Abstract
This study examined the impact of an existing 7-week summer learning program on children’s weight status and cardiorespiratory fitness (CRF).
Methods:
Using an observational repeated measures within-subjects design, children’s (N = 20 mean age = 6.35; 45% female; 80% African American) height, weight, and CRF (i.e., Fitnessgram PACER), were measured during the first and final week of the seven week program. Descriptive statistics were calculated for all variables. Median regression analysis examined estimated the differences in BMI zscore, overweight and obesity prevalence, and CRF during the first week (baseline) compared to the final week (outcome).
Results:
Of those enrolled initially in the program, 77% attended for more than 4 weeks. When controlling for attendance and sex, no statistically significant changes were observed for, median zBMI (pre: 0.12, post: 0.11) or CRF (pre: 10, post: 13.5 PACER laps). All children except for one maintained the same weight status (e.g. normal weight, overweight) from baseline to outcome. A total of 12 participants increased or maintained the number of PACER laps completed, while 8 participants’ PACER laps decreased.
Conclusion:
The results of this natural experiment provides preliminary evidence that participation in a structured summer program can potentially mitigate unhealthy weight gains and fitness loss over the summer for some children. Future studies with larger more representative samples are needed to establish the impact of structured summer programming on children’s CRF and weight status.
Keywords: Children, Weight, Fitness, Physical activity, Diet
1. Introduction
Childhood obesity has long been public health concern; with the prevalence of obesity among children aged 6–11 increasing over the last five decades.(Cunningham, Kramer, & Narayan, 2014) The prevalence of overweight/obesity is especially common among racial minorities. (Ogden, Lamb, Carroll, & Flegal, 2010; Stevens et al., 2017; Treviño et al., 2008) Overweight or obese children are more likely to develop non-communicable diseases, including high blood pressure, abnormal fasting glucose, insulin resistance, type 2 diabetes, sleep apnea, asthma, and joint problems,(Bacha & Gidding, 2016; Cote, Harris, Panagiotopoulos, Sandor, & Devlin, 2013; Mohanan, Tapp, McWilliams, & Dulin, 2014; Narang & Mathew, 2012; Pollock, 2015) children who are overweight or obese also more likely to become overweight/obese adults.(Serdula et al., 1993) Summer vacation has been identified as a period of accelerated weight gain and fitness loss.(Baranowski et al., 2014; Fu, Brusseau, Hannon, & Burns, 2017; Gutin, Yin, Johnson, & Barbeau, 2008; Moreno, Johnston, & Woehler, 2013; Sallis et al., 1997; von Hippel & Workman, 2016) Large-scale studies show that between kindergarten and second grade, U.S. children’s overweight and obesity prevalence increase during summer vacations.(von Hippel & Workman, 2016) These findings suggest that children who gain unhealthy weight during the summer may not subsequently lose that weight during the school year and that public health promotion efforts to reduce childhood obesity may be most effective if they target summer vacation.
The Structured Days Hypothesis (SDH) states that a structured day, defined as a pre-planned, segmented, adult-supervised compulsory environment (e.g., school day) protects children against engaging in obesogenic behaviors, and can ultimately prevent excessive weight gain. (Brazendale, Beets, Pate et al., 2017; Brazendale, Beets, Weaver et al., 2017) According to the SDH the lack of “structure” during the summer could be associated with an increase in obesogenic behaviors, which could lead to accelerated weight gain and losses in cardiorespiratory fitness (CRF) during the summer months.(Baranowski et al., 2014; Chen et al., 2016; Franckle, Adler, & Davison, 2014; McCue, Marlatt, & Sirard, 2013; Moreno et al., 2013; Von Hippel, Powell, Downey, & Rowland, 2007) Thus, recommendations to increase access to structured programming during the summer have been made, (Bohnert et al., 2017) with preliminary evidence showing this approach can be effective for adolescent children.(Park & Lee, 2015) To reduce practical and ethical concerns, natural experiments, where treatment and control groups are formed in ways that resemble random assignment have been employed to many scientific designs. (Lewis-Beck, Bryman, & Liao, 2003) The purpose of this natural experiment was to explore the impact of a 7 week structured summer learning program (SLP) on elementary children’s weight gain and fitness loss. We hypothesized that there would be no change in from week 1 to week 7 on any of the primary outcomes because the protective effect of the structured SLP on children’s obesogenic behaviors and in turn weight status and fitness. We also hypothesized that children would engage in more healthful behaviors on days that they attended the SLP because of its compulsory, restrictive, and positive environment.
2. Methods
2.1. Recruitment/participants
This study took place in one metropolitan city in the southeastern United States. Participating rising 1st and 2nd grade children were referred during the spring semester of their kindergarten or first grade years, by their classroom teachers to participate in a SLP because their reading proficiency was lower than their grade-level. Descriptive characteristics and demographics of participants in this study with full data are presented in Table 1. A total of 31 children (55.5% male) who were African American (n = 25), non-Hispanic White (n = 3), or of another race/ethnicity (n = 3) participated in the SLP. Children were 6.28 years (SD = 0.63 yrs.) old. Families were recruited to be a part of this study via parent brochures and an open house in which the researchers explained the goals, measurement protocols, and expectations of the study to parents. Inclusion criteria included parental consent and the child’s ability to wear accelerometer on their non-dominant wrist for multiple days without physical impediment. See Table 1 for details on participants individual and family demographics. Children who provided measurement at both baseline (week 1.) and outcome (week 7.) were included in the primary analyses.
Table 1.
