Abstract
Background
Measurement of bone mineral density is widely used to diagnose osteoporosis. The objectives of this study are to determine how bone densitometry affects subsequent treatment of osteopenia and osteoporosis with either hormone replacement therapy or bisphosphonates and to examine clinical factors associated with starting either therapy after bone densitometry.
Methods
We conducted a prospective study involving women over 50 years of age who were referred to a tertiary care hospital for the first time to undergo bone density measurement using dual-energy x-ray absorptiometry (DXA). Baseline clinical data were collected through face-to-face interviews before the test. Subsequently, the scans were reviewed and categorized as showing no bone loss, osteopenia or osteoporosis, based on World Health Organization criteria. Three months after DXA, subjects were contacted by telephone to determine their understanding of the test results and any new treatments started or recommended since the scan.
Results
Of 383 women recruited at the time of their DXA, 335 (87.5%) completed the 3-month follow-up. Among those reached at follow-up, DXA results showed no bone loss in 119 (35.5%), osteopenia in 137 (40.9%) and osteoporosis in 79 (23.6%). The proportion of subjects with osteoporosis receiving either hormone replacement therapy or bisphosphonate therapy was 15.2% before the test, increasing to 63.3% after the scan. The following factors were independently associated with the initiation of either therapy: actual DXA result showing osteoporosis (odds ratio [OR] 7.2; 95% confidence interval [CI] 1.7–30.3), compared with a normal scan; subjects' perception that their scan showed bone loss (osteopenia or osteoporosis) (OR 13.5; 95% CI 4.0–45.5) or that they were unclear about the results (OR 5.4; 95% CI 1.6–18.8), compared with the perception that the results were normal; and discussion of the DXA results with a physician (OR 5.5; 95% CI 1.9–16.0).
Interpretation
The proportion of women with osteoporosis receiving hormone replacement therapy or bisphosphonate therapy increases after diagnosis with densitometry. However, communication by physicians so that patients understand their test results is a critical component in the initiation of therapy after bone densitometry.
Osteoporosis is estimated to develop in 1 out of 4 women over the age of 50 years.1 Measurement of bone mineral density (BMD) is widely used to diagnose osteoporosis.2 However, the usefulness of bone densitometry relates directly to how the information obtained from the test affects management.
Earlier investigations showed that densitometry influenced patients' and physicians' decisions about therapy for osteoporosis.3,4,5,6,7,8,9 However, these trials were limited by retrospective study designs,3,7,8 they examined only the use of hormone replacement therapy (HRT) and not bisphosphonates,4,5,8 and they did not analyze factors other than BMD that may have influenced therapeutic choices.5,6,9
To address these issues, we conducted a prospective study involving women referred for the first time to undergo dual-energy x-ray absorptiometry (DXA) in order to determine how the test affects subsequent treatment of osteopenia and osteoporosis with either HRT or bisphosphonates and to examine clinical factors associated with starting either therapy after the scan.
Methods
This study was approved by the Ottawa Hospital Research Ethics Board. We identified all consecutive women over the age of 50 years scheduled to undergo an outpatient DXA scan at the Civic Site of The Ottawa Hospital between July 1 and Aug. 31, 1998. Only subjects for whom this was their first DXA scan were eligible. We excluded women who were unable to communicate in English or who did not provide informed consent.
Each woman was interviewed before their DXA scan by a research assistant (M.H.) using a questionnaire. Information was obtained in the following categories: demographic data (age, race and education level); referring physician who ordered the test; medication use (estrogen, bisphosphonates [alendronate or etidronate], calcitonin, fluoride, calcium preparations, vitamin D, prednisone [>> 6 months] and phenytoin [ever]); medical history (breast cancer, other cancers, diabetes mellitus, arthritis, cardiovascular disease, pulmonary problems, renal disorders, gastrointestinal illness and thyroid conditions); and osteoporotic risk factors (age at menarche [>> 12 years], menopause before age 45 years, pregnancy history and family history of osteoporosis). A history was elicited of falls and hip, wrist or vertebral fractures in the year before the scan. Information was also obtained about the subjects' habits and categorized as follows: smoking history greater than 20 cigarette pack-years, consumption of more than 7 alcoholic beverages per week, consumption of more than 20 cups of coffee per week, exercise at least 3 times per week and estimated dietary intake of more than 5.6 g of calcium per week. Women were asked to rate their health as excellent, good, fair or poor; results were classified into 2 groups (excellent and good v. fair and poor). Height and weight were measured at the time of the scan.
