Abstract
Background
We describe differences for probability of receiving a fistula attempt, achieving fistula use, remaining catheter-free and the rate of access-related procedures as a function of sex.
Methods
Prospectively collected vascular access data on incident dialysis patients from five Canadian programs using the Dialysis Measurement Analysis and Reporting System to determine differences in fistula-related outcomes between women and men. The probability of receiving a fistula attempt and the probability of fistula use were determined using binary logistic regression. Catheter and fistula procedure rates were described using Poisson regression. We studied time to fistula attempt and time to fistula use, accounting for competing risks.
Results
We included 1446 (61%) men and 929 (39%) women. Men had a lower body mass index (P < 0.001) and were more likely to have coronary artery disease (P < 0.001) and peripheral vascular disease (p < 0.001). A total of 688 (48%) men and 403 (43%) women received a fistula attempt. Women were less likely to receive a fistula attempt by 6 months {odds ratio [OR] 0.64 [95% confidence interval (CI) 0.52–0.79]} and to achieve catheter-free use of their fistula by 1 year [OR 0.38 (95% CI 0.27–0.53)]. At an average of 2.30 access procedures per person-year, there is no difference between women and men [incidence rate ratio (IRR) 0.97 (95% CI 0.87–1.07)]. Restricting to those with a fistula attempt, women received more procedures [IRR 1.16 (95% CI 1.04–1.30)] attributed to increased catheter procedures [IRR 1.50 (95% CI 1.27–1.78)]. There was no difference in fistula procedures [IRR women versus men 0.96 (95% CI 0.85–1.07)].
Conclusion
Compared with men, fewer women undergo a fistula attempt. This disparity increases after adjusting for comorbidities. Women have the same number of fistula procedures as men but are less likely to successfully use their fistula.
Keywords: catheter, fistula, hemodialysis, sex differences, vascular access
INTRODUCTION
Arteriovenous fistulas are the preferred type of vascular access for hemodialysis due to lower rates of complications and mortality as compared with catheter use [1–4]. Although fistulas are actively promoted, more women use catheters at initiation of dialysis [5, 6] and fewer women receive [7] and use a fistula [8–10]. These vascular access differences may contribute to the increased mortality risk in young women starting hemodialysis [11]. While sex as a risk factor for fistula maturation failure is acknowledged in clinical prediction tools [12, 13], the reasons for poor fistula outcomes among women are unclear. These may be related to biology (sex) or sociocultural determinants of health (gender) influencing fistula creation and subsequent use. There are biological differences in the prevalence of chronic kidney disease (higher prevalence among women), vessel size and structure [14, 15] and gender differences that influence the timing of renal replacement therapy (more women choose conservative therapy and those who choose to start dialysis do so at a lower GFR, indicating a later start [16]). Women are older than men at initiation of hemodialysis, but men tend to have more comorbidities, making it difficult to interpret the net interaction of sex and comorbidities on fistula creation and use.
Vascular access is responsible for a significant amount of morbidity and mortality in hemodialysis patients. An unreliable or nonfunctional access will significantly impact quality of life and lead to an increased number of procedures and hospitalizations [17]. Fistulas are promoted in guidelines as the first choice of access for both women and men despite the lack of evidence to guide decisions. Why fewer women use a fistula is unknown, but understanding potential barriers to fistula use has the possibility of making a difference in their mortality risk. We do not know if similar efforts at fistula creation are made among women as among men, since most studies include selected cohorts in whom a fistula attempt has already occurred. We do not know if the probability of independent fistula use over time is comparable in women and men. It is not known whether procedure rates, time to successful fistula use (defined by catheter removal or catheter avoidance) and the proportion of time spent catheter-free differ between women and men. This information would be useful in order to allow women and men to make an informed choice about vascular access options and provide the impetus for future research into sex and gender differences in vascular access.
