Abstract
Background
The control of the Coronavirus Disease 2019 (COVID-19) pandemic may be dependent on widespread receipt of an effective vaccine. It is important to understand patient health-related behaviors and perceptions to guide public health vaccination strategies.
Objectives
To examine perceptions of COVID-19 and vaccination beliefs, and identify predictors of intention to receive the COVID-19 vaccine in the US.
Methods
A cross-sectional, web-based survey guided by the Health Belief Model was conducted using a web-based Qualtrics survey panel of US adults. The main outcome was the intention to receive the COVID-19 vaccine if offered. Additional measures included: demographics, perceptions of COVID-19 severity, risk and susceptibility, views of a potential COVID-19 vaccine, virus and vaccine information sources, vaccine beliefs and behaviors, and seasonal flu vaccine history.
Results
A total of 1047 complete responses were included. Females had lower odds of intending to receive the COVID-19 vaccine than males (AOR = 0.54, 95% CI: 0.36–0.80). Those with a two-year degree/some college had lower odds of intending to receive the COVID-19 vaccine compared to those with a high school degree/GED (AOR = 0.59, 95% CI: 0.36–0.97). Respondents who perceived the severity of the virus to be higher, perceived a greater COVID-19 vaccine benefit, and perceived greater general vaccine benefits had higher odds of intending to receive a COVID-19 vaccine (AOR = 1.44, 95% CI: 1.09–1.91; AOR = 2.82, 95% CI: 2.24–3.56; AOR = 1.77, 95% CI 1.41–2.21, respectively).
Conclusions
In this study, intention to receive the COVID-19 vaccine varied across demographics, perceived virus severity, COVID-19 vaccine and general vaccine beliefs. Successful implementation of a COVID-19 immunization strategy by healthcare providers and public health officials will need to incorporate diverse COVID-19 vaccination education strategies tailored to patients' health beliefs.
Keywords: COVID-19 vaccine, Pandemic, Health belief model
Introduction
In March 2020, the World Health Organization (WHO) characterized Coronavirus Disease 2019 (COVID-19) as a pandemic, which led to interruptions in daily life such as closing businesses and schools and limiting social gatherings to prevent the spreading of the virus.1 COVID-19, caused by a novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), primarily affects the respiratory system and in some instances, can be fatal.2 , 3 As of August 17th, 2020 (when data collection began), there were roughly 21.8 million cases and over 774 thousand deaths worldwide, with about 5.4 million cases and 170,500 deaths in the United States (US).4 With cases and deaths continuing to rise, the long-term solution to mitigating the morbidity and mortality related to COVID-19 will likely be dependent on a globally available COVID-19 vaccine.5 However, for a safe and efficacious COVID-19 vaccine to be the solution, it must also be widely accepted and received by the general public to guarantee broad immunological protection.5
Vaccine hesitancy, which refers to individuals who may refuse, delay, or be unsure of some vaccines, poses a major challenge to the success of vaccination programs.6 The WHO listed vaccine hesitancy as one of the ten threats to global health in 2019.7 Previous studies on vaccine hesitancy have identified socioeconomic, demographic, and other belief factors to play a large role in the likelihood of vaccine acceptance.6
The Health Belief Model (HBM), a health promotion framework that assesses and predicts health-related behavior, has been used in studies to determine predictors of vaccination.8 , 9 Previous work used the HBM to explore intention to receive the 2009 H1N1 vaccine and found that barriers to vaccination, physician recommendation, and previous seasonal influenza vaccination were predictors of intent to receive the vaccine.9 When considering the distribution and administration of the COVID-19 vaccine, public health campaigns and strategies will need to address perceptions of vaccine-hesitant individuals to increase vaccine uptake. Using the HBM to identify predictors of intention to receive the COVID-19 vaccine will help inform vaccination campaigns.