Child and family-level demographics of participants in study (n = 20).
| Child-level | All (n = 20) | Boys (n = 12) | Girls (n = 8) |
|---|---|---|---|
| Mean | Mean | Mean | |
| Age - years, (± SD) | 6.4, (0.6) | 6.3, (0.5) | 6.4, (0.7) |
| African-American - n, (%) | 16, (80) | 9 (75) | 7, (88) |
| BMI Classification - n, (%) | |||
| Underweight | 1, (5) | 0, (0) | 1, (13) |
| Normal weight | 13, (65) | 12, (100) | 4, (50) |
| Overweight/Obese | 3, (15) | 0, (0) | 3, (38) |
| Missing | 3, (15) | 3, (100) | 0, (0) |
| Family-level | N | % |
|---|---|---|
| Parent/Guardian | ||
| Mother | 14 | 70 |
| Father | 3 | 15 |
| Missing | 3 | 15 |
| Education | ||
| No High School Diploma | 1 | 5 |
| High School Diploma | 4 | 20 |
| College Degree | 12 | 60 |
| Missing | 3 | 15 |
| Marital Status | ||
| Married | 9 | 45 |
| Single and Never Married | 5 | 25 |
| Widowed/Divorced/Separated | 2 | 10 |
| Other | 1 | 5 |
| Missing | 3 | 15 |
| Annual Household Income | ||
| $19,999 or less | 1 | 5 |
| $20,000 – $39,999 | 7 | 35 |
| $40,000 or more | 7 | 35 |
| Missing | 5 | 25 |
| No. of People in Household* | ||
| 3 or less | 3 | 15 |
| 4 or more | 14 | 70 |
| Missing | 3 | 15 |
| No. of Children in Household** | ||
| 2 or less | 9 | 45 |
| 3 or more | 8 | 40 |
| Missing | 3 | 15 |
SD = Standard Deviation, BMI = Body Mass Index.
Including respondent.
Including child participant.
2.2. Study design/procedure
Prior to enrolling participants in the study all protocols and procedures were approved by the lead author’s university institutional review board. This study is a seven-week natural experiment employing a repeated measures within-subjects design. The study took place in the summer (June and July) of 2017. Children’s baseline height, weight, and fitness levels were collected during the first and last week of the SLP. Children’s outcome height, weight, and fitness levels were collected in during last week of the SLP. Children’s physical activity, sleep, diet, and screen time behaviors were collected during the program (week two), and when the program was on a holiday break (week 4). For the purposes of this study, process outcomes included: PA, screen time, sleep, diet, and attendance.
2.3. Program description
The SLP was designed to close the achievement gap between high and low achieving students by providing structured reading opportunities during the summer for elementary students who were reading below grade level. The program was operated by a local community organization in collaboration with a local school district. As part of SLP, children participated in a daily (Monday to Thursday) academic achievement program at the school in which they were enrolled for 6 weeks during the summer. The SLP was a full-day (8:30 am-3:00 pm) program consisting of structured reading opportunities and lessons during the morning (8:30am-12:00pm). Children were allowed to arrive by 7:30am for a breakfast provided by the SLP. Children’s attendance was taken by the SLP staff upon arrival. As children arrived at the program, staff members recorded his/her attendance as the participants received their breakfast. The afternoon (12–3pm) scheduled approximately 30 min for lunch, followed by two hours of enrichment (e.g. social skills) and 60 min of physical activity (e.g. free play/recess). Reading opportunities and lessons were delivered by certified teachers employed by the school district. The enrichment and physical activity opportunities were delivered by employees of the local community organization. All children enrolled in the program were provided breakfast, lunch, and a snack, daily. All foods served at the SLP adhered to the USDA Summer Food Service Program Meal Patterns. (“United States Department of Agriculture Food & Nutrition Service, 2018)
2.4. Primary outcomes
2.4.1. Anthropometrics
Participants’ heights and weights were obtain using a digital scale (Healthometer model 500 K L, Healthometer, McCook, Ill.) and portable stadiometer (Model S100, Ayrton Corp., Prior Lake, Minn.). All weights were estimated to the nearest 0.1 lbs. while heights were estimated to the nearest 0.1 in. with children wearing light clothing and no footwear following standard protocols (Ogden, Carroll, Kit, & Flegal, 2012) All height and weight data were collected by trained research assistants under the guidance of the first author upon student arrival to the program. Height and weight data were converted into BMI and standardized (zBMI). Age and gender specific percentiles were then calculated using CDC growth charts. (Kuczmarski et al., 2002)
2.4.2. Fitness
Cardiorespiratory fitness (CRF) was measured using the 20-meter FitnessGram® Progressive Aerobic Cardiovascular Endurance Run (PACER) (Welk & Meredith, 2010) by trained research assistants under the guidance of the first author. The PACER was conducted outdoors on an open field at the school using audio played via a portable stereo. Twenty meters was marked using cones and each student was instructed to run from one cone to the other within a designated timeframe. The allotted time to run the 20 m decreased as students progressed through the PACER. If a student failed to complete the 20-meter distance within the allotted timeframe twice their test was complete and the lap upon which they failed to complete the 20-meter distance for the second time was recorded.
