Abstract
Purpose
To assess the initial utilization, safety, and patient experience with tele-ophthalmology during the COVID-19 pandemic.
Design
Cross-sectional study.
Methods
We conducted a telephone survey and interview of a random sample of patients who received different modalities of care (in-person, telephone, videocall, or visits deferred) during Michigan's shelter-in-place order beginning March 23, 2020. The survey assessed patient safety, patient satisfaction with care, perceptions of telehealth-based eye care, and worry about eyesight. Data were analyzed via frequency measures (eg, means and standard deviations), χ2 tests, ANOVA, and paired t tests. Interviews were analyzed using grounded theory.
Results
A total of 3,274 patients were called and 1,720 (53%) agreed to participate. In-person participants were significantly older than telephone (P = .002) and videocall visit (P = .001) participants. Significantly more white participants had in-person visits than minority participants (P = .002). In-person visit participants worried about their eyesight more (2.7, standard deviation [SD] = 1.2) than those who had telephone (2.5, SD = 1.3), videocall (2.4, SD = 1.1), or deferred visits (2.4, SD = 1.2) (P = .004). Of all telephone or videocall visits, 1.5% (n = 26) resulted in an in-person visit within 1 day, 2.9% (n = 48) within 2-7 days, and 2.4% (n = 40) within 8-14 days after the virtual visit demonstrating appropriate triage to telemedicine-based care. Patients frequently cited a desire for augmenting the telephone or videocall visits with objective test data.
Conclusions
When appropriately triaged, tele-ophthalmology appears to be a safe way to reduce the volume of in-person visits to promote social distancing in the clinic. A hybrid model of eye care combining ancillary testing with a video or phone visit represents a promising model of care.
Since the first confirmed case of COVID-19 in the United States on January 22, 2020, the pandemic has grown exponentially.1 In response, state governments initially ordered citizens to shelter in place. On March 23, 2020, 9 states had issued shelter-in-place orders, which grew to 42 states by April 22.2 During this time, in-person visits to eye care providers declined more than to any other specialty providers,3 causing an increase in the need for remote eye care. This need, coupled with policy changes that allowed clinicians to bill for telehealth services at the same level as an in-person encounter, fueled a rapid expansion of telehealth-based eye care services.
Prior to the COVID-19 pandemic, only 30% of ophthalmic clinicians reported using telemedicine to deliver eye care.4 However, studies of telemedicine-based eye care services during the pandemic suggests that about 60% of clinicians are likely to continue using telemedicine even after the pandemic.5 Likewise, many patients greatly appreciated being able to receive care via telemedicine during the COVID-19 pandemic.6, 7, 8 Patients reported the highest satisfaction with telemedicine systems that were easy to use, were inexpensive, decreased travel time, decreased wait time, and resulted in improved communication with their medical provider.9 , 10 However, participants have noted difficulty establishing rapport with their physician and concern about possible medical errors as potential barriers to using telemedicine.8 Despite these previous studies investigating the use of telemedicine during COVID-19, still little is known about telehealth-based eye care, such as the patient's experience, patient's satisfaction, and safety of triaging patients to receive eye care through telehealth during the COVID-19 pandemic.
The purpose of this study is to assess utilization, safety of the patient triage system, and the patient experience with telehealth-based eye care delivery during the COVID-19 pandemic. Our study was carried out at a tertiary referral center in Michigan, a state where shelter-in-place orders were issued in March 2020. These data are crucial for ensuring that telemedicine-based platforms promote safe, patient-centered eye care delivery.
Methods
Clinical Setting
This study was conducted at a tertiary, multispecialty care practice (University of Michigan Kellogg Eye Center, Ann Arbor, Michigan, USA). The center includes 108 faculty physicians who provided approximately 206,000 outpatient visits in 2019. In the state of Michigan, the shelter-in-place order began on March 23, 2020. From March 23, 2020 to May 25, 2020, the University of Michigan instituted a clinical policy to provide in-person care only for urgent or semi-urgent patients and defer care or provide telemedicine-based eye care for all other patients. The system for triaging urgent calls was changed during this time. Once a clerk identified an urgent call, rather than immediately schedule an in-person examination per prepandemic protocols, a physician was included in the decision of how a patient should be seen—in person or by telemedicine. The Kellogg Eye Center also implemented a drive-through intraocular pressure check with iCare tonometry (iCare, Vantaa, Finland).11 Patients were able to have this testing done and follow up the results with their physician through a virtual visit at a later time.
Participants and Sample Selection
We conducted a telephone survey of a random sample of patients who had a scheduled visit at the Kellogg Eye Center and its satellite sites between March 23, 2020 and May 8, 2020. All calls were made between April 30, 2020 and May 25, 2020. Recruitment was stratified by visit type, where 38% of patients who received in-person visits, 92% of patients who received video visits, 68% of patients who received telephone visits, and 15% of patients whose visits were deferred were contacted. We oversampled videocall and telephone visits because they had a lower number of encounters overall and we wanted a reasonable sample size of patients who had experienced each visit type. Patients who had multiple visit types were stratified into groups using the following algorithm: (1) anyone who received any in-person care at the eye center was classified as an in-person visit; (2) anyone who received a videocall visit, but no in-person visits, was classified as a video visit; (3) anyone who received a telephone visit, but not a videocall or an in-person visit, was classified as a telephone visit; (4) anyone whose care had only been deferred was classified as deferred. Duplicate entries were removed from call lists. A maximum of 3 calls were made to each patient if the patient was not reached on initial contact.
