Abstract
The novel coronavirus disease (COVID-19) has resulted in the worldwide disruption of everyday life but the impact and response to the pandemic have not been uniform. Many countries rapidly deployed physical-distancing mandates to curb the spread of the COVID-19; others did not. Whilst social distancing strategies are necessary to reduce the transmission of the virus, it is also important to examine unintended psychiatric consequences of social isolation. We examined psychological distress in four countries with distinct public health strategies (South Korea, Hong Kong, France and the United States) to identify common and region-specific factors that may contribute to mental illness. From March to July June 2020, an online survey of demographics, general health, mental health, loneliness and social networks was conducted. Overall, younger age, greater concern for COVID, and increased loneliness predicted worse psychological outcome, although the magnitudes of the effects were not uniform among the four countries. We also observed notable differences in psychological distress; Hong Kong, with the strictest lockdown mandate, suffered the most drastic worsening of mental health outcome. To explain differential exacerbations of psychological distress around the globe during the pandemic, contributions of social unrest, economic uncertainty, and disruption to regular routine should be considered.
1. INTRODUCTION
Beginning in December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the accompanying COVID-19 pandemic has dramatically altered the lives of people around the world. As of September 1, 2020, 25.3 million people worldwide have tested positive for the virus and 848,000 people have died, although the actual numbers are likely higher (https://COVID-19.who.int/).
Psychiatric consequences of COVID-19 worldwide will permeate all aspects of societal functioning long after the end of the pandemic (Holmes et al., 2020). Trauma and stress directly stemming from the COVID-19 infection as well as the social isolation and loneliness associated with social distancing practices are likely to exert direct and chronic impact on mental health. Even prior to the current pandemic, psychological disorders were ranked worldwide as the 5th leading cause of disability, according to the 2013 Global Burden of Diseases study, with 266 million cases of anxiety disorders and 253 million cases of major depressive disorder (Solomon et al, 2015; Vos et al, 2015; Murray et al, 2015). The extraordinary societal burden of mental illness is likely to grow rapidly in the near future, as trauma, distress, and desolation saturate the aftermath of the COVID-19 public health crisis.
Unfortunately, social distancing and quarantines that were deemed necessary to stem the spread of COVID-19 are expected to drastically increase feelings of social disconnection, loneliness, and distress. Loneliness and social disconnection are known to play a major role in poor physical and mental health (Badcock et al., 2020; Cacioppo et al., 2015; Holt-Lunstad et al., 2017). In addition, based on the catastrophic psychiatric outcomes of SARS survivors (cumulative incidence of DSM disorder in 58.9% of the survivors) (Mak et al., 2009), we expect a significant increase in the incidence of post-traumatic stress disorder (PTSD), depression, anxiety, substance use, suicide, and other mental disorders post-COVID among the survivors, their caregivers, and healthcare workers.
A rapidly developing body of work has focused on the mental health of samples in countries around the world. Preliminary results from China confirm the high prevalence of PTSD among the survivors of COVID-19 (Bo et al., 2020) and mental illness among the general population (Gao et al., 2020). In the United States of America (USA), a recent community report from the Centers for Disease Control and Prevention (CDC) in late June reported that younger adults, racial/ethnic minorities, healthcare workers, and caregivers are experiencing mental health issues at high rates, raising the concern for substance use and suicide (Czeisler et al., 2020). A large cohort of at-risk groups for both physical and mental illness in France (patients with breast cancer, asthma, depression and migraine) reported elevated rates of psychological distress, with female gender, unemployment, depression diagnosis, and smartphone usage predicting higher distress (Chaix et al., 2020). In addition, college students in France reported elevated levels of anxiety and stress, particularly among those who do not live with their family (Husky et al., 2020). In two earlier reports by member of our research group, we found elevated levels of depression, stress, anxiety, and loneliness in residents of South Korea and Hong Kong (Lee et al., n.d.; Tso and Park, 2020). Coping with COVID-19 place a heavy burden across the globe and different countries have followed distinct strategies to curb the impact of the virus on the society (e.g., different types of lockdown procedures and mitigation efforts). What is relatively unknown is whether the psychiatric consequences of coping with the pandemic are relatively uniform or divergent across the world.
In this study, we examined the psychosocial distress experienced among the general public during the initial phase of the pandemic (from March through July 2020) in four countries: the United States of America (USA), Republic of Korea, France and Hong Kong. There were two aims. First, we investigated potential differences in psychological distress among these four countries. Second, we examined how psychological distress might be associated with demographic characteristics (age, sex, education, employment status, marital status, and living arrangement), concern for COVID-19, loneliness, and social networks. We hypothesized that people in all four countries would show increased psychological distress. We also hypothesized that age, female sex, unemployment, living alone, concern for COVID, loneliness, and reduced social network would be related to worse psychological outcome.
