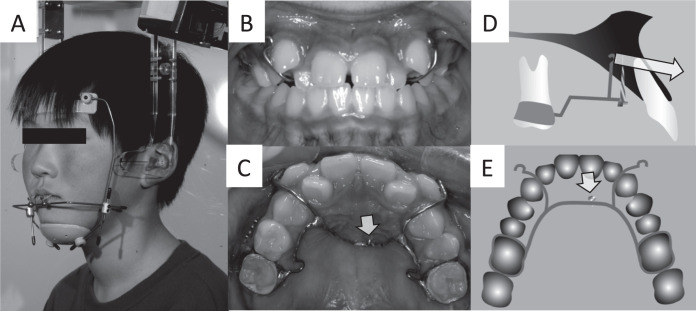
A lingual arch with soldered hooks was fixed to the maxillary arch in both groups, and a protractive force of 500 g (250 g per side) was applied from the facemask to the hooks by the use of elastics. Patients were instructed to use their facemask for 12 hours per day (Figures 2 and 3). The direction of the traction force was <3° from the occlusal plane (Figure 4).
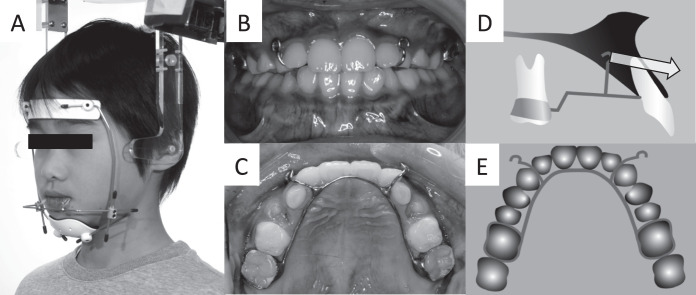
Figure 2.
Intra- and extraoral appliances of the FM group. (A) Facemask; (B) Lingual arch with soldered hooks (front view); (C) Lingual arch with soldered hooks (occlusal surface view); (D) lateral view (arrow shows direction of maxillary traction); (E) occlusal surface view. FM indicates facemask.
Figure 3.
Intra- and extraoral appliances of the FM+MS group. (A) facemask; (B) lingual arch with soldered hooks (front view); (C) lingual arch with soldered hooks (occlusal surface view; arrow shows a miniscrew); (D) lateral view (arrow shows direction of maxillary traction); (E) occlusal surface view (arrow shows a miniscrew).
Figure 4.
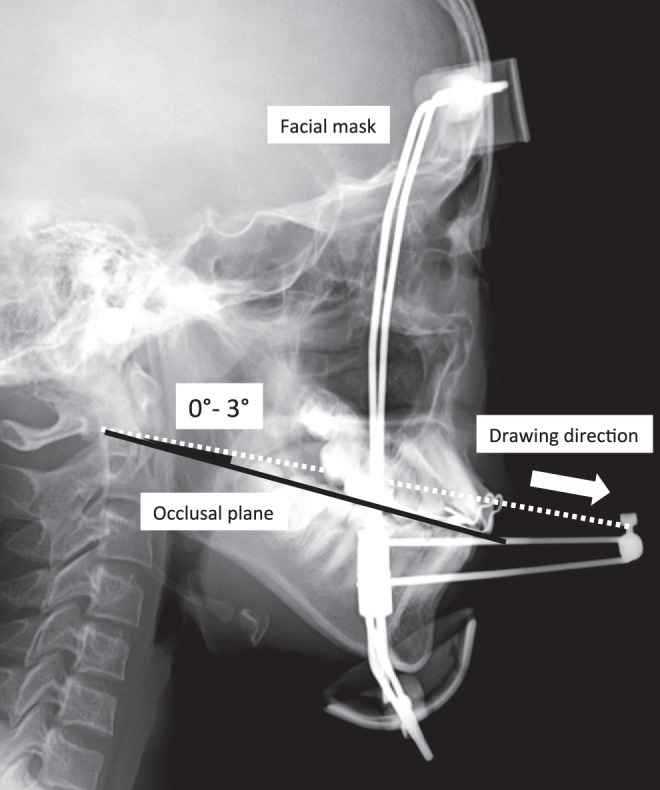
Direction of elastic force application.
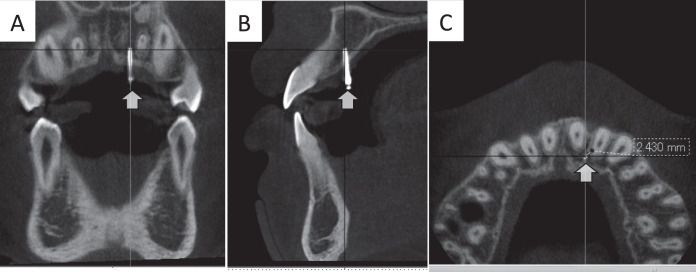
In the FM+MS group, a miniscrew (Absoanchor Dentos Inc., Taegu, Korea; diameter 1.4 mm, length 8 to 10 mm) was inserted in the anterior region of the palate (Figure 3). Multi-slice computed tomography scans were performed with a Somatom Definition (Siemens, Forchheim, Germany) with a 0.8-mm slice increment, 1.0-mm slice thickness, and a 512 × 512-mm matrix before miniscrew implantation.15 Miniscrews were inserted under local anesthesia into the anterior region of the palate, avoiding the roots of anterior teeth, incisive canal, and median palatine suture. A screw hole was made in the bone with a 1.0-mm round bur and a drill (ø 1.1 mm) operated at 500 rpm, and the miniscrew was placed via the self-tapping method. Cone-beam computed tomography scans (3D Accuitomo; J. Morita Co., Kyoto, Japan) were performed (80–90 mVp, 3.5–5 mA, scanning time 17.5 s, field of view 60 × 60 mm, and voxel size 0.125 mm) after miniscrew implantation (Figure 5).16 At 3–4 weeks after miniscrew implantation, mobility of the miniscrew was checked and the lingual arch was set. The lingual arch was attached to the miniscrew by tying with a ligature wire and fixing with resin. The treatment period was set at more than a half year. As a result, the treatment interval between initial observation (T1) and after facemask therapy (T2) was 1 year, 9 months ± 9.9 months in the FM+MS group and 1 year, 9 months ± 10.2 months in the FM group.
Figure 5.
Cone-beam computed tomography scans after miniscrew implantation. (A) coronal view; (B) Sagittal view; (C) Axial view. (For all panels, arrows show miniscrews.)
Outcomes
The main outcome of the study was determination of the effect of treatment in terms of skeletal and dentoalveolar change. A secondary outcome was that of the success rate for use of the miniscrew.
Cephalometric Analysis
All cephalograms at the time of T1 and T2 were traced by a single examiner. Cephalometric measures evaluated the vertical and anteroposterior position of the maxilla and mandible, pogonion, upper first molars, and incisors (Figure 6). All cephalograms were traced and measured two times within 1 week by the same examiner. Accidental errors in duplicate measurements were calculated from the equation: Sx = √ΣD2/2N, where Sx is the error of the measurement, D is the difference between duplicated measurements, and N is the number of double measurements.17 The error of linear measurement was 0.45 mm and that of angular measurement was 0.48°.