2.5. Process outcomes
2.5.1. Physical activity
Objective measures were used to capture children’s physical activity. A wrist worn activity monitor (Actigraph Link GT9X + accelerometer, Shalimar, FL) was worn for 6 weeks of the 7-week program. A trained research assistant placed the activity monitor on the child’s non-dominant wrist upon arrival to the SLP on each Monday morning of the observation week. Children were instructed to wear the water proof device at all times (day and night), including when sleeping, bathing, and swimming without removal for the following week. Devices from the previous week were collected prior to providing children with a new device each Monday. Epochs were set to five-second intervals to account for the transitionary physical activity patterns of children.(Chandler, Brazendale, Beets, & Mealing, 2016) Non-dominant wrist-based cut points of ≤ 161 and ≥ 530 accelerometer counts per five seconds were also used to distill sedentary time and moderate-to-vigorous physical activity (MVPA), respectively. (Chandler et al., 2016) A valid day of accelerometer wear was classified as ≥600 min per day (excluding sleep).(Cain, Sallis, Conway, Van Dyck, & Calhoon, 2013)
2.5.2. Screen time
Children’s screen time was assessed using self-report measures reported for two 7-day periods, one during the program (week two), and one during the holiday break (week four). Parents were asked to report on their child’s screen time on at least seven days including at least one weekend day. Parents were encouraged to complete the self-report measures with their child to enhance the accuracy of the estimates. Parent/children estimated the total amount of time (hours and minutes) spent in front of a screen that day (e.g., TV, computer, video game, smartphone, and tablet).(Eisenmann, Bartee, & Wang, 2002; Tandon et al., 2012) Hours were then converted to minutes, summed to provide total screen time for the entirety of the seven-day period. Average daily minutes was calculated by dividing the total screen time value by the number of days the daily diary was completed.
2.5.3. Sleep
Sleep time and quality were collected using the same wrist-worn accelerometers used for physical activity by following the same protocols. Proprietary ActiGraph sleep algorithms validated for children (Sadeh Algorithm) were used to determine total sleep duration.(Sadeh, 2011) Total sleep duration and individual files were reintegrated from five-second epochs to 60-second epochs and analyzed for inconsistencies with sleep duration, anything ≤ 4 and ≥ 15 h per night removed from further analysis based on previous literature.(Acebo et al., 1999)
2.5.4. Diet
Diet was assessed using the established Beverage and Snack Questionnaire (BSQ) completed by the participants’ parents. (Brazendale, Beets, Pate et al., 2017; Brazendale, Beets, Weaver et al., 2017; Neuhouser, Lilley, Lund, & Johnson, 2009) Parents were encouraged to complete the BSQ with their child to increase the accuracy of estimates. Diet was assessed during the same 7-day periods that screen time was collected. Items were scored by four possible response categories, responses consisted of the following: 0 (‘child did not consume’), 1(‘child consumed a little’), 2(‘child consumed some’), and 3 (‘child consumed a lot’) with those individual items. Because of the limited sample size and variability of responses, answers were then dichotomized to either (‘child did not consume’) to (‘child did consume’). For this study, individual BSQ items were grouped in accordance with the Healthy Meal Index (HMI).(Kasper et al., 2016) Food categories included; fruits, vegetables, dairy (non-sugar based), convenience foods, sweets and desserts and sugar sweetened beverages. Consumption was dichotomized (i.e., ‘did’ vs. ‘did not’ consume) and reported as mean days/week.(Neuhouser et al., 2009) Three groups were created for analysis of diet; healthy foods/drinks (fruits, vegetables, and dairy), unhealthy foods (convenience foods, and sweets/desserts), and unhealthy drinks (sugar sweetened beverages).
2.6. Data analysis
Descriptive statistics were calculated for all primary and process outcomes. Since the data was not normally distributed, a median regression examined change in CRF, BMI, zBMI, and BMI percentile from week 1 to week 7. All primary outcome models controlled for attendance and sex. A process descriptive analysis explored differences in PA, screen time, sleep, and diet. The comparisons include: weekday, in which the child attended the program (reference), weekday, in which the child did not attend the program, weekday during the program break, weekend during the program break, and a weekend during the program. The holiday break was a full week, in which those dates would be considered a weekday during the program break with the Saturday, and Sunday prior to the week, and the Saturday and Sunday following the break classified as weekends during the program break.
3. Results
Of the 31 children initially enrolled in the program, primary measures were collected on 20 (35% attrition) participants at both time points (Week 1 and Week 7). Children in the final sample were 6.4 years old (SD = 0.6), 45% female, and 80% African American. Physical activity and sleep data were collected on 23 children. Diet, and screen time behaviors were collected on 26 children. Of the 31 children initially enrolled in the program children attended for an average of 18.6 days (range = 5, 24) out of a maximum of 24 days. Only 1 child attended for less than 2 weeks, 6 children attend from 2 to 4 weeks, and 24 children attended for 5–6 weeks. On average children attend for 3.7 (93%) days out of 4 days that the program operated per week. Children who did not attend during the last week of the SLP (n = 11) were not available for outcome measures of BMI and fitness, thus those children are not included in the final analysis.
3.1. Primary outcomes
As presented in Table 2, no statistically significant change in median BMI, zBMI, or BMI percentile was observed from baseline to outcome. While median PACER laps did increase the change was not statistically significant (baseline = 11 laps, outcome = 14 laps, Δ = 3.00 laps, p = 0.26). A minimal decrease in median BMI was observed from baseline to outcome (baseline = 15.6, outcome = 15.4 Δ = −0.2, p = 0.38). No median changes were noted for both zBMI (baseline = 0.1, outcome = 0.1 Δ = 0.0, p = 0.42) or BMI percentile (baseline = 0.6, outcome = 0.6, Δ = 0.0, p = 0.42).
Table 2.