This study was approved by the University of Michigan institutional review board as exempt quality improvement research and adhered to the tenets of the Declaration of Helsinki.
Patient Assessments
Each participant was asked 5 questions over the phone after obtaining verbal assent to participate (Appendix; Supplemental Material available at AJO.com). The first question asked was “How is your eye problem doing?” to ensure that no participants had an unresolved medical issue. If a participant reported any eye problem, they were given the Kellogg Eye Center's triage phone number and directed to call immediately after their call with the study team member. If the issue was very urgent, the study caller also notified physicians on the team (M.A.W, P.A.N.C.). The second question was open-ended to elicit a broad range of responses. Depending on their type of visit, participants were asked 1 of the following questions: How did you feel about… (1) coming to the clinic during the coronavirus pandemic?, (2) having a virtual visit (via videocall or telephone) during the coronavirus pandemic?, or (3) being rescheduled during the coronavirus pandemic? The next 2 questions were closed-ended questions from the National Eye Institute Visual Function Questionnaire-912 that measures patients’ perception of their eyesight and how worried they are about their eyesight (Appendix). The last closed-ended question assessed participants’ satisfaction with the care they received: “On a scale from 1-10 where 1 is completely dissatisfied and 10 is completely satisfied, how would you rate your satisfaction with your eye care from the Kellogg Eye Center during the coronavirus pandemic, whether your care has been deferred, you were seen in person, or whether you were seen though a videocall or telephone visit?”
Sociodemographic and Clinical Data
Age, race, sex, city, state, and zip code were extracted from the electronic health record's research data warehouse (EPIC Clarity). Census tracts were used to assess median household income through the public file provided by the American Community Survey for the years 2014-2018.13 Eye care clinician subspecialty and primary eye diagnosis for the visit were extracted. The primary eye diagnosis ICD-10 codes were categorized into overarching disease categories. The primary clinician subspecialty was recategorized into Comprehensive (Comprehensive and Optometry), Anterior Segment (Adult Strabismus, Cornea, and Oculoplastics) and Posterior Segment (Glaucoma, Neuro-Ophthalmology, Retina-Uveitis, and Ocular Oncology).
Analysis of Open-ended Responses
During the first week (April 30-May 6) of telephone interviews, study team members took field notes on how participants felt about their eye care or eye care deferral during the COVID-19 pandemic. Using grounded theory, qualitative data were assessed.14 , 15 Once each study team member had reviewed their field notes and identified themes, the team came together to create a codebook of broader codes that incorporated all of the themes generated by the individual study members. Three study team members (J.C., D.B., L.A.) then coded all open-ended responses using the codebook. A random 10% sample of codes was compared between graders and percent agreement was calculated.
Statistical Analysis
Demographic characteristics of the participant sample (age, sex, race, median household income) were summarized with descriptive statistics including means, standard deviations (SD), frequencies, and percentages overall and for each visit type (in-person, videocall, telephone, and deferred). Clinical characteristics including clinician subspecialty and the top 5 primary eye diagnoses were summarized with frequency counts and proportions and displayed in rank order. The proportion of completed visits, in-person or virtual (telephone or videocall), was assessed as follows: [(in-person visits + videocall visits + telephone visits) divided by the total number of visits (in-person visits + videocall visits + telephone visits + deferred visits)]. To assess visit type utilization, the proportion of completed visits that were in-person visits, videocall visits, telephone visits, and deferred visits were calculated. Triage system safety was assessed by calculating the proportion of virtual visits that resulted in an in-person visit within 1 day, within 2-7 days, or within 8-14 days. For each virtual visit that resulted in an in-person evaluation within the 2-week window, clinician specialty type was recorded.
Participant satisfaction level was summarized with frequencies and percentages and stratified into nonsatisfied (score ≤ 7) and satisfied (score > 7) owing to having highly skewed satisfaction scores. Questions assessing participant perception of and worry about visual function were scored according to the methods of Kodjebacheva and associates.12 Scores were summarized with means and SDs. Differences between visit type and categorical variables were assessed with χ2 tests. In instances where there were significant differences, post hoc χ2 tests were performed to assess the differences. Differences between visit type and continuous variables were assessed using ANOVA. In instances where there were significant differences, pairwise t tests with a Bonferroni adjustment were performed to assess the differences. Qualitative measures of open-ended questions were summarized with frequencies and percentages and the top 5 categories were reported for each visit type. Quotes that represented each theme well were chosen to demonstrate the meaning of the theme.
Results
From March 23, 2020 until May 8, 2020, 5.7% (n = 6,542) of scheduled visits (n = 24,455) were completed. Of the completed visits, 74.3% (n = 4,861) were in-person visits, 4.8% (n = 314) were videocall visits, and 20.9% (n = 1,367) were telephone visits. Table 1 displays demographics overall and for respondents only.