Figure 6.
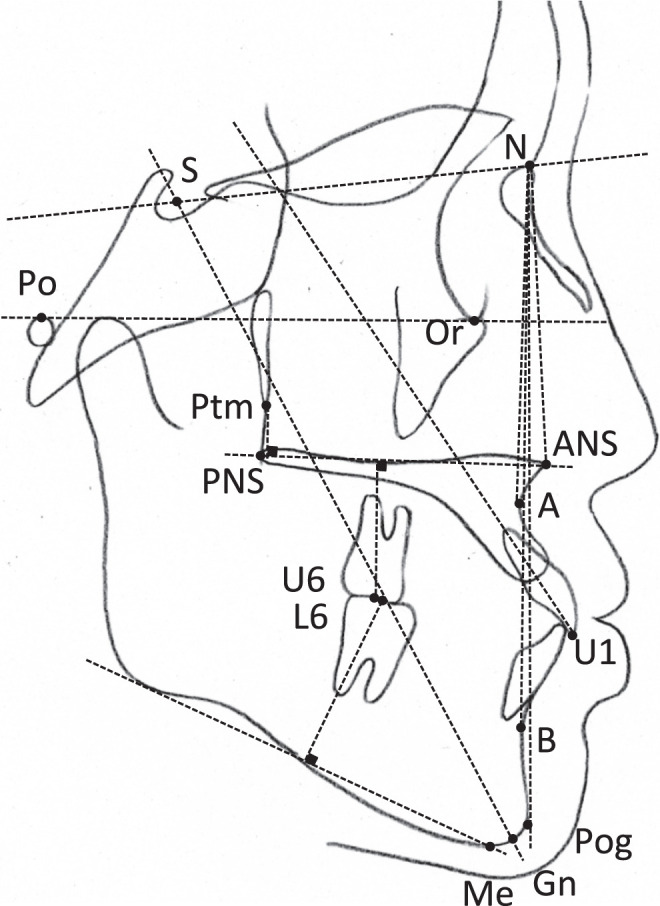
Landmarks and planes used in cephalometric analyses in this study.
Blinding
Blinding of both patient and operator to the intervention was impossible. However, the investigator who analyzed the cephalograms was blinded regarding the origin of the films and the group to which the individual subjects belonged. All data were labeled with numbers and sent to the statistician, who was also blinded to the patients' groups.
Statistical Analysis
All values were tested for normal distribution by use of the Shapiro-Wilk test. The significance of differences in age and the treatment period were tested by performing Welch's t tests since the respective data sets showed normal distributions. In the statistical analysis of the cephalometric variables, the data sets that showed a normal distribution were examined by using Welch's t tests whereas those not showing normality were examined by performing Mann-Whitney U-tests. Statistical significance was defined as *P < .05, **P < .01. All statistics were performed by using SPSS version 21 (IBM, Armonk, NY, USA).
RESULTS
There was no statistically significant difference between the FM+MS group and FM group in age (FM+MS group: 11 years, 1 month ± 1 year, 3 months; FM group: 10 years, 5 months ± 1 year, 8 months) or treatment period (FM+MS group: 1 year, 9 months ± 9.9 months; FM group: 1 year, 9 months ± 10.2 months). There were no statistically significant differences between the FM+MS group and FM group at T1 or between males and females for the cephalometric parameters analyzed (Table 1).
Table 1.
Cephalometric Values of the Patients at T1a
| Case No |
Sex |
Age |
SNA |
SNB |
ANB |
SN-ANS |
MP-SN |
U1-SN |
N-Me |
PTM-U6/NF |
U6/NF |
L6/MP |
Facial A |
Y Axis |
| FM group (T1) | ||||||||||||||
| 1 | M | 9Y4M | 78.6 | 78.9 | −0.3 | 81.5 | 35.6 | 112.6 | 120.6 | 14.6 | 19.8 | 28.9 | 88.5 | 60.6 |
| 2 | M | 11Y5M | 83.2 | 84.4 | −1.2 | 88.5 | 31.2 | 114.0 | 121.5 | 14.6 | 18.7 | 31.6 | 88.4 | 63.8 |
| 3 | M | 10Y7M | 82.9 | 81.7 | 1.2 | 85.0 | 34.8 | 115.5 | 109.8 | 17.2 | 17.4 | 27.3 | 90.0 | 56.7 |
| 4 | M | 13Y8M | 79.6 | 78.2 | 1.4 | 85.5 | 46.9 | 102.6 | 147.1 | 16.9 | 28.6 | 32.7 | 86.6 | 67.6 |
| 5 | M | 13Y0M | 79.0 | 78.5 | 0.5 | 84.5 | 37.7 | 109.4 | 133.5 | 20.0 | 24.4 | 35.6 | 87.3 | 62.7 |
| 6 | M | 7Y5M | 82.7 | 81.3 | 1.4 | 83.5 | 38.2 | 98.6 | 117.1 | 11.7 | 17.5 | 29.9 | 84.4 | 64.5 |
| 7 | M | 8Y11M | 75.8 | 73.5 | 2.3 | 80.0 | 49.0 | 108.0 | 124.6 | 15.5 | 21.3 | 27.8 | 85.5 | 64.5 |
| 8 | M | 10Y0M | 82.2 | 81.1 | 1.1 | 85.5 | 32.7 | 119.2 | 110.4 | 16.9 | 17.2 | 30.3 | 85.7 | 61.5 |
| 9 | M | 9Y1M | 73.2 | 73.6 | −0.4 | 78.0 | 40.8 | 95.1 | 118.7 | 13.8 | 19.6 | 29.2 | 88.4 | 59.1 |
| 10 | M | 9Y3M | 78.9 | 80.3 | −1.4 | 85.0 | 34.7 | 100.6 | 116.7 | 13.0 | 17.7 | 28.7 | 90.9 | 58.0 |
| 11 | M | 11Y11M | 80.7 | 82.9 | −2.2 | 86.0 | 34.6 | 122.5 | 119.5 | 11.7 | 19.3 | 24.9 | 89.7 | 61.2 |
| 12 | M | 9Y6M | 84.7 | 82.9 | 1.8 | 91.0 | 30.4 | 115.2 | 110.3 | 15.8 | 17.5 | 29.8 | 84.9 | 64.0 |
| 13 | F | 10Y1M | 84.0 | 83.3 | 0.7 | 87.0 | 35.1 | 112.9 | 105.6 | 19.7 | 17.2 | 26.7 | 89.7 | 57.6 |
| 14 | F | 13Y5M | 83.5 | 83.1 | 0.4 | 87.0 | 47.1 | 110.1 | 112.0 | 21.8 | 19.3 | 26.7 | 88.3 | 59.7 |
| 15 | F | 11Y7M | 83.5 | 82.1 | 1.4 | 86.5 | 27.6 | 117.2 | 121.1 | 19.5 | 22.6 | 32.8 | 89.2 | 60.2 |
| 16 | F | 10Y9M | 81.5 | 84.5 | −3.0 | 87.0 | 28.8 | 106.9 | 117.6 | 20.1 | 22.7 | 27.9 | 91.0 | 57.7 |
| 17 | F | 8Y4M | 81.7 | 82.4 | −0.7 | 84.0 | 35.7 | 111.6 | 108.1 | 11.1 | 9.1 | 27.0 | 86.9 | 62.4 |
| 18 | F | 9Y5M | 79.0 | 79.6 | −0.6 | 84.0 | 35.9 | 114.0 | 116.9 | 12.4 | 17.1 | 30.7 | 88.8 | 61.6 |
| 19 | F | 11Y3M | 80.7 | 80.1 | 0.6 | 84.0 | 41.6 | 112.0 | 127.8 | 17.2 | 20.6 | 28.6 | 88.8 | 60.4 |
| 20 | F | 9Y10M | 78.2 | 81.1 | −2.9 | 83.5 | 36.4 | 106.8 | 106.7 | 9.6 | 10.5 | 26.7 | 83.0 | 65.7 |