Surveys regarding the intention to receive the COVID-19 vaccine in the US have been published.10, 11, 12 Two national surveys of COVID-19 vaccine acceptability among national online survey panels were conducted in May 2020.10 , 12 One study found that the majority of adults were willing to receive a COVID-19 vaccine, with the greatest predictors being healthcare provider recommendation, higher levels of perceived susceptibility, perceived severity, perceived effectiveness, and moderate or liberal political leaning.10 The other study found differences in vaccine acceptance by participant demographics and geography.12 In July 2020, a third online survey of US adults assessed factors related to the likelihood of accepting a COVID-19 vaccine.11 They found that perceptions of vaccine-related attributes and participants' political partisanship were associated with the likelihood of vaccine acceptance.11 This current study builds upon previous research by providing a more recent survey of participant perceptions and utilizes the HBM framework to predict intention to receive the COVID-19 vaccine. Using the HBM as the theoretical framework, an online survey was developed and distributed to a nationally representative sample of US adults. This study seeks to examine (1) the perceptions of severity, risk, and susceptibility to COVID-19, (2) views of vaccine benefits and barriers and cues to action, and (3) identify predictors of intention to receive the COVID-19 vaccine if offered.
Methods
Study design and sample
This cross-sectional, descriptive study used a Qualtrics web-based survey panel (Qualtrics, Provo, UT). There were four pre-specified demographic quotas (gender, race, region, and age) matched to the 2010 US Census data to ensure the survey sample was reflective of the US population. Adults aged 18 years or older were eligible to participate.
Theoretical framework
There are six constructs in the HBM: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy.8 Perceived susceptibility is the individual's belief surrounding their risk of getting a condition or disease whereas perceived severity is the belief about how serious the condition or disease will be. Perceived benefits and perceived barriers are related to the beliefs around the efficacy and the costs of the advised action, respectively. Cues to action are strategies to encourage a state of “readiness,” while self-efficacy is the belief in one's ability to do something.8 All HBM constructs were used in this study and are reflected in the survey question items.
Survey instrument
A 60-item questionnaire was developed to collect information on demographics, perceptions of COVID-19 severity, risk and susceptibility, views on the potential COVID-19 vaccine, other general vaccine beliefs, and seasonal flu vaccine history. The questionnaire included questions on if the respondent belonged to or lived with an individual in a high-risk group, or if the respondent belonged to or lived with an individual that might be at an increased risk for severe illness (i.e., potentially high-risk group). These high-risk groups were defined by the Centers for Disease Control and Prevention (CDC) as groups at increased risk or might be at an increased risk for severe illness from COVID-19.3 A list of these high-risk groups was provided in the questionnaire for the respondent to check all that apply. This survey was adapted from a previous survey that assessed predictors of intent to receive the novel (2009) H1N1 influenza vaccine.9 The survey instrument is included as online material.
The first series of questions on demographics asked respondents for their age, gender, race, ethnicity, US region, education level, annual household income, if they are a member or living with a member of a COVID-19 high-risk group, and if they are a member or living with someone who might be at high-risk for serious illness from COVID-19, according to CDC definitions at the time of survey administration.3 The second series of questions consisted of 5-point Likert scale questions (1 = strongly disagree to 5 = strongly agree) on perceptions of COVID-19 severity, risk, and susceptibility. The next series asked about views of the potential COVID-19 vaccine, including perceptions of side effects, safety, cost, access, and availability. Respondents were asked about their perceived comfort in receiving COVID-19 vaccination at different locations (e.g., doctor's office, pharmacy, or drive-through car site). The last series of questions included a mix of 5-point Likert scale questions on general vaccine beliefs (e.g., “vaccines are safe” and “vaccines prevent disease”) along with questions about the respondent's seasonal flu vaccine history (e.g., if they received the vaccine and where).
The survey was pre-tested two times among faculty and graduate students for clarity and accuracy. The survey was modified based on feedback, which included minor revisions to the response options, the format, and the question wording. The survey did not collect any identifiable patient information. The Institutional Review Board at the University of Michigan approved this study.
Data collection
The Qualtrics survey was distributed to a nationally representative online survey panel in the US. Responses were collected until there was a minimum of 1000 completed surveys that met the four pre-specified demographic quotas. Qualtrics compensated each respondent for their participation. All responses were collected anonymously. Survey responses were collected from August 17–20, 2020.