Table 1.
Summary Statistics Overall and by Visit Type
| Total (N = 1,720) |
Deferred (N = 769) |
In Person (N = 536) |
Phone (N = 320) |
Video (N = 95) |
P Value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| Mean (SD) | 64.7 (16.8) | 64.7 (16.1) | 66.8 (17.3) | 62.6 (17.8) | 59.8 (15.0) | <.001 |
| Sex | ||||||
| Female | 1009 (58.7%) | 450 (58.5%) | 316 (59.0%) | 186 (58.1%) | 57 (60.0%) | .979 |
| Male | 711 (41.3%) | 319 (41.5%) | 220 (41.0%) | 134 (41.9%) | 38 (40.0%) | |
| Race | ||||||
| White | 1396 (81.2%) | 604 (78.5%) | 468 (87.3%) | 249 (77.8%) | 75 (78.9%) | .002 |
| Black | 180 (10.5%) | 87 (11.3%) | 42 (7.8%) | 39 (12.2%) | 12 (12.6%) | |
| Asian | 66 (3.8%) | 40 (5.2%) | 13 (2.4%) | 10 (3.1%) | 3 (3.2%) | |
| Other | 78 (4.5%) | 38 (4.9%) | 13 (2.4%) | 22 (6.9%) | 5 (5.3%) | |
| Ethnicity | ||||||
| Hispanic | 38 (2.3%) | 15 (2.1%) | 11 (2.1%) | 11 (3.7%) | 1 (1.1%) | .362 |
| Non-Hispanic | 1593 (97.7%) | 713 (97.9%) | 502 (97.9%) | 290 (96.3%) | 88 (98.9%) | |
| Median household income | ||||||
| Mean (SD) | 75387 (32696) | 76940 (34366) | 74657 (31346) | 73101 (29641) | 74547 (35671) | .327 |
| Provider specialty | ||||||
| Adult strabismus | 12 (0.7%) | 11 (1.4%) | 1 (0.2%) | 0 (0.0%) | 0 (0.0%) | <.001 |
| Comprehensive & cataract surgery | 345 (20.1%) | 205 (26.7%) | 43 (8.0%) | 79 (24.7%) | 18 (18.9%) | |
| Cornea, external disease, & refractive surgery | 327 (19.0%) | 87 (11.3%) | 65 (12.1%) | 137 (42.8%) | 38 (40.0%) | |
| Glaucoma | 243 (14.1%) | 180 (23.4%) | 27 (5.0%) | 33 (10.3%) | 3 (3.2%) | |
| Neuro-ophthalmology | 61 (3.5%) | 7 (0.9%) | 47 (8.8%) | 2 (0.6%) | 5 (5.3%) | |
| Ocular oncology | 31 (1.8%) | 10 (1.3%) | 17 (3.2%) | 1 (0.3%) | 3 (3.2%) | |
| Optometry | 144 (8.4%) | 115 (15.0%) | 22 (4.1%) | 5 (1.6%) | 2 (2.1%) | |
| Plastics | 56 (3.3%) | 31 (4.0%) | 5 (0.9%) | 5 (1.6%) | 15 (15.8%) | |
| Retina, uveitis, & rheumatology | 501 (29.1%) | 123 (16.0%) | 309 (57.6%) | 58 (18.1%) | 11 (11.6%) | |
| Provider type | ||||||
| Anterior segment | 395 (23.0%) | 129 (16.8%) | 71 (13.2%) | 142 (44.4%) | 53 (55.8%) | <.001 |
| Comprehensive | 489 (28.4%) | 320 (41.6%) | 65 (12.1%) | 84 (26.2%) | 20 (21.1%) | |
| Posterior segment | 836 (48.6%) | 320 (41.6%) | 400 (74.6%) | 94 (29.4%) | 22 (23.2%) |
A stratified random sample of 3,274 patients were called, and 1,720 (53% response rate) agreed to be surveyed. Those responding to our survey were older and less likely to have had their visit deferred (Supplemental Table 1; Supplemental Material available at AJO.com), but were otherwise similar in sex, race, and ethnicity to those who responded to the survey. The mean age was 64.7 years (SD = 16.8), 58.7% were female, 82.6% were white or Caucasian, and the median household income was $75,387 (SD = $32,696). All major provider subspecialties were represented.
The mean age of respondents differed significantly by visit type. In-person participants were significantly older compared to those receiving videocall visits (66.8 vs 59.8 years; P = .001) and telephone visits (66.8 vs 62.6 years; P = .002). White participants (87.3%, n = 468) were significantly more likely to have an in-person visit compared to minority participants (12.6%, n = 68; P = .002). Retina specialists provided more in-person visits and cornea specialists provided more telephone visits compared to other subspecialists (P < .001) (Table 1).
