Abstract
Background:
Femoroacetabular impingement (FAI) is a common cause of hip pain and a known risk factor for hip osteoarthritis (OA) and total hip arthroplasty (THA) at a young age. Unfortunately, little is known about the specific factors associated with an increased risk of OA.
Purpose:
To (1) report the overall rate of symptomatic hip OA and/or THA in patients with FAI without surgical intervention and (2) identify radiographic features and patient characteristics associated with hip OA.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A geographic database was used to identify all patients with hip pain and radiographs between 2000 and 2016. Chart review was performed to identify patients with FAI. Patient medical records were reviewed to obtain demographic information, clinical history, physical examination findings, imaging details, and treatment details. Kaplan-Meier analysis was used to determine the rate of hip OA. Univariate and multivariate proportional hazard regression models were performed to determine risk factors for OA.
Results:
The study included 952 patients (649 female; 303 male; 1104 total hips) with FAI. The majority of hips had mixed type (n = 785; 71.1%), 211 (19.1%) had pincer type, and 108 (9.8%) had cam type. Mean age at time of presentation was 27.6 ± 8.7 years. Mean follow-up time was 24.7 ± 12.5 years. The rate of OA was 13.5%. THA was performed in 4% of patients. Male sex, body mass index (BMI) greater than 29, and increased age were risk factors for OA (male sex: hazard ratio [HR], 2.28; P < .01; BMI >.29: HR, 2.11; P < .01; per year of increased age: HR, 1.11; P < .01.). Smoking and diabetes mellitus were not significant risk factors. No radiographic morphological features were found to be significant risk factors for OA.
Conclusion:
At mean follow-up of 24.7 years, 14% of hips had symptomatic OA and 4% underwent THA. BMI greater than 29, male sex, and increased age at the time of presentation with hip pain were risk factors for hip OA. The cohort consisted of a large percentage of mixed-type FAI morphologies, and no specific radiographic risk factors for OA were identified.
Keywords: femoroacetabular impingement, hip pain, osteoarthritis, FAI
Femoroacetabular impingement (FAI) was originally described by Myers et al22 in 1999. It involves abnormal morphologic features of the femoral neck or acetabulum leading to atypical contact between the 2 surfaces.12,13 FAI is a well-established cause of hip pain in adolescent and young adult patients.25 Multiple studies have demonstrated that patients with FAI hip morphology are at an increased risk of developing hip osteoarthritis (OA), some even requiring total hip arthroplasty (THA) at a young age.10,13,29 FAI is a broad term and includes different types based on radiographic features including cam, pincer, and mixed types.6 Little is known about the relative risk development of OA in patients with FAI who have varying hip morphological characteristics. Additionally, it is unknown whether modifiable patient characteristics such as smoking status or increased body mass index (BMI) are risk factors for hip OA progression in patients with FAI.
Increased BMI is a known risk factor for hip OA in the general population,16,20 whereas smoking has been protective against OA in some studies.2 These factors have not yet been evaluated in patients with FAI. The radiographic features of FAI are modifiable only by surgery such as hip arthroscopy or surgical hip dislocation, and to date it has not been demonstrated that these procedures modify the natural progression to OA. Multiple studies have established that cam and pincer deformities increase the risk of hip OA progression.1,5,15,27,29,30 Hartofilakidis et al15 reported on a cohort of 96 patients with FAI and found that 17.7% of patients developed OA and 12.5% underwent THA at mean follow-up of 18.5 years. This retrospective study15 involved a small cohort and found no difference in the development of OA between patients with cam-, pincer-, and mixed-type morphologies. Wyles et al29 identified 74 patients with FAI radiographic features and found that 18% of patients underwent THA at minimum 10-year follow-up. Their study cohort included only patients who had undergone a contralateral THA, which is a known independent risk factor for development of hip OA.29 Those investigators were also limited by only being able to analyze anteroposterior pelvic radiographs.
A large cohort study analyzing risk factors for hip OA in patients with FAI without previous contralateral THA would be an important addition to the literature. In addition, identification of modifiable risk factors for development of hip OA could be beneficial when counseling patients on their risk of developing hip OA. Therefore, the purposes of this study were (1) to report the overall rate of symptomatic hip OA and/or THA in patients with FAI without surgical intervention and (2) to identify radiographic features and patient characteristics associated with hip OA.