Data analysis
Data were analyzed using descriptive statistics and presented as number (percentage), median (interquartile range), or mean (standard deviation). The main outcome was the intention to receive a COVID-19 vaccine, analyzed as Yes (very likely and likely to receive the vaccine) vs. No (very unlikely and unlikely to receive the vaccine). Multivariable logistic regression was used to examine the association between demographic, seasonal influenza vaccine history, and HBM variables with the intention to receive a COVID-19 vaccine. Results are presented as odds ratios (OR) and adjusted odds ratios (AOR) with 95% confidence intervals. To assess reliability for the HBM variables, Cronbach's alpha was calculated for the domains with three or more items and Pearson's correlation was used for the domain with two items. Scale means were calculated for domains with a Cronbach's alpha or Pearson's correlation value > 0.5. A post-hoc analysis using the χ2 test was conducted to identify differences in perceived comfort of receiving a COVID-19 vaccine at different locations (doctor's office, pharmacy, or drive-through car site) between respondents that were likely or unlikely to receive a COVID-19 vaccine. The a priori level of significance was p < 0.05. Analyses were performed using SAS software (version 9.4, Cary, NC).
Results
Demographics
A total of 1050 respondents completed the survey. Of the 1050 total respondents, three were excluded because of incomplete responses. The majority were under the age of 65 years old (883, 84.3%), non-Hispanic or Latino (865, 82.6%), and white (755, 72.1%) (Table 1 ). There were slightly more female respondents (584, 55.8%). A little over one-third of the respondents were located in the South (392, 37.4%). Over one-third of the respondents had an annual household income of $15,000 to $49,000 (387, 37.0%).
Table 1.
Demographics and seasonal influenza vaccine history of survey participants.
| Demographic Characteristics | Total N = 1047, N (%) |
|---|---|
| Age (years), mean (SD, Range), median (IQR) | 45 (16.9, 18–96), 42 (31–59) |
| Age (years) | |
| Under 65 | 883 (84.3) |
| 65 and older | 164 (15.7) |
| Gender | |
| Female | 584 (55.8) |
| Male | 460 (43.9) |
| Transgender/Non-binary | 3 (0.3) |
| Race | |
| White | 755 (72.1) |
| Black or African American | 156 (14.9) |
| Asian | 58 (5.5) |
| Other Race | 33 (3.2) |
| More than one race | 22 (2.1) |
| American Indian or Alaska Native | 18 (1.7) |
| Native Hawaiian or Other Pacific Islander | 5 (0.5) |
| Ethnicity | |
| Not Hispanic or Latino | 865 (82.6) |
| Hispanic or Latino | 182 (17.4) |
| Region | |
| South | 392 (37.4) |
| West | 244 (23.3) |
| Midwest | 222 (21.2) |
| Northeast | 189 (18.1) |
| Education | |
| Less than high school | 14 (1.3) |
| Some high school | 35 (3.3) |
| High school graduate/GED | 273 (26.1) |
| Two-year degree/some college | 271 (25.9) |
| Bachelor's degree | 273 (26.1) |
| Graduate degree/Professional degree | 181 (17.3) |
| Annual household income | |
| < $15,000 | 114 (10.9) |
| $15,000 to $49,999 | 387 (37.0) |
| $50,000 to $99,999 | 296 (28.3) |
| $100,000 to $149,999 | 134 (12.8) |
| ≥ $150,000 | 116 (11.1) |
| Child < 18 years | |
| Yes | 375 (35.8) |
| No |
672 (64.2) |
|
Seasonal influenza vaccine history | |
| Ever had a past flu vaccine | |
| Yes | 732 (69.9) |
| No | 291 (27.8) |
| I don't know | 24 (2.3) |
| Flu vaccine last year | |
| Yes | 554 (52.9) |
| No | 474 (45.3) |
| I don't know | 19 (1.8) |
| Last year's location of flu vaccine receipt (N = 554) | |
| Physician's office | 223 (40.3) |
| Pharmacy | 145 (26.2) |
| Hospital | 63 (11.4) |
| Place of employment | 49 (8.8) |
| Health department | 34 (6.1) |
| Community health center | 18 (3.3) |
| Other | 16 (2.9) |
| School | 6 (1.1) |
Seasonal influenza vaccine history
Most respondents had a history of receiving a seasonal influenza vaccine (732, 69.9%) (Table 1). Approximately half had received the seasonal influenza vaccine last year (554, 52.9%). Of those who received the seasonal influenza vaccine last year, most received it at their physician's office (223/554, 40.3%).