| Average (total) | 10Y5M | 80.7 | 80.7 | 0.0 | 84.9 | 36.7 | 110.2 | 118.3 | 15.7 | 18.9 | 29.2 | 87.8 | 61.5 | |
| SD (Total) | 1Y8M | 2.9 | 3.0 | 1.5 | 2.9 | 5.9 | 7.0 | 9.9 | 3.5 | 4.3 | 2.6 | 2.2 | 2.9 | |
| 95% CI | 9Y6M | 79.3 | 79.3 | −0.7 | 83.5 | 34.0 | 107.0 | 113.6 | 14.0 | 16.9 | 28.0 | 86.8 | 60.1 | |
| 11Y2M | 82.0 | 82.1 | 0.7 | 86.2 | 39.5 | 113.5 | 122.9 | 17.3 | 20.9 | 30.4 | 88.8 | 62.9 | ||
| Average (M) | 10Y4M | 80.1 | 79.8 | 0.4 | 84.5 | 37.2 | 109.4 | 120.8 | 15.1 | 19.9 | 29.7 | 87.5 | 62.0 | |
| SD (M) | 1Y10M | 3.3 | 3.5 | 1.4 | 3.5 | 5.8 | 8.6 | 10.6 | 2.4 | 3.4 | 2.7 | 2.1 | 3.1 | |
| 95% CI | 8Y11M | 78.0 | 77.6 | −0.6 | 82.3 | 33.5 | 104.0 | 114.0 | 13.6 | 17.7 | 28.0 | 86.2 | 60.0 | |
| 11Y5M | 82.2 | 82.0 | 1.3 | 86.7 | 40.9 | 114.9 | 128.0 | 16.7 | 22.1 | 31.5 | 88.9 | 64.1 | ||
| Average (F) | 10Y7M | 81.5 | 82.0 | −0.5 | 85.4 | 36.0 | 111.4 | 114.5 | 16.4 | 17.4 | 28.4 | 88.2 | 60.7 | |
| SD (F) | 1Y7M | 2.1 | 1.7 | 1.7 | 1.6 | 6.3 | 3.5 | 7.8 | 4.7 | 5.1 | 2.3 | 2.4 | 2.6 | |
| 95% CI | 9Y3M | 79.7 | 80.6 | −1.9 | 84.0 | 30.8 | 108.5 | 108.0 | 12.5 | 13.1 | 26.5 | 86.2 | 58.5 | |
| 11Y10M | 83.3 | 83.4 | 0.9 | 86.7 | 41.3 | 114.4 | 121.0 | 20.4 | 21.7 | 30.3 | 90.2 | 62.9 | ||
| FM+MS group (T1) | ||||||||||||||
| 21 | M | 12Y11M | 83.9 | 84.9 | −1.0 | 88.0 | 35.4 | 114.6 | 131.0 | 16.5 | 22.9 | 33.6 | 88.3 | 67.7 |
| 22 | M | 12Y0M | 75.4 | 75.1 | 0.3 | 77.0 | 41.1 | 108.2 | 121.3 | 19.6 | 18.6 | 30.5 | 88.4 | 59.2 |
| 23 | M | 12Y6M | 82.2 | 81.6 | 0.6 | 85.0 | 42.4 | 118.3 | 112.3 | 11.1 | 16.3 | 21.8 | 91.1 | 58.2 |
| 24 | M | 13Y0M | 84.9 | 84.1 | 0.8 | 89.0 | 32.0 | 118.6 | 112.5 | 22.3 | 19.7 | 28.5 | 91.6 | 56.1 |
| 25 | M | 10Y1M | 80.0 | 79.8 | 0.2 | 84.0 | 39.0 | 112.1 | 125.2 | 16.9 | 21.7 | 32.2 | 87.0 | 64.0 |
| 26 | M | 10Y10M | 80.1 | 80.9 | −0.8 | 85.5 | 34.5 | 112.1 | 115.0 | 17.3 | 18.7 | 30.9 | 87.3 | 60.4 |
| 27 | M | 10Y4M | 81.5 | 80.7 | 0.8 | 86.0 | 33.9 | 116.0 | 117.2 | 17.7 | 19.5 | 31.1 | 89.0 | 59.6 |
| 28 | M | 11Y8M | 81.4 | 79.6 | 1.8 | 84.5 | 33.5 | 114.6 | 128.0 | 16.8 | 22.2 | 33.2 | 84.3 | 65.0 |
| 29 | M | 10Y0M | 74.7 | 74.1 | 0.6 | 77.5 | 36.4 | 102.3 | 117.9 | 15.3 | 18.7 | 31.1 | 84.9 | 62.0 |
| 30 | M | 10Y2M | 80.0 | 79.0 | 1.0 | 85.0 | 38.9 | 111.9 | 121.0 | 11.9 | 20.0 | 29.9 | 87.8 | 61.2 |
| 31 | M | 10Y4M | 81.9 | 81.8 | 0.1 | 90.0 | 33.8 | 111.7 | 121.3 | 14.7 | 20.0 | 30.4 | 90.3 | 59.9 |
| 32 | M | 11Y8M | 87.7 | 87.3 | 0.4 | 90.5 | 31.3 | 121.7 | 112.6 | 21.2 | 16.7 | 30.2 | 90.2 | 61.1 |
| 33 | F | 10Y11M | 83.2 | 85.7 | −2.5 | 85.0 | 31.2 | 116.6 | 114.0 | 18.4 | 18.7 | 27.8 | 91.8 | 58.1 |
| 34 | F | 8Y10M | 75.5 | 73.6 | 1.9 | 80.5 | 39.5 | 110.6 | 113.1 | 13.6 | 18.6 | 26.5 | 87.3 | 58.6 |
| 35 | F | 12Y1M | 83.7 | 87.8 | −4.1 | 86.5 | 30.2 | 118.7 | 113.5 | 22.7 | 23.4 | 28.8 | 90.5 | 56.5 |
| 36 | F | 9Y1M | 86.0 | 84.1 | 1.9 | 89.0 | 34.3 | 113.6 | 115.6 | 13.9 | 20.3 | 26.5 | 91.6 | 59.3 |
| 37 | F | 10Y5M | 81.9 | 84.0 | −2.1 | 87.0 | 35.3 | 109.8 | 115.5 | 16.3 | 19.8 | 26.5 | 90.6 | 59.9 |
| 38 | F | 12Y1M | 84.5 | 84.9 | −0.4 | 88.0 | 32.6 | 115.0 | 117.0 | 16.2 | 22.5 | 28.4 | 90.7 | 58.9 |
| 39 | F | 11Y1M | 81.9 | 84.3 | −2.4 | 84.5 | 33.4 | 116.4 | 129.5 | 15.8 | 26.6 | 30.8 | 89.8 | 62.1 |
| Average (Total) | 11Y1M | 81.6 | 81.8 | −0.2 | 85.4 | 35.2 | 113.8 | 118.6 | 16.7 | 20.3 | 29.4 | 89.1 | 60.4 | |
| SD (Total) | 1Y3M | 3.5 | 4.2 | 1.6 | 3.7 | 3.5 | 4.4 | 6.0 | 3.2 | 2.5 | 2.8 | 2.2 | 2.9 | |
| 95% CI | 10Y5M | 79.9 | 79.7 | −0.9 | 83.6 | 33.5 | 111.7 | 115.7 | 15.2 | 19.1 | 28.1 | 88.0 | 59.0 | |
| 11Y7M | 83.3 | 83.8 | 0.6 | 87.2 | 36.9 | 116.0 | 121.5 | 18.3 | 21.5 | 30.8 | 90.1 | 61.8 | ||
| Average (M) | 11Y3M | 81.1 | 80.7 | 0.4 | 85.2 | 36.0 | 113.5 | 119.6 | 16.8 | 19.6 | 30.3 | 88.4 | 61.2 | |