METHODS
Study Population and Design
A geographic population-based cohort study was performed with the Rochester Epidemiology Project (REP) database in Olmsted County, Minnesota, USA, which had a population of 144,260 in 2010. In brief, the REP is a medical record linkage system that provides access to the complete medical records for all residents of Olmsted County, regardless of the medical facility in which the care was delivered.24 After we obtained institutional review board approval (17–004959, 030-OMC-17), the REP was used to identify all patients in a geographic area who presented to a physician with an International Classification of Diseases, Ninth Revision, or Tenth Revision (ICD-10), diagnostic code of hip pain, hip impingement, or hip joint disorders between January 2000 and December 2016 (Table 1). Only patients between 14 and 50 years of age were included. The upper age limit of 50 years was chosen to remain consistent with, or slightly younger than, previous studies on FAI.15,29 The database contained complete diagnostic and procedural information from all applicable medical centers through December 1, 2019, to ensure sufficient follow-up to determine the natural history after FAI diagnosis. Clinical notes, radiographic images, and operative notes related to the injury were manually reviewed in detail. Patients with a history of avascular necrosis, neuromuscular disorder, trochanteric bursitis, hip fracture, pelvic fracture, previous hip surgery, and/or hip dislocation were excluded. These patients were excluded as part of the original database search. All patient charts were then reviewed to verify exclusion of these patients. Patients were included only if their symptoms, as documented in the chart, were consistent with FAI as defined by the Warwick Agreement: “The primary symptom of FAI syndrome is motion-related or position-related pain in the hip or groin. Pain may also be felt in the back, buttock or thigh.”14 Patients with hip OA were included if they had radiographic findings consistent with FAI. Radiographs were obtained as part of the routine clinical evaluation as determined necessary by the evaluating physician. Radiographs were not obtained strictly for the purpose of this study. All patients had radiographs evaluating for FAI at initial presentation to their physician with hip pain. Subsequent radiographs were obtained at the discretion of the evaluating physician. If patients were not symptomatic enough for future radiographs, it was assumed that they did not develop symptomatic OA.
TABLE 1.
Database Search Codesa
| Code | Code Description |
|---|---|
| ICD-9 | |
| 719.45 | Hip pain |
| 719.85 | Femoroacetabular impingement |
| 719.95 | Unspecified disorder of joint; pelvic region and thigh |
| ICD-10 | |
| M25.559 | Pain in unspecified hip |
| M25.551 | Pain in hip |
| M25.859 | Other specified joint disorders, unspecified hip |
| M25.852 | Other specified joint disorders, hip |
ICD-9/-10, International Classification of Diseases, Ninth Revision/Tenth Revision.
All patients underwent anteroposterior and lateral view (cross-table, frog-leg, or 45° Dunn) hip radiographs upon initial assessment by a physician for hip pain. Only 1 of the lateral views (cross-table, frog-leg, or 45° Dunn) was required for inclusion. All radiographic reviews were performed by attending or senior resident–level orthopaedic surgeons (H.P.M., J.Z.). The first 100 radiographic reviews were evaluated by each author (H.P.M., J.Z.) to verify agreement on the radiographic measurements. Radiographic parameters were standardized based on the parameters outlined by Clohisy et al.9 If radiographs were not compliant with these parameters, they were not used for measurement. The radiographic findings considered consistent with FAI are shown in Table 2.
TABLE 2.
Radiographic Findings Associated With Each FAI Typea
| FAI Type | Radiographic Findings |
|---|---|
| Cam type | Typical pistol grip deformity and/or Alpha angle >55° 3,7 |
| Pincer type | Crossover sign7,9,19,26
and/or Coxa profunda or protrusio acetabuli3,9,19,26,29 and/or Lateral center-edge angle >40° 19,26,29 and/or Tönnis angle <0° 9 |
| Mixed type | Both cam and pincer type features |
FAI, femoroacetabular impingement.
A cam deformity was defined as an alpha angle greater than 55°, as this cutoff has been used in previous studies.3,7 Frank et al11 concluded that an alpha angle greater than 50° to 55° defined a cam deformity. The higher of these was chosen in this study to increase specificity.
FAI syndrome is diagnosed according to the 2016 Warwick Agreement based on the presence of a triad of symptoms, clinical signs, and imaging findings.14 Due to the retrospective nature of this study, we were unable to confirm examination findings consistent with FAI in all cases. Physician understanding of FAI has increased since first described in 1999,22 but knowledge and documentation of physical examination techniques were limited in the early years of this study.23 In this study, patients were included only if they had symptoms and diagnostic imaging consistent with FAI as defined by the Warwick Agreement.14 Once it was confirmed that the symptoms and radiographic findings were consistent with FAI, patients were followed by chart and/or radiographic review to determine whether they developed symptomatic hip OA. Patients who underwent hip arthroscopy or hip preservation procedures were excluded. Subsequent physician visits were typically on an as-needed basis. Symptomatic hip OA was defined as hip symptoms significant enough for the patient to seek treatment from a physician and a Tönnis grade of 1 or higher on hip radiograph.18 Tönnis grade was determined on any radiographic image, and axial imaging was not used for Tönnis grade assessment. Symptoms included pain and/or hip clicking, catching, locking, stiffness, restricted range of motion, or giving way.14 The patient determined whether a physician visit was desired, as routine follow-up was not obtained in all cases. Patient factors such as sex, BMI, smoking status, antiinflammatory use, diabetes, previous intra-articular injections, sports participation, physical examination findings, physical therapy participation, and eventual surgery were recorded during the chart review. For all patients, time from hip pain to follow-up was calculated. Time from initial presentation to development of hip OA was recorded.