2. METHODS
2.1. Participants
There were 1306 participants (age 18-85). The survey was conducted online using RedCap in the USA, LimeSurvey in France, Google Forms in South Korea, and Qualtrics in Hong Kong. Links to each survey were distributed via social media (e.g., Twitter, Facebook, Reddit, and emailing lists). The survey, conducted in English, French, Korean and Chinese, was completely anonymous, and no identifying information was recorded. This study received exempt determination from the Vanderbilt University Institutional Review Board (IRB #200337) and University of Michigan IRB (IRB# HUM00179454). For the survey in France, ethics approval was obtained from the University of Strasbourg (Unistra/CER/2020-10).
Participants from the USA (n=334) completed the survey between March 16, 2020 to July 19, 2020. Participants from South Korea (n=395) completed the survey between March 22, 2020 to June 1, 2020. Participants from France (n=145) completed the survey between April 17 and April 30, 2020. Participants from Hong Kong (n=432) completed the survey between March 30, 2020 and May 30, 2020.
2.2. Measures
The survey collected self-reported information on demographics, general health, mental health, loneliness, and social networks.
Demographic variables included age, sex, years of education, employment status, marital status, and living arrangement (living alone or living with others). Education was transformed into a binary variable to make comparisons consistent across samples: the two levels included those who had secondary education or lower and those who had completed at least a bachelor’s degree. Marital status and living arrangement were collapsed into one variable because all married couples reported that they lived with family while unmarried people (never married, divorced, separated or widowed) either lived alone or lived with family. Concern for COVID-19 was measured on a 4-point scale ranging from “no concern” to “extremely concerned”.
General health questions encompassed 6 variables and included self-report of overall health, rated on a 1 (excellent) – 5 (poor) scale; number of days within the past 30 days that the respondent had experienced a physical illness or poor mental health; number of days when physical or mental illness impacted usual activities; number of days when pain affected usual activities; and days spent feeling worried, stressed, or anxious.
In order to measure specific mental health domains we administered the Depression Anxiety Stress Scales (DASS) (Lovibond and Lovibond, 1995). For DASS, scores for Depression, Anxiety, and Stress subscales were calculated for each participant.
To understand the psychosocial impact of COVID-19, we administered the UCLA Loneliness Scale (Russell, 1996) to gauge subjective feelings of loneliness and the Social Network Index (Cohen, 1997) to quantify objective levels of social isolation by incorporating the diversity (i.e., number of social roles) and size (number of people with whom the respondent has regular contact in person or remotely) of social networks.
2.3. Statistical Analysis
All analyses were carried out in R v3.6.2. Comparisons of continuous and categorical demographic variables between geographic regions were conducted using one-way analysis of variance (ANOVA) and chi-squared tests, respectively.
A psychological distress score was calculated using the 6 single-items from the physical/mental health inventory (general health, days physical health not good, days mental health not good, days physical or mental health affected usual activities, days of physical pain, days spent worried/stressed/anxious) and the DASS subscales. Each variable for each participant was transformed into a z-score, then summed together to create a total psychological distress score where more positive numbers indicated worse psychological distress overall.
Differences among geographic regions in terms of individual items that made up the psychological distress score, loneliness, diversity of social networks, and size of social networks were investigated using an analysis of covariance (ANCOVA) controlling for demographic variables.
In order to compare the contribution of demographic, loneliness, and social network variables to psychological distress among the four regions, a stepwise linear regression model comparison approach was used. In each model, the individual variable intercept and coefficient varied by region. The demographic variables were included in the first step, loneliness in the second step, and social network variables in the third and final step. For each step, a significant change in the adjusted R2 was used to examine whether the addition of each variable explained a significant proportion of variance in psychological distress. The Akaike information criterion (AIC) was further used to investigate the best fitting model. The summary function was used to examine the coefficients of the selected model.
Using the variables specified in the model comparison, a series of 4 multiple linear regressions were conducted to examine the contribution of those variables to psychological distress within each region separately.
3. RESULTS
3.1. Demographic characteristics of the samples
A total of 1306 participants were included in the analysis; 69.2% identified as female, 30.6% as male. Age ranged from 18 to 85 years (mean=35.3, SD=14). Of the participants, 66.1% had a college degree or higher level of education. 58.1% were never married, divorced or widowed and 40.7% married or cohabiting with a partner. Most of the participants (79.9%) were living with others at the time of the survey, and 58.1% were employed.
With respect to concerns about COVID-19, 72.5% expressed moderate (41.8%) or extreme (34.3%) concerns and 2.4% expressed no concern.