| SD (M) | 1Y2M | 3.6 | 3.7 | 0.8 | 4.3 | 3.6 | 5.1 | 6.2 | 3.3 | 2.0 | 3.0 | 2.3 | 3.1 | |
| 95% CI | 10Y6M | 78.8 | 78.4 | −0.1 | 82.4 | 33.7 | 110.3 | 115.7 | 14.7 | 18.3 | 28.4 | 86.9 | 59.2 | |
| 12Y0M | 83.4 | 83.1 | 0.9 | 87.9 | 38.3 | 116.8 | 123.5 | 18.9 | 20.9 | 32.2 | 89.8 | 63.2 | ||
| Average (F) | 10Y9M | 82.4 | 83.5 | −1.1 | 85.8 | 33.8 | 114.4 | 116.9 | 16.7 | 21.4 | 27.9 | 90.3 | 59.1 | |
| SD (F) | 1Y6M | 3.4 | 4.6 | 2.3 | 2.8 | 3.1 | 3.3 | 5.7 | 3.1 | 2.9 | 1.6 | 1.5 | 1.7 | |
| 95% CI | 9Y5M | 79.3 | 79.3 | −3.2 | 83.2 | 31.0 | 111.4 | 111.6 | 13.8 | 18.7 | 26.4 | 88.9 | 57.5 | |
| 11Y10M | 85.5 | 87.7 | 1.0 | 88.4 | 36.6 | 117.4 | 122.2 | 19.6 | 24.1 | 29.4 | 91.7 | 60.6 | ||
Upper section: FM group; Lower section: FM+MS group.
Cephalometric values of the patients at T2 are shown in Table 2. There were significant increases during T1 to T2 in SNA, ANB, SN-ANS, N-Me, PTM-U6/NF, U6/NF, and L6/MP values in both groups (P < .01); however, no changes were found for SNB, MP-SN, Facial A, Y axis in either group. Therefore, both FM and FM+MS patients showed a significant increase in maxillary forward growth without mandibular forward growth. In addition, there were significant differences (P < .01) in U1 to SN in the FM group, but not in the FM+MS group.
Table 2.
Cephalometric Values of the Patients at T2a
| Case No |
Sex |
Age |
SNA |
SNB |
ANB |
SN-ANS |
MP-SN |
U1-SN |
N-Me |
PTM-U6/NF |
U6/NF |
L6/MP |
Facial A |
Y Axis |
| FM group (T2) | ||||||||||||||
| 1 | M | 12Y1M | 79.9 | 80.4 | −0.5 | 82.5 | 34.7 | 121.6 | 124.4 | 18.1 | 21.3 | 29.3 | 90.0 | 59.3 |
| 2 | M | 13Y4M | 85.5 | 84.4 | 1.1 | 90.5 | 29.0 | 116.6 | 127.2 | 17.7 | 21.5 | 34.3 | 89.8 | 63.6 |
| 3 | M | 11Y10M | 83.1 | 81.7 | 1.4 | 85.0 | 32.9 | 120.7 | 110.8 | 20.7 | 19.0 | 27.9 | 90.0 | 56.3 |
| 4 | M | 15Y9M | 79.2 | 77.1 | 2.1 | 85.5 | 47.8 | 104.3 | 152.4 | 21.2 | 29.6 | 36.9 | 86.7 | 68.0 |
| 5 | M | 15Y10M | 80.8 | 79.9 | 0.9 | 86.5 | 37.0 | 114.9 | 141.0 | 21.4 | 27.4 | 38.6 | 87.2 | 63.3 |
| 6 | M | 9Y6M | 84.9 | 81.4 | 3.5 | 86.5 | 39.9 | 113.2 | 122.8 | 15.7 | 19.7 | 31.6 | 81.9 | 67.4 |
| 7 | M | 9Y8M | 75.2 | 72.8 | 2.4 | 78.5 | 49.5 | 113.3 | 128.5 | 16.9 | 21.8 | 30.1 | 84.6 | 65.0 |
| 8 | M | 11Y1M | 83.3 | 82.0 | 1.3 | 87.5 | 32.6 | 126.2 | 112.1 | 17.6 | 17.8 | 30.6 | 86.2 | 61.1 |
| 9 | M | 9Y10M | 74.7 | 74.0 | 0.7 | 80.0 | 40.8 | 104.0 | 123.0 | 16.6 | 20.7 | 31.4 | 89.3 | 58.9 |
| 10 | M | 10Y4M | 81.9 | 81.8 | 0.1 | 89.0 | 33.8 | 111.7 | 121.3 | 14.7 | 20.0 | 30.4 | 90.3 | 59.9 |
| 11 | M | 12Y7M | 82.6 | 84.1 | −1.5 | 87.0 | 33.5 | 121.9 | 119.8 | 18.2 | 21.3 | 26.0 | 89.6 | 61.7 |
| 12 | M | 10Y10M | 85.4 | 83.1 | 2.3 | 92.5 | 29.9 | 114.3 | 113.3 | 17.9 | 20.0 | 29.8 | 85.2 | 64.0 |
| 13 | F | 11Y3M | 84.6 | 80.2 | 4.4 | 88.0 | 34.8 | 118.2 | 108.5 | 19.9 | 17.6 | 28.9 | 89.4 | 57.1 |
| 14 | F | 15Y5M | 83.6 | 81.8 | 1.8 | 87.5 | 45.8 | 108.6 | 117.5 | 23.6 | 19.9 | 29.5 | 89.0 | 61.1 |
| 15 | F | 13Y7M | 83.3 | 82.5 | 0.8 | 88.0 | 27.5 | 122.7 | 124.7 | 25.8 | 23.5 | 33.0 | 90.2 | 59.3 |
| 16 | F | 11Y11M | 82.5 | 83.6 | −1.1 | 87.0 | 31.6 | 114.9 | 121.0 | 22.8 | 23.7 | 27.9 | 89.5 | 59.7 |
| 17 | F | 10Y0M | 83.6 | 80.5 | 3.1 | 87.0 | 36.4 | 112.3 | 112.7 | 11.8 | 14.7 | 30.3 | 84.2 | 64.7 |
| 18 | F | 11Y11M | 81.0 | 79.8 | 1.2 | 84.0 | 35.7 | 111.6 | 120.5 | 17.7 | 20.5 | 32.2 | 89.4 | 60.2 |
| 19 | F | 12Y4M | 81.2 | 80.7 | 0.5 | 85.0 | 42.0 | 115.5 | 130.2 | 17.2 | 22.4 | 28.6 | 89.2 | 60.1 |
| 20 | F | 13Y10M | 79.5 | 80.9 | −1.4 | 84.0 | 37.1 | 109.5 | 119.9 | 15.7 | 19.4 | 30.6 | 86.9 | 64.8 |
| Average (Total) | 12Y2M | 81.8 | 80.6 | 1.2 | 86.1 | 36.6 | 114.8 | 122.6 | 18.6 | 21.1 | 30.9 | 87.9 | 61.8 | |
| SD (Total) | 2Y0M | 3.0 | 3.0 | 1.6 | 3.3 | 6.1 | 5.9 | 10.3 | 3.3 | 3.3 | 3.0 | 2.4 | 3.2 | |
| 95% CI | 11Y2M | 80.4 | 79.2 | 0.4 | 84.5 | 33.8 | 112.0 | 117.7 | 17.0 | 19.6 | 29.5 | 86.8 | 60.3 | |