Statistical Analysis
Patient comorbidities, demographics, and radiographic measurements and their associated standard deviations and percentages of the population were reported for descriptive statistical purposes. Time to event was calculated as date of event or last follow-up date minus date of hip pain onset. Kaplan-Meier analysis was used to determine the rate of OA development. Kaplan-Meier analyses were then subanalyzed by sex through use of a Wilcoxon test. Data were censored by OA event.
Proportional hazard regressions were used to determine risk factors associated with OA after hip FAI. To determine the effect of comorbidity on OA development, comorbidity variables (sex, BMI >29, smoking status, and diabetes) were analyzed with a multivariate hazard regression model. After adjustment for comorbidities, univariate hazard models were performed on individual radiographic and procedural variables to determine individual risk factors for OA progression. Variables included in the analysis were as follows: cam morphology, pincer morphology, mixed morphology, lateral edge angle 40° or greater, Tönnis angle less than 0°, alpha angle greater than 55°, crossover sign, posterior wall sign, ischial spin sign, acetabular profunda, acetabular protrusio, os acetabuli, and previous injection. All variables were nominal, and risk factors were presented as positive criteria for the variable.
A multivariate proportional hazard regression was performed on all variables to determine risk factors for OA. Due to the size of the total cohort and those who had OA, up to 18 different variables were acceptable for predictive statistical analysis. Kaplan-Meier analyses were then performed on the significant risk factors associated with OA. Alpha values were set to < .05. Jmp Pro 14 (SAS Institute) was used for all analyses.
RESULTS
The overall prevalence of patients with radiographic cam and/or pincer morphology was 61% (1160 patients; 376 male, 784 female; 1361 total hips) of the 1893 patients treated for hip pain. Patients who had undergone hip arthroscopy or hip preservation procedures were excluded (n = 208). Therefore, the final cohort for this study consisted of 952 patients (303 male; 649 female; 1104 total hips). Mean follow-up time was 24.7 ± 12.5 years. Patient characteristics are shown in Table 3 and radiographic findings are shown in Table 4.
TABLE 3.
Patient Characteristicsa
| Total Group (n = 1104)b | Patients With Osteoarthritis (n = 149)b | |
|---|---|---|
| Age at onset of pain, y | 27.6 ± 8.7 | 33.0 ± 5.6 |
| Contralateral diagnosis | 332 (30.1) | 78 (52.3) |
| Sex | ||
| Male | 341 (30.9) | 66 (44.3) |
| Female | 763 (69.1) | 83 (55.7) |
| Laterality | ||
| Left | 523 (47.4) | 74 (49.7) |
| Right | 581 (52.6) | 75 (50.3) |
| Comorbidities | ||
| Body mass index | 28.6 ± 4.8 | 31.2 ± 4.1 |
| Smoker | 252 (22.8) | 39 (26.2) |
| Diabetes | 84 (7.6) | 27 (18.1) |
| Intra-articular steroid injection | 200 (18.1) | 57 (38.3) |
| Follow-up time, y | 24.7 ± 12.5 | 28.0 ± 15.7 |
Values are presented as mean ± SD or n (% of cohort).
n, number of hips.
TABLE 4.
Radiographic Findingsa
| Total Group (n = 1104)b | Patients With Osteoarthritis (n = 149)b | |
|---|---|---|
| Morphology type | ||
| Pincer | 211 (19.1) | 16 (10.7) |
| Cam | 108 (9.8) | 24 (16.1) |
| Mixed | 785 (71.1) | 109 (73.2) |
| Measurements | ||
| Tonnis angle, deg | 4.4 ± 6.3 | 5.2 ± 7.8 |
| Alpha angle, deg | 61.7 ± 14.5 | 67 ± 13.3 |
| Lateral center-edge angle, deg | 32.3 ± 7.0 | 32.5 ± 9.2 |
| Positive signs | ||
| Crossover sign | 854 (77.4) | 97 (65.1) |
| Posterior wall sign | 650 (58.9) | 88 (59.1) |
| Ischial spine sign | 629 (57.0) | 82 (55.0) |
| Acetabular profunda | 683 (61.9) | 75 (50.3) |
| Acetabular protrusion | 6 (0.5) | 2 (1.3) |
| Os acetabuli | 141 (12.8) | 22 (14.8) |
Values are presented as mean ± SD or n (% of cohort).
n, number of hips.