History, behaviors, and risk of COVID-19
Approximately half of the respondents identified as a member of a COVID-19 high-risk group (535, 51.1%) or a member of a potentially high-risk group (609, 58.2%) as classified by the CDC (Table 2 ).3 About half reported living with a person in a COVID-19 high-risk group (494, 47.2%) or a potentially high-risk group (536, 51.2%). Most did not have a history of a positive COVID-19 test (927, 88.5%) or did not know of someone with a positive COVID-19 test (715, 68.3%). In the last month, face mask use in public was reported as “Always” by most respondents (677, 64.7%). Avoiding crowded areas where 6 feet of social distance cannot be maintained and avoiding social gatherings outside of the home was reported as “Always” by slightly less than half of the respondents (518, 49.5% and 511, 48.8%, respectively). Respondent's mean number of information sources for receiving current COVID-19 information was 3.9 (SD = 2.4) and 3.1 (SD = 2.3) for receiving COVID-19 vaccine information. A summary of types and number of information sources respondents selected is provided in Supplemental Table 1.
Table 2.
History, behaviors, and risk of COVID-19 in survey participants.
| COVID-19 Characteristics | Total N = 1047, N (%) |
|---|---|
| Member of high-risk group | |
| Yes | 535 (51.1) |
| No | 512 (48.9) |
| Living with a member of high-risk group | |
| Yes | 494 (47.2) |
| No | 553 (52.8) |
| Member of potentially high-risk group | |
| Yes | 609 (58.2) |
| No | 438 (41.8) |
| Living with a member of potentially high-risk group | |
| Yes | 536 (51.2) |
| No | 511 (48.8) |
| Ever test positive for COVID-19 | |
| Yes | 89 (8.5) |
| No | 927 (88.5) |
| I don't know | 31 (3.0) |
| Know someone with a positive COVID-19 test | |
| Yes | 304 (29.0) |
| No | 715 (68.3) |
| I don't know |
28 (2.7) |
|
Behavior in the last month: | |
| Face mask use in public | |
| Never | 21 (2.0) |
| Sometimes | 53 (5.1) |
| About half the time | 87 (8.3) |
| Most of the time | 209 (20.0) |
| Always | 677 (64.7) |
| Avoided crowded areas where 6 feet of social distance cannot be maintained | |
| Never | 52 (5.0) |
| Sometimes | 93 (8.9) |
| About half the time | 92 (8.8) |
| Most of the time | 292 (27.9) |
| Always | 518 (49.5) |
| Avoided social gatherings outside of the home | |
| Never | 75 (7.2) |
| Sometimes | 81 (7.7) |
| About half the time | 107 (10.2) |
| Most of the time | 273 (26.1) |
| Always |
511 (48.8) |
| COVID-19 information sources per respondent (Mean (SD)) | 3.9 (2.4) |
| COVID-19 vaccine information sources per respondent (Mean (SD)) | 3.1 (2.3) |
General vaccine behaviors and intention to receive the COVID-19 vaccine
When respondents were asked if they were willing to get all recommended vaccines for themselves, the majority agreed with the statement (631, 60.3%) (Table 3 ). If offered a COVID-19 vaccine, most of the respondents indicated that they were likely or very likely to receive it (663, 63.3%). If the COVID-19 vaccine were to be administered in more than one dose, roughly the same number of respondents reported being likely or very likely to receive it (639, 61.0%). If the COVID-19 vaccine was required to return to work or school, most respondents selected likely or very likely to receive a COVID-19 vaccine (634, 60.6%).
Table 3.
COVID-19 vaccine and general vaccine receipt of survey participants.
