Abstract
Temporal visual field damage (VFD) is the common type of non-glaucomatous VF defects found in eyes with myopia. However, little is known about the factors associated with its progression. We investigated the characteristic of myopic eyes with progressive temporal VF defects. This retrospective, observational study included a total of 116 eyes: 39 eyes with temporal VFDs and an axial length greater than 24.5 mm, 77 eyes with typical glaucomatous VFDs who were followed up more than 5 years. VF progression was evaluated with Trend-based global progression analysis. In the temporal VFD group, the greater tilt ratios, the higher prevalence of β-zone peripapillary atrophy (β-PPA), the substantial increase in β-PPA were found, compared to the typical glaucomatous VFD groups (all P-values ≤ 0.001). The temporal VFD group had the slower progression than the typical glaucomatous VFD group on trend-based GPA (P = 0.047). In the multivariate linear regression analysis, the change of β-PPA area over years was related to temporal VFD progression (B, − 0.000088, P = 0.003). In conclusion, myopic eyes with the temporal VFD, which come with growing β-PPA area, should be monitored with extra caution.
Subject terms: Glaucoma, Optic nerve diseases, Refractive errors
Introduction
Myopia has become increasingly prevalent worldwide, especially in Asia1. Myopia could be a critical public health problem because it is associated with a risk of visual impairment2. In addition, myopia has been regarded as an independent risk factor for the development of glaucoma, and its high prevalence among glaucoma patients has been supported by epidemiological reports3,4.
Myopic eyes undergo the elongation of the posterior segment, and this elongation would result in structural changes to the optic nerve head (ONH) including tilt, torsion, and peripapillary atrophy (PPA)5–7. Considering the fact that diagnosis of glaucoma is based on characteristic ONH changes such as retinal nerve fiber layer (RNFL) loss with cupping, these bizarre degenerations around ONH may interrupt the accurate diagnosis of glaucoma based on structural changes.
In addition to ONH changes, visual field defect (VFD) is another essential requirement for the diagnosis of glaucoma. Therefore, when myopic patients present with stereotypical glaucomatous VFDs, the diagnosis is relatively easy and treatment can be initiated without hesitation. However, when it comes to atypical VFDs accompanied by structural myopic changes in the ONH, it is hard to decide whether the patient needs treatment.
Regarding VFDs in myopic eyes, several reports found that temporal VFDs, including enlarged blind spots, were the most frequently observed VFD in myopic patients8,9. In true glaucoma, however, the temporal VFD is not regarded as a typical type of the VFDs.
One study reported that some high myopic eyes without definite glaucoma showed a significant progression of VFDs9. Another study revealed that a gradual decrease in peripapillary RNFL thickness was observed, especially in older patients with high myopia10. Given those findings, there is a possibility that myopia-related VFD can progress, even though that is not a stereotypical glaucomatous VFD.
Little is known about the factors associated with the progression of VF damage in myopic patients with non-glaucomatous VFDs including temporal VFD. Understanding the clinical characteristics associated with the progression of VFD in these patients might help to provide the proper approach and better management for these populations.
In this study, we investigated the factors related to temporal VFDs and its progression in myopic patients, focusing on the temporal VFDs in myopic patients as non-classical glaucomatous VFDs. In addition, the characteristics of myopic patients with temporal VFDs were compared to those of patients with typical early glaucomatous VFDs.
Results
Among initially recruited 243 eyes, 127 eyes were excluded: 55 eyes due to less than three VF tests; 23 eyes with far advanced VFD; 33 eyes with VFD involving both periphery and center of VF test points; 12 eyes invading both the edge and periphery of the field; and 4 eyes with neurological disease.
A total of 116 eyes of 116 patients, with the mean follow-up 80.34 ± 18.56 months, were finally participated in this study, and according to VFD location, the numbers of patients are following: 39 myopic eyes with the temporal VFD and 79 eyes with typical glaucomatous VFD. Typical glaucomatous VFD group included 37 eyes with the peripheral VFD and 40 eyes with the paracentral VFD.
The patient demographics are shown in Table 1. Patients in the temporal VFD group had the significantly higher prevalence of hypertension (P = 0.025). As for glaucoma medication, although more than two third of the temporal VFD group was on glaucoma medication, the percentage of the patient and the number of the eyedrops were substantially lower compared to typical glaucomatous group. Regarding axial length, the temporal VFD group had the longer eyes(P < 0.001).
Table 1.
Patients demographics (Total 116 eyes).
| Temporal VFD (N, 39) | Typical glaucomatous VFD (N, 77) | P value | ||
|---|---|---|---|---|
| Age, mean (SD), year | 52.49 (13.66) | 56.12 (12.65) | 0.158a | |
| Female, No. (%) | 30 (76.9) | 47 (61.0) | 0.087b | |
| Laterality, No. (%) | OD | 21 (53.8) | 40 (51.9) | 0.847b |
| OS | 18 (46.2) | 37 (48.1) | ||
| HTN (No. (%)) | 1 (2.6) | 13 (16.9) | 0.025b | |
| DM (No. (%)) | 2 (5.1) | 4 (5.2) | 0.988b | |
| Aspirin (No. (%)) | 0 (0) | 4 (5.2) | 0.147b | |
| Migraine (No. (%)) | 4 (10.3) | 7 (9.1) | 0.840b | |
| Cold hands/ feet (No. (%)) | 4 (10.3) | 310(13.0) | 0.670b | |
| Baseline IOP, mean (SD), mmHg | 16.08 (3.32) | 15.44 (3.19) | 0.320a | |
| Final IOP, mean (SD), mmHg | 15.00 (2.86) | 14.25 (3.14) | 0.211a | |
| Number of patients with medication (No. (%)) | 28 (71.8) | 77 (100) | < 0.001b | |
| Number of medications, mean (SD), n | 1.03 (0.81) | 1.75 (0.79) | < 0.001a | |
| CCT, mean (SD), μm | 536.34 (55.96) | 536.74 (36.17) | 0.969a | |
| Axial length, mean (SD), mm | 27.74 (2.29) | 24.70 (1.62) | < 0.001a | |
| Number of VF test, mean (SD), n | 6.59 (1.39) | 6.10 (1.10) | 0.052a | |
| Total follow-up period, mean (SD), month | 86.43 (14.49) | 81.90 (20.20) | 0.072a | |
| Visual field test | MD, mean (SD), dB | − 3.23 (2.84) | − 2.98 (1.63) | 0.618a |
| PSD, mean (SD), dB | 4.83 (2.16) | 4.94 (2.37) | 0.807a | |
VFD visual field defect, HTN hypertension, DM diabetes mellitus, IOP intraocular pressure, n number, CCT central corneal thickness, VF visual field, MD mean deviation, PSD pattern standard deviation, dB decibel.
Mean values are presented with standard deviations aStudent’s t-test after Propensity score match, bchi-squared test.
Bold font indicates significant P values (P < 0.05).
Distribution of each VFD group in hemispheres was different. For the temporal VFD groups, VF loss was prominent in inferior hemisphere or in both hemispheres. Unlike the temporal VFD group, the typical glaucomatous VFD group saw a noticeable VF loss in superior hemisphere, and the difference between the two groups was significant. (P < 0.001) (Fig. 1).
Figure 3.