Rate of Hip Osteoarthritis
Of the 1104 FAI hips analyzed, 149 patients (13.5%) had OA. We noted that 45 of the hips with OA (4% of the total cohort) went on to THA. OA median survival time after FAI was 16.6 ± 0.2 years (Figure 1). Male patients had a statistically lower mean survival time to OA than female patients (11.1 ± 0.3 vs 17.2 ± 0.2 years; P < .01). Within the OA group, 76.5% (114 hips) were Tönnis grade 1, 20.8% (31 hips) were grade 2, and 2.7% (4 hips) were grade 3 at the time of follow-up.
Figure 1.
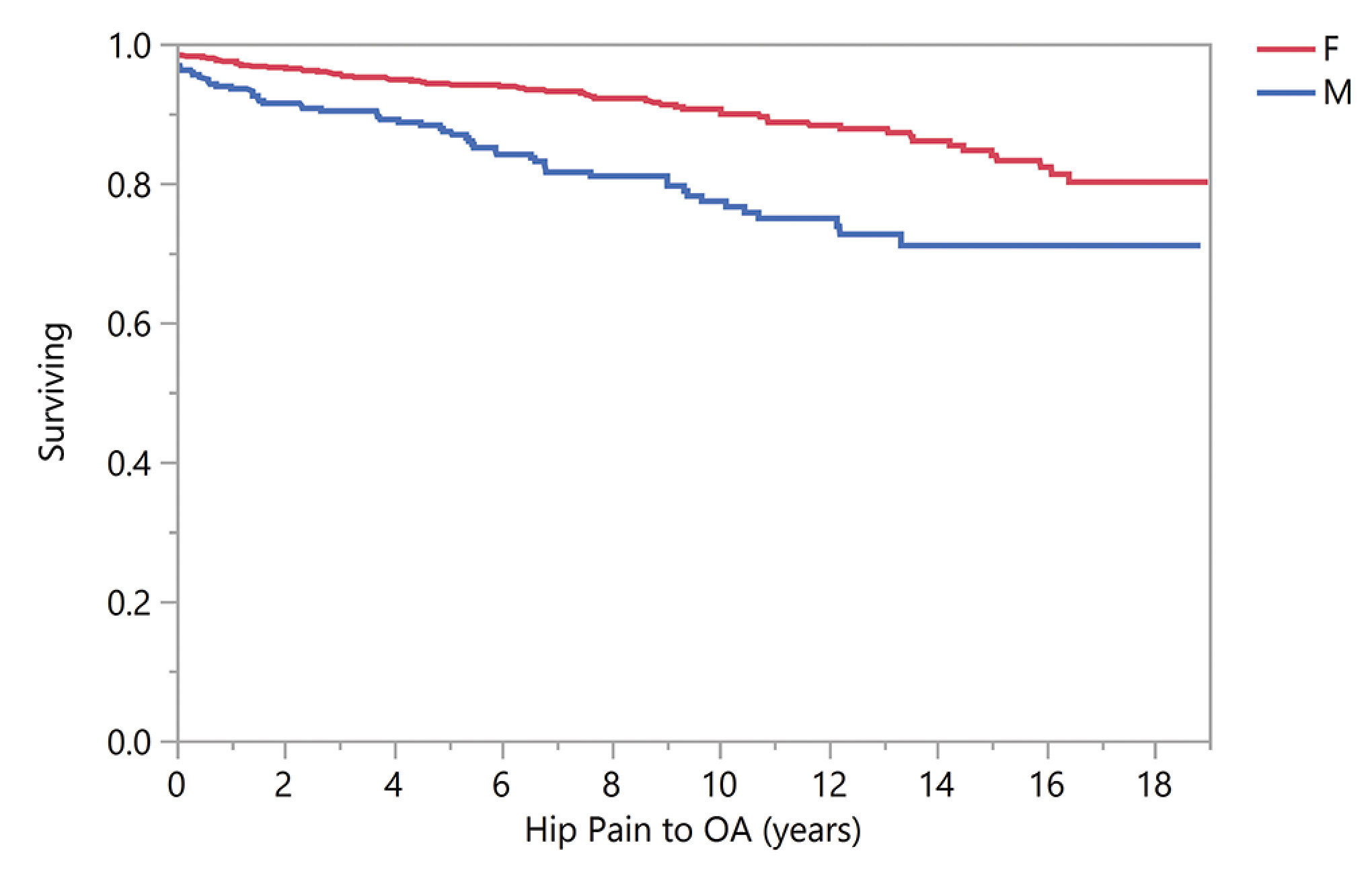
Kaplan-Meier survival analysis for osteoarthritis (OA) by sex (female [F] is top line, male [M] is bottom line).