We sought to describe the differences between men and women with regard to the probabilities of receiving a fistula attempt, achieving independent fistula use (i.e. achieving catheter-free status), remaining catheter-free over time and the rate of access-related procedures as a function of sex in a cohort of Canadian incident hemodialysis patients.
MATERIALS AND METHODS
Data source
We used data from five Canadian dialysis programs (Alberta Kidney Care South, Manitoba Renal Program, Sunnybrook Health Sciences Centre, London Health Sciences Center and the Ottawa Hospital) using the Dialysis Measurement Analysis and Reporting System, which prospectively collects detailed clinical information on incident dialysis patients [18–20]. To ensure data quality, all data elements were reviewed by experts. Data elements included demographics, comorbidities, laboratory values, history of predialysis care and changes in status (e.g. modality switch, death, etc.). In addition, all vascular access procedures are captured, permitting construction of a longitudinal record of vascular access use, including the type of vascular access in use and the start and stop dates of each period of use.
Study design
Adults (≥18 years of age) who started hemodialysis between 1 January 2004 and 31 May 2012 were eligible for this study. We excluded people who initiated hemodialysis following a failed kidney transplant, transitioned to peritoneal dialysis within 6 months of hemodialysis initiation, had a life expectancy of <1 year at hemodialysis initiation due to dialysis-unrelated reasons, such as metastatic cancer or other terminal illness, or used an arteriovenous graft at hemodialysis initiation (<5% of people starting dialysis in Canada) [19]. We followed participants from the start of hemodialysis until the earliest of death, kidney transplantation, loss to follow-up, transfer out of the program, switch to peritoneal dialysis, recovery of kidney function or the end of the study period. The research ethics boards at each of the five participating sites granted ethics approval for this study.
Exposure
We examined differences in fistula-related outcomes between women and men as defined by biological sex.
Outcomes
Outcome 1: Probability of receiving an attempt at fistula creation
Our first outcome of interest was whether the patient would receive a fistula attempt (including prior to hemodialysis start), measured in two ways: the overall probability of receiving a fistula creation attempt by 6 months (yes/no—restricted to patients with at least 6 months of follow-up) and time to a fistula creation attempt.
Outcome 2: Probability of successful fistula use
This analysis was restricted to patients who received a fistula attempt. We defined successful fistula use as independent use of a fistula for hemodialysis (i.e. without a catheter in place). We measured this outcome in three ways: probability of use within 1 year of dialysis (yes/no—restricted to patients with at least 1 year of follow-up), time to fistula use and proportion of follow-up time spent catheter-free. Follow-up was from dialysis start for fistulas created before dialysis start and from the creation attempt for fistulas created after dialysis start.
Outcome 3: Access-related procedures
We analyzed the count of access-related procedures (surgical and radiology) prior to the start of dialysis (i.e. baseline number of procedures at beginning of follow-up) and the rate of access-related procedures after dialysis start. Procedures were then subcategorized as catheter related or fistula related. Rates were defined as the average number of procedures per person-year of follow-up.
Statistical analyses
Standard methods for quantitative data to summarize baseline characteristics and binary logistic regression were used to obtain odds ratios (ORs) for the outcome of receiving and using a fistula. For time-to-event analyses (time to attempt and time to use), we examined the cumulative incidence of each event, treating death, transplant, recovery of kidney function and starting peritoneal dialysis (PD) as competing risks. The Fine and Grey method estimated subhazard ratios [21]. We analyzed the probability of catheter-free use for each day of follow-up using logistic regression of repeated Bernoulli trials within subjects, using robust variances to account for the dependency (correlations) in the data. Finally, crude procedure rates and counts with 95% confidence intervals (CIs) were described using Poisson regression. To obtain incidence rate ratios (IRRs), procedure rates were modeled using negative binomial regression to account for overdispersion in the data.