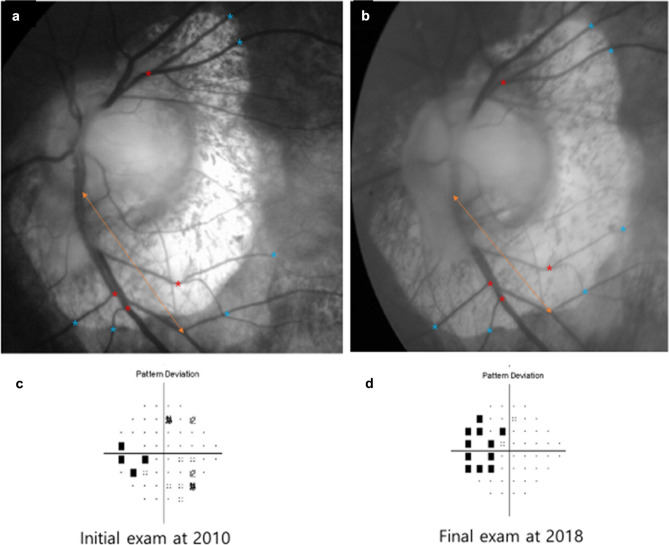
A Representative case with Enlargement of β-Peripapillary Atrophy. 59 years old female patient with axial length 28.41 mm showed that the overall change of β- PPA area over year was 12,115.8 pixel/year (a and b) and progression of the temporal visual field defect was observed (c and d).
The β-PPA measurements showed excellent reproducibility for the initial and final β-PPA areas (ICC = 0.874–0.996, ICC = 0.907–0.981, respectively), final disc area (0.871–0.988) (Table 2). The reproducibility for initial disc area was moderate to excellent (ICC = 0.710–0.778).
Table 2.
Reliability of β-zone PPA parameters.
| Variables | Temporal VFD (N, 39) | Typical glaucomatous VFD (N, 77) | |||
|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | ||
| β-zone PPA | Area of Initial β-zone PPA, mean (SD), pixel | 0.996 | 0.992–0.998 | 0.874 | 0.681–0.950 |
| Area of Initial disc, mean (SD), pixel | 0.778 | 0.488–0.904 | 0.710 | 0.267–0.885 | |
| Area of Final β-zone PPA, mean (SD), pixel | 0.907 | 0.786–0.960 | 0.981 | 0.954–0.992 | |
| Area of Final disc, mean (SD), pixel | 0.871 | 0.702–0.944 | 0.988 | 0.970–0.995 | |
VFD visual field defect, ICC intraclass correlation coefficient, PPA peripapillary atrophy.
Reproducibility of β-zone PPA parameters: excellent for areas of initial and final β-zone PPA of both groups, final disc areas of both groups, and initial disc area of temporal VFD group; moderate for initial disc area of typical glaucomatous VFD group.
The parameters related to optic discs and OCT were compared between two groups (Tables 3 and 4). The prevalence of the optic disc tilt and the degree of the tilt ratio were significantly greater in the temporal VFD group, compared to the other group (All P-values ≤ 0.001). All parameters related to β-PPA showed significantly greater values in the temporal VFD group than in the typical glaucomatous VFD group (All P-values < 0.001). As to OCT parameters (Table 4), the typical glaucomatous VFD group saw the substantially lower values in average, nasal, and temporal RNFL thicknesses, and average, inferonasal, inferior, and inferotemporal GCIPL thicknesses compared to the temporal VFD group.
Table 3.
Comparison of optic disc and posterior pole profiles.
| Variables | Temporal VFD (N, 39) | Typical glaucomatous VFD (N, 77) | P value | |
|---|---|---|---|---|
| Manually measured cup to disc ratio, mean (SD) | 0.67 (0.21) | 0.70 (0.17) | 0.349a | |
| Presence of Disc hemorrhage, (No. (%)) | 3 (7.7) | 14 (18.2) | 0.131b | |
| Optic disc tilt | Presence of Tilted disc (No. (%)) | 28 (71.8) | 17 (22.1) | < 0.001b |
| Tilt ratio, mean (SD) | 1.42 (0.23) | 1.21 (0.30) | < 0.001a | |
| Optic disc rotation | Rotation angle, mean (SD), ° | 5.04 (19.42) | − 1.00 (20.87) | 0.136a |
| Significant rotation (No. (%)) | 16 (41.0) | 41 (54.7) | 0.167b | |
| Inferior rotation (No. (%)) | 29 (74.4) | 38 (50.7) | 0.015b | |
| β-zone PPA | Presence (No. (%)) | 34 (87.2) | 39 (50.6) | < 0.001b27 |
| Area of Initial β-zone PPA, mean (SD), pixel | 62,451.3 (52,461.7) | 13,369.8 (7316.6) | < 0.001a | |
| Change of β-zone PPA over years, mean (SD), pixel/year | 3285.5 (3585.9) | 237.4 (782.8) | < 0.001a | |
VFD visual field defect, PPA peripapillary atrophy.
aStudent’s t-test after Propensity score match, bchi-squared test.
Bold font indicates significant P values (P < 0.05).
Table 4.
Comparison of optical coherence tomography parameters.
| Variable | Temporal VFD (N, 39) | Typical glaucomatous VFD (N, 77) | P value | |
|---|---|---|---|---|
| Optic disc parameters | Rim area, mean (SD) | 1.47 (0.78) | 0.90 (0.20) | < 0.001 |
| Disc area, mean (SD) | 2.76 (1.43) | 2.03 (0.59) | 0.005 | |
| Average cup to disc ratio, mean (SD) | 0.82 (0.23) | 0.75 (0.14) | 0.072 | |
| Vertical cup to disc ratio, mean (SD) | 0.75 (0.28) | 0.74 (0.14) | 0.812 | |
| Cup volume, mean (SD) | 0.30 (0.25) | 0.48 (0.30) | 0.004 | |
| Parapapillary RNFL thickness (μm) | Average, mean (SD) | 86.97 (16.14) | 77.88 (9.50) | 0.003 |
| Superior, mean (SD) | 92.70 (24.49) | 95.86 (20.10) | 0.484 | |
| Nasal, mean (SD) | 74.58 (24.06) | 63.58 (9.54) | 0.010 | |
| Inferior, mean (SD) | 96.91 (24.93) | 87.98 (16.76) | 0.056 | |
| Temporal, mean (SD) | 83.96 (23.56) | 64.23 (14.96) | < 0.001 | |
| GCIPL thickness (μm) | Average, mean (SD) | 78.13 (9.64) | 71.01 (7.08) | < 0.001 |
| Minimum, mean (SD) | 64.89 (19.04) | 58.87 (10.77) | 0.105 | |
| Superior, mean (SD) | 73.27 (14.63) | 73.47 (9.90) | 0.945 | |
| Superonasal, mean (SD) | 81.38 (17.05) | 78.52 (7.83) | 0.373 | |
| Inferonasal, mean (SD) | 80.17 (13.42) | 73.77 (8.34) | 0.005 | |
| Inferior, mean (SD) | 73.01 (12.39) | 64.64 (10.65) | < 0.001 | |
| Inferotemporal, mean (SD) | 79.81 (14.39) | 63.54 (10.93) | < 0.001 | |
| Superotemporal, mean (SD) | 80.85 (15.31) | 71.26 (10.00) | 0.309 | |
Values obtained from optical coherence tomography was corrected with the Littmann’s formula.
VFD visual field defect, RNFL retinal nerve fiber layer, GCIPL ganglion cell inner plexiform layer.
Mean values are presented with standard deviations.
Student’s t-test after Propensity score match.
Bold font indicates significant P values (P < 0.05).
