Abstract
Background
Public Health England guidance stipulates the use of filtering facepiece (FFP3) masks for healthcare workers engaged in aerosol-generating procedures. Mask fit-testing of respiratory protective equipment is essential to protect healthcare workers from aerosolized particles.
Aim
To analyse the outcome of mask fit-testing across National Health Service (NHS) hospitals in the UK during the first wave of the coronavirus disease 2019 (COVID-19) pandemic.
Methods
Using the Freedom of Information Act, 137 NHS hospitals were approached on May 26th, 2020 by an independent researcher to provide data on the outcome of fit-testing at each site.
Findings
Ninety-six hospitals responded to the request between May 26th, 2020 to October 29th, 2020. There was a total of 86 mask types used across 56 hospitals, 13 of which were used in at least 10% of these hospitals; the most frequently used was the FFP3M1863, used by 92.86% of hospitals. Overall fit-testing pass rates were provided by 32 hospitals with mean pass rate of 80.74%. The most successful masks, in terms of fit-test failure rates, were the Alpha Solway 3030V and the Alpha Solway S–3V (both reporting mean fit-test failures of 2%). Male- and female-specific pass and failure rates were provided by seven hospitals. Across the seven hospitals, 20.1% of men tested failed the fit-test for all masks used, whereas 19.9% of women tested failed the fit-test for all masks used. Failure rates were significantly higher in staff from Black, Asian, and Minority Ethnic (BAME) backgrounds 644/2507 (25.69%) across four hospitals.
Conclusion
Twenty percent of healthcare workers tested during the first response to the pandemic failed fit-testing for masks. A small sample revealed that this was most prominent in staff from BAME backgrounds.
Keywords: COVID-19, Fit-testing, Freedom of Information Act, FFP3, BAME
Introduction
The COVID-19 virus is transmitted principally via either inhaled respiratory droplets or physical contact. Public Health England (PHE) currently recommends droplet and contact precautions for professionals working with COVID-19 patients, alongside airborne precautions for aerosol-generating procedures (AGPs) [1]. Thus, respiratory protective equipment (RPE) has become a critical component of protecting the healthcare workforce. The filtering facepiece 3 respirator (FFP3) is the most widely RPE used within the UK healthcare system. FFP3 comes in many different forms and is defined by the European Union standards as set out in EN 149:2001 guidance, which states that an FFP3 mask must achieve a filter efficacy of >99% (for particles ≥0.3 μm) with a total inward leakage of <2% [2].
Guidance on the use of personal protective equipment (PPE) in health and social care workers was revised at the advent of the current COVID-19 pandemic. AGPs convey a higher risk of transmission and thus require enhanced protective measures for healthcare workers (HCWs) involved [1]. The greatest risk of transmission of respiratory viruses is during AGPs. PPE guidance advises the use of long-sleeved disposable fluid-repellent gowns, an FFP3 respirator, a full-face shield or visor, and gloves [1].
The Health and Safety Executive (HSE) is a UK government agency that regulates workplace health and safety. HSE directs that RPE fit-testing is essential to ensure that HCWs treating COVID-19 patients are fitted with an RPE that does not leak and is suitable for the wearer. Adequate respirator fit is vital, as poor fit can reduce the protective capacity of the respirator, thus increasing the risk of infection. HSE recognizes a variety of factors that could compromise the fit of RPE such as weight loss or gain, substantial dental work, facial pier-cings, and facial hair [3]. HSE provides a specific note on facial hair, highlighting that alternative forms of RPE are available for those who have good reason to have a beard (e.g. for religious reasons). The HSE does not, however, specifically recognize the potential for anthropomorphic differences between genders or ethnicities and how this could influence the adequacy of protection rendered by RPE and which could be putting female and Black, Asian, and Minority Ethnic (BAME) individuals at risk [4].
The potential for anthropomorphic differences in mask fit-testing failure rates has been studied in a previous large-scale prospective study which found that the highest mask fit-test failure rates were among Asian HCWs, and the lowest failure rates were among the White HCWs, with race being highly correlated with face shapes [5]. Han et al. assessed mask fit-testing in South Korea and identified that males were more suited for the three respirators in the study when compared with female staff [6].