| 13Y0M | 83.2 | 82.0 | 1.9 | 87.6 | 39.5 | 117.6 | 127.4 | 20.1 | 22.6 | 32.3 | 89.1 | 63.3 | ||
| Average (M) | 11Y11M | 81.4 | 80.2 | 1.2 | 85.9 | 36.8 | 115.2 | 124.7 | 18.1 | 21.7 | 31.4 | 87.6 | 62.4 | |
| SD (M) | 2Y2M | 3.6 | 3.7 | 1.4 | 4.1 | 6.6 | 6.8 | 12.0 | 2.1 | 3.4 | 3.6 | 2.7 | 3.5 | |
| 95% CI | 10Y6M | 79.1 | 77.9 | 0.3 | 83.3 | 32.6 | 110.9 | 117.1 | 16.7 | 19.5 | 29.1 | 85.8 | 60.1 | |
| 13Y3M | 83.7 | 82.6 | 2.0 | 88.5 | 41.0 | 119.5 | 132.3 | 19.4 | 23.8 | 33.7 | 89.3 | 64.6 | ||
| Average (F) | 12Y6M | 82.4 | 81.3 | 1.2 | 86.3 | 36.4 | 114.2 | 119.4 | 19.3 | 20.2 | 30.1 | 88.5 | 60.9 | |
| SD (F) | 1Y8M | 1.7 | 1.3 | 2.0 | 1.7 | 5.7 | 4.7 | 6.7 | 4.6 | 3.1 | 1.8 | 2.0 | 2.7 | |
| 95% CI | 11Y1M | 81.0 | 80.2 | −0.5 | 84.9 | 31.6 | 110.2 | 113.8 | 15.4 | 17.6 | 28.6 | 86.8 | 58.7 | |
| 13Y11M | 83.8 | 82.3 | 2.8 | 87.7 | 41.1 | 118.1 | 125.0 | 23.2 | 22.8 | 31.6 | 90.1 | 63.1 | ||
| FM+MS group (T2) | ||||||||||||||
| 21 | M | 13Y6M | 85.4 | 85.0 | 0.4 | 90.5 | 35.7 | 116.8 | 131.4 | 18.0 | 23.7 | 33.7 | 86.3 | 67.7 |
| 22 | M | 14Y5M | 77.6 | 73.1 | 4.5 | 79.0 | 42.0 | 110.1 | 131.2 | 20.0 | 22.1 | 32.0 | 86.9 | 61.0 |
| 23 | M | 14Y9M | 87.5 | 82.8 | 4.7 | 89.8 | 41.7 | 114.9 | 119.9 | 13.7 | 19.2 | 24.6 | 91.8 | 58.8 |
| 24 | M | 15Y10M | 86.0 | 84.8 | 1.2 | 90.0 | 30.1 | 115.9 | 121.4 | 27.1 | 21.4 | 34.4 | 92.0 | 56.1 |
| 25 | M | 13Y6M | 83.9 | 80.6 | 3.3 | 90.5 | 38.5 | 115.9 | 135.5 | 22.8 | 25.2 | 35.3 | 87.9 | 64.3 |
| 26 | M | 14Y0M | 83.9 | 82.2 | 1.7 | 90.0 | 34.1 | 110.8 | 123.7 | 21.2 | 22.0 | 32.7 | 89.2 | 60.2 |
| 27 | M | 11Y6M | 84.8 | 81.2 | 3.6 | 87.0 | 32.3 | 116.4 | 118.3 | 18.3 | 19.6 | 31.1 | 88.9 | 59.2 |
| 28 | M | 13Y7M | 82.2 | 79.6 | 2.6 | 85.0 | 34.4 | 109.1 | 132.8 | 20.8 | 21.8 | 38.4 | 85.2 | 64.7 |
| 29 | M | 10Y6M | 75.1 | 73.7 | 1.4 | 78.5 | 35.8 | 101.4 | 118.8 | 14.6 | 18.2 | 32.6 | 82.5 | 62.4 |
| 30 | M | 11Y8M | 82.3 | 79.5 | 2.8 | 88.0 | 38.6 | 115.7 | 127.5 | 15.2 | 22.2 | 30.3 | 88.6 | 60.7 |
| 31 | M | 11Y4M | 83.7 | 81.9 | 1.8 | 91.5 | 32.9 | 122.4 | 129.3 | 16.6 | 19.8 | 33.6 | 90.4 | 59.9 |
| 32 | M | 13Y7M | 90.2 | 88.4 | 1.8 | 93.0 | 29.5 | 119.9 | 122.1 | 24.5 | 18.8 | 32.8 | 89.2 | 60.0 |
| 33 | F | 13Y1M | 84.5 | 81.9 | 2.6 | 88.0 | 34.8 | 108.8 | 122.0 | 20.8 | 19.3 | 31.5 | 88.1 | 61.6 |
| 34 | F | 10Y4M | 78.1 | 73.7 | 4.4 | 82.5 | 39.8 | 114.8 | 115.4 | 15.0 | 19.5 | 27.2 | 87.5 | 59.0 |
| 35 | F | 14Y0M | 86.5 | 89.0 | −2.5 | 89.0 | 29.9 | 115.0 | 117.6 | 23.2 | 23.2 | 30.5 | 93.2 | 56.2 |
| 36 | F | 10Y11M | 86.9 | 83.3 | 3.6 | 89.5 | 35.7 | 112.0 | 121.6 | 16.6 | 21.2 | 28.5 | 91.1 | 59.8 |
| 37 | F | 11Y3M | 83.2 | 84.7 | −1.5 | 88.5 | 35.1 | 107.9 | 118.7 | 17.5 | 20.3 | 27.9 | 92.2 | 59.0 |
| 38 | F | 13Y2M | 85.6 | 84.1 | 1.5 | 89.5 | 32.8 | 115.3 | 118.3 | 18.0 | 22.4 | 28.7 | 91.0 | 58.8 |
| 39 | F | 12Y4M | 84.0 | 85.9 | −1.9 | 90.0 | 32.4 | 112.1 | 140.8 | 23.8 | 27.9 | 36.3 | 92.5 | 60.7 |
| Average (Total) | 12Y10M | 83.8 | 81.9 | 1.9 | 87.9 | 35.1 | 113.4 | 124.5 | 19.4 | 21.5 | 31.7 | 89.2 | 60.5 | |
| SD (Total) | 1Y7M | 3.6 | 4.5 | 2.1 | 4.0 | 3.7 | 4.8 | 7.1 | 3.8 | 2.4 | 3.4 | 2.8 | 2.8 | |
| 95% CI | 12Y0M | 82.0 | 79.7 | 0.9 | 86.0 | 33.3 | 111.1 | 121.1 | 17.5 | 20.3 | 30.1 | 87.8 | 59.2 | |
| 13Y7M | 85.5 | 84.0 | 2.9 | 89.8 | 36.8 | 115.7 | 128.0 | 21.2 | 22.6 | 33.3 | 90.5 | 61.9 | ||
| Average (M) | 13Y2M | 83.6 | 81.1 | 2.5 | 87.7 | 35.5 | 114.1 | 126.0 | 19.4 | 21.2 | 32.6 | 88.2 | 61.3 | |
| SD (M) | 1Y6M | 4.1 | 4.4 | 1.3 | 4.7 | 4.1 | 5.5 | 6.0 | 4.1 | 2.1 | 3.3 | 2.7 | 3.1 | |
| 95% CI | 12Y2M | 81.0 | 78.3 | 1.6 | 84.8 | 32.9 | 110.6 | 122.2 | 16.8 | 19.8 | 30.5 | 86.5 | 59.3 | |
| 14Y2M | 86.1 | 83.8 | 3.3 | 90.7 | 38.1 | 117.6 | 129.8 | 22.0 | 22.5 | 34.7 | 90.0 | 63.2 | ||
| Average (F) | 12Y2M | 84.1 | 83.2 | 0.9 | 88.1 | 34.4 | 112.3 | 122.1 | 19.3 | 22.0 | 30.1 | 90.8 | 59.3 | |