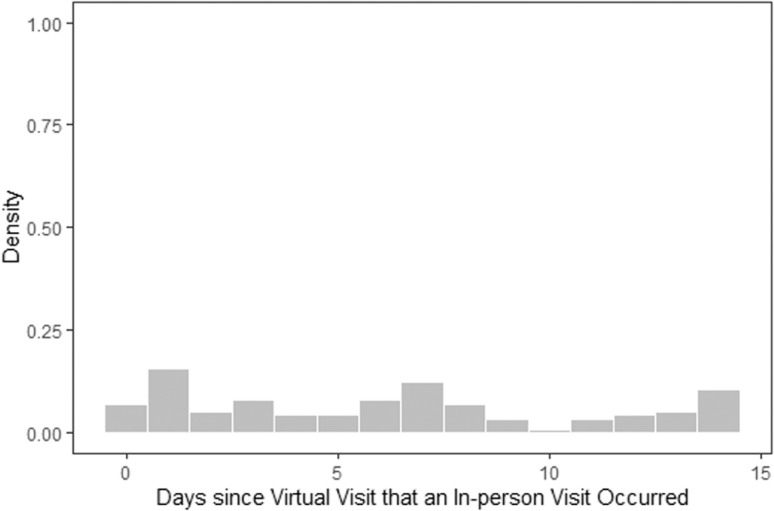
The top 5 diagnostic categories over all visit types were glaucoma (all forms) (10.3%), macular degeneration (9.9%), status post operation (9.2%), other retinal conditions (7.1%), and corneal defects (3.9%). Supplemental Table 2 (Supplemental Material available at AJO.com) includes descriptions of diagnostic categories by visit type. Of all the virtual visits (telephone or videocall), 6.8% (n = 114) resulted in an in-person visit within 2 weeks; 1.5% (n = 26) within 1 day, 2.9% (n = 48) within 2-7 days, and 2.4% (n = 40) within 8-14 days after the virtual visit. The Figure 1 is a histogram of the number of virtual visits that resulted in an in-person visit within 2 weeks. Top 6 reasons for why patients were seen in person within 1 week of a virtual visit were infectious (n = 16, 19.3%), status post operation (n = 15, 18.1%), corneal defects (n = 15, 18.1%), other retinal conditions (n = 6, 7.2%), uveitis (n = 5, 6.0%), and dry eye (n = 5, 6.0%).
Figure 1.
Histogram of days since virtual visit that resulted in in-person visit.
Of the survey participants, the mean perception of visual function score was 2.5 (SD = 1.0) on a scale of 1-5, where 1 represents “excellent vision” and 5 represents “very poor vision” (Table 2 ). Perception of visual function did not differ significantly by visit type. Participants rated worry about eyesight at a mean of 2.5 (SD = 1.2) on a scale from 1 to 6, where 1 represents being worried “none of the time” and 6 represents being worried “all of the time.” Participants who had in-person visits worried about their eyesight more (2.7, SD = 1.2) than those who had telephone (2.5, SD = 1.3) or videocall (2.4, SD = 1.1) visits or had their visit deferred (2.4, SD = 1.2) (P = .004). When stratified by clinician specialty type, patients seeing comprehensive ophthalmologists rated their eyesight as better and worried less about their eyesight compared to patients who saw anterior or posterior segment disease clinicians (P < .05 for all comparisons) (Table 3 ).
Table 2.
Perception of Eyesight, Worry of Eyesight, and Satisfaction by Visit Type
| Total (N = 1,720) |
Deferred (N = 769) |
In Person (N = 536) |
Phone (N = 320) |
Video (N = 95) |
P Valuea | |
|---|---|---|---|---|---|---|
| At the present time, would you say your eyesight (with glasses or contact lenses, if you wear them) is: (1-6) | ||||||
| Mean (SD) | 2.5 (1.0) | 2.4 (1.0) | 2.6 (1.0) | 2.6 (1.1) | 2.5 (0.9) | .058 |
| How much of the time do you worry about your eyesight (1-5) | ||||||
| Mean (SD) | 2.5 (1.2) | 2.4 (1.2) | 2.7 (1.2) | 2.5 (1.3) | 2.4 (1.1) | .004 |
| How would you rate your satisfaction with your eye care during the COVID-19 epidemic? | ||||||
| Nonsatisfied | 198 (11.9%) | 110 (14.7%) | 38 (7.3%) | 43 (14.2%) | 7 (7.6%) | <.001 |
| Satisfied | 1,466 (88.1%) | 639 (85.3%) | 483 (92.7%) | 259 (85.8%) | 85 (92.4%) |
ANOVA was performed on the continuous measures. χ2 test was performed on the categorical measure.
Table 3.
Perception of Eyesight, Worry of Eyesight, and Satisfaction by Provider Specialty Type
| Total (N = 1,720) |
Anterior Eye Disease (N = 395) |
Comprehensive (N = 489) |
Posterior Eye Disease (N = 836) |
P Valuea | |
|---|---|---|---|---|---|
| At the present time, would you say your eyesight (with glasses or contact lenses, if you wear them) is: (1-6) | |||||
| Mean (SD) | 2.5 (1.0) | 2.6 (1.1) | 2.3 (1.0) | 2.5 (1.0) | <.001 |
| How much of the time do you worry about your eyesight (1-5) | |||||
| Mean (SD) | 2.5 (1.2) | 2.6 (1.3) | 2.4 (1.1) | 2.6 (1.2) | .004 |
| How would you rate your satisfaction with your eye care during the COVID-19 epidemic? | |||||
| Nonsatisfied | 198 (11.9%) | 48 (12.5%) | 67 (14.2%) | 83 (10.3%) | .106 |
| Satisfied | 1,466 (88.1%) | 337 (87.5%) | 405 (85.8%) | 724 (89.7%) |
ANOVA was performed on the continuous measures. χ2 test was performed on the categorical measure.