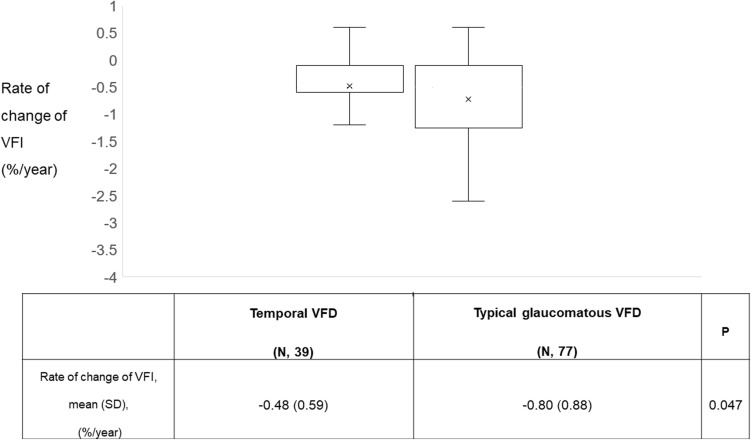
In terms of VFD progression, temporal VFD group had a noticeably slower progression rate than typical glaucomatous VFD group (− 0.49 ± 0.59, − 0.80 ± 0.88, P = 0.047) (Fig. 2).
Figure 4.
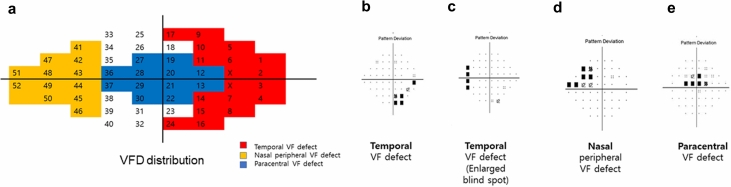
Visual Field Defect (VFD) regions. The distribution of the VFD regions is shown on (a). Blue region stands for paracentral VFD, while red region is classified as temporal VFD. Rest regions fall into the category for peripheral VFD. X regions corresponds to the blind spots. (b) and (c) show examples of the temporal VFD, while (d) and (e) describe nasal peripheral VFD, and paracentral VFD, respectively.
In multivariate analysis to determine the parameters associated with VFD progression using trend-based GPA, manually measured cup to disc ratio, tilt ratio and change of β-zone PPA over years were noticeable factors in univariate analysis, however, in multivariate analysis, tilt ratio was of the most significant association (B, 1.063, P = 0.011) (Table 5).
Table 5.
Linear regression analysis to Determine the Correlation between Variables and Visual Field defect progression (trend- based GPA) in All eyes (N, 116).
| Variable | Univariate | Multivariate1 | |||
|---|---|---|---|---|---|
| B | P value | B | P value | ||
| Age | − 0.009 | 0.214 | |||
| Baseline intraocular pressure | − 0.025 | 0.356 | |||
| Dependency on medication | 0.082 | 0.798 | |||
| Central corneal thickness | − 0.003 | 0.196 | |||
| Axial length | 0.012 | 0.741 | |||
| Manually measured cup to disc ratio | − 1.118 | 0.015 | |||
| Tilt ratio | 1.063 | 0.011 | 1.063 | 0.011 | |
| Rotation degree | 0.005 | 0.339 | |||
| Parameters for PPA | Initial PPA area | − 0.000001 | 0.613 | ||
| Change of β-zone PPA over years | − 0.000043 | 0.184 | |||
| Optical coherence tomography | Average RNFL thickness | 0.007 | 0.262 | ||
| Average GCIPL thickness | 0.008 | 0.447 | |||
| Visual field test | MD | − 0.057 | 0.145 | ||
| PSD | − 0.009 | 0.810 | |||
| Type of visual field defect | Temporal | 0.323 | 0.074 | ||
GPA guided progression analysis, PPA peripapillary atrophy, RNFL retinal nerve fiber layer, GCIPL ganglion cell inner plexiform layer, MD mean deviation, PSD pattern standard deviation.
Average RNFL and GCIPL thicknesses were corrected with the Littmann’s formula.
Only variables with a P value < 0.10 in the univariate analysis were included in the multivariate model.
(Multivariate1 Analysis with stepwise or forward method, while Multivariate2 Analysis with backward method).
Bold font indicates significant P values (P < 0.05).
Meanwhile, in the analysis of the temporal VFD progression, manually measured cup to disc ratio, initial PPA area, change of β-zone PPA over years were significant in univariate analysis. Among those, it was change of β-zone PPA over years that had the most significance in multivariate analysis (B, − 0.000088, P = 0.003) (Table 6).
Table 6.
Linear regression analysis to determine the correlation between variables and visual field (VF) defect progression (trend- based GPA) in temporal VF defect group (N, 39).
| Variable | Univariate | Multivariate1 | |||
|---|---|---|---|---|---|
| B | P value | B | P value | ||
| Age | − 0.009 | 0.277 | |||
| Baseline intraocular pressure | − 0.031 | 0.324 | |||
| Dependency on medication | 0.361 | 0.155 | |||
| Central corneal thickness | − 0.002 | 0.342 | |||
| Axial length | − 0.018 | 0.699 | |||
| Manually measured cup to disc ratio | − 0.983 | 0.043 | |||
| Tilt ratio | 0.697 | 0.115 | |||
| Rotation degree | 0 | 0.960 | |||
| Parameters for PPA | Initial PPA area | − 0.000004 | 0.059 | ||
| Change of β-zone PPA over years | − 0.000088 | 0.003 | − 0.000088 | 0.003 | |
| Optical coherence tomography | Average RNFL thickness | 0.009 | 0.123 | ||
| Average GCIPL thickness | 0.002 | 0.852 | |||
| Visual field test | MD | − 0.022 | 0.551 | ||
| PSD | − 0.009 | 0.857 | |||
GPA guided progression analysis, MD mean deviation, PSD pattern standard deviation, RNFL retinal nerve fiber layer, GCIPL ganglion cell inner plexiform layer, PPA peripapillary atrophy.
Average RNFL and GCIPL thicknesses were corrected with the Littmann’s formula.
Only variables with a P value < 0.10 in the univariate analysis were included in the multivariate model.
Bold font indicates significant P values (P < 0.05).
Based on the finding that increment in β-zone PPA was a significant factor in VFD progression in the temporal VFD group, we divided the patients of the temporal VFD group according to the presence of β-PPA progression. The patients with enlargement in β-zone PPA had lower tilt ratio, but vaster initial β-zone PPA, rim, and disc areas, and remarkable amount of β-zone PPA growth over years compared to those without enlargement in β-zone PPA (All P-values ≤ 0.002) (Table 7).
Table 7.