The nuclear medicine reports of all DXA scans were reviewed by one of us (N.S.F.). The reports included T scores (values for BMD given as the number of standard deviations [SDs] below the mean for young adult women) and Z scores (the number of SDs below the mean for women of the same age). The DXA results were categorized on the basis of T scores using WHO criteria10,11,12 as follows: osteoporosis (a value for BMD more than 2.5 SDs below the mean for young adult women), osteopenia (a value for BMD between 1.0 and 2.5 SDs below the mean) or normal (a value for BMD not more than 1.0 SD below the mean).
Subjects were contacted by telephone about 3 months after their DXA scan by 1of 2 research assistants unfamiliar with the scan results. Subjects were asked if they had discussed the test results with the referring physician. The subjects' understanding of the results was categorized as follows: normal (no bone loss), bone loss (osteoporosis or osteopenia) or unclear about the findings. Subjects were asked whether there had been any changes in their medications (specifically the initiation of HRT or bisphosphonate therapy with either alendronate or etidronate) subsequent to the scan.
The frequencies of categorical variables and the mean age (and SD) of subjects were determined. To determine factors associated with the initiation of either HRT or bisphosphonate therapy (dependent variable) after the DXA scan, only subjects who were not taking either of these medications before their scan were included in the analyses. Factors considered a priori to be possibly associated with the initiation of treatment included DXA scan result, communication with their physician about the result, category of referring physician (family physician v. specialist), age (dichotomized by median), race (white v. other), height (< 164 cm), weight (< 55 kg), education (>> high school), self-rated health, fracture history, falls, comorbid illness, previous refusal or intolerance of estrogen or bisphosphonate therapy, history of breast cancer and osteoporosis risk factors. Bivariate analyses using χ2 tests and unadjusted logistic regression were conducted to determine the association of these individual factors with the initiation of either HRT or bisphosphonate therapy. Factors significantly associated with the initiation of therapy in the bivariate analyses (p < 0.05) were entered into a stepwise logistic regression model. Odds ratios and confidence intervals were derived from these analyses.
Results
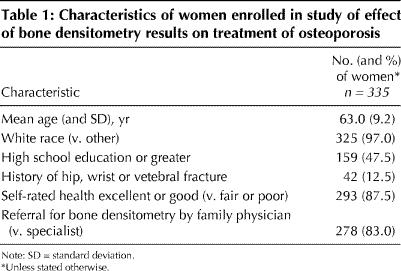
Of the 383 women recruited at the time of their DXA, 335 (87.5%) completed the questionnaire at the 3-month follow-up. The reasons for loss to follow-up included refusal to answer the questionnaire (n = 6) and inability to contact the subject (n = 42). Subjects lost to follow-up did not differ significantly from those contaced with respect to age, race, education level, osteoporosis risk factors and BMD (data not shown). The characteristics of the 335 women who completed the follow-up questionnaire are shown in Table 1.
Table 1
Of the women who were reached at follow-up, 79 (23.6%) had DXA results showing osteoporosis, 137 (40.9%) osteopenia and 119 (35.5%) no bone loss (Table 2). Of the women with osteopenia, 29.2% were receiving HRT or bisphosphonate therapy before the scan, compared with 37.9% after the scan. The proportion of subjects with osteoporosis taking either therapy was 15.2% before and 63.3% after the scan. There was a relatively greater increase in the use of bisphosphonates (particularly etidronate) compared with HRT among women with osteoporosis and osteopenia.