Most participants (88.1%; n = 1,466) rated their satisfaction with the eye care greater than or equal to 8 out of 10. A higher proportion of those who had in-person or video visits had higher satisfaction compared to canceled-visit or telephone-visit participants (P < .001). There were no significant differences in patient-reported satisfaction scores between those seen by different specialty providers.
Open-ended questions were answered by 1,706 (99.2%) of survey respondents; 536 (31.2%) had in-person visits, 95 (5.5%) had videocall visits, 320 (18.6%) had telephone visits, and 769 (44.7%) had deferred visits. The 3 coders had 96.4% agreement for coding the interviews from participants seen in person, 92.0% agreement for participants seen through videocall visits, 90.7% agreement for participants seen through telephone visits, and 96.4% agreement for participants whose visits were deferred.
When asked how they felt about their in-person care, the 5 most common themes were (1) feeling reassured by COVID-19 precautions, 54.9% (n = 294), (2) feeling indifferent to modality of care, 19.4% (n = 104), (3) expressing a positive perception of the quality of care, 10.3% (n = 55), (4) feeling that the care was appropriate given the risk of exposure, 9.9% (n = 53), and 5) expressing a negative perception of the quality of care, 7.3% (n = 39). Two hundred and ninety-four participants who had in-person visits commented that they felt reassured by the precautions the center had taken to minimize the risk of COVID-19 infections: “I was apprehensive at first, but I think they had everything under control, you had to wear a mask, we had to keep our distance from each other.” One hundred and four participants were not as concerned about COVID-19, saying, “I don't care about [COVID-19], I just want some help with my eyes.” Fifty-five participants felt that being seen in person had a positive impact on the quality of care they received: “I was so grateful to come in because I really need my serum tears.” Fifty-three participants felt that coming in person was worth the risk of exposure to COVID-19: “There was anxiety but there was even more anxiety about losing my eyesight, so I'll take risks to avoid losing my eyesight.” Lastly, 39 participants felt that changes made to their in-person appointment resulted in a poorer quality of care: “I was upset that I didn't get to see my own doctor, and nobody told me, I wouldn't have come in if I had known.”
The 5 most common themes for videocall visits were (1) expressing a negative perception of the quality of care, 45.7% (n = 43); (2) expressing a positive perception of the quality of care, 39.4% (n = 37); (3) feeling that the care was convenient, 30.9% (n = 29); (4) feeling that the technology worked well, 21.3% (n = 20); and (5) feeling like the care was appropriate given their disease severity, 14.9% (n = 14). Forty-three participants were skeptical about the quality of their videocall visits, mentioning how “I need an eye exam, so video conference isn't doing me any good.” However, 37 participants expressed the opposite sentiment, saying, “I thought [the videocall visit] was amazing, because it felt like I was sitting right in front of her speaking to her.” Twenty-nine participants liked the videocall visit for its convenience: “It's my first video visit and for follow-up it was perfect, because it saved me a lot of time, especially with not having to leave work, drive, park and wait. It's a real time saver.” Twenty participants liked how easy the technology was to use: “[I] was able to use the technology with ease […] I was worried because of my age, but it was easier than I thought it would be.” Lastly, about 14 participants thought the medium was appropriate given the severity of their illness: “I thought it was adequate and appropriate. If it's for a regular visit I would prefer a video visit [even] under normal circumstances.”
The 5 most common themes about telephone visits were (1) expressing a negative perception of the quality of care, 33.9% (n = 106); (2) expressing a positive perception of the quality of care, 22.4% (n = 70); (3) feeling indifferent to the modality of care, 17.9% (n = 56); (4) feeling that the modality of care was appropriate given their disease severity, 12.1% (n = 38); and (5) feeling that the care was appropriate given the risk of exposure, 10.9% (n = 34). One hundred and six participants felt that the telephone visits were of poorer quality than in-person visits: “The phone visit was helpful, but nothing like having them looking at the eye itself.” However, 126 participants expressed that the telephone visits were equal to, if not better than, in-person visits: “[I received] more undivided attention than when I'm in the office,” or “I don't think it was very different from having a face-to-face conversation.” Thirty-eight participants thought that telephone visits were appropriate given the severity of their eye illness, saying, “My issue's not too serious so this is a good way to handle it right now.” Thirty-four participants thought that phone visits were appropriate given the risk of in-person visits posed by the pandemic: “I know that [arranging phone visits] is not for a wrong reason […] I love that we're protecting all people.”
