Abstract
Spontaneous pneumothorax (SP) is characterized by the escape of broncho-alveolar air into presence of air in the pleural space without preceding blunt or penetrating trauma. SP requires prompt diagnosis and treatment. SP is divided into two groups as primary and secondary. Primary SP is usually seen in tall and thin patients with no clinically evident underlying lung disease (especially in tall and thin subjects), whereas secondary SP cases have an underlying lung disease, such as cystic lung disease, cavitary lung lesions, severe asthma, emphysema or pneumonia. Patients with Coronavirus-2019 (COVID-19) may experience the SP during the diagnosis and treatment processes, and it is a significant cause of morbidity. However, late-onset SP after recovering from COVID-19 is unusual. Herein we present a case with post-COVID-19 pulmonary fibrosis-like changes and subsequent late onset spontaneous pneumothorax (SP). We also present the patient's radiological findings.
Keywords: COVID-19; Pneumothorax; Fibrosis, computed tomography, complication
1. Introduction
Coronavirus disease-2019 (COVID-19) causes various pulmonary, vascular, neurological, and abdominal complications [[1], [2], [3]]. COVID-19-associated secondary spontaneous pneumothorax (SP) is a significant cause of morbidity, and many COVID-19 cases with SP at the time of initial diagnosis or during treatment have been reported [4]. However, late-onset SP in patients who recovered from COVID-19 is unusual. Only one case of late-onset SP has been reported in the literature that recovered from COVID-19 pneumonia and presented with SP on the 17th day of discharge [4]. Herein we present a case with post-COVID-19 pulmonary fibrosis-like changes and subsequent late onset spontaneous pneumothorax (SP). We also present the patient's radiological findings.
2. Case report
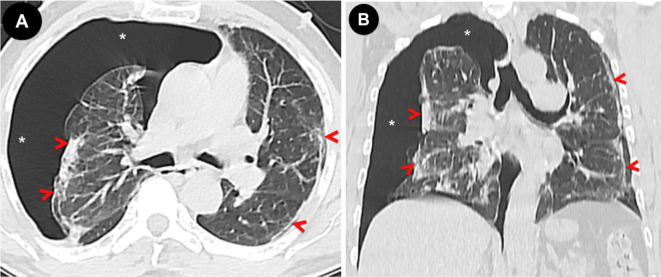
A 68-year-old male was admitted to the emergency room with complaints of severe dyspnea that started suddenly during sleep. The patient had a history of five days of hospitalization due to moderate coronavirus disease-2019 (COVID-19) three months prior to the current presentation (Fig. 1 ). The patient had a history of hypertension and hyperlipidemia for approximately eight years. The patient had no history of smoking and had a history of occasional shortness of breath with an effort that started after COVID-19 pneumonia. On physical examination, respiratory sounds in the right hemithorax were not detected. The oxygen saturation was 88% on room air, and the patient was tachypneic (22 breaths/min) at admission. The body temperature (36.1 degrees Celsius) and blood pressure (105/65 mmHg) of the patient were within normal limits. Chest computed tomography (CT) was obtained with a preliminary diagnosis of spontaneous pneumothorax. CT showed massive right pneumothorax, bilateral pulmonary fibrotic opacities (pleuro-parenchymal bands, subpleural irregularities, ground-glass opacities, and interstitial thickening) in the peripheral lung areas, and arcade-like atelectasis (Fig. 2 ). Pulmonary opacities were compatible with post-COVID-19 fibrotic-like lung opacities, and laboratory test results were within normal limits. A chest tube was placed through the right fifth intercostal space at the midaxillary line. The patient's complaints regressed rapidly, and the patient was discharged on the third day of admission. In further laboratory analysis for interstitial lung disease's possible etiology, rheumatoid antibodies, including rheumatoid factor and antinuclear antibody, were negative. The patient's follow-up for two months after discharge was uneventful.
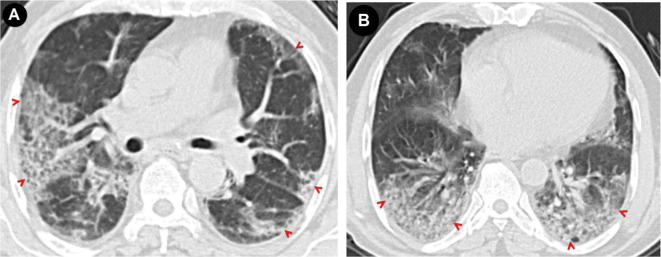
Fig. 1.
A, B: Axial chest CT images of the patient at the time of COVID-19 diagnosis (three months ago) show bilateral, peripheral consolidation and ground-glass opacities (arrowheads).
Fig. 2.
A) Axial and B) coronal chest CT images at current admission show massive right pneumothorax (*), bilateral pulmonary fibrotic opacities (pleuro-parenchymal bands, subpleural irregularities, ground-glass opacities, and interstitial thickening) in the peripheral areas (arrowheads).
3. Discussion
While fever, myalgia, cough, fatigue, and dyspnea are the most common symptoms in COVID-19 patients, it has been reported that approximately 1% of patients with COVID-19 may experience pneumothorax during the diagnosis and treatment processes [1,2]. High-pressure mechanical ventilation is the most common cause of the pneumothorax, pneumomediastinum, and pulmonary interstitial emphysema in COVID-19 patients. Moreover, spontaneous pneumothorax and pneumomediastinum can rarely be seen due to alveolar rupture in the course of the COVID-19 pneumonia and these are poor prognostic factors [3].
Recently, Sayan et al. [4] reported a never-smoker patient with spontaneous pneumothorax (SP) 17 days after recovery from COVID-19 pneumonia. The patient presented by Sayan et al. [4] had postinfectious ground-glass lung opacities, subsegmental atelectasis, and early fibrotic-like lung opacities on imaging. Similarly, our patient presented with bilateral pulmonary fibrotic opacities without any emphysematous lung areas. However, the delayed development of SP three months after the patient's initial COVID symptoms is novel.
4. Conclusions
The present case demonstrates that fibrotic-like lung opacities and spontaneous pneumothorax can be seen as of late complications of COVID-19. Both these complications should be kept in mind in patients with previous COVID-19 infection who present with abrupt onset of shortness of breath.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ufuk F., Bulgurcu E., Sari T. COVID-19-associated pancytopenia and typhlitis. Am J Emerg Med. 2021 Jan 4 doi: 10.1016/j.ajem.2020.12.049. S0735–6757(20)31169–4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bayraktaroğlu S., Çinkooğlu A., Ceylan N., Savaş R. The novel coronavirus pneumonia (COVID-19): a pictorial review of chest CT features. Diagn Interv Radiol. 2021 Mar;27(2):188–194. doi: 10.5152/dir.2020.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chougar L., Shor N., Weiss N., et al. Retrospective observational study of brain MRI findings in patients with acute SARS-CoV-2 infection and neurologic manifestations. Radiology. 2020;297(3):E313–E323. doi: 10.1148/radiol.2020202422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayan M., Turk M.S., Ozkan D., Kankoc A., Tombul I., Celik A. Hemopneumothorax as an unusual and delayed complication of coronavirus disease 2019 pneumonia. J Chest Surg. 2021 Feb 15 doi: 10.5090/jcs.20.149. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]