| SD (F) | 1Y4M | 3.0 | 4.8 | 2.8 | 2.6 | 3.1 | 3.0 | 8.6 | 3.4 | 3.0 | 3.1 | 2.2 | 1.7 | |
| 95% CI | 10Y10M | 81.4 | 78.8 | −1.7 | 85.8 | 31.5 | 109.5 | 114.1 | 16.1 | 19.2 | 27.2 | 88.8 | 57.7 | |
| 13Y5M | 86.9 | 87.6 | 3.5 | 90.5 | 37.2 | 115.1 | 130.0 | 22.4 | 24.7 | 33.0 | 92.8 | 60.9 | ||
Upper section: FM group; Lower section: FM+MS group.
Changes between T1 and T2 revealed significant differences between the two groups with respect to the effects of active treatment (Table 3). In particular, SNA change was significantly greater in the FM+MS group than in the FM group (FM+MS group: 2.2° ± 1.3°; FM group: 1.1° ± 1.0°; P < .01; Table 3). SN-ANS change was significantly greater in the FM+MS group than in the FM group (FM+MS group: 2.5° ± 1.7°; FM group: 1.2° ± 1.3°; P < .05; Table 3). ANB change was significantly greater in the FM+MS group compared with that for the FM group (FM+MS group: 2.0° ± 1.3°; FM group: 1.2° ± 1.2°; P < .05; Table 3). Also, the increase in proclination of the maxillary incisors was significantly greater in the FM group than in the FM+MS group (FM group: 4.6° ± 4.5°; FM+MS group: −0.4° ± 4.2°; P < .01; Table 3).
Table 3.
Changes After Treatment With Active Protraction (T2-T1)
| FM Group |
95% CI |
FM+MS Group |
95% CI |
Difference |
P Value |
Significance |
|||||
| Mean |
SD |
Mean |
SD |
||||||||
| T2-T1 (total)a | |||||||||||
| SNA, ° | 1.1 | 1.0 | 0.6 | 1.6 | 2.2 | 1.3 | 1.6 | 2.8 | 1.1 | .006 | ** |
| SNB, ° | 0.0 | 1.0 | −0.6 | 0.5 | 0.1 | 1.3 | −0.5 | 0.7 | 0.1 | .531 | NSd |
| ANB, ° | 1.2 | 1.2 | 0.6 | 1.7 | 2.0 | 1.3 | 1.4 | 2.7 | 0.8 | .034 | * |
| SN-ANS, ° | 1.2 | 1.3 | 0.6 | 1.8 | 2.5 | 1.7 | 1.7 | 3.3 | 1.3 | .021 | *d |
| MP-SN, ° | −0.1 | 1.2 | −0.7 | 0.4 | −0.1 | 1.3 | −0.7 | 0.5 | 0.0 | .976 | NS |
| U1-SN, ° | 4.6 | 4.5 | 2.5 | 6.6 | −0.4 | 4.2 | −2.4 | 1.6 | −5.0 | .001 | ** |
| N-Me, mm | 4.3 | 2.7 | 3.0 | 5.6 | 5.9 | 3.6 | 4.2 | 7.7 | 1.6 | .113 | NSd |
| PTM-U6/NF, mm | 2.9 | 2.0 | 2.0 | 3.9 | 2.6 | 2.1 | 1.6 | 3.6 | −0.3 | .652 | NS |
| U6/NF, mm | 2.2 | 2.0 | 1.2 | 3.1 | 1.2 | 1.4 | 0.5 | 1.9 | −1.0 | .089 | NSd |
| L6/MP, mm | 1.7 | 1.3 | 1.1 | 2.3 | 2.3 | 1.8 | 1.4 | 3.2 | 0.6 | .262 | NS |
| Facial A, ° | 0.1 | 1.4 | −0.5 | 0.8 | 0.0 | 1.6 | −0.7 | 0.9 | −0.1 | .771 | NS |
| Y axis, ° | 0.3 | 1.2 | −0.3 | 0.9 | 0.1 | 1.1 | −0.4 | 0.6 | −0.2 | .771 | NSd |
| T2-T1 (M)b | |||||||||||
| SNA, ° | 1.3 | 1.1 | 0.5 | 2.0 | 2.4 | 1.4 | 1.5 | 3.3 | 1.1 | .038 | * |
| SNB, ° | 0.4 | 0.9 | −0.1 | 1.0 | 0.3 | 0.9 | −0.2 | 0.9 | −0.1 | .795 | NSd |
| ANB, ° | 0.8 | 0.8 | 0.3 | 1.3 | 2.1 | 1.3 | 1.3 | 2.9 | 1.3 | .007 | ** |
| SN-ANS, ° | 1.4 | 1.5 | 0.5 | 2.3 | 2.6 | 1.8 | 1.4 | 3.7 | 1.2 | .105 | NS |
| MP-SN, ° | −0.4 | 1.1 | −1.1 | 0.3 | −0.5 | 0.9 | −1.1 | 0.0 | −0.1 | .784 | NS |
| U1-SN, ° | 5.8 | 4.7 | 2.8 | 8.8 | 0.6 | 4.3 | −2.1 | 3.3 | −5.2 | .009 | ** |
| N-Me, mm | 3.9 | 2.1 | 2.6 | 5.2 | 6.4 | 3.7 | 4.0 | 8.7 | 2.5 | .043 | *d |
| PTM-U6/NF, mm | 2.9 | 1.6 | 1.9 | 3.9 | 2.6 | 1.9 | 1.4 | 3.9 | −0.3 | .693 | NS |
| U6/NF, mm | 1.8 | 0.8 | 1.2 | 2.3 | 1.6 | 1.6 | 0.6 | 2.6 | −0.2 | .736 | NS |
| L6/MP, mm | 1.7 | 1.3 | 0.9 | 2.5 | 2.3 | 1.9 | 1.2 | 3.5 | 0.6 | .323 | NS |
| Facial A, ° | 0.0 | 1.1 | −0.6 | 0.7 | −0.1 | 1.3 | −1.0 | 0.7 | −0.1 | .764 | NS |
| Y axis, ° | 0.4 | 1.1 | −0.3 | 1.1 | 0.0 | 0.7 | −0.4 | 0.5 | −0.4 | .427 | NS |
| T2-T1 (F)c | |||||||||||
| SNA, ° | 0.9 | 0.8 | 0.2 | 1.6 | 1.7 | 0.8 | 1.0 | 2.4 | 0.8 | .062 | NS |
| SNB, ° | −0.8 | 1.3 | −1.8 | 0.3 | −0.3 | 1.8 | −1.9 | 1.4 | 0.5 | .530 | NS |
| ANB, ° | 1.7 | 1.6 | 0.4 | 3.0 | 2.0 | 1.5 | 0.6 | 3.4 | 0.3 | .706 | NS |
| SN-ANS, ° | 0.9 | 1.0 | 0.1 | 1.8 | 2.3 | 1.7 | 0.9 | 3.8 | 1.4 | .073 | NS |
| MP-SN, ° | 0.3 | 1.2 | −0.7 | 1.3 | 0.6 | 1.5 | −0.8 | 2.0 | 0.3 | .744 | NS |
| U1-SN, ° | 2.7 | 3.6 | −0.3 | 5.7 | −2.1 | 3.8 | −5.6 | 1.4 | −4.8 | .025 | * |