There were significant regional differences in all demographic categories including age (F(3,1302)=37.43, p<0.001, ηp=0.08), sex (χ2=50.9, df=3, p<0.001, education (χ2=114.4, df=3, p<0.001), employment (X2=193.77, df=3, p<0.001), and living arrangement (χ2=185.98, df=6, p<0.001). In addition, there were significant regional differences with regard to overall concern for COVID-19, (F(3, 1300)=37.02, p<0.001, ηp=0.08). See Table 1 for more details.
Table 1.
Demographic characteristics of the sample by region and total.
| USA | Korea | France | Hong Kong | Total | |
|---|---|---|---|---|---|
| n=334 | n=395 | n=145 | n=432 | n=1306 | |
| Age | 38.4 (16.9) | 31.8 (12.3) | 43.8 (15.1) | 33.4 (10.6) | 35.3 (14.0) |
| Sex (F/M) | 254/78 | 286/109 | 118 /27 | 246/186 | 904/400 |
| Education | |||||
| Secondary or lower | 65 | 212 | 38 | 126 | 441 |
| Bachelor's degree or higher | 269 | 175 | 107 | 306 | 857 |
| Employed (Y/N) | 239/95 | 120/275 | 120/25 | 280/152 | 759/547 |
| Living Arrangement | |||||
| Married/Partnered | 172 | 118 | 98 | 143 | 531 |
| Singles living alone | 82 | 97 | 34 | 37 | 250 |
| Singles living with family | 80 | 180 | 13 | 252 | 525 |
| Concern for COVID19 | |||||
| No Concern | 1 | 8 | 17 | 5 | 31 |
| Somewhat Concerned | 61 | 90 | 61 | 67 | 279 |
| Moderately Concerned | 146 | 168 | 48 | 184 | 546 |
| Extremely Concerned | 124 | 129 | 19 | 176 | 448 |
In an exploratory analysis we investigated regional differences in the individual variables that defined the psychological distress score. There were significant regional differences in several of the psychological distress variables including self-reported overall health, days physical health not good, days mental health not good, days feeling worried or anxious as well as DASS subscales for depression, anxiety, and stress. There were no regional differences in days usual activities affected by physical or mental health, or days affected by pain. See Table 2 for regional comparisons.
Table 2.
Mean (SD) of individual items among regions that make up the psychological distress score, loneliness, and social network diversity and number of people in network. ANCOVA comparisons included covariates for age, sex, education, employment, living arrangement and concern for COVID-19.
| USA | South Korea | France | Hong Kong | Total | Regional Comparison* | |
|---|---|---|---|---|---|---|
| n=334 | n=395 | n=145 | n=432 | n=1306 | ||
| Self-Reported Health | 2.28 (0.85) | 2.94 (0.93) | 2.54 (0.93) | 2.90 (0.97) | 2.71 (0.98) | F(3, 1249)=38.95,p<0.001, ηp=0.08 |
| Days physical health not good | 3.62 (6.72) | 4.02 (5.57) | 4.75 (7.70) | 4.77 (6.85) | 4.23 (6.56) | F(3, 1248)=2.99, p=0.03, ηp=0.01 |
| Days mental health not good | 8.33 (8.28) | 6.74 (7.97) | 6.03 (7.94) | 11.5 (9.79) | 8.58 (8.91) | F(3, 1248)=22.48, p=0.001, ηp=0.06 |
| Days usual activities affected by physical and mental health | 6.32 (6.50) | 6.50 (6.71) | 5.76 (6.02) | 5.14 (6.21) | 5.94 (6.44) | F(3, 1239)=1.44, p=0.23, ηp=0.01 |
| Days usual activities affected by pain | 2.20 (5.22) | 2.62 (5.32) | 2.10 (5.00) | 1.86 (4.48) | 2.21 (5.01) | F(3, 1247)=0.88, p=0.47, ηp=0 |
| Days feeling worries, anxious, or tense | 12.7 (9.95) | 7.41 (8.89) | 8.55 (8.55) | 14.22 (10.8) | 11.1 (10.2) | F(3, 1246)=28.57, p=0.001, ηp=0.08 |
| DASS Depression | 8.96 (9.28) | 11.7 (9.92) | 8.85 (8.79) | 15.1 (11.0) | 11.7 (10.3) | F(3, 1230)=19.27, p=0.001, ηp=0.06 |
| DASS Anxiety | 5.68 (6.39) | 7.39 (7.21) | 4.96 (6.11) | 9.46 (7.97) | 7.29 (7.31) | F(3, 1230)=12.26, p=0.001, ηp=0.05 |
| DASS Stress | 13.2 (9.41) | 12.2 (9.06) | 10.7 (9.36) | 16.0 (9.53) | 13.5 (9.50) | F(3, 1230)=9.39, p=0.001, ηp=0.04 |
| UCLA Loneliness | 41.2 (11.0) | 43.3 (12.5) | 35.8 (11.8) | 49.7 (10.5) | 43.8 (12.3) | F(3, 1217)=44.6, p=0.001, ηp=0.13 |
| Diversity of Social Networks | 4.17 (1.57) | 4.46 (2.03) | 6.35 (1.72) | 4.93 (1.80) | 4.74 (1.92) | F(3, 1214)=57.3, p=0.001, ηp=0.12 |
| Number of people in social networks | 14.0 (6.58) | 13.5 (8.58) | 21.4 (9.39) | 8.67 (7.14) | 12.9 (8.61) | F(3, 1282)=81.2, p=0.001, ηp=0.18 |
3.2. Predictors of psychological distress among geographic regions
There was a significant difference in the psychological distress score among regions (F(3, 1283)=15.92, p<0.001, ηp=0.05). Post hoc testing using a Tukey HSD correction for multiple comparisons showed that people in Hong Kong reported worse psychological distress compared to the USA, South Korea, and France (all p-values<0.001). There were no significant differences in psychological distress scores among the USA, South Korea, and France (all p-values>0.05).