Fit-testing is differentiated into qualitative or quantitative. Qualitative fit-testing is used widely for half-mask respirators such as FFP3s and is performed by assessing sense of smell or taste. By detecting the presence of bitter- or sweet-tasting aerosol as a measuring agent, the wearer subjectively assesses any leakage through the face mask. Quantitative assessment produces an objective numerical ratio comparing the proportion of aerosolized particles inside and outside the mask and can be used for all mask types [3].
In order to obtain information across the health service, the Freedom of Information (FOI) act 2000 and Freedom of Information (Scotland) Act 2002 enable requests for information to be made to any public body including NHS hospitals [7,8]. An FOI request consists of a written form of communication requesting the release of information from any number of public bodies who must release the information, if present, within 20 days, except if data is exempt. FOI allows researchers to obtain large data sets swiftly while maintaining an open and transparent culture within the NHS.
With the advent of the COVID-19 pandemic, widespread use of RPE in global healthcare systems has become mandatory protection for AGPs. Studies of mask fit-tests in the COVID-19 pandemic are limited. We present a prospective analysis of the results of a freedom of information request to NHS hospitals across the UK.
Methods
Setting
A retrospective analysis of RPE and fit-tests was conducted across healthcare staff working in UK NHS hospitals. This was achieved through a series of FOI requests sent on May 26th, 2020. These comprised specific criteria detailed below and were submitted to 137 acute UK NHS hospitals. Hospitals that provide community-based, mental health, and ambulance services were excluded. Responses collected until October 29th, 2020 were included.
Study population
NHS staff tested in 2020 for FFP3 masks before May 26th, 2020 of all ages were included. Staff working in private UK hospitals were not included. We were unable to ascertain whether bank staff working in a variety of hospitals accounted for multiple data points. Masks provided by three or more hospitals with pass and failure rates were included in the cross-mask comparison.
Outcome measurements
A single FOI request was sent to 137 UK NHS hospitals on May 26th, 2020. The FOI request asked for data collected during RPE fit-testing schemes across NHS hospitals. With regards to the RPE fit-testing, we asked for the genders of the participants, the associated pass rates, and whether qualitative or quantitative methods were used. We also asked hospitals to detail the specific mask types on which they performed fit-testing and to provide any further demographic data attached to participants that they had collected, such as age and ethnicity. Data were obtained via e-mail correspondence from various hospitals in the UK.
When comparing RPE fit-test failure rates between mask types, the number of failures was converted into a mean failure rate for mask type by weighting the number of fails by the total number of fit-tests carried out on that mask type, by hospitals that provided comparable data sets.
Our primary outcome was comparing mask-specific fit-test failure rates, to establish which mask performed best across hospitals. Secondary outcomes compared gender failure rates, mask-specific gender failure rates, ethnicity-related failure rates, and analysis of which mask types were most frequently used across hospitals. Overall failure rates for all masks were also evaluated if the data were provided by the hospital.
Statistical analysis
Statistical analysis was performed by an independent researcher using IBM SPSS version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistics included means and standard deviations presented where available. An independent samples t-test was used to assess continuous data, and categorical data were assessed using Pearson's χ2-test. If data values were <5 for categorical data, Fisher's exact test was used. Throughout, a 95% confidence interval was applied to test for significance, defined as P < 0.05.
Results
Hospital responses
Of the 137 FOI requests sent out, 96 responses were obtained between March 26th, 2020 and October 29th, 2020. All 96 hospitals had performed fit-testing of staff members. Of the 96 responses, 69 hospitals provided information that was pertinent to the FOI request to varying degrees. The remaining 68 hospitals were not included in the analysis for the following reasons: failing to respond prior to October 29th, 2020; not collecting the relevant information to answer the FOI request; not providing data in a format comparable to others; stating that answering the FOI request would exceed appropriate costs and time (as the data requested were not recorded in an easily retrievable format).
Masks most frequently used across hospitals
A total of 56 hospitals provided data regarding the different types of mask used by their staff. Across these 56 hospitals, the mask most frequently available was the 3M1863 (used by 52/56 hospitals, 92.86%). There was a total of 86 mask types reported across all 56 hospitals, 13 of which were used in at least 10% of these hospitals (Table I ; Appendix A). The remaining 73 mask types were only used in one to five hospitals; a comprehensive list of all mask types reported are listed in Appendix B.