Regression models were adjusted for age, a history of diabetes mellitus or cardiovascular disease [including coronary artery disease (CAD), congestive heart failure, cerebrovascular disease and peripheral vascular disease] and whether the patient started dialysis as an inpatient. Stata 14 was used for all analyses (StataCorp, College Station, TX, USA).
RESULTS
Demographics
After applying the exclusion criteria, 929 (39%) women and 1446 (61%) men were included in this study (Figure 1). Women had a higher body mass index (BMI; P < 0.001) and were less likely to have CAD (P < 0.001) and peripheral vascular disease (P < 0.001) than men (see Table 1). Only 13% (118 women) were <47 years old. There were no differences between women and men in terms of age (P = 0.34), diabetes (P = 0.13), congestive heart failure (P = 0.15), cerebrovascular disease (P = 0.37) and cancer (P = 0.58). There were no statistically significant differences in the number of inpatient or intensive care unit dialysis starts, but slightly more women had predialysis care (79% versus 75%; P = 0.01).
FIGURE 1:

Cohort creation. Description of study cohort.
Table 1.
Patient characteristics
| Variable |
|
|
P- value |
|---|---|---|---|
| Age (years), mean (SD) | 65.4 (15.1) | 64.8 (15.0) | 0.34 |
| BMI, mean (SD) | 29.4 (98.6) | 28.0 (7.0) | <0.001 |
| eGFR at start of dialysis, mean (SD) | 9.5 (5.9) | 10.3 (5.8) | 0.001 |
| Diabetes, n (%) | 539 (58) | 793 (55) | 0.13 |
| Cardiovascular disease (any), n (%) | 504 (54) | 839 (58) | 0.07 |
| CAD, n (%) | 296 (32) | 567 (39) | <0.001 |
| Congestive heart failure, n (%) | 284 (31) | 402 (28) | 0.15 |
| Cerebrovascular disease, n (%) | 137 (15) | 233 (16) | 0.37 |
| Peripheral vascular disease, n (%) | 119 (13) | 309 (21) | <0.001 |
| Cancer, n (%) | 176 (19) | 261 (18) | 0.58 |
| Started dialysis as inpatient, n (%) | 534 (58) | 873 (60) | 0.16 |
| Started dialysis in the ICU, n (%) | 149 (16) | 237 (16) | 0.82 |
| Any predialysis care, n (%) | 739 (79) | 1082 (75) | 0.01 |
| Four months of predialysis care, n (%) | 604 (65) | 905 (63) | 0.23 |
| Twelve months of predialysis care, n (%) | 488 (53) | 726 (50) | 0.27 |
eGFR, estimated glomerular filtration rate; ICU, intensive care unit.
Follow-up
The median follow-up time from dialysis start was 1 year and did not differ between women and men. The most common reason for exiting the study was reaching the end of study date (47%), followed by death (27%), recovery of kidney function (10%), transfer to another program (7%), receipt of kidney transplant (5%) and transfer to PD (3%). Loss to follow-up was negligible (<1%). Women were more likely to reach the end of study date (51% versus 45%; P = 0.006), while men were slightly more likely to receive a transplant (6% versus 4%; P = 0.02) or recover kidney function (11% versus 9%; P = 0.05).
Probability of receiving an attempt at fistula creation
Overall, 403 (43%) women and 688 (48%) men received a fistula creation attempt. Of those who received a fistula attempt, there were no statistically significant differences in the number of attempts (up to three) or how many creations occurred before dialysis initiation versus after dialysis initiation. For those with 6 months of follow-up, 288 (44%) women and 538 (54%) men received a fistula attempt by 6 months. The modeled probability adjusting for covariates (age, diabetes, cardiovascular disease and inpatient starts) suggested women were less likely to receive a fistula creation attempt by 6 months [OR 0.64 (95% CI 0.52–0.79)].