Model comparison indices showed that there was a significant difference between the base model with only demographic variables and the second model including both demographic variables and loneliness F(4, 1189)=99.84, p < 0.001, R2=0.35, ΔR2=21.5%, AIC=7658.41. There were no differences between the second model and the third model which included demographic, loneliness, and social network variables F(8, 1181)=0.51, p=0.85, R2=0.35, ΔR2=0.21%, AIC=7670.22. This suggests that differences in social network between regions did not significantly improve the variance explained by demographic and loneliness variables. Coefficients in model 2 suggest that there were differential effects between regions in terms of age, employment, living arrangement, and loneliness. Younger age (β=−0.13, t=−2.98, p=0.002), greater concern for COVID-19 (β=0.15, t=3.01, p=0.003), and greater feelings of loneliness (β=−0.23, t=8.20, p < 0.001) were significant predictors across regions. See Table S1 for more information.
In the USA, younger age (β=−0.18, t= −5.58, p < 0.001) and unemployment (β=−0.10, t= −1.98, p=0.049) was related to more psychological distress. Married/partnered people reported less psychological distress compared to singles living alone (β=0.10, t=1.98, p=0.049). There were no differences between singles living alone and living with family (β=0.01, t=0.22, p=0.83). Greater concern for COVID-19 was associated with more psychological distress (β=0.16, t=3.22, p=0.001) as was more loneliness (β=0.42, t=8.77, p < 0.001). Sex and education were not significant predictors of psychological distress in the USA.
In South Korea, female sex (β=0.16, t=3.95, p < 0.001), greater concern for COVID (β=0.11, t=2.78, p=0.006), and greater loneliness (β=0.60, t=15.05, p < 0.001) predicted worse psychological distress. Age, education, employment, and living arrangement were not significant predictors.
In France, younger age (β=−0.37, t=−4.83, p < 0.001), greater concern for COVID-19 (β=0.30, t=4.04, p < 0.001), and loneliness (β=0.18, t=2.40, p=0.02) were significant predictors of greater psychological distress. Unemployment was marginally related to greater psychological distress. Sex, education, and living arrangement were not significant predictors of psychological distress in France.
In Hong Kong, greater concern for COVID-19 (β=0.27, t=6.07, p < 0.001) and loneliness were significant predictors of psychological distress. Age, sex, education, employment, and living arrangement were not significant predictors of psychological distress in Hong Kong.
4. DISCUSSION
The current findings highlight the complexity of psychosocial responses to COVID-19 in four regions of the world (USA, South Korea, France, and Hong Kong). Our model comparison approach suggests that demographic characteristics and loneliness but not social network index (diversity and size) predict psychological distress although there are differential effects among the regions in the degree to which age, employment status, living arrangement, and loneliness play a factor. Across samples, younger age, greater concern for COVID-19, and greater loneliness predict worse psychological distress. In the USA, multiple factors predict psychological distress including age, employment, living arrangement (married vs single), concern for COVID-19, and loneliness. In South Korea, female sex, concern for COVID-19, and loneliness predicted psychological distress. In France, age, greater concern for COVID-19, and loneliness were significant predictors. And in Hong Kong, where psychological distress is greatest, only concern for COVID-19 and loneliness predicted psychological distress.