Median Regression Results Examining Median Changes for PACER and Weight Status.
| Outcome | Median Baseline (wk. 1) | Median Outcome (wk.7) | Change | 95% CI | |
|---|---|---|---|---|---|
| PACER (laps) | 11.0 | 14.0 | 3.0 | −4.7 | 6.7 |
| BMI | 15.6 | 15.4 | −0.2 | −0.9 | 1.4 |
| zBMI | 0.1 | 0.1 | 0.0 | −0.3 | 0.4 |
| BMI Percentile | 0.6 | 0.6 | 0.0 | −0.2 | 0.4 |
All Analyses controlled for attendance.
indicates significant finding p < 0.05.
3.2. Process outcomes
3.2.1. Physical activity
Children’s average minutes spent in MVPA are presented in Table 3. When children attended the SLP they spent 89.4 min in MVPA (SD = 38.6). On days that the SLP operated but children did not attend they accumulated 11.3 fewer minutes of MVPA (78.1 min, SD = 38.0). During the week of the program break children accumulated 10.0 fewer minutes of MVPA (79.4 min, SD = 37.3). During the weekends of the program break, children accumulated 17.0 fewer minutes of MVPA (72.4 min, SD = 45.5). During the weekends of the SLP children accumulated 13.5 fewer minutes of MVPA (75.9 min, SD = 45.0).
Table 3.
Summer Learning Program Secondary Outcomes by Behavior Descriptive Statistics.
| Screen time minutes (n = 26) | Healthy Foods Index (n = 26) | Unhealthy Foods Index (n = 26) | Unhealthy Drinks Index (n = 26) | Minutes of Sleep (n = 23) | MVPA minutes (n = 23) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Diffa | Mean | SD | Diffa | Mean | SD | Diffa | Mean | SD | Diffa | Mean | SD | Diffa | Meana | SD | Diffa | |
| Weekday during SLP and child attended (Ref) | 87.1 | 75.3 | - | 1.4 | 0.8 | - | 1.2 | 1.2 | - | 0.7 | 0.7 | - | 455.1 | 80.3 | - | 89.4 | 38.6 | - |
| Weekday during SLP and child did not attend | 163.2 | 119.1 | 76.1 | 1.5 | 0.7 | 0.1 | 1.6 | 1.1 | 0.3 | 0.8 | 0.8 | 0.1 | 429.2 | 49.0 | −25.9 | 78.1 | 38.0 | −11.3 |
| Weekday during SLP break | 136.8 | 102.1 | 49.7 | 1.7 | 0.6 | 0.3 | 1.9 | 1.3 | 0.3 | 1.0 | 0.6 | 0.3 | 462.2 | 93.3 | 7.0 | 79.4 | 37.3 | −10.0 |
| Weekend during SLP break | 115.7 | 92.9 | 28.7 | 1.5 | 1.0 | 0.1 | 1.5 | 1.0 | −0.4 | 1.1 | 0.7 | 0.1 | 411.7 | 57.7 | −43.5 | 72.4 | 44.7 | −17.0 |
| Weekend during SLP | 149.7 | 100.4 | 62.7 | 1.6 | 0.7 | 0.2 | 1.5 | 1.2 | 0.3 | 0.8 | 0.8 | 0.1 | 405.9 | 71.9 | −49.2 | 75.9 | 45.1 | −13.5 |
All secondary outcomes are compared to the reference of weekdays in which children attended the SLP.
On average, when children attended the program, MVPA attained within program operating hours (8:00am- 3:30pm) was 45 min compared to 24 min for children when they did not attend the program or when the program was on break.
3.2.2. Screen time
On days children attended the SLP they used screens for an average of 87.0 min (SD = 75). On days that the SLP operated, but children did not attend they accumulated 76 more minutes of screen time (163.2 min, SD = 119.1). During the week that the SLP was on break, children accumulated 50 more minutes of screen time (136.8 min, SD = 102.1). During the weekends of the SLP program break, children accumulated 29 more minutes of screen time (115.7 min, SD = 92.9). During weekends of the SLP, children accumulated 63 more minutes of screen time (149.7 min, SD = 100.4) when compared to when children attended the SLP.
3.2.3. Sleep
On nights prior to attending the SLP children accumulated 455 min (SD = 80.3) of sleep. On nights that the SLP operated, but children did not attend they accumulated 26 fewer minutes (429.2 min, SD = 49.0) of sleep. On week nights of the SLP program break, children accumulated 7 more minutes (462.2 min. SD = 93.3) of total sleep. Weekend nights during the SLP program break, children accumulated 44 fewer minutes (411.7 min, SD = 57.7) of total sleep. Weekend nights of the SLP, children accumulated 49 fewer minutes (405.9 min, SD = 71.9) of total sleep when compared to nights in which the SLP operated and children attended.