| Vaccine receipt items | Total N = 1047, N (%) |
|---|---|
| I am willing to get all of the recommended vaccines for myself | |
| Strongly disagree | 119 (11.4) |
| Somewhat disagree | 103 (9.8) |
| Neither agree nor disagree | 194 (18.5) |
| Somewhat agree | 271 (25.9) |
| Strongly agree | 360 (34.4) |
| The COVID-19 pandemic has made me more likely to get the seasonal flu vaccine | |
| Strongly disagree | 179 (17.1) |
| Somewhat disagree | 171 (16.3) |
| Neither agree nor disagree | 291 (27.8) |
| Somewhat agree | 214 (20.4) |
| Strongly agree |
192 (18.3) |
|
Perceived comfort in receiving the COVID-19 vaccine by going into a: | |
| Doctor's office/health clinic | |
| Extremely comfortable | 295 (28.2) |
| Somewhat comfortable | 280 (26.7) |
| Neither comfortable nor uncomfortable | 214 (20.4) |
| Somewhat uncomfortable | 116 (11.1) |
| Extremely uncomfortable | 142 (13.6) |
| Pharmacy | |
| Extremely comfortable | 221 (21.1) |
| Somewhat comfortable | 297 (28.4) |
| Neither comfortable nor uncomfortable | 219 (20.9) |
| Somewhat uncomfortable | 153 (14.6) |
| Extremely uncomfortable | 157 (15.0) |
| Drive-through (in your car) site | |
| Extremely comfortable | 229 (21.9) |
| Somewhat comfortable | 243 (23.2) |
| Neither comfortable nor uncomfortable | 212 (20.3) |
| Somewhat uncomfortable | 149 (14.2) |
| Extremely uncomfortable |
214 (20.4) |
|
If offered a COVID-19 vaccine … |
|
| Likelihood of receiving it | |
| Very likely | 345 (33.0) |
| Likely | 318 (30.4) |
| Unlikely | 207 (19.8) |
| Very unlikely | 177 (16.9) |
| Likelihood of receiving it if administered in more than one dose | |
| Very likely | 302 (28.8) |
| Likely | 337 (32.2) |
| Unlikely | 202 (19.3) |
| Very unlikely | 206 (19.7) |
| Likelihood of receiving it if required to return to work and/or school | |
| Very likely | 407 (38.9) |
| Likely | 227 (21.7) |
| Unlikely | 89 (8.5) |
| Very unlikely | 127 (12.1) |
| Not applicable | 197 (18.8) |
The majority of respondents likely to receive a COVID-19 vaccine reported they were comfortable getting a COVID-19 vaccine at a doctor's office, pharmacy, or drive-through car site (75.4%, 67.3%, and 60.9%, respectively). In those unlikely to receive a COVID-19 vaccine, approximately half reported that they were uncomfortable getting a COVID-19 vaccine at a doctor's office, pharmacy, or drive-through care site (49.5%, 53.4%, and 58.6%, respectively) (Supplemental Table 2).
Predictors of intention to receive a COVID-19 vaccine
Older adults had higher odds of intending to receive the COVID-19 vaccine than those under age 65 (OR = 1.71, 95% CI: 1.18–2.47) (Table 4 ). Female respondents, Black and Other race respondents, and those with an annual household income of < $15,000 had lower odds of intending to receive the COVID-19 vaccine compared to male respondents, White race respondents, and those with an annual household income of $50,000–99,999 (ORfemale = 0.57, 95% CI: 0.44–0.74, ORBlack race = 0.36, 95% CI: 0.25–0.51, OROther race = 0.62, 95% CI: 0.43–0.90, OR<$15,000 annual household income = 0.54, 95% CI: 0.35–0.83). Respondents had higher odds of intending to receive the COVID-19 vaccine if they were located in the Midwest, Northeast, or West compared to the South (ORMidwest = 1.83, 95% CI: 1.29–2.58, ORNortheast = 1.57, 95% CI: 1.09–2.24, ORWest = 2.13, 95% CI: 1.51–3.00), had an annual household income of $150,000 or more compared to an annual household income of $50,000–99,999 (OR = 2.20, 95% CI: 1.33–3.66), and had a bachelor's degree or higher education compared to those with a high school/GED degree (ORBachelor's degree = 1.43, 95% CI: 1.01–2.03, ORGraduate/Professional degree = 2.79, 95% CI: 1.81–4.31). Receipt of a past influenza vaccine and receipt of an influenza vaccine last year were associated with higher odds of intending to receive the COVID-19 vaccine (OR = 2.44, 95% CI: 1.85–3.23 and OR = 2.61, 95% CI: 2.01–3.39, respectively).
Table 4.