Pandemics of the 20th and early 2st century have shaped response to the current COVID-19 pandemic. Summarizing influenza pandemics of the 20th century, Kilbourne noted that “all pandemics are different” and responses to pandemic have varied across the world (Kilbourne, 2006). It is important to point out that people in Hong Kong, many of whom experienced the SARS epidemic, reported the worst psychological distress and highest amounts of loneliness despite avoiding a complete lockdown. Concern for COVID-19 was uniformly high for people in the USA, Korea, and Hong Kong; people in France reported less concern than the other regions (see Table 1). The magnitude of concern for COVID-19 is somewhat incongruent with the rates of total cases and deaths due to the virus during the study timeframe (see Figure 3). The number of cases and deaths were higher in the USA and France than in Asian countries which did not institute complete lockdowns. The psychological distress of people in Hong Kong during the initial phases of COVID-19 could also be associated with the social unrest in the city (Tso and Park, 2020). Arguably, France had stringent lockdowns that required individuals to only leave their homes on essential errands and required signed documents for traveling. The USA, in contrast, had varying levels of lockdowns from state to state with variable compliance and timing. France and USA had similar levels of psychological distress to South Korea, suggesting that the policies toward lockdowns may not be the primary explanation for people’s psychological distress. Rather, it is likely that the downstream disruptions to people’s livelihoods and plans for the future have more impact on psychological distress.
Figure 3:
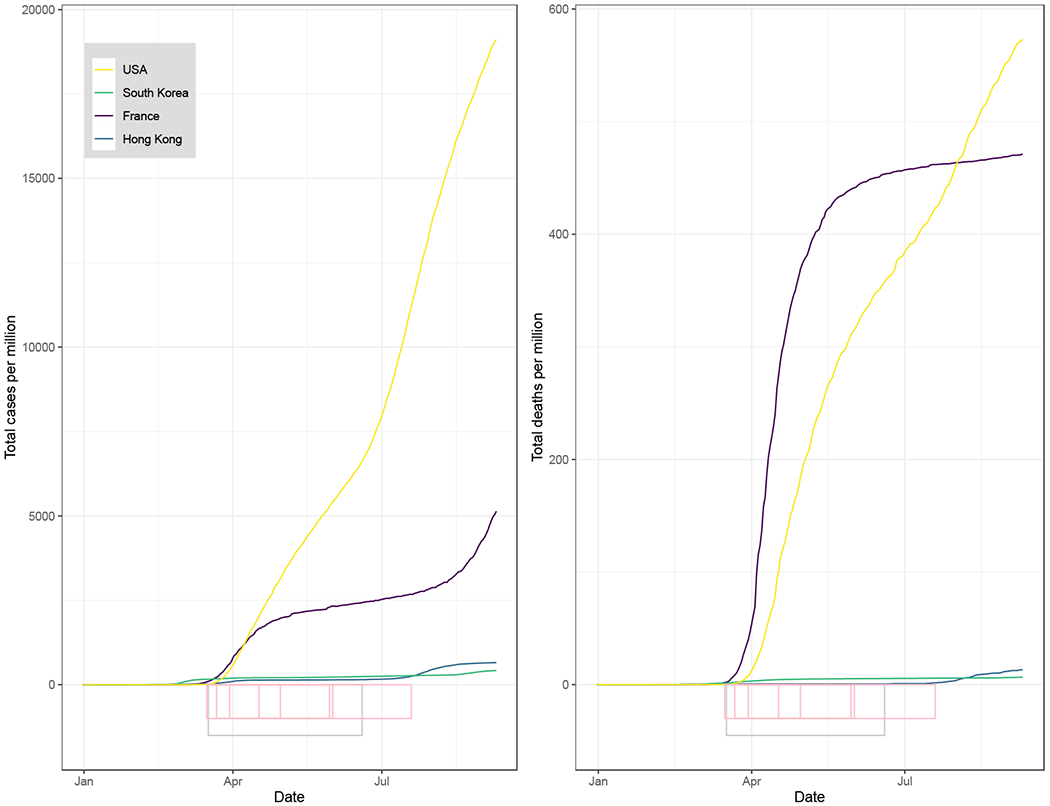
Data from ourworldindata.org and data.gov.hk showing the total number of cases and total deaths from COVID-19 during the initial phase of pandemic. The approximate dates of lockdowns in the USA and France are noted on the x-axis using a grey bar. The dates of data collection for each region are noted on the x-axis using pink bars.
Across the regions studied, younger age was associated with worse psychological distress. Surveys of college students have noted that economic effects of the COVID-19 pandemic, changes in daily life, and delays of academic achievement are associated with greater anxiety (Cao et al., 2020). Disruption to daily life has been cited as an important contributor to psychological wellbeing early in the course of the pandemic (Tull et al., 2020). It is possible that younger people may not have acquired all of the skills to cope with the uncertainty that the pandemic has caused, may feel powerless to change their circumstances because they are dependent on others (e.g., local and state officials, academic administrators, parents) and may be worried about not achieving important milestones including entry into the workforce. While younger people do not seem to be at substantially greater risk of health problems due to COVID-19, the disruption to their lives and resulting mental health crises may be an important factor to consider in helping young people learn to cope and emerge after the pandemic.