3.2.4. Diet
According to the parent-report, children consumed a total of 1.4 (SD = 0.8) healthy foods on days they attended the SLP. On days that the SLP operated, but children did not attend, children consumed 0.1 (1.5, SD = 0.7) more healthy foods. On days in which the SLP was on a break, children consumed 0.3 (1.7, SD = 0.6) more healthy foods. During weekends of the SLP program break, children consumed 0.1 (1.5, SD = 1) more healthy foods. During the weekends of the SLP, children consumed 0.2 (1.6, SD = 0.7) more healthy foods when compared to days in which children attended the SLP. On Average children consumed 1.2 (SD = 1.2) unhealthy foods on days they attended the SLP. On days that the SLP operated, but children did not attend, 0.3 (1.6, SD = 1.1) more unhealthy foods were consumed. On week days during SLP program break, children consumed 0.3 (1.9, SD = 1.3) more unhealthy foods. During the weekends of the SLP program break, children consumed 0.4 (1.5, SD = 1) less unhealthy foods. During the weekends of the SLP, children consumed 0.3 (1.5, SD = 1.2) more unhealthy foods when compared to weekdays in which children attended the SLP. On average, children consumed 0.7, (SD = 0.7) unhealthy drinks on days they attended the SLP. On days that the SLP operated, but children did not attend 0.1 (0.8, SD = 0.8) more unhealthy drinks were consumed. On weekdays in which the SLP was on a program break, children consumed 0.3 (1.0, SD = 0.6) more unhealthy drinks. During the weekends of the SLP program break, children consumed 0.1 (1.1, SD = 0.7) more unhealthy drinks. During the weekends of the SLP, children consumed 0.1 (0.8, SD = 0.8) more unhealthy drinks.
4. Discussion
Summer is a time when accelerated weight gain and fitness losses occur,(Baranowski et al., 2014; Brazendale, Beets, Pate et al., 2017; Brazendale, Beets, Weaver et al., 2017; Chen et al., 2016; Economos et al., 2013; Franckle et al., 2014; Gutin et al., 2008; McCue et al., 2013; Moreno et al., 2013; Von Hippel et al., 2007; Yin, Moore, Johnson, Vernon, & Gutin, 2012) however, in this small scale study, children’s weight and fitness remained stable from the beginning until the end of the SLP. This finding, although preliminary, suggests that accelerated weight gain and fitness loss during the summer could be mitigated through access to structured summer programs. Thus, this highly attended program should be used a model to reduce accelerations in weight gain that have been noted during the summer months. Public health promotion should focus on providing children, especially those from low income families affordable access to structured summer programs.
Park et al. (Park & Lee, 2015) found that, similar to the findings of this study, adolescents who attended summer school did not experience increases in BMI and losses in fitness.(Park & Lee, 2015) Findings from this study and Park et al. (Park & Lee, 2015) are important to note, because both were designed for students who were struggling academically, not designed to assist children with maintaining a healthy weight. However, maintenance of a healthy weight status and fitness levels were unintended, positive byproducts of both programs.
The findings herein support the Structured Days Hypothesis (Brazendale, Beets, Pate et al., 2017; Brazendale, Beets, Weaver et al., 2017) by demonstrating that children’s obesogenic behaviors were less favorable during unstructured days (i.e., non-program/weekend days) when compared to structured days (i.e., days attending the SLP). Children were more physically active when they attended the SLP compared to when they did not attend. We also examined children’s engagement in physical activity during program hours to confirm that the increase in physical activity on program days occurred during the SLP. Fig. 1 represents the average weekday MVPA minutes by hour during both program and non-program days. On program days when children attended the SLP they participated in approximately 20 additional minutes of MVPA during program hours (i.e., 8:30am-3:00pm), compared to the same time period on days they did not attend.
Fig. 1.
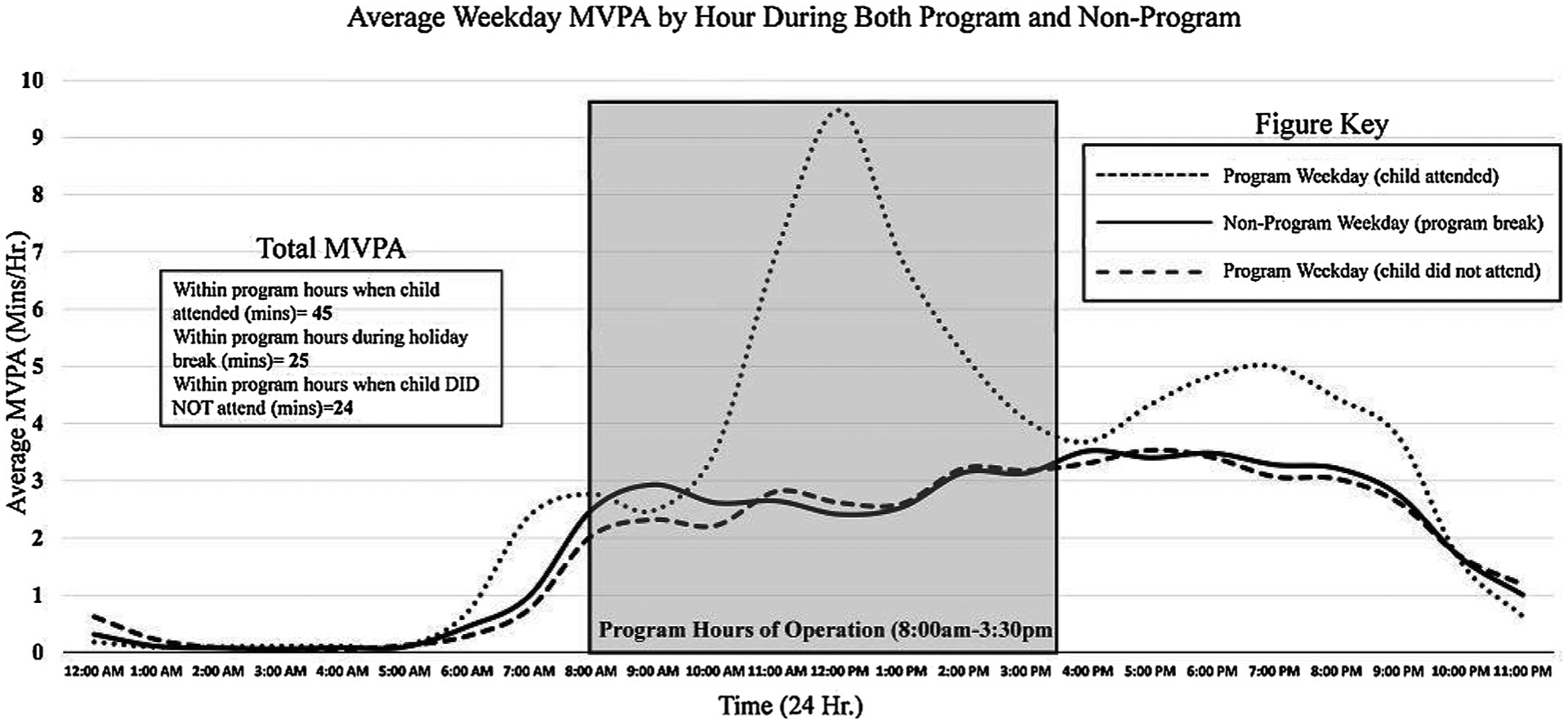
Summer Learning Programs Moderate-to-Vigorous Physical Activity by Child Attendance and Program Hours of Operation.