Demographics, seasonal influenza vaccine history, and HBM domains associated with intention to receive a COVID-19 vaccine.
| Demographics |
Unadjusted OR [95% CI] |
Adjusted OR [95% CI] |
|---|---|---|
| N = 1047 | N = 887 | |
| Age (years) | ||
| Under 65 | 1.0 | 1.0 |
| 65 and older | 1.71 [1.18–2.47] | 1.05 [0.58–1.90] |
| Gender (N = 1045) | ||
| Male | 1.0 | 1.0 |
| Female | 0.57 [0.44–0.74] | 0.54 [0.36–0.80] |
| Race | ||
| White | 1.0 | 1.0 |
| Black | 0.36 [0.25–0.51] | 0.59 [0.35–1.00] |
| Other | 0.62 [0.43–0.90] | 0.73 [0.42–1.26] |
| Ethnicity | ||
| Not Hispanic or Latino | 1.0 | 1.0 |
| Hispanic or Latino | 0.99 [0.71–1.38] | 1.24 [0.76–2.02] |
| Region | ||
| South | 1.0 | 1.0 |
| Midwest | 1.83 [1.29–2.58] | 1.05 [0.63–1.74] |
| Northeast | 1.57 [1.09–2.24] | 1.19 [0.72–1.98] |
| West | 2.13 [1.51–3.00] | 1.80 [1.09–2.96] |
| Education | ||
| No high school degree | 0.75 [0.41–1.37] | 1.15 [0.48–2.77] |
| High school graduate/GED | 1.0 | 1.0 |
| Two-year degree/some college | 0.93 [0.66–1.31] | 0.59 [0.36–0.97] |
| Bachelor's degree | 1.43 [1.01–2.03] | 0.63 [0.37–1.07] |
| Graduate/Professional degree | 2.79 [1.81–4.31] | 1.50 [0.74–3.04] |
| Annual household income | ||
| < $15,000 | 0.54 [0.35–0.83] | 1.12 [0.55–2.26] |
| $15,000 to $49,999 | 0.87 [0.64–1.19] | 1.34 [0.86–2.09] |
| $50,000 to $99,999 | 1.0 | 1.0 |
| $100,000 to $149,999 | 1.40 [0.90–2.18] | 0.94 [0.51–1.74] |
| ≥ $150,000 | 2.20 [1.33–3.66] | 1.32 [0.63–2.77] |
| Child < 18 years | ||
| No | 1.0 | 1.0 |
| Yes | 1.05 [0.81–1.36] | 0.90 [0.61–1.34] |
| COVID-19 Vaccine Information Sources | 1.11 [1.05–1.18] | 1.08 [0.98–1.18] |
| Past influenza vaccine | ||
| No | 1.0 | 1.0 |
| Yes | 2.44 [1.85–3.23] | 1.41 [0.89–2.26] |
| Influenza vaccine last year | ||
| No | 1.0 | 1.0 |
| Yes |
2.61 [2.01–3.39] |
1.39 [0.90–2.13] |
|
Health Belief Model Domains |
||
| Perceived Severity of the Virus (n = 941) | 1.66 [1.42–1.94] | 1.44 [1.09–1.91] |
| If I get COVID-19, I will get sick | ||
| If I get COVID-19, other members in my home will get sick | ||
| If I get COVID-19, I will lose income | ||
| If I get COVID-19, I will die | ||
| Perceived Susceptibility to the Virus (n = 948) | 1.67 [1.45–1.93] | 1.01 [0.81–1.27] |
| I am at risk for getting COVID-19 | ||
| Individuals in my household are at risk for getting COVID-19 | ||
| I feel knowledgeable about my risk for getting COVID-19 | ||
| Perceived Clinical Barriers to Vaccination | 0.90 [0.75–1.08] | 0.97 [0.67–1.42] |
| I will have side effects from the COVID-19 vaccine | ||
| The COVID-19 vaccine will be safe | ||
| I will get sick from the COVID-19 vaccine | ||
| I will die from the COVID-19 vaccine | ||
| The COVID-19 vaccine will be painful | ||
| Perceived Access Barriers to Vaccination | 0.95 [0.83–1.09] | 0.79 [0.61–1.02] |
| It will be hard for me to get the COVID-19 vaccine | ||
| There will not be enough of the COVID-19 vaccine for me | ||
| The COVID-19 vaccine will cost me a lot of my own money | ||
| Perceived COVID-19 Specific Vaccine Benefit | 4.35 [3.58–5.28] | 2.82 [2.24–3.56] |
| The COVID-19 vaccine will help things go back to normal | ||
| If I receive the COVID-19 vaccine, it will protect me from COVID-19 | ||
| Perceived General Vaccine Benefits | 3.10 [2.64–3.64] | 1.77 [1.41–2.21] |
| Vaccines prevent disease | ||
| Vaccines are safe | ||
Three demographics variables remained significant predictors of intention to receive the COVID-19 vaccine in the adjusted logistic regression model. Females had lower odds of intending to receive the COVID-19 vaccine than males (AOR = 0.54, 95% CI: 0.36–0.80). Those with a 2-year degree/some college had lower odds of intending to receive the COVID-19 vaccine than those with a high school/GED degree (AOR = 0.59, 95% CI: 0.36–0.97). Respondents located in the West had higher odds of intending to receive the COVID-19 vaccine than those located in the South (AOR = 1.80, 95% CI: 1.09–2.96).