Comparison of optic disc and optical coherence tomography parameters in eyes of the temporal visual field defect group in terms of presence of β-zone PPA progression.
| Variable | Enlargement in β-zone PPA (N, 21) | No Enlargement in β-zone PPA (N, 14) | P value | |
|---|---|---|---|---|
| Manually measured cup to disc ratio, mean (SD) | 0.74 (0.19) | 0.60 (0.20) | 0.058 | |
| Tilt ratio, mean (SD) | 1.35 (0.16) | 1.61 (0.22) | < 0.001 | |
| Rotation angle, mean (SD), ° | 3.99 (21.38) | 10.22 (10.95) | 0.275 | |
| Area of Initial β-zone PPA, mean (SD), pixel | 90,192.8 (50,250.9) | 22,820.5 (20,504.0) | < 0.001 | |
| Change of β-zone PPA over years, mean (SD), pixel/year | 5249.8 (3522.5) | 479.4 (301.5) | < 0.001 | |
| Direction of β-zone PPA enlargement (No. (%)) (Inferotemporal/ Temporal/ Superonasal / Superotemporal) | 10 / 7/ 3/ 1 (47.6%/ 33.3%/ 14.3%/ 4.8%) | NA | ||
| Optic disc parameters | Rim area, mean (SD) | 1.79 (0.86) | 1.16 (0.50) | 0.018 |
| Disc area, mean (SD) | 3.46 (1.62) | 2.05 (0.62) | 0.002 | |
| Average cup to disc ratio, mean (SD) | 0.89 (0.21) | 0.75 (0.25) | 0.071 | |
| Vertical cup to disc ratio, mean (SD) | 0.82 (0.25) | 0.68 (0.33) | 0.162 | |
| Cup volume, mean (SD) | 0.32 (0.29) | 0.27 (0.22) | 0.633 | |
| Parapapillary RNFL thickness (μm) | Average, mean (SD) | 90.49 (16.49) | 85.79 (15.98) | 0.415 |
| Superior, mean (SD) | 99.92 (24.85) | 86.55 (23.61) | 0.125 | |
| Nasal, mean (SD) | 82.23 (23.86) | 69.17 (23.83) | 0.126 | |
| Inferior, mean (SD) | 89.63 (25.04) | 105.45 (25.63) | 0.082 | |
| Temporal, mean (SD) | 90.22 (22.06) | 82.48 (24.34) | 0.342 | |
| GCIPL thickness (μm) | Average, mean (SD) | 80.22 (11.43) | 77.35 (8.73) | 0.462 |
| Minimum, mean (SD) | 61.67 (24.09) | 67.83 (16.15) | 0.435 | |
| Superior, mean (SD) | 74.25 (18.40) | 73.96 (12.49) | 0.962 | |
| Superonasal, mean (SD) | 85.80 (17.15) | 79.01 (18.80) | 0.327 | |
| Inferonasal, mean (SD) | 82.15 (14.54) | 79.57 (13.67) | 0.633 | |
| Inferior, mean (SD) | 70.71 (16.23) | 75.04 (8.51) | 0.387 | |
| Inferotemporal, mean (SD) | 81.51 (19.84) | 78.50 (9.16) | 0.610 | |
| Superotemporal, mean (SD) | 86.96 (19.43) | 77.56 (9.45) | 0.116 | |
Progression of β-zone PPA was defined with a change of β-zone PPA area over 1000 pixel /year.
PPA peripapillary atrophy, NA not available, RNFL retinal nerve fiber layer, GCIPL ganglion cell inner plexiform layer.
Values obtained from optical coherence tomography was corrected with the Littmann’s formula.
Student’s t test.
Bold font indicates significant P values (P < 0.05).
aBonferroni correction for multiple measurement comparison was applied, and a level of significance was set at 0.002 (0.05/23).
Additionally, we further analyzed the data after applying 1:1 propensity-score matching for axial length, and a total of 54 eyes was included: 27 eyes for temporal VFD group and 27 eyes for typical glaucomatous VFD group. After 1:1 propensity-score matching, the mean axial length was 26.77 ± 1.15 mm for temporal VFD group, 26.21 ± 1.04 mm for typical glaucomatous VFD group (P = 0.061), and no significant differences except the percentage of the patient with eyedrops and the number of glaucoma medication were found (Supplementary Table S1 online). In terms of factors related to temporal VFD progression, unlike high myopic eyes, average RNFL thickness and manually measured cup to disc ratio were significantly associated with the VFD progression (B, 0.014, P = 0.022, B, − 1.086, P = 0.019, respectively) (Supplementary Table S2 online). However, in axial length -matched typical glaucomatous VFD group, there was no significant factors related to its VFD progression (Supplementary Table S3 online).
A representative case of a patient with progressive temporal VFDs is shown in Fig. 3. Figure 3 highlights that the progression of temporal VFDs in eyes with β- PPA enlargement was prominent (Fig. 3a–d).
Figure 5.
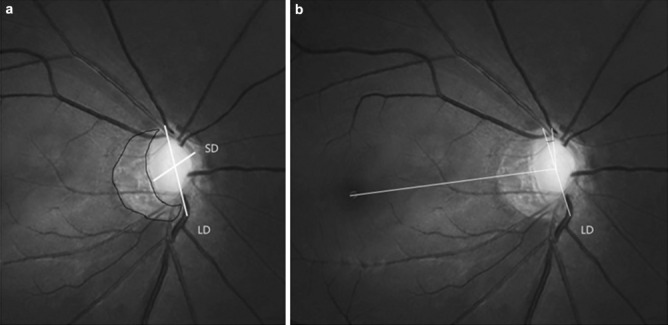
Identification of Tilt ratio, β-Peripapillary Atrophy area, and Torsion degree. (a) Tilt ratio was defined as the ratio between the longest diameter and the shortest diameter of the optic disc. The border of β-peripapillary atrophy area was drawn manually with ImageJ software, and the pixel are was calculated automatically. (b) Torsion degree was defined as the angle between the longest diameter and the vertical meridian of the optic disc, which meant a vertical line 90 degrees from the reference line connecting the fovea to the center of the optic disc. LD longest diameter, SD shortest diameter.
Discussion
In this study, we found that eyes with myopia and temporal VFDs had prominent development and changes in β-PPA than typical glaucomatous VFD group. In the temporal VFD group, incremental β-PPA changes was associated with deterioration in the VF.
In this study, eyes with temporal VFDs showed myopic features including larger β-PPA areas than those with typical glaucomatous VFDs. The previous study suggested that myopic eyes with VFDs presented more extensive β-PPA than those without VFDs11, which were consistent with our findings. Regarding the presence of temporal VFDs in myopic eyes, there are some possible explanations. First, the β-PPA area is histologically known as having a complete loss of retinal pigment epithelial cells and decrease in retinal photoreceptors12–15. Temporal VFDs, including enlarged blind spots, might be connected to the histological changes in β-PPA. Secondly, we presume that RNFL axonal damage, as a consequence of myopic optic disc deformation, might affect the development of temporal VFDs. Along with axial elongation, defects like peripapillary scleral stretching and bending could be generated, and these defects might lead to damage to peripapillary deep structures including RNFL axons. According to Akagi et al11, in myopic patients with β-PPA, temporal scleral protrusion was detected in the eyes with VFD, and the angle of the temporal scleral bending correlated significantly with RNFL thickness above the scleral bending and VFD severity. In our study, significant differences in almost average RNFL thickness and average GCIPL thickness regions were found between the temporal VFD group and the typical glaucomatous VFD group. Although the values of the temporal VFD group were higher, they were far from within normal limit values. We presumed that this finding might reflect that RNFL damage also occurred concurrently with myopic optic nerve head deformation, but the degree of the damage might be subtle compared to general glaucomatous eyes.
In terms of the VFD progression rate, a significant difference was found between the two groups. Namely, although the progression rate was slower in temporal VFD group, there was a definite VF aggravation in some temporal VFD patients. This result was inconsistent with the previous study’s findings in young Chinese male patients with glaucoma or glaucoma suspect who had myopia and tilted optic discs and showed nonprogressive patterns of the VFD16. However, there were only 16 subjects in the study, which was not enough to generalize the findings. On the contrary to the precedent study, Ohno-Matsui et al9 reported that temporal VFDs were the most commonly observed VFD in high myopic, non-glaucomatous eyes, and those who had temporal VFDs showed aggravated VFDs.