On days that children attended the SLP, they engaged in less screen time. Similar to the findings herein, a previous study found that on non-school days Australian children increased their screen time usage by 70 min. (Olds, Ridley, & Dollman, 2006) Numerous studies also report that children dramatically increase screen time during the summer when compared to school. (Brazendale et al., 2018; Schmitz et al., 2004; Staiano, Broyles, & Katzmarzyk, 2015; Wang, Vine, Hsiao, Rundle, & Goldsmith, 2015) We found that screen time increased an average of 55 min/day when children did not attend the SLP. Evidence has shown that reduced screen time is associated with a reduction in obesity.(Berkey, Rockett, Gillman, & Colditz, 2003; Francis, Lee, & Birch, 2003; Robinson et al., 1993)
Children in this study also slept marginally longer on nights prior to attending the SLP. This is important as longer sleep duration and earlier bed and wake times have been associated with decreased risk of overweight or obesity.(Appelhans et al., 2014; Chahal, Fung, Kuhle, & Veugelers, 2013; Olds, Maher, & Matricciani, 2011) The structured environment provided by the SLP may have helped parents to regulate bed and wake times on nights prior to their child’s attendance. Apart from weekdays during the program break, children had the greatest total sleep duration on nights when they attended the program the following day. Children however did sleep longer on weekdays during the program break. While it is unclear why this was the case, it may be because parent’s children shifted to a later wake time when there was no program to attend, resulting in longer sleep durations.
On days that children attended the SLP they reported eating marginally fewer healthy and unhealthy foods, when compared to days they did not attend the SLP. Parents also reported that their children consumed fewer unhealthy drinks when attending the SLP. These findings suggest that structured programing can regulate the number of foods, regardless of nutritional benefit, that children are eating. This is similar to other studies, Brazendale et al. (Brazendale et al., 2018) recently found that parents report greater overall consumption of unhealthy and healthy foods in the summer (i.e., unstructured days) when compared to the school year (i.e., structured days).
Overall, results from this study highlight that when children are enrolled in structured programing during the summer months, there is a protective effect on weight and fitness. Children also displayed more healthy behaviors when attending the SLP, compared to when they did not attend. This study does have limitations that should be considered when interpreting the results. First, the small sample limits the generalizability of the findings. Second, this was a natural experiment with no control group, thus the internal validity of the findings are weakened. However, the comparison of children’s obesogenic behaviors on program days compared to days they did not attend the SLP offers a limited counterfactual. Third, the participants enrolled in the SLP were primarily normal weight, thus future studies need to include participants who are overweight or at risk of obesity. Fourth, the program only operated for 7 weeks, this time period does not capture the entire typical summer break for most children. Finally, findings related to diet and screen time should be interpreted with caution due to the use of proxy parent-report and the fact that the BSQ has not be validated in young elementary children. Further, it is important to note that this study did not capture the portion sizes or total calories consumed, rather parents reported if a food was consumed or not consumed. Thus, it is impossible for this study to conclude if the program had a positive impact on children’s total calorie consumption. Future studies should explore structured programming’s impact on the diet of children using gold standard measures. Nonetheless, dietary measures were based on validated measures that have been used previously. (Aires et al., 2010; Eisenmann et al., 2002; Neuhouser et al., 2009; Schmitz et al., 2004; Staiano et al., 2015) Further, parents were encouraged to complete the questionnaire with their children to help with the accuracy of recall. The within subject’s design is a strength of this study. This allowed us to explore changes in weight status, fitness, and obesogenic behaviors over time within the same children. This study also included a sample of children who were primarily African American (80%). Previous studies have shown that children who are African American are at increased risk of accelerated weight gain during the summer (Franckle, 2014). Thus, this study focused on a population of high need. The use of objective PA, sleep, weight classifications, and fitness measures is also a strength.
5. Conclusion
This study examined the impact of a structured SLP on children’s weight gain and fitness loss, and obesogenic behaviors. Children maintained fitness, BMI, zBMI, and BMI percentile from the beginning until the end of the SLP. This finding suggests that attending a structured summer program may mitigate increases in BMI and losses in CRF, by helping children engage in more healthy behaviors. While these findings are preliminary and should be interpreted with caution, this promising strategy should be tested in a larger more representative sample using a rigorous scientific design (e.g., Randomized Control Trials).