The economic effects of the pandemic will be felt for a long time to come. Unemployment and being single is a significant predictor of worse psychological distress across the four regions studied. Unemployment is an important predictor of mental health, and epidemiologists have suggested that the unemployment resulting from COVID-19 could result in an increase from 2135 to 9570 suicides worldwide this year (Kawohl and Nordt, 2020). Having a strong social support system and a spouse or partner can be protective of wellbeing (Soulsby and Bennett, 2015). The current results suggest that being married may be associated with better wellbeing than being single and living with family, suggesting that during COVID-19, intimate relationships may provide more support than other social relationships. Loneliness is also a strong predictor of greater psychological distress, and in previous work by our group, loneliness accounted for a large proportion of the variance in psychological health in both South Korean and Hong Kong samples (Lee et al., n.d.; Tso and Park, 2020). Here we re-iterate that it seems like the quality of relationships has mattered more during the pandemic than the quantity of relationships, especially as the number of social roles or people in social networks does not predict psychological distress in any of the regions studied or across the entire sample. Arguably, when people are constrained at home due to the pandemic, being single and living alone may become a more salient indicator of social isolation and a more serious risk factor for mental illness than social network size or diversity.
There are several strengths and limitations of the current study. First, it is cross sectional and the people samples for this study responded during the initial phases of the pandemic. It is not possible to know if their psychological distress persisted, or if changes during the summer produced a different outcome. The sampling strategy employed email lists to academic institutions and colleagues, which may have biased some of the results towards people who have a higher levels of education and economic security. We tried to mitigate this by employing a variety of sampling methods (e.g., social media, internet forums) but work in larger samples should attempt to contact people at all levels of income and education. We also did not collect information about pre-existing mental health problems; it is difficult to know whether the values reported here are similar to baseline or reflect changes due to COVID-19. However, published data on DASS prior to 2020 indicate that psychological distress and loneliness is higher during COVID-19. For example, 27% of college students report moderate or greater depression, 47% report moderate or worse anxiety, and 27% report moderate or worse stress (Bayram and Bilgel, 2008). In our sample, 34% of respondents report moderate or greater depression, 24% reported moderate or worse anxiety, and 25% moderate or worse stress suggesting that the prevalence of depression may be elevated in this sample. Normative studies of the UCLA loneliness for respondents 16-89 years of age note that average total loneliness score is approximately 35. In our sample, 68.52% of respondents report a UCLA loneliness score greater than 35 suggesting that this sample is overwhelmingly lonely. Furthermore, with the exception of France, respondents in the USA, South Korea, and Hong Kong report an average loneliness score of 41.2, 43.3, and 49.7, respectfully (Knight et al., 1988). To that point, the results from France should be approached with some caution, as the sample had a fairly high number of social contacts and a recent preprint of a sample in France found UCLA loneliness scores (M=41.71, SD=8.87) from otherwise healthy individuals that were more in line with those of the current sample from the USA, South Korea, and Hong Kong (Bortolon et al., 2020).
To summarize, significant regional differences in one mental health outcome, psychological distress, were observed. Residents of Hong Kong endorsed the most psychological distress compared with the residents of South Korea, USA, and France, possibly due to the combined effects of the pandemic and social unrest. However, there were also commonalities across the four countries. Youth, greater concern for COVID, and greater loneliness predicted worse psychosocial distress, although the magnitudes of the effects were not uniform among the four countries. Social unrest, economic uncertainty, and loss of regular routine during the pandemic may contribute significantly to deteriorating mental health. These findings underscore the need to allocate social support for individuals who may be at heightened risk for psychiatric disorders during a global pandemic. Importantly, the central role of loneliness in the deterioration of mental health suggests that societal efforts to reduce loneliness may be the most effective way to battle the impending epidemic of mental illness worldwide.
Supplementary Material
Figure 1.