When asked how they felt about their deferred care, the 5 most common themes were as follows: (1) felt deferral was appropriate given the pandemic restrictions, 57.6% (n = 439); (2) felt deferral was appropriate given the potential risk of exposure, 21.4% (n = 163); (3) felt indifferent to the deferral, 16.9% (n = 129); (4) felt that the deferral was inappropriate despite the pandemic, 12.5% (n = 95); and (5) expressed a negative perception of the quality of care, 11.8% (n = 90). A majority of participants with deferred appointments felt that their care was appropriately deferred given the pandemic: “We understood there was no other option. If you hadn't canceled, we would have.” One hundred and sixty-three felt that the deferral of care was appropriate given the risk of COVID-19 exposure: “We just think it was too early after the virus and we weren't comfortable going into the hospital.” One hundred and twenty-nine participants felt indifferent about the decision to defer their visit: “I don't feel like I needed an eye doctor to begin with.” However, 95 participants felt that their care was inappropriately deferred despite the ongoing pandemic, and 90 participants associated it with a poorer quality of care. These sentiments were reflected in the quotes "I get the impression that [my strabismus] was not being taken as seriously" and “I have not been seen for months […] I just feel like I'm not a priority.”
Discussion
In a large academic tertiary referral center, over 75% of eye care visits were canceled during shelter-in-place orders. Of the completed visits, 74.3% were in-person visits, 4.8% were videocall visits, and 20.9% were telephone visits. In other words, 25.7% of all visits during the study period were conducted virtually, which represents a 28-fold increase in proportion of virtual care usage compared to its prepandemic level of 0.9% in February 2020. Minority patients were less likely to have in-person visits compared to white patients; while minority patients represented 18.8% of our entire study participants, they only represented 12.6% of patients seen in person. Likewise, younger patients were less likely to have in-person visits compared to older patients. Overall, satisfaction with telehealth-based eye care was excellent during the pandemic but was significantly higher among those undergoing videocall visits compared to telephone visits. This suggests that when videocall visits are available and patients are able to use it, they are often preferred, perhaps suggesting the importance of face-to-face interactions. Taken together, our study suggests that telehealth-based eye care may potentially be a promising eye care delivery model that in some situations may be acceptable to patients, but it also has the potential to exacerbate eye care disparities.
Virtual ophthalmology visits at our center were used for a wide array of conditions, such as corneal abrasions, glaucoma, retinal conditions, autoimmune disease, uveitis, postoperative checks, and triaging visual symptom complaints. Because visualizing the anterior segment of the eye on a video visit was more feasible than visualizing the posterior segment with the current systems used by the University of Michigan, some specialties were able to use telemedicine at higher rates than others. For example, cornea specialists had the highest volume of telemedicine visits in this sample, while retina specialists had the lowest. Cornea specialists triaged phone calls for their own clinics in March and April to minimize in-person visits and were more comfortable conducting visits via videocall or telephone call, as they could still visualize the anterior segment if needed by photo or videocall. Second, our center implemented a drive-through intraocular pressure check with iCare tonometry and the results were followed up via a virtual visit at a different time. This hybrid model of in-person ancillary testing followed by a virtual visit likely accounts for the increase in virtual care utilization by glaucoma providers and patients.
Of the all the virtual visits (telephone or videocall), only 1.5% resulted in an in-person visit within 1 day of the virtual visit, while 2.9% resulted in an in-person visit 2-7 days after the virtual visit. This small proportion of patients eventually needing in-person care speaks to the safety and effectiveness of the triaging system used at our center in identifying which patients may safely be seen virtually. Additionally, we found that participants who were more worried about their eyesight were more likely to receive in-person care, suggesting that the triage system was also effective from a patient-centered perspective. Despite its rapid implementation, telemedicine-based eye care represented an effective and safe modality of care for our patients.
A survey of 1,051 glaucoma patients’ experiences and concerns during the COVID-19 pandemic over 4 days in May 2020 found that 63% of participants were “somewhat comfortable” or “extremely comfortable” receiving glaucoma care in person as long as face masks were worn and the waiting rooms were less crowded.16 Of the participants, 68% preferred an in-person visit, 28% would consider telemedicine, and 4% preferred telemedicine. However, 97% of the patients surveyed for this study had never used telemedicine, in effect resulting in an “in vitro” or hypothetical study of patient perception toward telemedicine rather than an “in vivo” study of perceptions toward telemedicine from those who had actually experienced it. In our in vivo study of telemedicine, we found that participants who received virtual care—especially those who had video visits that allowed for face-to-face interactions with their provider—had high satisfaction. Furthermore, it is important to note that 24% of our participants felt positive about their in-person visit explicitly because of low waiting room occupancies. For instance, a participant mentioned that “I am usually terrified of your waiting room, but I was so glad when I came in the last time and there were only 6-7 people in it.” Both virtual and deferred visits kept waiting room occupancies low. Thus, virtual care for patients with lower-risk disease is an ideal way to lower patient volume in clinic, waiting room occupancies, and risk of receiving in-person care for high-risk patients.17 , 18
Kruse and associates conducted a systematic review of telehealth and patient satisfaction and found that ease of use, low cost, and decreased travel time are aspects of telemedicine that contribute to increased satisfaction.9 Low cost can refer not only to the visit cost itself, but also to the relatively lower opportunity cost of not having to miss work or force a family member/friend to accompany the patient to the appointment. In our qualitative analysis, we found that people liked their telemedicine visits for many of these reasons; for instance, 1 participant mentioned that “It was smooth and the process was easy. It's much nicer to not have to wait and I appreciated the efficiency” while another said, “I thought it was amazing, because it felt like I was sitting right in front of her speaking to her. It felt like an office visit. I would do it again.” One participant mentioned liking the virtual visit better than in-person visits, as “it seemed more one-on-one than going into the office where [my doctor] is talking to the scribe.”