Biography
Ethan Hunt, MPH.Ethan has a background in children’s public health focusing on childhood obesity and physical activity. He has worked in several professional roles primarily responsible for the promotion and education of physical activity for youth. He is currently conducting experimental research pertaining to practical strategies that reduce obesity among minority populations. He is also interested in improving physical activity management practices for childcare professionals to maximize physical activity opportunities for youth.
Footnotes
Potential conflicts of interest
None.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, … Carskadon MA (1999). Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep, 22(1), 95–103. [DOI] [PubMed] [Google Scholar]
- Aires L, Andersen LB, Mendonça D, Martins C, Silva G, & Mota J (2010). A 3-year longitudinal analysis of changes in fitness, physical activity, fatness and screen time. Acta Paediatrica, 99(1), 140–144. [DOI] [PubMed] [Google Scholar]
- Appelhans BM, Fitzpatrick SL, Li H, Cail V, Waring ME, Schneider KL, … Pagoto SL (2014). The home environment and childhood obesity in low-income households: Indirect effects via sleep duration and screen time. BMC Public Health, 14(1), 1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacha F, & Gidding SS (2016). Cardiac abnormalities in youth with obesity and type 2 diabetes. Current Diabetes Reports, 16(7), 62. [DOI] [PubMed] [Google Scholar]
- Baranowski T, O’Connor T, Johnston C, Hughes S, Moreno J, Chen T-A, … Baranowski J (2014). School year versus summer differences in child weight gain: A narrative review. Childhood Obesity, 10(1), 18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkey CS, Rockett HR, Gillman MW, & Colditz GA (2003). One-year changes in activity and in inactivity among 10-to 15-year-old boys and girls: Relationship to change in body mass index. Pediatrics, 111(4), 836–843. [DOI] [PubMed] [Google Scholar]
- Bohnert A, Zarrett N, Beets MW, Hall G, Buscemi J, Heard A, … Pate R (2017). Society of Behavioral Medicine (SBM) position statement: SBM supports curbing summertime weight gain among America’s youth. Translational Behavioral Medicine, 7(4), 912–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazendale K, Beets MW, Pate R, Turner-McGrievy GM, Kazcynski A, & Weaver RG (2018). Children’s obesogenic behaviors during summer versus school: A within-person comparison (in press) The Journal of School Health. [DOI] [PubMed] [Google Scholar]
- Brazendale K, Beets M, Pate RR, Turner-McGrievy B, Kaczynski AT, Weaver RG, … Bohnert A (2017). Understanding differences between summer vs. School obesogenic behaviors of children: The Structured Days Hypothesis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazendale K, Beets MW, Weaver RG, Pate RR, Turner-McGrievy GM, Kaczynski AT, … von Hippel PT (2017). Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. The International Journal of Behavioral Nutrition and Physical Activity, 14(1), 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain KL, Sallis JF, Conway TL, Van Dyck D, & Calhoon L (2013). Using accelerometers in youth physical activity studies: A review of methods. Journal of Physical Activity & Health, 10(3), 437–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chahal H, Fung C, Kuhle S, & Veugelers P (2013). Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatric Obesity, 8(1), 42–51. [DOI] [PubMed] [Google Scholar]
- Chandler J, Brazendale K, Beets M, & Mealing B (2016). Classification of physical activity intensities using a wrist-worn accelerometer in 8–12-year-old children. Pediatric Obesity, 11(2), 120–127. [DOI] [PubMed] [Google Scholar]
- Chen T-A, Baranowski T, Moreno JP, O’Connor TM, Hughes SO, Baranowski J, … Johnston CA (2016). Obesity status trajectory groups among elementary school children. BMC Public Health, 16(1), 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cote AT, Harris KC, Panagiotopoulos C, Sandor GG, & Devlin AM (2013). Childhood obesity and cardiovascular dysfunction. Journal of the American College of Cardiology, 62(15), 1309–1319. [DOI] [PubMed] [Google Scholar]
- Cunningham SA, Kramer MR, & Narayan KV (2014). Incidence of childhood obesity in the United States. The New England Journal of Medicine, 370(5), 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economos CD, Hyatt RR, Must A, Goldberg JP, Kuder J, Naumova EN, … Nelson ME (2013). Shape up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Preventive Medicine, 57(4), 322–327. [DOI] [PubMed] [Google Scholar]
- Eisenmann JC, Bartee RT, & Wang MQ (2002). Physical activity, TV viewing, and weight in US youth: 1999 youth risk behavior survey. Obesity, 10(5), 379–385. [DOI] [PubMed] [Google Scholar]
- Francis LA, Lee Y, & Birch LL (2003). Parental weight status and girls’ television viewing, snacking, and body mass indexes. Obesity, 11(1), 143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franckle R (2014). Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: A systematic review. Preventing Chronic Disease, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franckle R, Adler R, & Davison K (2014). Peer reviewed: Accelerated weight gain among children during summer versus school year and related Racial/Ethnic disparities: A systematic review. Preventing Chronic Disease, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y, Brusseau TA, Hannon JC, & Burns RD (2017). Effect of a 12-week summer break on school day physical activity and health-related fitness in low-income children from CSPAP schools. Journal of Environmental and Public Health, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutin B, Yin Z, Johnson M, & Barbeau P (2008). Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: The Medical College of Georgia Fitkid Project. Pediatric Obesity, 3(S1), 3–9. [DOI] [PubMed] [Google Scholar]