Health Belief Model domain predictors of intention to receive the COVID-19 vaccine
Perceived severity of the COVID-19 virus
Respondents who perceived the severity of the virus to be greater had higher odds of intending to receive a COVID-19 vaccine (OR = 1.66, 95% CI: 1.42–1.94). Perceived severity of the virus remained a significant predictor of intention to receive a COVID-19 vaccine in the adjusted logistic regression model (AOR = 1.44, 95% CI: 1.09–1.91).
Perceived susceptibility to the COVID-19 virus
A higher perceived susceptibility to the virus was associated with higher odds of intending to receive the COVID-19 vaccine (OR = 1.67, 95% CI: 1.45–1.93). The HBM domain of perceived susceptibility did not retain significance in the adjusted logistic regression model.
Perceived COVID-19 specific and general vaccine benefits
Respondents with a higher perceived COVID-19 vaccine benefit had higher odds of intending to receive the COVID-19 vaccine in both unadjusted and adjusted logistic regression models (OR = 4.35, 95% CI: 3.58–5.28 and AOR = 2.82, 95% CI: 2.24–3.56). Those who perceived greater overall general vaccine benefits also had higher odds of intending to receive a COVID-19 vaccine (OR = 3.10, 95% CI: 2.64–3.64 and AOR = 1.77, 95% CI 1.41–2.21).
Perceived clinical and access barriers to COVID-19 vaccination
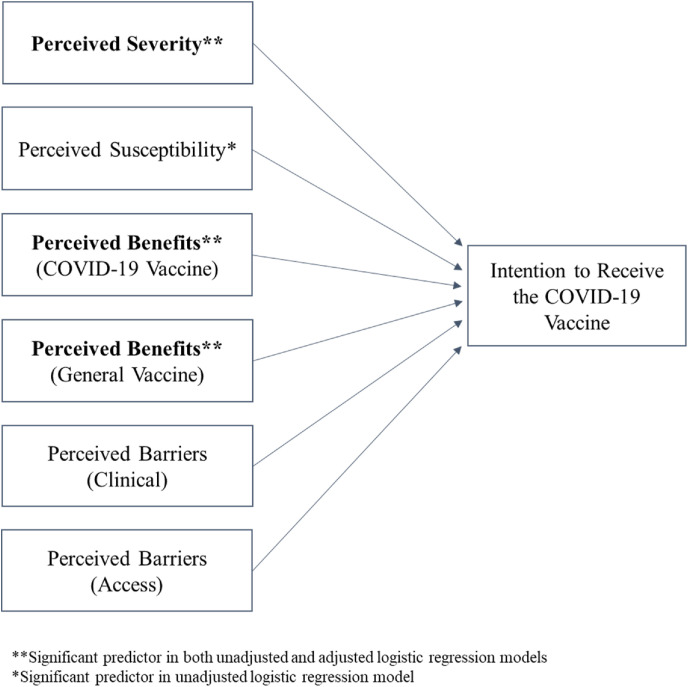
Respondents’ perceived clinical and access barriers to COVID-19 vaccination were not significant predictors of intention to receive the COVID-19 vaccine. Summary responses to the HBM domains are provided in Supplemental Table 3. Fig. 1 provides the conceptual model for this study with significant HBM domains.