While not within the scope of this research study, provider perspectives are another important factor to consider when transitioning to telehealth-based healthcare delivery platforms. In another study published by the authors, we have found that at least 66% of providers felt at least somewhat confident in their ability to use remote screening for eye care, which represented a dramatic shift compared to prepandemic confidence levels, where 60% of clinicians were not confident in their ability.4 In the same study, we found that confident clinicians were significantly more willing to continue telemedicine for the following year and see opportunities for expansion, and concluded that continued exposure, familiarization, and utilization of telehealth-based platforms are important in sustaining providers’ confidence.4
When participants were asked open-ended question about their care, the response was overwhelmingly positive across all 4 visit types and an overall 88.1% of all participants were highly satisfied with their care. Among those who had their visits deferred, the number of participants who felt that the deferral was appropriate (owing to pandemic precautions and owing to fear of exposure) was more than 5 times the number of participants who felt that the deferral was inappropriate. Among those who had their visits in person, 22 times more participants felt reassured by the precautions taken by the center than those who were not reassured. Among those who had video visits, the perception of the quality of care was nearly equal between those who thought it was good and bad. However, 66.3% of participants had at least 1 positive thing to say about their videocall visits, such as stating that it improved the quality of care, that it was more convenient than an in-person visit, that the technology worked well, or that the modality of care was appropriate given the risk of COVID-19 exposure. Among those who had telephone visits, more patients (40.3%) thought that their quality of care either benefited or was not impacted than patients who thought their care was negatively impacted (33.9%) by having their care delivered over the phone. Furthermore, even among the 106 patients who had a negative perception of the quality of care delivered over the phone visit, 50 patients had at least 1 positive thing to say about their telephone visit, with 20 patients mentioning the appropriateness of the modality given the pandemic and 13 patients praising the clear communication used with arranging the telephone visit.
Many participants identified the lack of ancillary testing as one of the biggest concerns they had about virtual visits. For instance, a participant mentioned, “I really appreciated [the videocall visit] but [.] I want to go in to get the visual field test that is a gold-standard measurement.” Most ancillary testing, including visual acuity, intraocular pressure, ocular coherence tomography, fundus photographs, and visual field testing could be performed face-to-face as a “testing-only visit” in 30 minutes or less. Testing without simultaneous in-person clinician consultation can greatly decrease wait times and waiting room occupancy and enable greater social distancing. Based on this experience, patient comments, and the potential benefits of this approach, our center has begun offering a hybrid care platform where a patient completes in-person testing and then participates in a video or phone visit with their clinician at a separate time. Although this hybrid model has not yet been studied extensively, we hypothesize that it may alleviate both patient and provider concerns of the lack of ancillary testing in virtual care and thereby increase utilization of virtual care in a specialty that is heavily reliant on testing and imaging to deliver care.
The study had several limitations. The majority of our participants were non-Hispanic white, thus limiting the generalizability of our results to the broader population in the United States. The open-ended interview of patients involved many interviewers, so each interview varied considerably in length and themes explored. However, given the sheer number of interviews conducted, we are confident that we have reached thematic saturation. Furthermore, given that our interview was entirely open-ended, the participants who shared their view may have felt more strongly inclined to share their view. For instance, individuals who had an extremely positive or negative experience with their visits are more likely to speak about their experience than those who may have had a slightly positive or slightly negative experience. Lastly, this was a descriptive study focusing on the initial utilization, safety, and patient experience with tele-ophthalmology. We did not directly investigate the deterioration of eye conditions or missed pathology as a result of patients being seen virtually, as this study was conducted during the shelter-in-place order in the state of Michigan where all nonurgent care was suspended. However, we did analyze and present the frequency of requiring an urgent in-person visit after being seen through a telemedicine visit, which was small. A total of 4.4% of those seen via telemedicine required an in-person visit within 1 week of their telemedicine visit.
In conclusion, our patient-centered assessment of tele-ophthalmology during the COVID-19 pandemic demonstrated that telemedicine can be used to provide care safely, with high patient satisfaction. Our mixed-methods approach to understanding our patients’ experience with their care during the pandemic lead us to hypothesize that a hybrid model of care combining in-person testing followed by a virtual physician consultation may improve efficiency, maintain safe distancing, and increase patient satisfaction. While the pandemic continues, leveraging tele-ophthalmology to deliver low-contact, low-wait ophthalmic care is necessary to provide high-quality care in a safe environment. However, based on how satisfied our participants were with their experiences with tele-ophthalmology, we suspect that virtual care will continue to be an important part of how eye care is delivered even after the COVID-19 pandemic. Further, with increasing globalization and travel, the world has experienced the rapid transmission of the COVID 19 virus parallel to the Spanish flu from 1 century before. Given the absolute uncertainty as to future global pandemics, the Centers for Disease Control and Prevention has recommended readiness strategies; and from an eye care provider perspective, this should include mechanisms to use telemedicine during such public health crises.19 Additionally, though global crises are relatively rare, ophthalmology should still be poised to deliver care during local crises, which arise more frequently.