In our analysis of time to fistula creation, accounting for competing risks, we found that at 6 months after dialysis start, 37% of women and 43% of men received a fistula attempt, and at 12 months the proportions were 43% and 49%, respectively [adjusted hazard ratio (HR) women versus men 0.83 (95% CI 0.73–0.93); Figure 2].
FIGURE 2:
Time to fistula creation. Cohort includes those with and without fistula attempts. The y-axis is the cumulative incidence of patients receiving a fistula creation attempt, accounting for the competing risks of death, transplant, recovery of kidney function and transfer to PD. The x-axis is the time from dialysis start in months (note some patients received a fistula attempt prior to starting dialysis).
Type of fistula creation
Despite the policy of distal fistula first, there is a significant difference in the site of placement of the fistula between men and women (P < 0.0001). Table 2 shows the distribution of fistula placement according to sex; the most common type of fistula in women is a radiocephalic fistula and in men it is a brachiocephalic fistula.
Table 2.
Anatomic location of fistula
| Fistula type | Sex |
|
|---|---|---|
| Male, n (%) | Female, n (%) | |
| Brachiobasilic | 35 (7) | 25 (9) |
| Brachiocephalic | 169 (35) | 169 (61) |
| Radiocephalic | 284 (58) | 84 (30) |
| Total | 488 (100) | 278 (100) |
Probability of successful fistula use
A total of 727 patients (261 women and 466 men) had at least 1 year of follow-up. At 1 year, 147 (56%) women and 354 (76%) men achieved catheter-free use of their fistula. Modeled probability adjusting for covariates indicated that women were less likely to achieve catheter-free use than men [OR 0.38 (95% CI 0.27–0.53)].
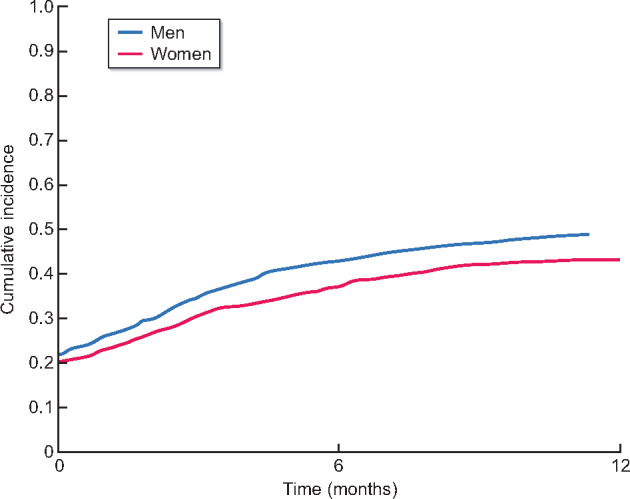
Time-to-first-use analysis accounting for competing risks showed that 44% of women achieved catheter-free use by 6 months compared with 56% of men, and at 12 months, it was 53% and 71%, respectively [HR women versus men 0.65 (95% CI 0.56–0.76); see Figure 3].
FIGURE 3:

Time to first catheter-free use of a fistula. Cohort includes only those with a fistula attempt. The y-axis is the cumulative incidence of patients achieving catheter-free use of their fistula, accounting for the competing risks of death, transplant, recovery of kidney function and transfer to PD. The x-axis is the time from dialysis start (for those with a predialysis fistula attempt) or from a fistula creation attempt (for those with a postdialysis initiation fistula attempt) in months (note some patients began dialysis with a functioning fistula).
The crude average follow-up time spent catheter-free was 37% for women and 52% for men. Modeled probability adjusting for covariates suggests women were less likely to use their fistula catheter-free per day of follow-up [OR 0.42 (95% CI 0.32–0.56)].