Risk Factors for Hip Osteoarthritis
Nonradiographic factors associated with OA are noted in Table 5. Male sex, BMI greater than 29 at the time of presentation, and increased age at the time of presentation with hip pain had a significantly higher risk of OA (male sex: hazard ratio [HR], 2.28; 95% CI, 1.60–3.23; P < .01; BMI >29: HR, 2.11; 95% CI, 1.47–3.02; P < .01; per year of increased age: HR, 1.11; 95% CI, 1.08–1.15; P < .01). Smoking and diabetes were not statistically significant (P = .14 and P = .06, respectively). Radiographic risk factors for OA are shown in Figure 2. We found no significant radiographic risk factors for OA when comorbidities were adjusted. Multivariate model results are presented in Figure 3.
TABLE 5.
Nonradiographic Risk Factors for Hip Osteoarthritisa
| Hazard Ratio | 95% CI | P Value | |
|---|---|---|---|
| Male sex | 2.28 | 1.60–3.23 | <.01 |
| Body mass index >29 | 2.11 | 1.47–3.02 | <.01 |
| Age | 1.11 | 1.08–1.15 | <.01 |
| Smoker | 0.72 | 0.48–1.10 | .14 |
| Diabetes | 1.57 | 0.98–2.55 | .06 |
Boldface signifies statistical significance.
Figure 2.
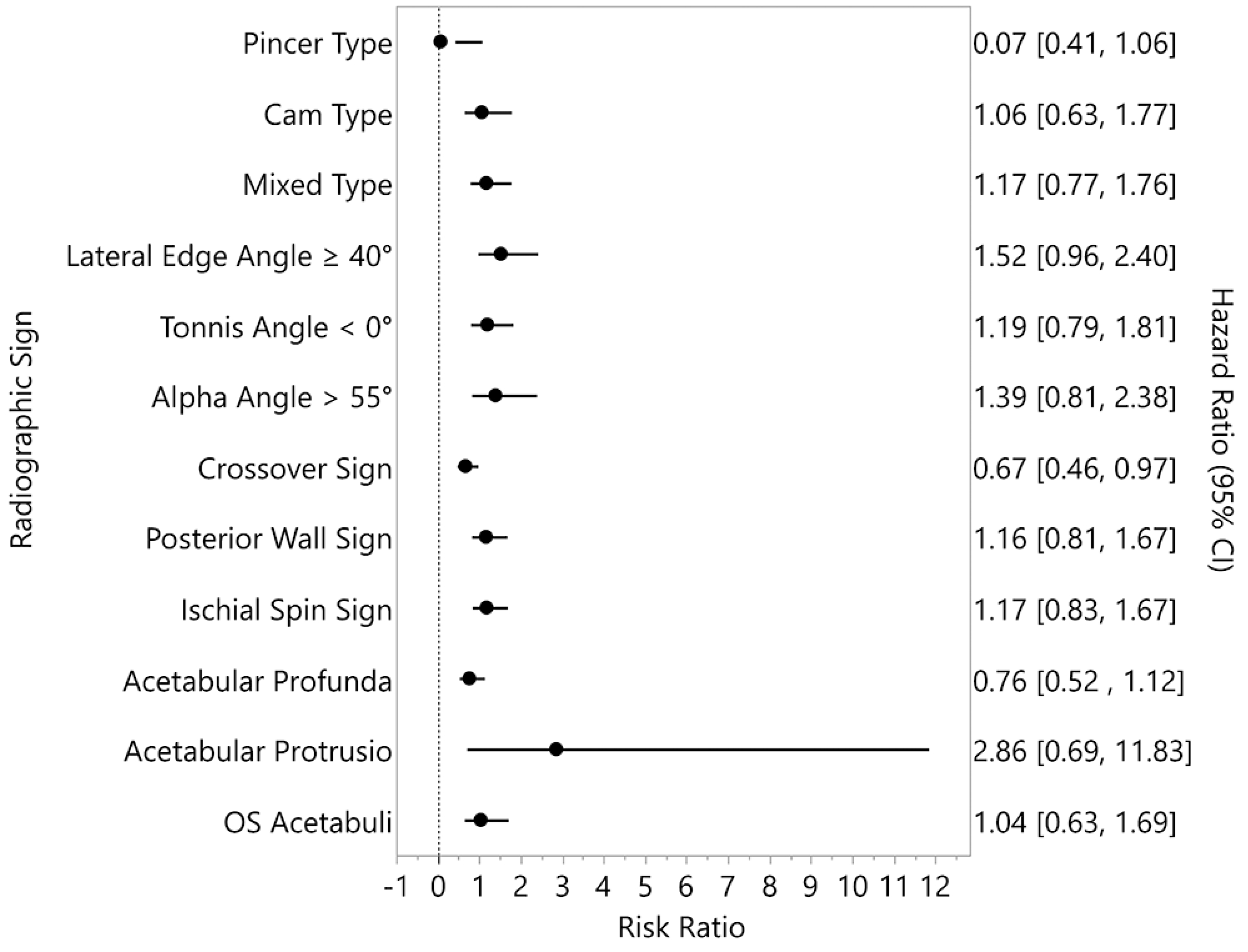
Forest plot of radiographic morphology and associated hazard ratios for osteoarthritis. Data were adjusted for comorbidities.