Table I.
Types of mask used by >10% of the hospitals
| Mask type | No. of hospitals using mask type | Proportion of hospitals using mask type (%) |
|---|---|---|
| RFP3FV | 22 | 39.3 |
| 3M1863 | 52 | 92.9 |
| 3M1863+ | 25 | 44.6 |
| 3M1873V | 48 | 85.7 |
| 3M8833 | 44 | 78.6 |
| 3M7500 | 6 | 10.7 |
| 3M 9332+ Aura | 6 | 10.7 |
| Easimask FSM14 | 10 | 17.9 |
| Easimask FSM15 | 7 | 12.5 |
| Easimask FSM16 | 16 | 28.6 |
| Easimask FSM18 | 4 | 25.0 |
| Alpha Solway 3030V | 10 | 17.9 |
| Alpha Solway S3V | 8 | 14.3 |
The maximum number of mask types used in a single hospital was 24 (South Tees NHS Foundation Trust). The minimum number of mask types used in a single hospital was two (Royal Orthopaedic Hospital NHS Foundation Trust, Norfolk and Suffolk NHS Foundation Trust and Northumbria Healthcare NHS Foundation Trust). Across 56 hospitals the mean number of mask types offered by a single hospital was 6.9 (SD ± 4.3).
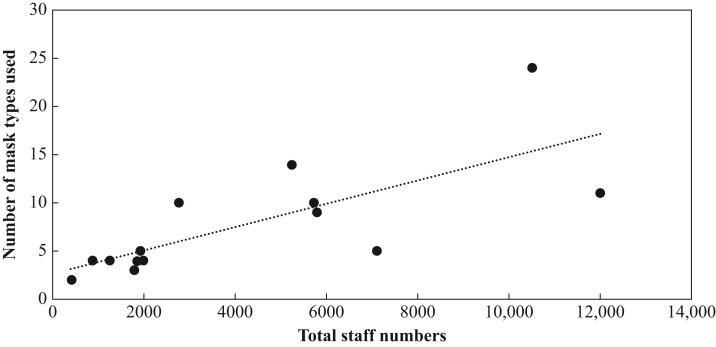
A total of 14 hospitals reported both their total staff numbers and the number of mask types available to these staff. A positive correlation was found between staff numbers and number of mask types available at hospitals (r = 0.75, P = 0.002) (Figure 1 ).
Figure 1.
Total staff numbers in a hospital compared with the number of mask types used within the hospital. A positive correlation was found (r = 0.75, P = 0.002).
Generic pass rates at hospitals
The overall fit-testing pass rates were provided by 32 hospitals. The mean percentage pass rate across these hospitals was 80.74%.
Mask-specific pass rates
A total of 12 hospitals provided data on how many staff passed or failed fit-testing on individual masks. Due to the high variability in masks used across hospitals (Appendix A), the masks compared here had to be used by at least three of these hospitals. Table II details the masks compared, their total, pass and fail fit-test numbers, and the average proportion of fit-test failures for each mask type, weighted according to the total number of fit-tests performed on that mask type across these hospitals. As seen in Table II the mask type with the highest mean proportion failure was the Honeywell Superone 3208 (mean fit-test failure of 67%) which was only reported to be used at four hospitals, three of which provided fit-test data. The 3M1873V had the second highest average proportion failure (mean fit-test failure of 47%) but was used more frequently across hospitals with 13 hospitals reporting its use, four of which provided fit-test data. The most successful masks, in terms of fit-test failure rates, were the Alpha Solway 3030V and the Alpha Solway S–3V (both reporting average fit-test failures of 2%); these masks had been used in ten and eight hospitals, respectively.
Table II.