Access-related procedures
Overall, there was an average of 2.30 procedures per person-year after the start of dialysis, with no significant difference between women and men [adjusted IRR women versus men 0.97 (95% CI 0.87–1.07); see Table 3]. Restricting the cohort to the catheter-only group, women received fewer catheter-related procedures than men [IRR women versus men 0.80 (95% CI 0.67–0.95)]. Restricting the cohort to those who received a fistula attempt, women received more procedures overall [IRR women versus men 1.16 (95% CI 1.04–1.30)], which was due to increased catheter-related procedures [IRR women versus men 1.50 (95% CI 1.27–1.78)]. There was no difference in the total number of fistula-related procedures in this subcohort [IRR women versus men 0.96 (0.85–1.07)] nor the number of fistula-related interventions [IRR women versus men 0.93 (0.80–1.08)]. Counts of procedures before dialysis were similar between women and men.
Table 3.
Counts and rates of procedures before and after dialysis initiation
|
|
|
||||
|---|---|---|---|---|---|---|
| Procedure |
|
|
|
|
|
|
| Procedure rates (95% CI) per person-year after the start of dialysis Adjusted IRR women versus men (95% CI) | ||||||
| Total procedure rates |
|
|
|
|
|
|
| IRR 0.97 (0.87–1.07) | *IRR 0.80 (0.67–0.95) | *IRR 1.16 (1.04–1.30) | ||||
| Catheter related |
|
|
|
|
||
| *IRR 0.80 (0.67–0.95) | *IRR 1.50 (1.27–1.78) | |||||
| Fistula related |
|
|
||||
| IRR 0.96 (0.85–1.07) | ||||||
| Fistula intervention |
|
|
||||
| IRR 0.93 (0.80–1.08) | ||||||
| Procedure counts (95% CI) per person prior to the start of dialysis | ||||||
| Total |
|
|
|
|
|
|
| Catheter related |
|
|
|
|
||
| Fistula related |
|
|
||||
| Fistula related (intervention) |
|
|
||||
Crude Poisson rates per person-year with 95% CI. IRR from negative binomial regression models, adjusting for age, gender, diabetes, cardiovascular disease and inpatient dialysis start. Crude Poisson counts per person and 95% CIs.
*p< 0.001.
DISCUSSION
Our study of Canadian incident hemodialysis patients reveals differences in vascular access management and outcomes between women and men. We found that, as compared with men, fewer women underwent a fistula creation attempt. This sex disparity increased after adjusting for comorbidities, with women less likely to undergo fistula creation surgery. Even with more time on dialysis, these differences did not improve. Not only did women have fewer fistula creations, they also spent more time with a catheter and took longer to achieve catheter-free use of their fistula. Men were almost three times more likely to achieve catheter-free use of their fistula. Despite the fact that women were less likely to have a successful fistula, we did not find any overall differences in the number of access-related procedures, although in the cohort that had a fistula attempt, women had significantly more catheter-related procedures.
Similar to our findings, large cohort studies indicate that women are less likely than men to receive a fistula [7, 9, 10] and use a fistula on dialysis (OR 0.85) [8, 10]. Woodside et al. [9] also noted fewer women within a prevalent hemodialysis cohort had a fistula placed (43% versus 57% men) and used the fistula. Catheter use at the time of dialysis start is consistently higher in women than men [5, 6]. Recent US data reveal a persistent difference in fistula use at 1 year in a cohort of patients >65 years of age (56% women versus 71% men) [10], findings that are similar to those of our younger cohort.
Notably, some non-North American studies have found no sex difference in vascular access outcomes [22] or even better outcomes in women [23], which leaves one to question whether some of the vascular access disparity has a possible gender component. Access to predialysis care may increase the opportunity for timely referral to surgery and subsequent fistula creation prior to dialysis start. In our study, slightly more women received predialysis care, and yet more men underwent fistula creation. Access to surgeons or the willingness of surgeons to create fistulas may be different in women, implying inequity in gender-related access to care similar to other areas of medicine [24, 25]. Alternatively, surgeons may be appropriately determining that the vasculature of women is unsuitable for fistula creation and making the choice to avoid fistula placement or to place the fistula at a more proximal site (brachiocephalic) that is associated with better success rates. However, the center-dependent fistula creation rate (data not shown) varies widely, with some centers attempting fistulas equally between men and women while others have more attempts in men, showing variability in fistula care.