Table 2
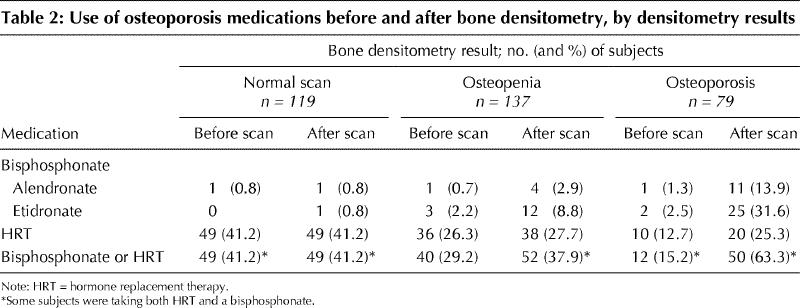
Table 3 shows the bivariate analyses of factors associated with starting HRT or bisphosphonate therapy after DXA among the 234 subjects who were not taking these medications at baseline. The following factors were significantly associated with initiation of therapy: actual DXA result showing osteopenia or osteoporosis, compared with a normal scan; subjects' perception that their scan showed bone loss (osteopenia or osteopenia) or that they were unclear about the results, compared with the perception that the results were normal; discussion of the DXA results with a physician; height less than 164 cm; and a history of wrist, hip or vertebral fractures.
Table 3
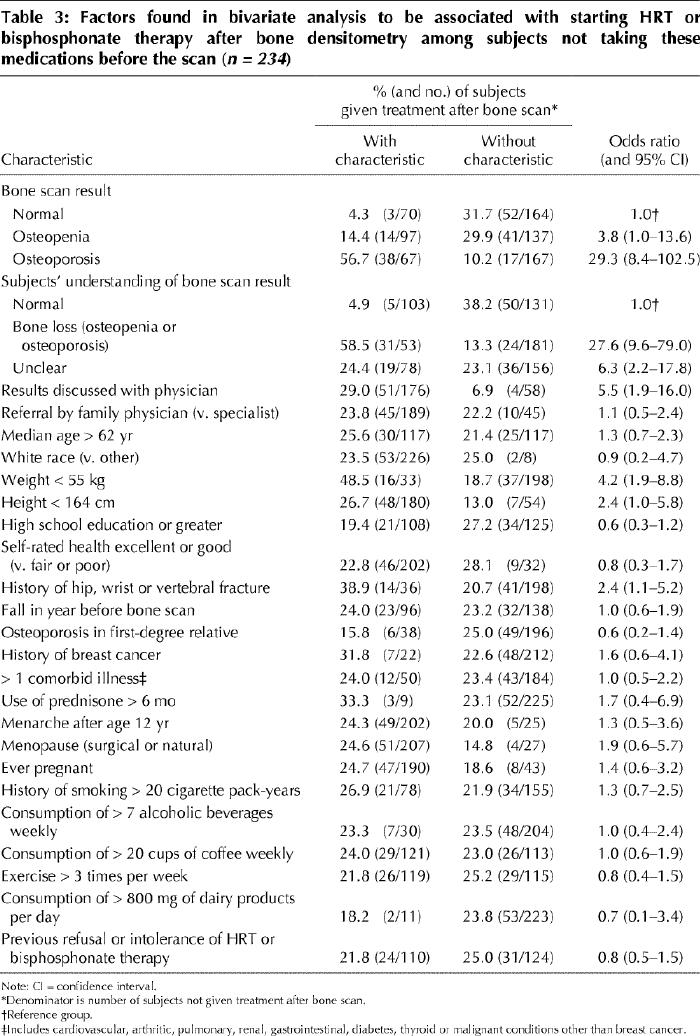
In the multivariate model the following factors remained independently associated with initiation of therapy: actual DXA result showing osteoporosis (odds ratio [OR] 7.2; 95% confidence interval [CI] 1.7–30.3), compared with a normal scan; subjects' perception that their scan showed bone loss (osteopenia or osteoporosis) (OR 13.5; 95% CI 4.0–45.5) or that they were unclear of the results (OR 5.4; 95% CI 1.6–18.8), compared with the perception that the results were normal; and discussion of the DXA results with a physician (OR 5.5; 95% CI 1.9–16.0).
Fig. 1 illustrates the association between the actual DXA results and the subjects' perception of the results. None of the subjects with a normal scan thought that they had osteopenia or osteoporosis. Only 6.4% of the women found to have osteoporosis thought that they had normal scans. The greatest disparity was among subjects with osteopenia, among whom 24.2% perceived that they had some bone loss, 25.1% were unclear about the results, and 51.0% thought that their scan was normal.