As to the factor associated with VFD progression in all eyes, lower tilt ratio was the ultimate determinant. Tilt ratio as a contributor to VFD progression has been still on debate. Namely, Lee et al17 found that tilt ratio was not associated with VF progression rate, while Choy et al18 reported there were more VFDs found in eyes with increasing tilt ratio. In our study, compared to typical glaucomatous VFD group, temporal VFD group had greater tilt ratio and its progression rate was slower. We assumed that greater tilt ratio in the temporal VFD group might affect the results on VFD progression in multivariate analysis, even though the temporal VFD group itself did not remain as the significantly associated factor with progression of VFD.
Meanwhile, in myopic patients with the temporal VFD, our study revealed that incremental changes in β-PPA over time was associated with temporal VFD progression. According to previous findings, in glaucoma patients with myopia, growing β-PPA was associated with the progression of VFDs19. There also have been a report of changes in the extent of β-PPA in elderly myopic patients20. However, to our best knowledge, no study has found a direct relationship between changes in the β-PPA area and progression in VFDs in elderly myopic patients without definite glaucoma.
To explain these findings, we hypothesized some possible theories for the association between the progression of β-PPA and the aggravation of temporal VFDs. The first feasible explanation is that aggravation of temporal VFDs might be due to progressive degeneration in the outer retina, including the photoreceptor cells, followed by enlargement of the β-PPA area. Secondly, according to Chen et al.21, myopic eyes with profuse PPA showed choroidal thinning and decreased choroidal blood supply. In this regard, the disrupted choroidal blood circulation might result in insufficient blood supply to the ONH and thus, incremental changes in PPA could have an impact on the progression of VFDs. Lastly, the progression of temporal VFDs might be the co-result of retinal ganglion cell damage. This could be supported by our finding that the temporal VFD patients with progressive temporal VFD had thinner RNFL or GCIPL thickness as shown in supplemental Table 2.
In typical glaucomatous VF defect group, regarding factors related to VFD progression, a plethora of factors such as disc hemorrhage22–25, age26, baseline IOP26, inadequate IOP control24,25,27, tilt ratio28–30 and its direction31,32 were reported. However, there are still on-going controversies over these risk factors’ contribution to disease progression. In our study, none of the parameters were found to be significant. We presume these discrepancies between the studies might stem from assessment of patients with different severity; compared to the studies above, our study included the patients with the earliest stage of the disease in terms of MD. Also, small sample size might have led to this conclusion.
As for the direction of β-PPA enlargement, Bak et al.33 reported that inferotemporal area for primary open angle glaucoma (POAG), and the temporal area for normal eyes were the most frequent directions of expansion. Previous studies suggested that the direction of β-PPA enlargement was in accordance with that of RNFL defects in glaucomatous eyes34,35. Our study found that the direction of β-PPA enlargement was in the order of the inferotemporal area, followed by the temporal, superonasal, and superotemporal areas (Table 7). This distribution might imply that even myopic eyes without typical glaucomatous features could have some features of glaucomatous β-PPA.
Limitations
First, our sample sizes were modest and this could mean other variables may not have been fully represented in the present study. However, the total follow-up period for all patients was more than six years, and this long-term follow-up might compensate for the weakness of the sample size. Second, due to weaknesses in a retrospective study including selection bias and lack of clarification of causal relationship, a prospective and longitudinal investigation is necessary. Third, since this study was conducted in a retrospective manner, we could not keep tracing changes of the AL. Nevertheless, we could not find the development or existence of posterior staphyloma, and thus, we presume there would have not been an extreme change in axial length. Lastly, thorough and specific analysis of other retinal layers including photoreceptor layer might have been helpful for better understanding of their impacts on temporal VF progression. Due to the fact that the whole OCT images were acquired from the Cirrus- OCT, it was impossible to perform more rigorous segmentation of the images. Future studies using swept-source OCT would be necessary to see the relationship between other retinal layers and the VFD progression.
Conclusions
Myopic eyes with temporal VFDs demonstrated larger β-PPA areas, and slower VFD progression rate than glaucoma patients with typical VFDs. Among the myopic eyes with temporal VFDs, the eyes with increment in β-PPA area over years were predisposed to VFD progression. It has not been easy to tell high myopic patients with massive structural deformations around the ONH about the prognosis and predisposing factors associated with progression of atypical VFD. We believe our findings could be a tangible back-up resource when it comes to looking after those patients. It is never enough to stress the importance of extra-attention and care to myopic patients, particularly with presenting growing β-PPA.
Patients and methods
This retrospective, observational study was approved by the Institutional Review Board (IRB) of Seoul St. Mary’s Hospital, Seoul, South Korea (KC20RASI0355) and followed the tenets of the Declaration of Helsinki. Written informed consent was waived due to the characteristics of the retrospective study design and the waiver was approved by the IRB of Seoul St. Mary’s Hospital, South Korea.
Patient data was collected from Feb 2010 to Feb 2020 from the electronic medical record and all patients were visiting the glaucoma clinic at Seoul St. Mary’s Hospital for glaucoma screening. A comprehensive ophthalmic assessment, including the measurement of best-corrected visual acuity, refraction, slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry, central corneal thickness using ultrasound pachymetry (Tomey Corporation, Nagoya, Japan), the estimation of axial length using ocular biometry (IOL Master; Carl Zeiss Meditec, Dublin, CA, USA), dilated stereoscopic examination of the optic disc and fundus, color disc photography, red-free RNFL photography (Canon, Tokyo, Japan), OCT (Cirrus OCT; Carl Zeiss Meditec), and Humphrey VF examination (24–2 Swedish Interactive Threshold Algorithm Standard program; Carl Zeiss Meditec) was carried out at initial work-up36. After the initial work-up, the patients were followed-up every 6 to 12 months according to their disease severity.
The inclusion criteria were: a best-corrected visual acuity of ≥ 20/40, a mean deviation (MD) better than − 6.00 decibels (dB) based on the Hodapp-Anderson-Parish criteria37, and five or more consistently reliable VFs (defined as a false-negative rate of < 15%, a false positive rate of < 15%, and fixation losses of < 20%). Patients were excluded based on any of the following criteria: less than five reliable VFs after excluding the initial one; a history of any retinal disease, including diabetic or hypertensive retinopathy or other retinal complications; a history of eye trauma or surgery, including glaucoma incisional surgery or laser procedure; another optic nerve disease besides glaucoma; or a history of systemic or neurological diseases that might affect the VF. Additionally, to exclude eyes with pathologic myopia, patients who showed either posterior staphyloma or myopic maculopathy on wide photography (Optos, Dunfermline, UK) or OCT images from Cirrus—OCT macular scan were refrained from participating in the study.
If both eyes were eligible, one eye was randomly selected from each patient that met the inclusion and exclusion criteria.
Definition of the temporal VFD group
To be included in the temporal VFD group, the patients were required to meet the following criteria: temporal VFDs defined by VFDs that were restricted to either the temporal edges of the field (Fig. 4b) or around the blind spot (Fig. 4c) and myopic eyes with an axial length ≥ 24.5 mm without definite glaucoma diagnosed by the criteria described below.
Figure 1.