Mask-specific fit-test failure rates and mean proportion fail across hospitals
| Mask | Total no. of tests | Pass | Fail | Proportion fail | Weight | Average proportion fail |
|---|---|---|---|---|---|---|
| RFP3FV | 396 | 58 | 60 | 0.51 | 0.30 | 0.36 |
| 107 | 15 | 0.12 | 0.31 | |||
| 0 | 6 | 1.00 | 0.02 | |||
| 14 | 16 | 0.53 | 0.08 | |||
| 60 | 35 | 0.37 | 0.24 | |||
| 16 | 9 | 0.36 | 0.06 | |||
| 3M1863 | 15,755 | 478 | 262 | 0.35 | 0.05 | 0.31 |
| 1114 | 831 | 0.43 | 0.12 | |||
| 1606 | 979 | 0.38 | 0.16 | |||
| 4212 | 1337 | 0.24 | 0.35 | |||
| 85 | 64 | 0.43 | 0.01 | |||
| 914 | 514 | 0.36 | 0.09 | |||
| 989 | 726 | 0.42 | 0.11 | |||
| 715 | 82 | 0.10 | 0.05 | |||
| 701 | 146 | 0.17 | 0.05 | |||
| 3M1863+ | 3193 | 527 | 192 | 0.27 | 0.23 | 0.28 |
| 1318 | 425 | 0.24 | 0.55 | |||
| 272 | 238 | 0.47 | 0.16 | |||
| 148 | 44 | 0.23 | 0.06 | |||
| 19 | 10 | 0.35 | 0.01 | |||
| 3M1873V | 2730 | 433 | 106 | 0.20 | 0.20 | 0.47 |
| 43 | 144 | 0.77 | 0.07 | |||
| 6 | 9 | 0.60 | 0.01 | |||
| 967 | 1022 | 0.51 | 0.73 | |||
| 3M8833 | 9885 | 715 | 128 | 0.15 | 0.09 | 0.24 |
| 331 | 165 | 0.33 | 0.05 | |||
| 1490 | 404 | 0.21 | 0.19 | |||
| 1386 | 447 | 0.24 | 0.19 | |||
| 48 | 8 | 0.14 | 0.01 | |||
| 745 | 414 | 0.36 | 0.12 | |||
| 1895 | 676 | 0.26 | 0.26 | |||
| 568 | 42 | 0.07 | 0.06 | |||
| 335 | 88 | 0.21 | 0.04 | |||
| EasiMask FSM 16 | 448 | 36 | 3 | 0.08 | 0.09 | 0.32 |
| 252 | 130 | 0.34 | 0.85 | |||
| 18 | 9 | 0.34 | 0.06 | |||
| EasiMask FSM 18 | 139 | 15 | 1 | 0.06 | 0.12 | 0.18 |
| 98 | 25 | 0.20 | 0.88 | |||
| Alpha Solway 3030V | 4226 | 4142 | 80 | 0.02 | 1.00 | 0.02 |
| 4 | 0 | 0.00 | 0.00 | |||
| Alpha Solway S–3V | 434 | 422 | 7 | 0.02 | 0.99 | 0.02 |
| 5 | 0 | 0.00 | 0.01 | |||
| Honeywell Superone 3204 | 881 | 103 | 205 | 0.67 | 0.35 | 0.67 |
| 192 | 377 | 0.66 | 0.65 | |||
| 0 | 4 | 1.00 | 0.00 |
Gender comparative failure rates
Data on the male:female ratio of staff members was provided by 23 hospitals. The mean across all hospitals was 76.49% females and 21.90% males.
Male- and female-specific pass and failure rates were provided by eight hospitals. These describe the numbers of male and female staff who passed or failed across all mask types on offer by that hospital. The total number of male staff who underwent fit-testing across these seven hospitals was 4863; the total number of female staff who underwent fit-testing across these seven hospitals was 17,920. Across all seven hospitals 18.98% of men tested failed the fit-test for all masks tested; 19.89% of women tested failed the fit-test for all masks used, χ2 = 0.079 (P = 0.398).
Gender failure rates on specific mask types
Gender-specific pass rates for specific mask types were reported by a single hospital. A total of 889 staff (642 females, 247 males) underwent RPE fit-testing within this hospital. Overall failure rates across all masks were significantly higher in women (225/642 (35.05%) vs 61/247 (24.70%) in men, χ2 = 8.76; P = 0.002). For 3M8833 and 3M1873V masks, women had significantly higher failure rates of 38/344 (11.05%) vs 6/138 (4.35%) in men (χ2 = 5.33; P = 0.013) and 62/90 (68.89%) in women vs 19/39 (48.72%) in men (χ2 = 4.74; P = 0.025), respectively. The 3M8833 mask was the second most frequently used across hospitals (44/56, 78.57%) and the 3M1873V was also reported to be used widely across hospitals (13/56, 23.21%). 3M1863, FSM18, CH0194, and SR100 did not show significantly different failure rates between men and women at this hospital.