- Kasper N, Mandell C, Ball S, Miller AL, Lumeng J, & Peterson KE (2016). The Healthy Meal Index: A tool for measuring the healthfulness of meals served to children. Appetite, 103, 54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL (2002). 2000 CDC Growth Charts for the United States: Methods and development. Vital and health statistics. Series 11, Data from the national health survey; (246)1–190. [PubMed] [Google Scholar]
- Lewis-Beck M, Bryman AE, & Liao TF (2003). The Sage encyclopedia of social science research methods. Sage Publications. [Google Scholar]
- McCue MC, Marlatt KL, & Sirard J (2013). Examination of changes in youth diet and physical activity over the summer vacation period. Internet Journal of Allied Health Sciences and Practice, 11(1), 8. [Google Scholar]
- Mohanan S, Tapp H, McWilliams A, & Dulin M (2014). Obesity and asthma: Pathophysiology and implications for diagnosis and management in primary care. Experimental Biology and Medicine, 239(11), 1531–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno JP, Johnston CA, & Woehler D (2013). Changes in weight over the school year and summer vacation: Results of a 5-year longitudinal study. The Journal of School Health, 83(7), 473–477. [DOI] [PubMed] [Google Scholar]
- Narang I, & Mathew JL (2012). Childhood obesity and obstructive sleep apnea. Journal of Nutrition and Metabolism, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhouser ML, Lilley S, Lund A, & Johnson DB (2009). Development and validation of a beverage and snack questionnaire for use in evaluation of school nutrition policies. Journal of the American Dietetic Association, 109(9), 1587–1592. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, & Flegal KM (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Jama, 307(5), 483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Lamb MM, Carroll MD, & Flegal KM (2010). Obesity and socioeconomic status in children and adolescents: United States, 2005–2008. NCHS Data Brief. Number 51National Center for Health Statistics. [PubMed] [Google Scholar]
- Olds T, Ridley K, & Dollman J (2006). Screenieboppers and extreme screenies: The place of screen time in the time budgets of 10–13 year-old Australian children. Australian and New Zealand Journal of Public Health, 30(2), 137–142. [DOI] [PubMed] [Google Scholar]
- Olds TS, Maher CA, & Matricciani L (2011). Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep, 34(10), 1299–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park K-S, & Lee M-G (2015). Effects of summer school participation and psychosocial outcomes on changes in body composition and physical fitness during summer break. Journal of Exercise Nutrition & Biochemistry, 19(2), 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock NK (2015). Childhood obesity, bone development, and cardiometabolic risk factors. Molecular and Cellular Endocrinology, 410, 52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TN, Hammer LD, Wilson DM, Killen JD, Kraemer HC, Hayward C, … Taylor CB (1993). Does television viewing increase obesity and reduce physical activity? Cross-sectional and longitudinal analyses among adolescent girls. Pediatrics, 91(2), 273–280. [PubMed] [Google Scholar]
- Sadeh A (2011). The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews, 15(4), 259–267. [DOI] [PubMed] [Google Scholar]
- Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, & Hovell MF (1997). The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, Play and Active Recreation for Kids. American Journal of Public Health, 87(8), 1328–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz KH, Harnack L, Fulton JE, Jacobs DR, Gao S, Lytle LA, … Coevering P (2004). Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. The Journal of School Health, 74(9), 370–377. [DOI] [PubMed] [Google Scholar]
- Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, & Byers T (1993). Do obese children become obese adults? A review of the literature. Preventive Medicine, 22(2), 167–177. [DOI] [PubMed] [Google Scholar]
- Staiano AE, Broyles ST, & Katzmarzyk PT (2015). School term vs. School holiday: Associations with Children’s physical activity, screen-time, diet and sleep. International Journal of Environmental Research and Public Health, 12(8), 8861–8870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J, Pratt C, Boyington J, Nelson C, Truesdale KP, Ward DS, … Moore S (2017). Multilevel interventions targeting obesity: Research recommendations for vulnerable populations. American Journal of Preventive Medicine, 52(1), 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, & Saelens BE (2012). Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. The International Journal of Behavioral Nutrition and Physical Activity, 9(1), 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treviño RP, Fogt DL, Wyatt TJ, Leal-Vasquez L, Sosa E, & Woods C (2008). Diabetes risk, low fitness, and energy insufficiency levels among children from poor families. Journal of the American Dietetic Association, 108(11), 1846–1853. [DOI] [PubMed] [Google Scholar]
- United States Department of Agriculture Food and Nutrition Service (2018). Summer food service program. Retrieved from https://www.fns.usda.gov/sfsp/summer-food-service-program.
- von Hippel PT, & Workman J (2016). From kindergarten through second grade, US children’s obesity prevalence grows only during summer vacations. Obesity, 24(11), 2296–2300. [DOI] [PubMed] [Google Scholar]
- Von Hippel PT, Powell B, Downey DB, & Rowland NJ (2007). The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. American Journal of Public Health, 97(4), 696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YC, Vine S, Hsiao A, Rundle A, & Goldsmith J (2015). Weight-Related Behaviors When Children Are in School Versus on Summer Breaks: Does Income Matter? The Journal of School Health, 85(7), 458–466. [DOI] [PubMed] [Google Scholar]
- Welk G, & Meredith MD (2010). Fitnessgram and activitygram test administration manual-updated 4th edition. Human Kinetics. [Google Scholar]
- Yin Z, Moore JB, Johnson MH, Vernon MM, & Gutin B (2012). The impact of a 3-year after-school obesity prevention program in elementary school children. Childhood Obesity, 8(1), 60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]