In our study, we found that even after a fistula was created, women had prolonged exposure to catheters and were less likely to successfully use their fistula. Whether this represents a sex difference in fistula maturation or a gender difference with more women choosing to use a catheter is unknown. Women perceive pain differently than men [26], which might be a factor leading to more women choosing to avoid fistula use, perhaps for fear of pain with cannulation. We did find more catheter-related procedures in women with fistula creation. Since the duration of catheter exposure and the number of catheter insertions are associated with reduced fistula maturation [27], the higher number of catheter procedures and the longer time of exposure to catheters may contribute to reduced successful fistula use seen in women.
The disparity in fistula creation and use between men and women is not explained by the clinical and demographic patient characteristics captured in our dataset. We found that peripheral vascular disease and CAD, which are associated with a higher risk of fistula failure [12, 13], were less frequent in women. BMI was higher in women, but the effect of BMI as a risk factor for fistula failure is not well established [12].
Other factors that may impact fistula maturation and successful use include vein size at the time of creation and assisted maturation interventions. We do not have data on vessel size at the time of fistula creation, however, vessel size does not appear to be sex dependent when using objective [27] ultrasound criteria [28]. In our study, we found that while women had the same number of fistula procedures as men, they were less likely to use their fistula. This is similar to the observations by Wilmink et al. [29] in which women had lower rates of maturation regardless of the type of fistula. If differences in biology lead to reduced fistula maturation in women, one might expect to find more fistula interventions in women in an effort to promote fistula function. Others have shown that women are more likely to require a salvage procedure to promote fistula maturation [10, 14, 30, 31], but the likelihood of maturation after a procedure is similar among women and men [14]. The similar numbers of fistula interventions despite reduced fistula use in women may suggest reduced access to salvage therapies for women.
Our study is different from most in that it included all incident HD patients regardless of whether they receive a fistula attempt and it is not restricted to patients >65 years of age [10]. By including all incident hemodialysis patients, our study provides an opportunity to determine the sex-specific probability of receiving fistula surgery and of achieving catheter-free use of the fistula or remaining with a catheter over time. Other strengths of our study include a robust dataset that is collected in a prospective manner from multiple centers across Canada. Limitations include the lack of detail on fistula maturation and fistula cannulation, thereby limiting the ability to understand the reasons for prolonged catheter use. Information such as vessel diameter, fistula flow rates, fistula maturation and patient preference are absent from our dataset but could be useful to explain sex and gender differences in vascular access outcomes. The study does not include details such as the timing of referral for access creation or the thresholds for access intervention. The lack of qualitative data regarding patient preference or provider reasons for fistula-related procedures is another limitation of the study. The dataset does not include menopause status, but since the median age of menopause is 47 years in a dialysis cohort [32], premenopausal women are underrepresented in our sample (only 118 or 13% were <47 years old). Patients were classified according to self-identified binary gender and this was assumed to be representative of biological sex for data analysis purposes. Finally, our dataset does not capture other potential gender-based variables, like education or socioeconomic status, that may impact on fistula creation and/or use.
In conclusion, we found differences between women and men in the likelihood of receiving a fistula creation attempt or successful use of a fistula among incident hemodialysis patients. It is possible that the lower fistula use in women may have health implications. We have previously shown that regardless of sex, fistula use is associated with better patient survival and fewer infections [33]. Similarly, although not statistically significant, in this study we also found more deaths in the catheter-only group as compared with those who underwent a fistula attempt (P = 0.08), regardless of sex.