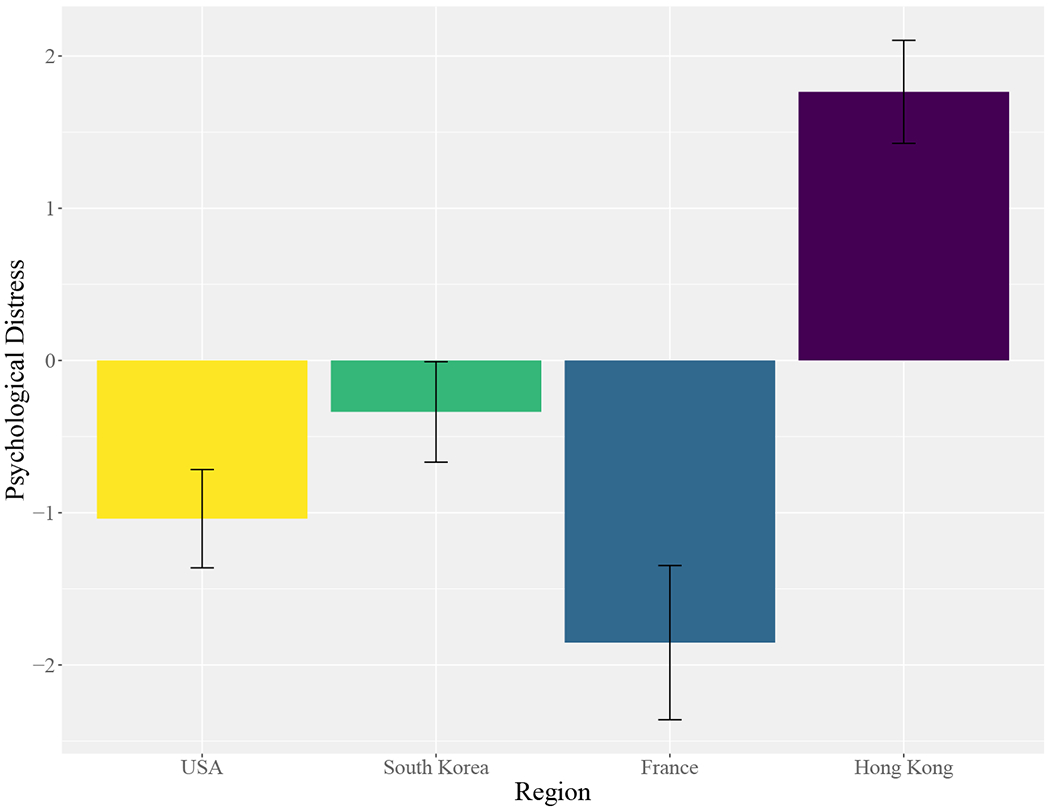
Comparisons of psychological distress among regions. The psychological distress variable was created by transforming individual items measuring general health, psychological health, and DASS subscales into a z-score and then summing those measures. Error bars represent standard error of the standardized psychological distress score.
Figure 2.
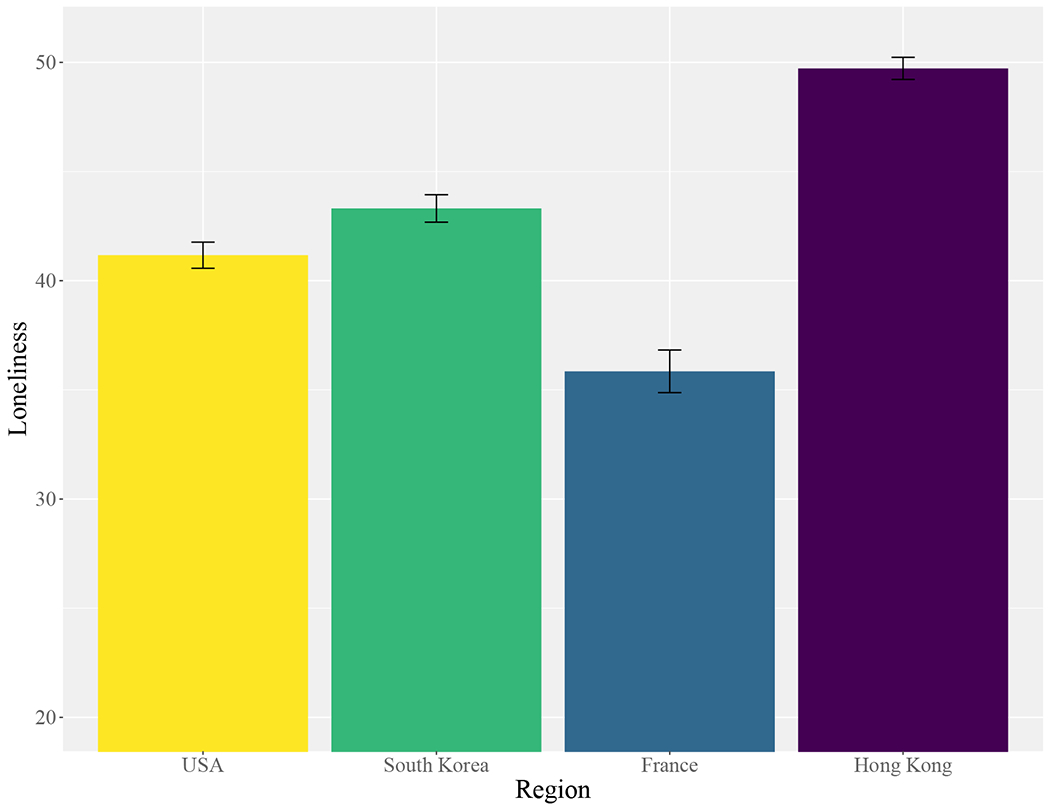
Comparisons of the UCLA Loneliness total score among USA, Korea, France and Hong Kong. Error bars represent standard error.