| N-Me, mm | 4.9 | 3.5 | 2.0 | 7.8 | 5.2 | 3.5 | 1.9 | 8.4 | 0.3 | .999 | NSd |
| PTM-U6/NF, mm | 2.9 | 2.7 | 0.7 | 5.1 | 2.6 | 2.5 | 0.3 | 4.9 | −0.3 | .999 | NSd |
| U6/NF, mm | 2.8 | 3.0 | 0.3 | 5.4 | 0.6 | 0.5 | 0.1 | 1.1 | −2.2 | .054 | NSd |
| L6/MP, mm | 1.7 | 1.6 | 0.4 | 3.0 | 2.2 | 1.8 | 0.5 | 3.9 | 0.5 | .616 | NS |
| Facial A, ° | 0.3 | 1.9 | −1.4 | 1.9 | 0.2 | 2.0 | −1.6 | 2.5 | −0.1 | .919 | NS |
| Y axis, ° | 0.2 | 1.5 | −1.0 | 1.4 | 0.2 | 1.6 | −1.2 | 1.7 | 0.0 | .970 | NS |
Upper section: total; Middle section: males; Lower section: females.
FM group (N = 20), FM+MS group (N = 19).
FM group (N = 12), FM+MS group (N = 12).
FM group (N = 8), FM+MS group (N = 7).
P < .05; **P < .01;d Mann-Whitney U-test.
In males (FM group: N = 12; FM+MS group: N = 12), increase in SNA was significantly greater in the FM+MS group compared with that for the FM group (FM+MS group: 2.4° ± 1.4°; FM group: 1.3° ± 1.1°; P < .05; Table 3). Increase in ANB was significantly greater in the FM+MS group than in the FM group (FM+MS group: 2.1° ± 1.3°; FM group: 0.8° ± 0.8°; P < .01; Table 3). The increase in proclination of the maxillary incisors in the FM group was significantly greater than that in the FM+MS group (FM group: 5.8° ± 4.7°; FM+MS group: 0.6° ± 4.3°; P < .01; Table 3). Additionally, the increase in anterior facial height (N-Me) was significantly greater in the FM+MS group than in the FM group (FM+MS group: 6.4 mm ± 3.7 mm; FM group: 3.9 mm ± 2.1 mm; P < .05; Table 3).
In females (FM group: N = 8; FM+MS group: N = 7), the increase in proclination of the maxillary incisors was significantly greater in the FM group than in the FM+MS group (FM group: 2.7° ± 3.6°; FM+MS group: −2.1° ± 3.8°; P < .05; Table 3).
Harms
No serious harm to the patients was observed during treatment. For three of the screws (three patients), the insertion direction was changed immediately after CBCT imaging because root proximity of the miniscrew to the root was confirmed in those individuals. There was no looseness or mobility of the miniscrews during treatment in the FM+MS group.
DISCUSSION
The present study clarified that facemask therapy with miniscrew anchorage exhibited fewer negative side effects and more efficiently delivered orthopedic forces to the maxillary complex. The amount of maxillary protraction was approximately twofold greater in the FM+MS group than in the FM group. Nienkemper et al.10,11 evaluated the effect of the Hybrid Hyrax RPE appliance on treatment with a facemask. They reported a significant improvement in skeletal sagittal values in the treatment group compared with the control group. Their report was useful for understanding the effect of the Hybrid Hyrax bone-anchored RPE appliance. However, the effect of the miniscrew itself was not apparent. Ngan et al.12 compared the effect of the Hybrid Hyrax bone-anchored RPE appliance with that of the tooth-borne RPE appliance on treatment with a facemask. They reported that the bone-anchored RPE appliance significantly minimized side effects such as forward movement of the maxillary molars, excessive proclination of the maxillary incisors, and an increase in lower face height encountered with the tooth-borne RPE appliance.12 However, the amount of maxillary protraction with the Hybrid Hyrax bone-anchored RPE appliance was almost the same as that obtained with the tooth-borne RPE appliance.12 The reason for this similarity might have been the difference in the intraoral appliance used (Ngan et al., RPE; this study, lingual arch), the treatment period (Ngan et al., 6 months; this study, 1 year, 9 months), the age at the start of the treatment (Ngan et al., 9.6 years; this study, 11.1 years), and the ratio of males and females (Ngan et al., eight males and 12 females; this study, 12 males and seven females).