Gender- and sex-specific effects may underlie the vascular access differences we observed. The choice to abandon a fistula or a differential access to fistula surgery or fistula salvage interventions is possibly driven by gender factors. We do not know the influence of biology or behavior on vascular access outcomes between men and women, but the nephrology community needs to be aware of this disparity. This critical area of future research should include gender- and sex-related differences in vascular access care and outcomes. Further knowledge in these areas will allow for policy development and informed decision-making regarding vascular access options for both women and men.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the study participants. Funding for this work was provided by Canadian Institutes of Health Research grant number PJT 162369 (A 406897).
FUNDING
Canadian Institute of Health Research Operating Grant, FRN 1622369.
CONFLICT OF INTEREST STATEMENT
J.M.M., S.B.A., A.C., M.E., K.K.-S., S.H., B.H., M.J. and N.S.-D. have no disclosures to report. R.B.Q. and M.J.O. are the co-creators of the Dialysis Measurement Analysis and Reporting System. P.R. received funding from the Canadian Institutes of Health Research for the study.
REFERENCES
- 1. Pastan S, Soucie JM, McClellan WM.. Vascular access and increased risk of death among hemodialysis patients. Kidney Int 2002; 62: 620–626 [DOI] [PubMed] [Google Scholar]
- 2. Ravani P, Palmer SC, Oliver MJ. et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol 2013; 24: 465–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moist LM, Trpeski L, Na Y. et al. Increased hemodialysis catheter use in Canada and associated mortality risk: data from the Canadian Organ Replacement Registry 2001–2004. Clin J Am Soc Nephrol 2008; 3: 1726–1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Astor BC, Eustace JA, Powe NR. et al. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 2005; 16: 1449–1455 [DOI] [PubMed] [Google Scholar]
- 5. Saran R, Li Y, Robinson B. et al. US Renal Data System 2015 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2016; 67(3 Suppl 1): Svii–S305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Noordzij M, Jager KJ, van der Veer SN. et al. Use of vascular access for haemodialysis in Europe: a report from the ERA-EDTA Registry. Nephrol Dial Transplant 2014; 29: 1956–1964 [DOI] [PubMed] [Google Scholar]
- 7. Pisoni RL, Young EW, Dykstra DM. et al. Vascular access use in Europe and the United States: results from the DOPPS. Kidney Int 2002; 61: 305–316 [DOI] [PubMed] [Google Scholar]
- 8. Shah S, Leonard AC, Meganathan K. et al. Gender and racial disparities in initial hemodialysis access and outcomes in incident end-stage renal disease patients. Am J Nephrol 2018; 48: 4–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Woodside KJ, Bell S, Mukhopadhyay P. et al. Arteriovenous fistula maturation in prevalent hemodialysis patients in the United States: a national study. Am J Kidney Dis 2018; 71: 793–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee T, Qian J, Thamer M. et al. Gender disparities in vascular access surgical outcomes in elderly hemodialysis patients. Am J Nephrol 2019; 49: 11–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carrero JJ, de Jager DJ, Verduijn M. et al. Cardiovascular and noncardiovascular mortality among men and women starting dialysis. Clin J Am Soc Nephrol 2011; 6: 1722–1730 [DOI] [PubMed] [Google Scholar]
- 12. Siddiqui MA, Ashraff S, Santos D. et al. Predictive parameters of arteriovenous fistula maturation in patients with end-stage renal disease. Kidney Res Clin Pract 2018; 37: 277–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lok CE, Allon M, Moist L. et al. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I). J Am Soc Nephrol 2006; 17: 3204–3212 [DOI] [PubMed] [Google Scholar]