Acknowledgments
We would like to thank the anonymous respondents of this survey for their time and attention. We would also like to thank the Vanderbilt Institute for Clinical and Translational Research (VICTR) for making REDCAP available to distribute this survey.
5. REFERENCES
- Badcock JC, Adery LH, Park S, 2020. Loneliness in psychosis: A practical review and critique for clinicians. Clin. Psychol. Sci. Pract. 10.1111/cpsp.12345 [DOI] [Google Scholar]
- Bayram N, Bilgel N, 2008. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc. Psychiatry Psychiatr. Epidemiol. 43, 667–672. 10.1007/s00127-008-0345-x [DOI] [PubMed] [Google Scholar]
- Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, Wu X, Xiang YT, 2020. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 1–2. 10.1017/S0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolon C, Capdevielle D, Dubreucq J, Raffard stéphane, 2020. Persecutory ideation and anomalous perceptual experiences in the context of the COVID-19 outbreak in France: what’s left one month later? 10.31234/osf.io/f8gxk [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT, 2015. Loneliness: Clinical Import and Interventions. Perspect. Psychol. Sci. 10, 238–249. 10.1177/1745691615570616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J, 2020. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287, 112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B, Delamon G, Guillemasse A, Brouard B, Bibault J-E, 2020. Psychological Distress during the COVID-19 pandemic in France: a national assessment of at-risk populations. medRxiv 2020.05.10.20093161. 10.1101/2020.05.10.20093161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, 1997. Social Ties and Susceptibility to the Common Cold. JAMA J. Am. Med. Assoc. 277, 1940. 10.1001/jama.1997.03540480040036 [DOI] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, Rajaratnam SMW, 2020. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR. Morb. Mortal. Wkly. Rep. 69, 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao W, Ping S, Liu X, 2020. Gender differences in depression, anxiety, and stress among college students: A longitudinal study from China. J. Affect. Disord. 263, 292–300. 10.1016/j.jad.2019.11.121 [DOI] [PubMed] [Google Scholar]
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Worthman CM, Yardley L, Cowan K, Cope C, Hotopf M, Bullmore E, 2020. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Robles TF, Sbarra DA, 2017. Advancing social connection as a public health priority in the United States. Am. Psychol. 72, 517–530. 10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husky MM, Kovess-Masfety V, Swendsen JD, 2020. Stress and anxiety among university students in France during Covid-19 mandatory confinement. Compr. Psychiatry 102, 152191. 10.1016/j.comppsych.2020.152191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawohl W, Nordt C, 2020. COVID-19, unemployment, and suicide. The Lancet Psychiatry 10.1016/S2215-0366(20)30141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne ED, 2006. Influenza pandemics of the 20th century. Emerg. Infect. Dis. 10.3201/eid1201.051254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight RG, Chisholm BJ, Marsh NV, Godfrey HPD, 1988. Some normative, reliability, and factor analytic data for the revised UCLA Loneliness scale. J. Clin. Psychol. 44, 203–206. [DOI] [PubMed] [Google Scholar]
- Lee H. (Hanson), Dean D, Baxter T, Griffith T, Park S, n.d. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. 10.31234/OSF.IO/S7QJ8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH, 1995. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 33, 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL, 2009. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 31, 318–326. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, 1996. UCLA Loneliness Scale (Version 3): Reliability,Validity, and Factor Structure. J. Pers. Assess. 66, 20–40. 10.1207/s15327752jpa6601 [DOI] [PubMed] [Google Scholar]
- Soulsby LK, Bennett KM, 2015. Marriage and Psychological Wellbeing: The Role of Social Support. Psychology 6, 1349–1359. 10.4236/psych.2015.611132 [DOI] [Google Scholar]
- Taouk Moussa M, Lovibond PF, Laube R, 2001. Psychometric Properties of a Chinese Version of the 21-Item Depression Anxiety Stress Scales (DASS21). Sydney, Australia. [Google Scholar]
- Tso I, Park S, 2020. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: A case study of Hong Kong. Psychiatry Res. 293, 113423. 10.31234/osf.io/wv9y2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL, 2020. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 289, 113098. 10.1016/j.psychres.2020.113098 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