Ethnicity-specific failure rates
Ethnicity-specific fit-test data were provided by four hospitals which gave the numbers of fit-test passes and failures according to each ethnicity. The different ethnicity subsets were broken down into two distinct groups for the purpose of our analysis: BAME and non-BAME. BAME is defined here as all non-white ethnic groups without relating to country origin or affiliation. Across these four hospitals, a total of 15,963 staff underwent RPE fit-testing; 13,456 of these staff were of non-BAME ethnicities whereas 2507 of these staff were of BAME ethnicities. Failure rates were significantly higher in staff from BAME backgrounds 644/2507 (25.69%) compared to those from non-BAME backgrounds (2265/13,456 (16.83%), χ2 = 111.2; P < 0.001).
Fit-testing methods
Hospitals were asked to disclose whether they used quantitative, qualitative, or both fit-testing methods. Of the hospitals responding to the FOI request, 58 disclosed their fit-testing methods. Quantitative fit-testing methods were used by 41/58 (70.7%) of these hospitals, while qualitative methods were used by 55/58 (94.8%). Both quantitative and qualitative methods were used concurrently at 37/58 (63.8%) of these hospitals.
Discussion
This is the first large-scale, detailed analysis of mask fit-testing outcomes during the first wave of the COVID-19 pandemic in the UK. We have identified potential factors that may have contributed to failed fit-tests, including ethnicity, mask type, and gender. Mask fit-testing of RPE is crucial to ensure adequate protection of frontline HCWs involved in AGPs, which pose the highest risk of transmission of COVID-19.
Pan et al. highlighted individuals of BAME to be a risk factor for mortality in patients who have contracted COVID-19 [9]. Ethnicity has been shown to have a significant impact on anthropometric facial features [10]. Our study found that BAME healthcare workers had a significantly higher mask fit-test failure rate by comparison with non-BAME. Contributing reasons for this outcome have been highlighted in previous studies [5,6,10]. Our analysis of four NHS hospitals has suggested a potential contributing factor for the increased risk of mortality of COVID-19 in BAME HCWs. The findings indicate that BAME may not be sufficiently protected by RPE, thus increasing their risk of contracting COVID-19. As data were provided by only four NHS hospitals, a larger sample size would help increase the statistical power of our results.
Across 56 NHS hospitals, 87 different mask types were reported with only 14 types being used in more than 10% of the hospitals. The supply of FFP3 masks in the UK is not standardized due to the variability of masks available at each NHS hospital. A single national supply of masks evenly distributed across all NHS hospitals may provide a better financial outcome and ensure standardized supply and fit-testing processes. It is noted that there may be possible duplications in the mask types reported as different hospitals may refer to the same mask with different terminology. This further emphasizes disparity between hospitals and the need for consistency across the board for NHS HCWs.
The number of mask types available within a hospital was compared with the number of personnel, and a positive correlation between the two factors was found. A wider range of masks allows a hospital to accommodate for the multitude of differences among staff members. As we work in an increasingly diverse NHS workforce, it is important to ensure that all HCWs have equal protection regardless of their gender or ethnicity. Another solution would be to have a tailored-to-fit mask design. A recent project supported by the Engineering and Physical Sciences Research Council (EPSRC) in collabor-ation with University of Birmingham and King's College London to produce a custom-fitted reusable FFP3, which is currently in prototype stage, may help provide a solution to individual facial phenotypes resulting in variable mask-fitting within the healthcare population [11].
Women and men are shown to have significantly different anthropometric facial features which could contribute to difference in RPE fit [10]. Fit-test failure rates across all masks were not found to be significantly different between genders when comparing outcomes from seven NHS hospitals. A similar conclusion was reached by Foreland et al., investigating outcomes for 701 fit-tests in the Norwegian smelting industry, a small study compared to our cohort of >20,000 HCWs [12]. One limitation of our analysis is that the data from the FOI request considered only binary genders and thus did not incorporate non-disclosed/non-binary genders. Data from a single hospital showed gender-related differences in fit-test failure rates on specific masks: women failed fit-testing significantly more than men with both the 3M883 and 3M1873V masks, two of the most frequently used types of mask across all hospitals (Table I). This would require further investigation across multiple hospitals as it could influence which mask types the hospitals should be supplying, given that the majority of HCWs are female.