- 14. Miller CD, Robbin ML, Allon M.. Gender differences in outcomes of arteriovenous fistulas in hemodialysis patients. Kidney Int 2003; 63: 346–352 [DOI] [PubMed] [Google Scholar]
- 15. Robbin ML, Chamberlain NE, Lockhart ME. et al. Hemodialysis arteriovenous fistula maturity: US evaluation. Radiology 2002; 225: 59–64 [DOI] [PubMed] [Google Scholar]
- 16. Carrero JJ, Hecking M, Chesnaye NC. et al. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol 2018; 14: 151–164 [DOI] [PubMed] [Google Scholar]
- 17. Domenick Sridharan N, Fish L, Yu L. et al. The associations of hemodialysis access type and access satisfaction with health-related quality of life. J Vasc Surg 2018; 67: 229–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Quinn RR, Ravani P, Zhang X. et al. Impact of modality choice on rates of hospitalization in patients eligible for both peritoneal dialysis and hemodialysis. Perit Dial Int 2014; 34: 41–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Quinn RR, Oliver MJ, Devoe D. et al. The effect of predialysis fistula attempt on risk of all-cause and access-related death. J Am Soc Nephrol 2017; 28: 613–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oliver MJ, Verrelli M, Zacharias JM. et al. Choosing peritoneal dialysis reduces the risk of invasive access interventions. Nephrol Dial Transplant 2012; 27: 810–816 [DOI] [PubMed] [Google Scholar]
- 21. Fine J, Gray RJ.. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509 [Google Scholar]
- 22. Puskar D, Pasini J, Savic I. et al. Survival of primary arteriovenous fistula in 463 patients on chronic hemodialysis. Croat Med J 2002; 43: 306–311 [PubMed] [Google Scholar]
- 23. Erkut B, Unlu Y, Ceviz M. et al. Primary arteriovenous fistulas in the forearm for hemodialysis: effect of miscellaneous factors in fistula patency. Ren Fail 2006; 28: 275–281 [DOI] [PubMed] [Google Scholar]
- 24. Steingart RM, Packer M, Hamm P. et al. Sex differences in the management of coronary artery disease. Survival and Ventricular Enlargement Investigators. N Engl J Med 1991; 325: 226–230 [DOI] [PubMed] [Google Scholar]
- 25. Daumit GL, Hermann JA, Powe NR.. Relation of gender and health insurance to cardiovascular procedure use in persons with progression of chronic renal disease. Med Care 2000; 38: 354–365 [DOI] [PubMed] [Google Scholar]
- 26. Enck P, Klosterhalfen S.. Does sex/gender play a role in placebo and nocebo effects? Conflicting evidence from clinical trials and experimental studies. Front Neurosci 2019; 13: 160–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ozpak B, Yilmaz Y.. Arteriovenous fistulas ipsilateral to internal jugular catheters for hemodialysis have decreased patency rates. Vascular 2019; 27: 270–276 [DOI] [PubMed] [Google Scholar]
- 28. Caplin N, Sedlacek M, Teodorescu V. et al. Venous access: women are equal. Am J Kidney Dis 2003; 41: 429–432 [DOI] [PubMed] [Google Scholar]
- 29. Wilmink T, Hollingworth L, Powers S. et al. Natural history of common autologous arteriovenous fistulae: consequences for planning of dialysis. Eur J Vasc Endovasc Surg 2016; 51: 134–140 [DOI] [PubMed] [Google Scholar]
- 30. Lee T, Ullah A, Allon M. et al. Decreased cumulative access survival in arteriovenous fistulas requiring interventions to promote maturation. Clin J Am Soc Nephrol 2011; 6: 575–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Harms JC, Rangarajan S, Young CJ. et al. Outcomes of arteriovenous fistulas and grafts with or without intervention before successful use. J Vasc Surg 2016; 64: 155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Holley JL, Schmidt RJ, Bender FH. et al. Gynecologic and reproductive issues in women on dialysis. Am J Kidney Dis 1997; 29: 685–690 [DOI] [PubMed] [Google Scholar]
- 33. Ravani P, Quinn R, Oliver M. et al. Examining the association between hemodialysis access type and mortality: the role of access complications. Clin J Am Soc Nephrol 2017; 12: 955–964 [DOI] [PMC free article] [PubMed] [Google Scholar]