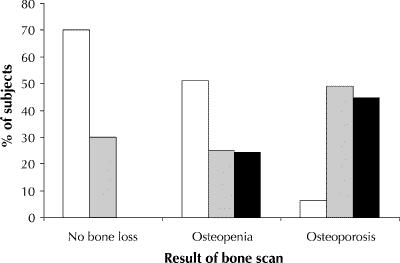
Fig. 1: Subjects' perception of bone densitometry results compared with actual results. Actual results are categorized as no bone loss, osteopenia or osteoporosis. In each category, bars represent the proportion of subjects who perceived that their scan was normal (white bars), who were unclear about the scan result (grey bars) or who perceived that their scan showed bone loss (osteopenia or osteoporosis) (black bars).
Additional analyses revealed that, among the 67 subjects with osteoporosis who were not taking HRT or bisphosphonate therapy before the scan, the proportion of subjects initiating either therapy afterward was significantly less among those who were either unclear about their test results or thought that the result was normal (46.0% [17/37]) than among those who understood that they had osteoporosis (70.0% [21/30]) (p = 0.05).
Interpretation
Our findings demonstrate that DXA scans do influence the management of osteoporosis. Only 15.2% of the subjects with osteoporosis were receiving HRT or bisphosphonate therapy before the scan, compared with 63.3% after the test. Nevertheless, one third of the subjects with osteoporosis were not receiving either therapy at the 3-month follow-up. Three factors were independently associated with starting therapy: the actual bone scan result, the subjects' understanding of the results and discussion of the results with their physician. These findings underscore 2 important concepts. First, communication between physicians and patients is critical to therapeutic decision-making. Second, it is important that physicians not merely tell their patients results but that they also facilitate an understanding of the results.
Our finding that a diagnosis of osteoporosis by DXA increases the proportion of women receiving appropriate treatment supports the results of previous investigations.3,7,8 Coupland and associates7 reported that the proportion of patients with osteoporosis receiving therapy significantly increased after diagnosis in a specialized clinic where work-up included a DXA scan. However, it is difficult to discern whether their findings were due to the test results specifically or to the attention received at a specialized clinic. The majority of referrals in our study were made by family physicians, which suggests that DXA can influence treatment beyond the setting of a specialty clinic.
Our study adds to a growing body of evidence that patients' understanding of their BMD increases their acceptance to initiate HRT,3,4,5,6,9 and it extends this knowledge to bisphosphonates. Torgerson and colleagues5 randomly assigned women to receive either screening DXA or no DXA. At the 2-year follow-up, more of the women who underwent DXA than of those who did not undergo DXA were receiving HRT. Most recently, a prospective cohort study involving 37 postmenopausal women evaluated the effect of an education kit supplemented by knowledge of bone densitometry on the decision to start HRT. After the educational component 24% of the women with low BMD requested HRT; this proportion increased to 38% after the women were informed of their DXA results.11
Our study provides additional information regarding the type of treatment chosen for osteoporosis after bone densitometry. The majority of the women with osteoporosis were given a bisphosphonate (in most cases etidronate) rather than HRT. The preference for etidronate over alendronate is likely attributed to the fact that only the former is covered under the Ontario drug plan. Interestingly, women found to have normal BMD had the highest proportion of HRT use; in theory, this could represent the protective effect of HRT on bone mass.
Our study has several limitations. The setting was a single teaching hospital, which may not be representative of other settings. In addition, we do not know how many of the subjects requested to have a DXA scan. These women may differ from those whose referral was initiated by their physician in their willingness to accept proposed treatment. The follow-up data relied solely on the subjects' reports; therefore, there may have been some inaccuracies with respect to their recall of the physicians' recommendations. The practitioners who ordered the test may not have been familiar with interpreting DXA reports or with management guidelines for osteoporosis.10,11,12 For example, we do not know whether they used the Z score or the T score in their decision-making. The study was conducted before the introduction of nasal calcitonin or raloxifene in the management of osteoporosis; therefore, we do not know the influence of DXA on these therapies. Finally, we did not assess the impact of DXA on nonpharmacological approaches to osteoporosis or on the use of calcium and vitamin D supplements.