In the present study, proclination of the maxillary anterior teeth at T1 in the FM+MS group, which was due to dental compensation, was reduced by the improvement of the maxillomandibular relationship at T2. In a previous report, Ito et al.18 inserted miniplates into the maxilla and mandible of beagle dogs and applied orthopedic force (2.0 N) by using coil springs. They reported that bone apposition occurred at the zygomaticomaxillary sutures and that the maxillary bone was positioned anteriorly. Additionally, maxillary anterior teeth showed lingual inclination due to dental compensation. The current study findings showed that, compared with orthopedic force alone, that force anchored by miniscrews had fewer negative side effects on the maxillary dentition although a greater maxillary orthopedic effect was exerted.
Recently, a new method consisting of the application of miniplates into the jaw, combined with the use of elastics to apply maxillary orthopedic force, has been reported to improve skeletal mandibular prognathism during the growth period.14,19,20 In a previous animal study, Ito et al.18 reported that posterior dislocation of the mandibular condyle occurred during the application of maxillary orthopedic force through the use of miniplates. Similarly, De Clerck et al.20 also reported backward displacement of the mandible and bone remodeling occurred in the anterior portion of the articular fossa, with bone resorption observed in the posterior wall of the articular fossa. In the present study, SNB, facial angle, MP-SN, and Y-axis angle remained virtually unchanged after treatment in both the FM and FM+MS groups. Therefore, although forward growth of the mandible was suppressed and the mandibular growth was shifted forward and downward, there was neither clockwise rotation of the mandible nor posterior displacement of it. These findings suggest that facemask therapy with a miniscrew caused less posterior displacement of the mandible compared with the use of miniplates and elastics.
Limitations
One limitation of this study was the lack of untreated mild skeletal Class III patients as a control. However, it would not be ethical for the control patients to go untreated, and to expose control subjects to radiation despite their need for immediate intervention. In addition, the absence of blinding for participants and operators were limitations of this study. However, though this factor is an inherent issue in this kind of study, it is very unlikely that this source of bias would have influenced the results.
Generalizability
The results of this study could be applied to similar patients with mild skeletal Class III malocclusions.
CONCLUSIONS
In the treatment of mild skeletal Class III malocclusion, facemask therapy with a miniscrew for anchorage may promote more maxillary forward growth than facemask therapy alone.
In addition, this new method resulted in fewer negative side effects, such as proclination of the maxillary incisors.
Miniscrews in the palate exhibited a high success rate in growing patients.
ACKNOWLEDGMENTS
This study did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.Roberts CA, Subtenly JD. An American Board of Orthodontics case report. Use of mask in treatment of maxillary skeletal retrusion. Am J Orthod Dentofacial Orthop. 1988;93:388–394. doi: 10.1016/0889-5406(88)90097-2. [DOI] [PubMed] [Google Scholar]
- 2.Nanda R. Biomechanical and clinical considerations of modified protraction headgear. Am J Orthod. 1980;78:125–139. doi: 10.1016/0002-9416(80)90055-x. [DOI] [PubMed] [Google Scholar]
- 3.Kama JD, Ozer T, Baran S. Orthodontic and orthopaedic changes associated with treatment in subjects with class III malocclusions. Eur J Orthod. 2006;28:496–502. doi: 10.1093/ejo/cjl011. [DOI] [PubMed] [Google Scholar]
- 4.Roberts WE, Engen DW, Schneider PM, Hohlt WF. Implant-anchored orthodontics for partially edentulous malocclusions in children and adults. Am J Orthod Dentofacial Orthop. 2004;126:302–304. doi: 10.1016/j.ajodo.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Kuroda S, Sugawara Y, Tamamura N, Takano-Yamamoto T. Anterior open bite with Temporomandibular disorder treated with titanium screw anchorage: evaluation of morphological and functional improvement. Am J Orthod Dentofacial Orthop. 2007;131:550–560. doi: 10.1016/j.ajodo.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Fukunaga T, Kuroda S, Kurosaka H, Takano-Yamamoto T. Skeletal anchorage for orthodontic correction of maxillary protrusion with adults periodontitis. Angle Orthod. 2006;76:148–155. doi: 10.1043/0003-3219(2006)076[0148:SAFOCO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Sugawara Y, Kuroda S, Tamamura N, Takano-Yamamoto T. Adult patient with mandibular protrusion and unstable occlusion treated with titanium screw anchorage. Am J Orthod Dentofacial Orthop. 2008;133:102–111. doi: 10.1016/j.ajodo.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 8.Takano-Yamamoto T, Kuroda S. Titanium screw anchorage for correction of canted occlusal plane in patients with facial asymmetry. Am J Orthod Dentofacial Orthop. 2007;132(2):237–242. doi: 10.1016/j.ajodo.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Motoyoshi M, Matsuoka M, Shimizu N. Application of orthodontic mini-implants in adolescents. Int J Oral Maxillofac Surg. 2007;36(8):695–699. doi: 10.1016/j.ijom.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Nienkemper M, Wilmes B, Pauls A, Drescher D. Maxillary protraction using a hybrid hyrax-facemask combination. Prog Orthod. 2013;14:5. doi: 10.1186/2196-1042-14-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nienkemper M, Wilmes B, Franchi L, Drescher D. Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: a controlled clinical study. Angle Orthod. 2015;85(5):764–770. doi: 10.2319/071614-497.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ngan P, Wilmes B, Drescher D, Martin C, Weaver B, Gunel E. Comparison of two maxillary protraction protocols: tooth-borne versus bone-anchored protraction facemask treatment. Prog Orthod. 2015;16:26. doi: 10.1186/s40510-015-0096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baccetti T, Franchi L, McNamara JA., Jr An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 2002;72(4):316–323. doi: 10.1043/0003-3219(2002)072<0316:AIVOTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Cevidanes L, Baccetti T, Franchi L, McNamara JA, Jr, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suzuki M, Deguchi T, Watanabe H, et al. Evaluation of optimal lengthand insertion torque for miniscrews. Am J Orthod Dentofacial Orthop. 2013;144:251–259. doi: 10.1016/j.ajodo.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe H, Deguchi T, Hasegawa M, Ito M, Kim S, Takano-Yamamoto T. Orthodontic miniscrew failure rate and root proximity, insertion angle, bone contact length, and bone density. Orthod Craniofac Res. 2013;16:44–55. doi: 10.1111/ocr.12003. [DOI] [PubMed] [Google Scholar]
- 17.Dahlberg G. Statistical methods for medical and biological students. BMJ. 1940;2:358. [Google Scholar]
- 18.Ito Y, Kawamoto T, Moriyama K. The orthopaedic effects of bone-anchored maxillary protraction in a beagle model. Eur J Orthod. 2014;36:632–640. doi: 10.1093/ejo/cjt083. [DOI] [PubMed] [Google Scholar]
- 19.De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67(10):2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Clerck H, Nguyen T, de Paula LK, Cevidanes L. Three-dimensional assessment of mandibular and glenoid fossa changes after bone-anchored Class III intermaxillary traction. Am J Orthod Dentofacial Orthop. 2012;142(1):25–31. doi: 10.1016/j.ajodo.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]