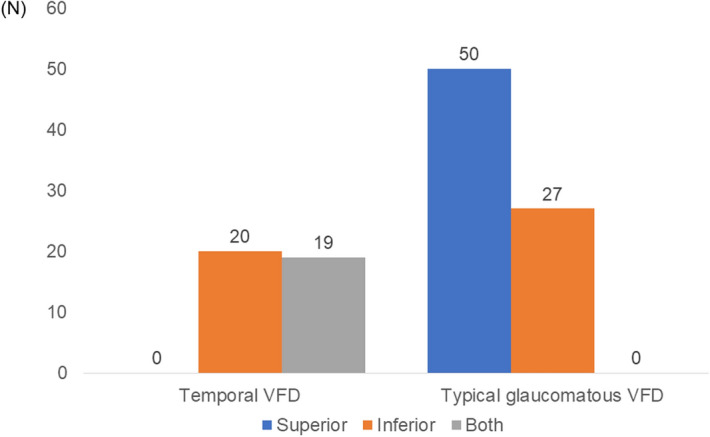
Location of Visual Field Defect in All eyes (N, 74). Distributions of visual field defect in each hemisphere are shown. (chi-squared test, P < 0.001). VFD visual field defect.
Definition of the typical glaucomatous VFD groups: Peripheral nasal step or paracentral scotoma groups
The peripheral nasal and paracentral scotoma groups were recruited from patients with early open-angle glaucoma with MD better than − 6.00 decibels (dB). Peripheral nasal VFD was defined as a glaucomatous VFD in one hemifield in the nasal periphery outside 10 degrees of fixation with no involvement within the central 10 degrees and the presence of at least three contiguous test points within the same hemifield on the pattern standard deviation (PSD) plot at P < 1%, with at least one at P < 0.5% (Fig. 4d)38. The paracentral VFD group included patients with a glaucomatous VFD in one hemifield within 10 degrees of fixation, with at least one point at P < 0.5% lying at the two innermost paracentral points and no VFDs outside the central 10 degrees (Fig. 4e)38. For those with two VFDs, points on the edge of the VF field or those directly around the blind spot were excluded. To elucidate specific features of myopic eyes with temporal VFD, we classed patients into two groups: 1) temporal VFD group and 2) typical glaucomatous VFD group, a combination of patients with peripheral nasal VFD and paracentral VFD. Figure 4 details specific distribution of the VFD types.
For glaucoma diagnosis, following criteria were applied to patients: glaucomatous optic disc appearances (presenting diffuse or localized rim thinning, a notch in the rim, or a cup-to-disc ratio higher than that of the other eye by > 0.2), VF changes consistent with glaucomatous VFD such as a cluster of ≥ 3 non-edge points on the pattern deviation plot with a probability of < 5% of the normal population, with one of these points having a probability of < 1%, a pattern standard deviation with P < 5%, or a Glaucoma Hemifield Test result outside the normal limits in a consistent pattern on two qualifying VFs—these results were confirmed by two glaucoma specialists (K.I.J. and C.K.P.)-, and an open-angle evident on gonioscopy.
Assessment of VFD progression
Defects VFD progression was evaluated by the glaucoma progression analysis (GPA) II trend analysis algorithm of the visual field index (VFI)39. The VFI allocates more importance to central points than to peripheral points and is adjusted for age. This parameter is expressed in percent, with 100% a perimetrically normal visual field, and 0% a totally blind one. To minimize the effect of cataracts, a pattern deviation probability map was used to identify the test points with normal sensitivity (100% VFI); those showing a relative loss, which is scored as a function of total deviation and an age-corrected normal threshold; and those with no sensitivity (0% VFI). If the change slope of the VFI was statistically significant (P < 0.05) by GPA, a noticeable trend was considered.
Assessment with optical coherence tomography
OCT images were obtained by scanning the eyes with the Cirrus OCT using software version 6.0. Once the ONH was centered, the laser scanned a 6 × 6 mm area, which captured a cube of data consisting of 200 A scans from 200 linear B scans (40,000 points) over approximately 1.5 s (27,000 A scans). After determining the optic disc, the OCT algorithms automatically placed a circle of 3.46 mm in diameter around the disc. Software version 6.0 provided the data of the ONH parameters, including the disc area, the rim area, the cup-to-disc ratio, the vertical cup-to-disc ratio, and the cup volume. The RNLF thickness within a 3.46 mm diameter circle (256 A scan) automatically positioned around the ONH was measured and analyzed in 17 parameters: average, superior, nasal, inferior, temporal, and 12 clock-hour sectors. Regarding the GCIPL thickness, the GCIPL thickness within a 6 × 6 × 2 mm (14.13mm2) elliptical annulus around the fovea was measured and computed by the GCA algorithm embedded in the OCT. The annulus cube was 1 mm in inner vertical diameter, 4 mm in outer vertical diameter, 1.2 mm in inner horizontal diameter, and 4.8 mm in outer horizontal diameter, excluding the central portions of the fovea where the layers are thin and difficult to defect. GCIPL thickness was then analyzed in eight parameters: average, minimum, superior, superonasal, inferonasal, inferior, inferotemporal, and superotemporal40,41.
To correct axial length -related ocular magnification, the Littmann’s formaula (t = p*q*s) was applied42,43, and additionally, the ONH area was modified with the modified formula (t2 = p2*q2*s2) as well44,45.
Poor images due to involuntary saccade, misalignment, or artifacts, and signal strengths < 6 were excluded.
Measurement of Optic Disc Tilt, Torsion, and PPA
Digital retinal photographs centered on the optic disc and macular were used for assessing the degree of optic disc tilt, torsion, and PPA. They were measured by a glaucoma specialist (J. L) using the National Institutes of Health image analysis software (ImageJ version 1.52; available at http://rsb.info.nih.gov/ij/index.html; developed by Wayne Rasband, National Institutes of Health, Bethesda, MD, USA).
With reference to the precedent study46, optic disc tilt was defined as the ratio between the longest and shortest diameters of the optic disc was more than 1.30 (Fig. 5a). Optic disc torsion was measured by the deviation of the long axis of the optic disc from the vertical meridian and was defined when the degree of the deviation was more than 15° (Fig. 5b). The β-PPA, an inner crescent of chorioretinal atrophy with visible sclera and choroidal vessels, was drawn with a mouse to trace the disc and the PPA margins and the area of β-PPA was calculated using the ImageJ software (Fig. 5a). Photographic magnification was corrected with Littmann’s method47,48. The area of βPPA was measured by two authors who were masked to the clinical data (J.L and K.I.J). The values were determined as the mean of the measurements performed by the two authors. A third adjudicator (C.K.P) resolved disagreements between two observers.
Figure 2.
Glaucoma progression analysis using assessment with Trend- based analysis. Mean values of the rate of change of VFI (%/year) are shown. VFD indicates visual field defect; VFI, visual field index. Bold font indicates significant P values (P < 0.05). X in the box stands for the mean value for each group.
Subgroup analysis
To determine whether there were different clinical characteristics or risk factors related to the presence of progression of β- zone PPA, we performed subgroup analyses in the temporal VFD group. Specifically, the temporal VFD group was divided into two groups, one with true β-PPA enlargement and the other without true β-PPA enlargement. To assess β-PPA enlargement, the initial and final areas of β-PPA were measured and the change between areas was divided by the total follow-up year. True β-PPA enlargement was defined as increments of over 1000 pixels per year.
Furthermore, we analyzed the data after applying 1:1 propensity-score matching for axial length because there is a significant difference in axial length between groups.