The use of bone densitometry in the diagnosis of osteoporosis is firmly established. The test clearly can have a positive impact on the management of people with this condition. Physician–patient communication appears to be a critical component in using the information provided by this test to its full potential. Future research should focus on strategies aimed at maximizing accurate transfer of DXA results between practitioner and patient and on educational strategies that facilitate the patients' understanding of the test result.
Footnotes
This article has been peer reviewed.
Acknowledgements: This study was supported by a grant from Physicians Services Incorporated. Dr. Mitchell is a recipient of an Ontario Ministry of Health Career Scientist Award. Dr. Cranney is a recipient of the Arthritis Society Scholarship.
Competing interests: None declared.
Reprint requests to: Dr. Susan L. Mitchell, Hebrew Rehabilitation Center for Aged, 1200 Centre St., Roslindale MA 02131, USA; fax 617 363-8929
References
- 1.Melton LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective: How many women have osteoporosis? J Bone Miner Res 1992;7:1005-10. [DOI] [PubMed]
- 2.Sturtridge W, Lentle B, Hanley DA. Prevention and management of osteoporosis: consensus statements from the Scientific Advisory Board of the Osteoporosis Society of Canada. 2. The use of bone density measurement in the diagnosis and management of osteoporosis. CMAJ 1996;155(7 Suppl):924-9. Available: www.cma.ca/disease/osteo_p1/no2.htm [PMC free article] [PubMed]
- 3.Rubin SM, Cummings SR. Results of bone densitometry effect on women's decisions about taking measures to prevent fractures. Ann Intern Med 1992;116: 990-5. [DOI] [PubMed]
- 4.Silverman SL, Greenwald M, Klein RA, Drinkwater BL. Effect of bone density information on decisions about hormone replacement therapy: a randomized trial. Obstet Gynecol 1997;89:321-5. [DOI] [PubMed]
- 5.Torgerson DJ, Thomas RE, Campbell MK, Reid DM. Randomized trial of osteoporosis screening. Use of hormone replacement therapy and quality-of-life results. Arch Intern Med 1997;157:2121-5. [DOI] [PubMed]
- 6.Papaioannou A, Parkinson W, Adachi J, O'Connor A, Jolly EE, Tugwell P, et al. Women's decisions about hormone replacement therapy after education and bone densitometry. CMAJ 1998;159(10):1253-7. Abstract available: www.cma.ca/cmaj/vol-159/issue-10/1253.htm [PMC free article] [PubMed]
- 7.Coupland CA, Packham I, Lyons AR, Chilvers CE, Hosking DJ. The contribution of bone densitometry to the diagnosis and treatment of osteoporosis. Public Health 1997;111:191-4. [DOI] [PubMed]
- 8.Rozenberg S, Kroll M, Vandromme J, Paesmans M, Ham H. Effect of bone density evaluation on hormone replacement therapy prescription. Maturitas 1996;24:57-61. [DOI] [PubMed]
- 9.Marci CD, Viechnicki MB, Greenspan SL. Bone mineral densitometry substantially influences health-related behaviors of postmenopausal women. Calcif Tissue Int 2000;66:113-8. [DOI] [PubMed]
- 10.Scientific Advisory Board, Osteoporosis Society of Canada. Clinical practice guidelines for the diagnosis and management of osteoporosis. CMAJ 1996;155(8 Suppl):1113-33. Available: www.cma.ca/disease/osteo_p2/osteocpg.htm [PMC free article] [PubMed]
- 11.Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D. Guidelines for diagnosis and management of osteoporosis. The European Foundation for Osteoporsis and Bone Disease. Osteoporos Int 1997;7;390-406. [DOI] [PubMed]
- 12.Meunier PJ, Delmas PD, Eastell R, McClung MR, Papapoulos S, Rizzoli R, et al. Diagnosis and management of osteoporosis in postmenopausal women: clinical guidelines. International Committee for Osteoporosis Clinical Guidelines. Clin Ther 1999;21(6):1025-44. [DOI] [PubMed]