Figure 3.
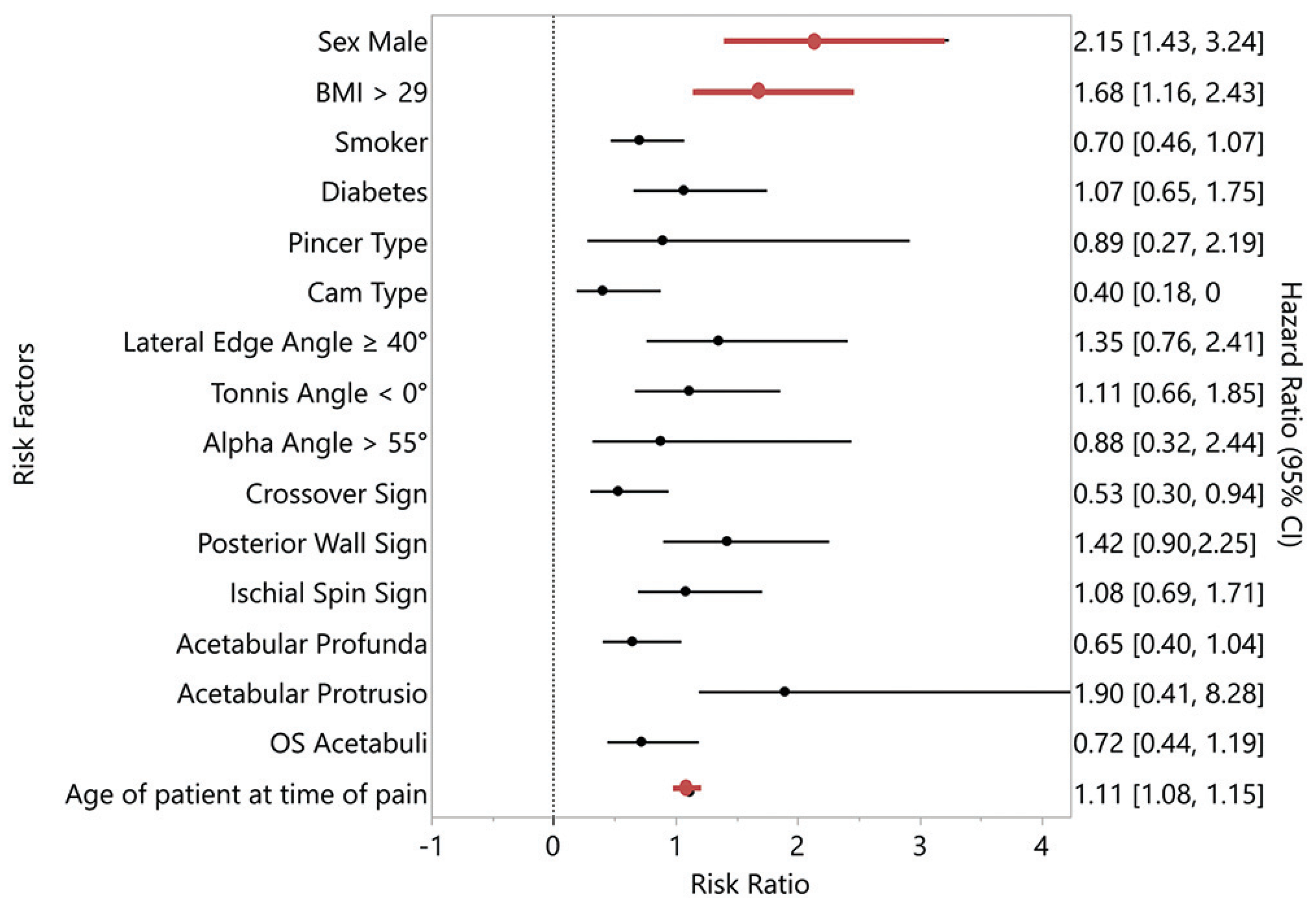
Forest plot of multivariate hazard ratios associated with osteoarthritis. Male sex, BMI >29, and patient age were statistically signficant, P < .05. BMI, body mass index.