Statistical analysis
All statistical analyses were performed using the SPSS statistical package (SPSS, Inc, Chicago, IL, USA). A propensity score analysis was performed to match eyes between the temporal VFD group and the typical glaucomatous VFD group regarding axial length. By using multiple logistic regression analysis, the propensity scores were calculated49. Using predicted probabilities, we sought to match a patient in the temporal VFD group with the closest patient in the typical glaucomatous VFD group using propensity score values. Applying the Greedy 5 → 1 digit match algorithm50, we created propensity score-matched pairs without replacement (a 1:1 match). Unless this could be achieved, the algorithm proceeded sequentially to the next highest digit match (4-,3-,2-, or 1- digit match) until no further matches were possible.
Test–retest variability was estimated adopting the intraclass correlation coefficient (ICC). ICC scores ≥ 0.75, 0.40–0.75, and ≤ 0.40 are considered to be excellent, moderate, and poor, respectively51. Student’s t-test was adopted to compare the differences between the groups. The chi-square test was applied to compare frequencies. A P-value of less than 0.05 was considered statistically significant. Linear regression analysis was used to determine the factors associated with VFD progression in the total group and the temporal VFD group. The variables with significance at P < 0.10 in univariate analysis were included in the multivariate model. P < 0.05 was considered to represent statistical significance. In order to adjust multiple comparisons, Bonferroni correction was used when needed.
Supplementary Information
Acknowledgements
None of the authors has any proprietary interests in any device or drug mentioned in the article.
Author contributions
J. L. wrote the main manuscript text. J.L, C.K.P and K.I.J performed the data review and analysis. The critical revision of the manuscript was done by J.L and K.I.J. All authors reviewed the manuscript.
Funding
This research was supported by the Research Fund of Seoul St. Mary’s Hospital, the Catholic University of Korea.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-88832-1.
References
- 1.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/s0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106(10):2010–2015. doi: 10.1016/s0161-6420(99)90416-5. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006;113(9):1613–1617. doi: 10.1016/j.ophtha.2006.03.059. [DOI] [PubMed] [Google Scholar]
- 5.Jonas JB, Gusek GC, Naumann GO. Optic disk morphometry in high myopia. Graefes Arch. Clin. Exp. Ophthalmol. 1988;226(6):587–590. doi: 10.1007/bf02169209. [DOI] [PubMed] [Google Scholar]
- 6.Jonas JB, Dichtl A. Optic disc morphology in myopic primary open-angle glaucoma. Graefes Arch. Clin. Exp. Ophthalmol. 1997;235(10):627–633. doi: 10.1007/bf00946938. [DOI] [PubMed] [Google Scholar]
- 7.Samarawickrama C, Mitchell P, Tong L, et al. Myopia-related optic disc and retinal changes in adolescent children from singapore. Ophthalmology. 2011;118(10):2050–2057. doi: 10.1016/j.ophtha.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 8.Ding X, Chang RT, Guo X, et al. Visual field defect classification in the Zhongshan ophthalmic center-brien holden vision institute high myopia registry study. Br. J. Ophthalmol. 2016;100(12):1697–1702. doi: 10.1136/bjophthalmol-2015-307942. [DOI] [PubMed] [Google Scholar]
- 9.Ohno-Matsui K, Shimada N, Yasuzumi K, et al. Long-term development of significant visual field defects in highly myopic eyes. Am. J. Ophthalmol. 2011;152(2):256–265.e1. doi: 10.1016/j.ajo.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 10.Lee MW, Kim JM, Shin YI, Jo YJ, Kim JY. Longitudinal changes in peripapillary retinal nerve fiber layer thickness in high myopia: a prospective, observational study. Ophthalmology. 2019;126(4):522–528. doi: 10.1016/j.ophtha.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Akagi T, Hangai M, Kimura Y, et al. Peripapillary scleral deformation and retinal nerve fiber damage in high myopia assessed with swept-source optical coherence tomography. Am. J. Ophthalmol. 2013;155(5):927–936. doi: 10.1016/j.ajo.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Fantes FE, Anderson DR. Clinical histologic correlation of human peripapillary anatomy. Ophthalmology. 1989;96(1):20–25. doi: 10.1016/s0161-6420(89)32929-0. [DOI] [PubMed] [Google Scholar]
- 13.Kubota T, Jonas JB, Naumann GO. Direct clinico-histological correlation of parapapillary chorioretinal atrophy. Br. J. Ophthalmol. 1993;77(2):103–106. doi: 10.1136/bjo.77.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jonas JB, Königsreuther KA, Naumann GO. Optic disc histomorphometry in normal eyes and eyes with secondary angle-closure glaucoma. II. Parapapillary region. Graefes Arch. Clin. Exp. Ophthalmol. 1992;230(2):134–139. doi: 10.1007/bf00164651. [DOI] [PubMed] [Google Scholar]
- 15.Curcio CA, Saunders PL, Younger PW, Malek G. Peripapillary chorioretinal atrophy: Bruch's membrane changes and photoreceptor loss. Ophthalmology. 2000;107(2):334–343. doi: 10.1016/s0161-6420(99)00037-8. [DOI] [PubMed] [Google Scholar]
- 16.Doshi A, Kreidl KO, Lombardi L, Sakamoto DK, Singh K. Nonprogressive glaucomatous cupping and visual field abnormalities in young Chinese males. Ophthalmology. 2007;114(3):472–479. doi: 10.1016/j.ophtha.2006.07.036. [DOI] [PubMed] [Google Scholar]
- 17.Lee JR, Kim S, Lee JY, Back S, Lee KS, Kook MS. Is myopic optic disc appearance a risk factor for rapid progression in medically treated glaucomatous eyes with confirmed visual field progression? J. Glaucoma. 2016;25(3):330–337. doi: 10.1097/ijg.0000000000000218. [DOI] [PubMed] [Google Scholar]
- 18.Choy YJ, Kwun Y, Han JC, Kee C. Comparison of visual field progression between temporally tilted disc and nontilted disc, in patients with normal tension glaucoma. Eye (Lond). 2015;29(10):1308–1314. doi: 10.1038/eye.2015.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teng CC, De Moraes CG, Prata TS, Tello C, Ritch R, Liebmann JM. Beta-Zone parapapillary atrophy and the velocity of glaucoma progression. Ophthalmology. 2010;117(5):909–915. doi: 10.1016/j.ophtha.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Xu L, Zhang L, Yang H, Ma Y, Jonas JB. Peripapillary atrophy in elderly Chinese in rural and urban Beijing. Eye (Lond). 2008;22(2):261–266. doi: 10.1038/sj.eye.6702601. [DOI] [PubMed] [Google Scholar]
- 21.Chen Q, He J, Yin Y, et al. Impact of the morphologic characteristics of optic disc on choroidal thickness in young myopic patients. Invest Ophthalmol. Vis. Sci. 2019;60(8):2958–2967. doi: 10.1167/iovs.18-26393. [DOI] [PubMed] [Google Scholar]