The rate for a failed mask fit-testing across all hospitals was 19.6%. Although FOI responses did not provide information on the cause of a failed test, it is important that hospitals supply alternatives in the form of hoods/respirators in this circumstance. Multiple hospitals had reported the use of hoods/respirator masks with the most frequently used respirator being the 3M7500M model. In cases of failed fit-test, clinical exposure may be limited to reduce exposure to the virus; however, in cases where this could not be achieved, alternative PPE may be offered including hoods and powered air-purifying respirators (PAPR). PAPRs use a high-efficiency particulate air (HEPA) filter which filters 99.97% particles measuring 0.3 μm [13]. However, a recent study by Chakladar et al. identified that bacteria and fungi remain on the internal components of PAPRs despite disinfection following use. Another consideration with PAPRs is cost per unit of each respirator, which has a significant impact financially for hospitals, which in turn may limit the number of available respirators at each hospital [14].
Upon analysing the fit-test failure rates for each mask, it was noted that the 3M1873V had one of the higher failure rates while also being one of the most used masks across hospitals (Table I, Table II). The 3M1873V mask was also shown to have a higher fit-test failure rate in women at a single hospital. Conversely, the Alpha Solway 3030V and the Alpha Solway S–3V were found to have the lowest fit-test failure rates across hospitals but were only reported in a small proportion of hospitals (Table I, Table II). These findings emphasize the importance of collecting fit-test data, as it may influence the mask types supplied to HCWs.
The response rate to our FOI request was 70%, but only 72% of these responses yielded data that was pertinent to the request. This could be explained by multiple reasons. First, the FOI request was sent only once and was not re-sent for the 46 non-responders. Another contributing factor was that the COVID-19 pandemic was at a peak during this time, hence some hospitals did not have the resources to respond to the request. We accommodated for this by allowing a longer response time despite the legal obligation of a response within 20 days. Fit-testing is a legal requirement for all FFP3 masks as set out by the Control of Substances Hazardous to Health regulations and all 96 hospitals who responded had performed fit-testing of staff members; however, 27 hospitals reported not collecting the fit-test information pertinent to the FOI request and thus were excluded from the data analysis. Responses continued to arrive beyond the timeframe set by the study; however, in order to analyse and interpret the data in a timely manner, a deadline for these responses needed to be set. Ultimately, we obtained data outcome from 69 NHS hospitals, thus reducing the dataset size for analysis.
In all, 137 NHS hospitals had been sent an FOI request. Hospitals that provided community-based, mental health, and ambulance services were excluded as they would be less likely to have exposure to aerosolized particles and thus would not have used routine fit-testing in the first wave of the pandemic.
Qualitative fit-testing method was used by most hospitals (94.8%) that provided that data. The HSE guidance currently recommends that qualitative fit-testing methods are suitable only for disposable and reusable half-masks only, not full-face masks [3]. Quantitative fit-test methods were adopted to a lesser extent (70.7%). HSE guidance states that quantitative methods can be used for disposable masks, half-masks, and full-face masks. The two main quantitative methods include ambient particle counting and controlled negative pressure, which both utilize formulas to calculate the fit-factor specific to the wearer and the mask they are testing [3]. Both qualitative and quantitative methods were used concurrently by 63.8% of hospitals, with FOI responses mentioning that some hospitals began initially using qualitative methods, then introduced quantitative methods alongside once they had sourced the appropriate equipment. This highlights a lack of preparedness for wide-scale fit-testing and lack of consistency between hospitals with regards to fit-testing policy and equipment availability.
The responsibility of fit-testing lies upon both the individual and the hospital. It is important that the hospital provides the resources to carry out a fit-testing programme and to provide alternatives in the instance of a failed fit-test. The individual needs to take responsibility for fit-testing prior to entering a clinical area with a risk of COVID-19 exposure.