DISCUSSION
FAI is considered a risk factor for the development of hip OA and the need for THA at a young age.4,10,13,25 Before our study, only radiographic risk factors for hip OA in patients with FAI had been evaluated.1,15,27,29,30 The present study has identified multiple nonradiographic risk factors for development of hip OA in patients with FAI. Male sex, increased age, and BMI greater than 29 were all risk factors for hip OA.
At mean follow-up of 24.7 years, 13.5% of hips had OA and 4% underwent THA. This is higher than the reported prevalence of symptomatic hip OA in the general population.2,17 Louer et al21 recently reported the rate of disease progression in the contralateral hip in patients who underwent hip arthroscopy for FAI. Those investigators found that 52% of patients developed contralateral symptoms within 4 years but did not report on the development of OA. The findings of the present study are similar to those of Hartofilikidas et al.15 At mean follow-up of 18.5 years, they reported a 17.7% rate of OA in a cohort of 96 patients with radiographic evidence of FAI on anteroposterior or lateral radiographs. Their slightly increased rate of OA is likely related to the higher mean age of 49.3 years.15 The Academic Network of Conservational Hip Outcomes Research (ANCHOR) study group reported a mean age of 28 years in their study of FAI patients undergoing surgery.8 Our study reports the same mean age for patient presentation to their physician with hip pain. It is important to understand the rate of hip OA progression in this age group, especially given that this is also the typical age for surgical intervention.8 This study provides baseline data for hip OA progression in young patients with hip pain and will allow for future comparison of progression in patients who undergo surgery. Another important finding in this study was that increased age was a risk factor for development of OA. We would expect the rate of OA and THA to increase with longer follow-up in this cohort.
Multiple studies have evaluated radiographic risk factors for hip OA in patients with FAI,1,15,27,29,30 but further knowledge is needed to identify nonradiographic risk factors for OA. In a recent review, Van Klij et al28 stated that cam morphology has been more consistently associated with OA than pincer morphology. They noted that more research is needed on this topic. In the present study, BMI greater than 29, male sex, and increased age were nonradiographic risk factors for development of OA. These variables have not been evaluated in patients with FAI but have been studied in the general population. Increased BMI is a well established risk factor for development of hip OA.16,20 Jiang et al16 performed a systematic review and meta-analysis and determined that a 5-unit increase in BMI was related to an increased risk of hip OA. Although women tend to develop OA more often than men, men have been found to have more OA involving the hip specifically.2,17 The exact reason for this is unknown, but the findings of the present study suggest that the same is true in patients with FAI. Smoking was not found to be a significant risk factor for development of OA in this cohort. This is consistent with findings in the general population, as smoking has been shown to be protective against hip OA in multiple studies.2
No specific radiographic morphologies were found to be statistically significant risk factors for hip OA. Beck et al5 concluded that acetabular overcoverage is a cause of hip OA, but cam morphology at the femoral head-neck junction has more often been associated with the development of OA.1,27,30 A large percentage of our cohort had mixed-type FAI, which made it difficult to determine specific radiographic risk factors. We suspect that the development of OA in patients with FAI is dependent upon the activity level and the relationship between abnormal morphologies on both the acetabulum and femur. More research is needed to determine what combinations of acetabular and femoral morphologies are risk factors for OA in patients with FAI.
There are limitations of this study to consider. It was retrospective, there was no control group, and the follow-up time was inconsistent. Due to the retrospective design, we were limited to chart review when evaluating physical examination findings. Physician understanding of FAI has increased since first described in 1999,22 but knowledge and documentation of physical examination techniques were limited in the early years of this study. Due to this, we were unable to confirm impingement examination findings in all cases. The mean age of the group was young, which is consistent with the typical presentation of FAI, but we would expect the rate of OA and THA to increase with age. Patients with mild or borderline acetabular dysplasia with concomitant femoral cam lesions were included in the study. It is known that these patients are at an increased risk of OA. The indication for THA was not standardized in all patients, so this group was not analyzed separately. In addition, this rate of symptomatic OA may be underestimated, as there would likely be more patients with radiographic OA progression who were not symptomatic enough to seek treatment from a physician. Despite these limitations, this study involves a large cohort of patients with hip pain and radiographic signs of FAI. The identification of modifiable risk factors for hip OA progression in patients with FAI will prove helpful when counseling patients.
CONCLUSION
At mean follow-up of 24.7 years, 14% of hips had symptomatic OA and 4% underwent THA. BMI greater than 29, male sex, and increased age at the time of presentation with hip pain were risk factors for hip OA. The cohort consisted of a large percentage of mixed-type FAI morphologies, and no specific radiographic risk factors for OA were identified.