- 22.Ha A, Kim YK, Jeoung JW, Park KH. Impact of optic disc hemorrhage on subsequent glaucoma progression in mild-to-moderate myopia. PLoS ONE. 2017;12(12):e0189706. doi: 10.1371/journal.pone.0189706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nitta K, Sugiyama K, Wajima R, Tachibana G. Is high myopia a risk factor for visual field progression or disk hemorrhage in primary open-angle glaucoma? Clin. Ophthalmol. 2017;11:599–604. doi: 10.2147/opth.S131370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seol BR, Kim S, Kim DM, Park KH, Jeoung JW, Kim SH. Influence of intraocular pressure reduction on progression of normal-tension glaucoma with myopic tilted disc and associated risk factors. Jpn. J. Ophthalmol. 2017;61(3):230–236. doi: 10.1007/s10384-017-0508-y. [DOI] [PubMed] [Google Scholar]
- 25.Sung MS, Kang YS, Heo H, Park SW. Optic disc rotation as a clue for predicting visual field progression in myopic normal-tension glaucoma. Ophthalmology. 2016;123(7):1484–1493. doi: 10.1016/j.ophtha.2016.03.040. [DOI] [PubMed] [Google Scholar]
- 26.Park HL, Hong KE, Park CK. Impact of age and myopia on the rate of visual field progression in glaucoma patients. Medicine (Baltimore) 2016;95(21):e3500. doi: 10.1097/md.0000000000003500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee J, Ahn EJ, Kim YW, et al. Impact of myopia on the association of long-term intraocular pressure fluctuation with the rate of progression in normal-tension glaucoma. Br. J. Ophthalmol. 2020 doi: 10.1136/bjophthalmol-2019-315441. [DOI] [PubMed] [Google Scholar]
- 28.Sawada Y, Hangai M, Ishikawa M, Yoshitomi T. Association of myopic deformation of optic disc with visual field progression in paired eyes with open-angle glaucoma. PLoS ONE. 2017;12(1):e0170733. doi: 10.1371/journal.pone.0170733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoon JY, Sung KR, Yun SC, Shin JW. Progressive optic disc tilt in young myopic glaucomatous eyes. Korean J. Ophthalmol. 2019;33(6):520–527. doi: 10.3341/kjo.2019.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi JA, Park HY, Shin HY, Park CK. Optic disc characteristics in patients with glaucoma and combined superior and inferior retinal nerve fiber layer defects. JAMA Ophthalmol. 2014;132(9):1068–1075. doi: 10.1001/jamaophthalmol.2014.1056. [DOI] [PubMed] [Google Scholar]
- 31.Han JC, Han SH, Park DY, Lee EJ, Kee C. Clinical course and risk factors for visual field progression in normal-tension glaucoma with myopia without glaucoma medications. Am. J. Ophthalmol. 2020;209:77–87. doi: 10.1016/j.ajo.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 32.Han JC, Lee EJ, Kim SH, Kee C. Visual field progression pattern associated with optic disc tilt morphology in myopic open-angle glaucoma. Am. J. Ophthalmol. 2016;169:33–45. doi: 10.1016/j.ajo.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 33.Bak E, Ha A, Kim YW, et al. Ten years and beyond longitudinal change of ß-zone parapapillary atrophy: comparison of primary open-angle glaucoma with normal eyes. Ophthalmology. 2020;20:2020. doi: 10.1016/j.ophtha.2020.01.057. [DOI] [PubMed] [Google Scholar]
- 34.Quigley HA, Addicks EM. Regional differences in the structure of the lamina cribrosa and their relation to glaucomatous optic nerve damage. Arch. Ophthalmol. 1981;99(1):137–143. doi: 10.1001/archopht.1981.03930010139020. [DOI] [PubMed] [Google Scholar]
- 35.Cho BJ, Park KH. Topographic correlation between β-zone parapapillary atrophy and retinal nerve fiber layer defect. Ophthalmology. 2013;120(3):528–534. doi: 10.1016/j.ophtha.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Shin DY, Jeon SJ, Kim EK, Jung KI, Park HYL, Park CK. Association between peripapillary scleral deformation and choroidal microvascular circulation in glaucoma. Sci Rep. 2019;9(1):18503. doi: 10.1038/s41598-019-54882-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hodapp E, Anderson DR. Clinical decisions in glaucoma. Mosby, St Louis. 1993;20:52–61. [Google Scholar]
- 38.Park SC, De Moraes CG, Teng CC, Tello C, Liebmann JM, Ritch R. Initial parafoveal versus peripheral scotomas in glaucoma: risk factors and visual field characteristics. Ophthalmology. 2011;118(9):1782–1789. doi: 10.1016/j.ophtha.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Bengtsson B, Heijl A. A visual field index for calculation of glaucoma rate of progression. Am. J. Ophthalmol. 2008;145(2):343–353. doi: 10.1016/j.ajo.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 40.Mwanza JC, Durbin MK, Budenz DL, et al. Profile and predictors of normal ganglion cell-inner plexiform layer thickness measured with frequency-domain optical coherence tomography. Invest Ophthalmol. Vis. Sci. 2011;52(11):7872–7879. doi: 10.1167/iovs.11-7896. [DOI] [PubMed] [Google Scholar]
- 41.Mwanza JC, Oakley JD, Budenz DL, Chang RT, Knight OJ, Feuer WJ. Macular ganglion cell-inner plexiform layer: automated detection and thickness reproducibility with spectral domain-optical coherence tomography in glaucoma. Invest Ophthalmol Vis. Sci. 2011;52(11):8323–8329. doi: 10.1167/iovs.11-7962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bennett AG, Rudnicka AR, Edgar DF. Improvements on Littmann's method of determining the size of retinal features by fundus photography. Graefes Arch. Clin. Exp. Ophthalmol. 1994;232(6):361–367. doi: 10.1007/bf00175988. [DOI] [PubMed] [Google Scholar]
- 43.Kang SH, Hong SW, Im SK, Lee SH, Ahn MD. Effect of myopia on the thickness of the retinal nerve fiber layer measured by Cirrus HD optical coherence tomography. Invest Ophthalmol. Vis. Sci. 2010;51(8):4075–4083. doi: 10.1167/iovs.09-4737. [DOI] [PubMed] [Google Scholar]
- 44.Leung CK, Cheng AC, Chong KK, et al. Optic disc measurements in myopia with optical coherence tomography and confocal scanning laser ophthalmoscopy. Invest Ophthalmol. Vis. Sci. 2007;48(7):3178–3183. doi: 10.1167/iovs.06-1315. [DOI] [PubMed] [Google Scholar]
- 45.Savini G, Barboni P, Parisi V, Carbonelli M. The influence of axial length on retinal nerve fibre layer thickness and optic-disc size measurements by spectral-domain OCT. Br. J. Ophthalmol. 2012;96(1):57–61. doi: 10.1136/bjo.2010.196782. [DOI] [PubMed] [Google Scholar]
- 46.Park HY, Lee K, Park CK. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology. 2012;119(9):1844–1851. doi: 10.1016/j.ophtha.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 47.Littmann H. Determination of the real size of an object on the fundus of the living eye. Klin. Monbl. Augenheilkd. 1982;180(4):286–289. doi: 10.1055/s-2008-1055068. [DOI] [PubMed] [Google Scholar]
- 48.Uhm KB, Lee DY, Kim JT, Hong C. Peripapillary atrophy in normal and primary open-angle glaucoma. Korean J. Ophthalmol. 1998;12(1):37–50. doi: 10.3341/kjo.1998.12.1.37. [DOI] [PubMed] [Google Scholar]
- 49.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 1998;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 50.Austin PC. Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: a systematic review and suggestions for improvement. J. Thorac. Cardiovasc Surg. 2007;134(5):1128–1135. doi: 10.1016/j.jtcvs.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 51.Jl F. Reliability of measurements. The design and analysis of clinical experiments. Wiley; 1986. pp. 1–32. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.