Acknowledgments
Funding/Support: This work was supported by National Eye Institute (Bethesda, Maryland, USA; K23EY025320, P.A.N.C.; K23EY027849, L.D.L.; R01EY031033, M.A.W.), National Center for Advancing Translational Sciences (Bethesda, Maryland, USA; TL1TR002242, J.C.), and Research to Prevent Blindness (Career Development Award, P.A.N.C.). The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Financial Disclosures: The authors have no financial disclosures. All authors attest that they meet the current ICMJE criteria for authorship.
Drs De Lott and Newman-Casey served jointly as first authors.
Supplemental Material available at AJO.com.
Footnotes
Supplemental Material available at AJO.com.
Appendix. Supplementary materials
References
- 1.Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 - Cases in the US. 2020;2019:1-5. Available at https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed April 8, 2021.
- 2.Mervosh S., Lu D., Swales V. See Which States and Cities Have Told Reidents to Stay at Home. New York Times. 2020 https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html Available at. Accessed April 8, 2021. [Google Scholar]
- 3.Mehrota A., Chernew M.E., Linetsky D., Hatch H., Cutler D. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. The Commonwealth Fund. Available at https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. Accessed April 8, 2021.
- 4.Woodward M.A., Ple-plakon P., Blachley T., et al. Eye care providers’ attitudes towards tele-ophthalmology. Telemed e-Health. 2015;21:271–273. doi: 10.1089/tmj.2014.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Lott L.B., Newman-Casey P.A., Lee P.P., et al. Change in ophthalmic clinicians’ attitudes toward telemedicine during the Coronavirus 2019 pandemic. Telemed e-Health. 2021;27:231–235. doi: 10.1089/tmj.2020.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang S., Thomas P.B.M., Sim D.A., Parker R.T., Daniel C., Uddin J.M. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye. 2020;34:1193–1195. doi: 10.1038/s41433-020-0953-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kothari M., Rathod V., Sugathan S., Kothari M. A pilot study on the perspectives of pediatric ophthalmologists and their patients towards online consultation during COVID-19 lockdown in India. Indian J Ophthalmol. 2020;68:1494–1495. doi: 10.4103/ijo.IJO_1306_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gordon H.S., Solanki P., Bokhour B.G., Gopal R.K. I'm not feeling like i'm part of the conversation.” Patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med. 2020;35:1751–1758. doi: 10.1007/s11606-020-05673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valikodath N.G., Leveque T.K., Wang S.Y., et al. Patient attitudes toward telemedicine for diabetic retinopathy. Telemed e-Health. 2017;23:205–212. doi: 10.1089/tmj.2016.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baughman B.D., Hansemann B.K., Shah M.M., Weizer J.S. Drive-through intraocular pressure checks during the COVID-19 pandemic. J Glaucoma. 2021;30:223–226. doi: 10.1097/IJG.0000000000001748. [DOI] [PubMed] [Google Scholar]
- 12.Kodjebacheva G., Coleman A.L., Ensrud K.E., et al. Reliability and validity of abbreviated surveys derived from the National Eye Institute Visual Function Questionnaire: The study of osteoporotic fractures. Am J Ophthalmol. 2010;149:330–340. doi: 10.1016/j.ajo.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Community Survey. ACS 2014-2018 5-Year Estimates Now on Social Explorer. Available at https://www.socialexplorer.com/blog/post/acs-2014-2018-5-year-estimates-now-on-social-explorer-10261. Accessed April 8, 2021.
- 14.Bryant A., Charmaz K. SAGE Publications Ltd; London: 2007. The SAGE Handbook of Grounded Theory. [Google Scholar]
- 15.Chapman A., Hadfield M., Chapman C. Qualitative research in healthcare: An introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45:201–205. doi: 10.4997/JRCPE.2015.305. [DOI] [PubMed] [Google Scholar]
- 16.Glaucoma Research Foundation. National Glaucoma Research Foundation Survey Reveals Patients’ Experiences and Concerns During COVID-19. Available at https://www.glaucoma.org/news/national-glaucoma-research-foundation-survey-reveals-glaucoma-patients-experiences-and-concerns-duri.php. Accessed April 8, 2021.
- 17.Reddy J., Vaddavalli P., Sharma N., et al. A new normal with cataract surgery during COVID-19 pandemic. Indian J Ophthalmol. 2020;68:1269–1276. doi: 10.4103/ijo.IJO_1528_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tejwani S., Angmo D., Nayak B., et al. Preferred practice guidelines for glaucoma management during COVID-19 pandemic. Indian J Ophthalmol. 2020;68:1277–1280. doi: 10.4103/ijo.IJO_1724_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). National Pandemic Strategy | Pandemic Influenza (Flu). Available at https://www.cdc.gov/flu/pandemic-resources/national-strategy/index.html. Accessed April 8, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.