ACKNOWLEDGMENT
The authors thank Dr Zhefeng Chen, MD, of the Department of Orthopedic Surgery, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, for his advice regarding the measurement and evaluation of radiographs.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was partially funded by the National Institutes of Health (NIH) under grants T32AR056950 as well as Jiangsu Health International Exchange Program (JSH-2018–004), and Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. A.J.K. has received IP royalties from Arthrex; consulting fees from Arthrex, JRF Ortho, DePuy, and Vericel; research support from Aesculap/B.Braun, Arthritis Foundation, Ceterix, Exactech, Gemini Medical, and Histogenics; and honoraria from Musculoskeletal Transplant Foundation; and he is a shareholder in Responsive Arthroscopy. B.A.L. has received IP royalties from Arthrex; consulting fees from Arthrex and Smith & Nephew; research support from Biomet, Smith & Nephew, and Stryker; and speaking fees from Linvatec. M.L. has a family member who receives royalties from Arthrex, Ossur, and Smith & Nephew and receives consulting fees from Arthrex, Linvatec, Ossur, and Smith & Nephew. H.P.M. has received hospitality payments from DePuy Synthes Sales. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
REFERENCES
- 1.Agricola R, Heijboer MP, Bierma-Zeinstra SM, et al. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–923. [DOI] [PubMed] [Google Scholar]
- 2.Allen KD, Golightly YM. State of the evidence. Curr Opin Rheumatol. 2015;27(3):276–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34(11):691–701. [DOI] [PubMed] [Google Scholar]
- 4.Beaule PE, Grammatopoulos G, Speirs A, et al. Unravelling the hip pistol grip/cam deformity: origins to joint degeneration. J Orthop Res. 2018;36(12):3125–3135. [DOI] [PubMed] [Google Scholar]
- 5.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 6.Bedi A, Kelly BT. Femoroacetabular impingement. J Bone Joint Surg Am. 2013;95(1):82–92. [DOI] [PubMed] [Google Scholar]
- 7.Blankenbaker DG, Tuite MJ. The painful hip: new concepts. Skeletal Radiol. 2006;35(6):352–370. [DOI] [PubMed] [Google Scholar]
- 8.Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 9.Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46–52. [DOI] [PubMed] [Google Scholar]
- 11.Frank JM, Flams JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31 (6): 1199–1204. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. [DOI] [PubMed] [Google Scholar]
- 13.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 14.Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 15.Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93(5):580–586. [DOI] [PubMed] [Google Scholar]
- 16.Jiang L, Rong J, Wang Y, et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2): 150–155. [DOI] [PubMed] [Google Scholar]
- 17.Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66(11 ):3013–3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kovalenko B, Bremjit P, Fernando N. Classifications in brief: Tönnis classification of hip osteoarthritis. Clin Orthop Relat Res. 2018; 476(8): 1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36(3):505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lievense AM, Bierma-Zeinstra SM, Verhagen AP, et al. Influence of obesity on the development of osteoarthritis of the hip: a systematic review. Rheumatology (Oxford). 2002;41(10):1155–1162. [DOI] [PubMed] [Google Scholar]
- 21.Louer CR, Pashos G, Clohisy JC, Nepple JJ. A prospective analysis of the contralateral hip among patients with femoroacetabular impingement: what are the risk factors for disease progression? Am J Sports Med. 2018;46(10):2486–2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. [PubMed] [Google Scholar]
- 23.Prather H, Harris-Hayes M, Hunt DM, et al. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010;2(10):888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanders TL, Pareek A, Desai VS, et al. Low accuracy of diagnostic codes to identify anterior cruciate ligament tear in orthopaedic database research. Am J Sports Med. 2018;46(12):2894–2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sankar WN, Nevitt M, Parvizi J, et al. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21(suppl 1):S7–S15. [DOI] [PubMed] [Google Scholar]
- 26.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007; 188(6):1540–1552. [DOI] [PubMed] [Google Scholar]
- 27.Thomas GE, Palmer AJ, Batra RN, et al. Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women: a 20 year longitudinal cohort study. Osteoarthritis Cartilage. 2014;22(10): 1504–1510. [DOI] [PubMed] [Google Scholar]
- 28.van Klij P, Heerey J, Waarsing JH, Agricola R. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. J Orthop Sports Phys Ther. 2018;48(4):230–238. [DOI] [PubMed] [Google Scholar]
- 29.Wyles CC, Heidenreich MJ, Jeng J, et al. The John Charnley Award: Redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475(2):336–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wyles CC, Norambuena GA, Howe BM, et al. Cam deformities and limited hip range of motion are associated with early osteoarthritic changes in adolescent athletes: a prospective matched cohort study. Am J Sports Med. 2017;45(13):3036–3043. [DOI] [PubMed] [Google Scholar]