We would recommend all hospitals in the UK and worldwide to standardize data collection of mask fit-testing to incor-porate age, gender (including non-binary), ethnicity, mask types used, availability of mask types to inform future public health research on mask fit-testing and supply. This would help to ensure adequate protection of the entire healthcare workforce. Furthermore, our results have identified factors in addition to those mentioned by the HSE guidance for fit-testing. This includes age, gender, and ethnicity. Product design can be improved by manufacturers incorporating a diverse test population to test the best fit of mask designs.
Further research is required to investigate mask fit-testing. Investigation into the product design of RPE by manufacturers would be useful to understand what anthropomorphic measurements are used. The current FOI request did not ascertain whether hospitals routinely fit-tested HCWs prior to the COVID-19 pandemic. This would be a question to explore in further studies to ascertain whether it improved hospital preparedness and fit-testing outcomes during the pandemic.
In conclusion, this study is the first detailed analysis of mask fit-testing in UK NHS hospitals, and has shown potential contributing factors resulting in failed fit-tests, including ethnicity, sex, and mask type.
Acknowledgements
The authors wish to thank all NHS hospitals/trusts who have responded to the FOI request and for allowing us to use the data to analyse the outcome of RPE fit-tests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhin.2021.04.024.
Conflict of interest statement
None declared.
Funding sources
None.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Public Health England . 2020. COVID-19 personal protective equipment (PPE)https://www.gov.uk/government/collections/coronavirus-covid-19-personal-protective-equipment-ppe Available at: [last accessed February 2021] [Google Scholar]
- 2.European Centre for Disease Prevention and Control Using face masks in the community. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-use-face-masks-community.pdf 2020. Available at: [last accessed February 2021]
- 3.Health and Safety Executive . 2020. Guidance on respiratory protective equipment (RPE)https://www.hse.gov.uk/pubns/indg479.pdf Available at: [last accessed February 2021] [Google Scholar]
- 4.NHS Scotland . 2020. Assessing the evidence base for medical procedures which create a higher risk of respiratory infection transmission from patient to healthcare worker.https://hpspubsrepo.blob.core.windows.net/hps-website/nss/3055/documents/1_agp-sbar.pdf Version 1.1. Available at: [last accessed February 2021] [Google Scholar]
- 5.Wilkinson I.J., Pisaniello D., Ahmad J., Edwards S. Evaluation of a large-scale quantitative respirator–fit testing program for healthcare workers: survey results. Infect Control Hosp Epidemiol. 2010;31:918–925. doi: 10.1086/655460. [DOI] [PubMed] [Google Scholar]
- 6.Han D. Fit factors for quarter masks and facial size categories. Ann Occup Hygiene. 2000;44:227–234. [PubMed] [Google Scholar]
- 7.UK Ministry of Justice . 2000. Freedom of information act. [Google Scholar]
- 8.Scottish Ministers . 2002. Freedom of information (Scotland) act 2002. Edinburgh. [Google Scholar]
- 9.Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P., et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhuang Z., Landsittel D., Benson S., Roberge R., Shaffer R. Facial anthropometric differences among gender, ethnicity, and age groups. Ann Occup Hyg. 2010;54:391–402. doi: 10.1093/annhyg/meq007. [DOI] [PubMed] [Google Scholar]
- 11.UK Research, Innovation Custom-fit facemasks in 24 hours. 2020. https://www.ukri.org/our-work/tackling-the-impact-of-covid-19/addressing-technological-challenges/custom-fit-facemasks-in-24-hours Available at: [last accessed February 2021]
- 12.Foereland S., Robertsen O., Hegseth M.N. Do various respirator models fit the workers in the Norwegian smelting industry? Saf Health Work. 2019;10:370–376. doi: 10.1016/j.shaw.2019.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Licina A., Silvers A. Use of powered air-purifying respirator (PAPR) as part of protective equipment against SARS-CoV-2 – a narrative review and critical appraisal of evidence. Am J Infect Control. 2021;49:492–499. doi: 10.1016/j.ajic.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chakladar A., Jones C.G., Siu J., Hassan-Ibrahim M.O., Khan M. Microbial contamination of powered air purifying respirators (PAPR) used by healthcare staff during the COVID-19 pandemic: an in situ microbiological study. Am J Infect Control. 2021 Feb 13;S0196–6553(21) doi: 10.1016/j.ajic.2021.02.006. [Epub ahead of print]. S0196e6553(21)00061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.