Fig. 1.
Adapted health belief model domains and intention to receive the COVID-19 vaccine.
Discussion
This study found that roughly 6 in 10 adults in the US intend to receive a COVID-19 vaccine if offered. This finding is slightly lower than other surveys conducted in the US, which found 67–69% of adults reported a willingness to get a COVID-19 vaccine,10 , 12 , 13 but higher than other parts of the world.14 , 15 Though most respondents in this US study intended to receive the COVID-19 vaccine, it is still a significant public health concern that 40% did not intend to get the vaccine.
For the HBM domains in this study, perceived severity of the virus, perceived greater COVID-19 vaccine benefit, and perceived overall general vaccine benefits were all predictors of the respondent's intention to receive a COVID-19 vaccine. These findings are consistent with previous studies on vaccination that support the notion that detecting the behaviors, beliefs, and perceptions of respondents will likely increase vaccine uptake and decrease health disparities in vaccine receipt.6 , 9, 10, 11, 12 , 16 Other HBM domains in this study, perceived COVID-19 virus susceptibility, clinical barriers, and access barriers to the COVID-19 vaccine were not significant predictors of the respondent's intention to receive the COVID-19 vaccine in the multivariable model. In contrast, one study indicated that perceived severity was not a significant predictor of intention to receive the COVID-19 vaccine.17 The study by Guidry et al. found that perceived susceptibility, benefits, barriers, and self-efficacy were predictors of vaccine uptake intent.17 The variance of significant HBM predictors across studies indicates a need to determine each individual's concerns and provide concordant vaccine education.
This study supports that strategies to increase COVID-19 vaccine uptake should address the HBM domains of perceived virus severity and belief in vaccine benefits. Evidence-based strategies may include using effective communication (e.g., motivational interviewing) to educate patients and reinforcing the role of community protection (vaccine benefits) to increase vaccine receipt.18 A recent study indicated that perceived community benefit was associated with respondents’ intention to receive a COVID-19 vaccine.19
Although not a significant finding in this group of survey respondents, addressing concerns about immunization side effects or barriers is recommended as a strategy to increase vaccine uptake. Studies have indicated that safety concerns or barriers were associated with a negative intention to receive a COVID-19 vaccine and addressing these patient-specific concerns may increase vaccine receipt.17 , 19
Our findings suggest that those who were likely to intend to receive a COVID-19 vaccine were comfortable receiving the vaccination at a doctor's office, a pharmacy, or a drive-through car site, based on the survey options provided. For those who are likely to receive a COVID-19 vaccine, improved convenience and access to vaccines are strategies to increase vaccine uptake.20 With these findings, public health officials should increase the number of accessible community-based vaccination sites, such as doctor's offices, pharmacies, large vaccination events, local churches, and schools.
In this study, females were less likely to intend to receive a COVID-19 vaccine which is consistent with previous survey research on acceptance of the COVID-19 vaccine.10 , 11 In only the unadjusted model, self-reported Black or Other race respondents were less likely to intend to receive the COVID-19 vaccine than White respondents. Another survey indicated that Black race respondents compared to White race respondents were less likely to intend to get the COVID-19 vaccine, including under emergency use authorization.17 This study found that respondents with an annual household income of less than $15,000 were less likely to intend to receive the COVID-19 vaccine in an unadjusted model, similar to another study.13 Variation in intent to receive the COVID-19 vaccine was seen by region of the US, as seen in work by Malik et al.12 This study demonstrates that intention to receive the COVID-19 vaccine differs across demographic characteristics, such as education level, area of the US, and gender. This highlights the need for vaccination strategies that specifically address certain demographic groups.
Limitations
While this study's demographics were matched to the US adult population, participation was limited to those who participate in Qualtrics survey panels, which may not reflect the overall population. A second limitation is that trust was not included as a survey component and cannot be assessed as a predictor of vaccine receipt. Another limitation is the changing context of COVID-19 vaccine information and news reporting. This study was conducted in mid-August 2020 before emergency use authorization of COVID-19 vaccines. Another limitation is that this study did not examine the actual health behavior of receiving a COVID-19 vaccine. However, this study provides useful information on vaccine perceptions before a vaccine is available to the public that may help design future pandemic responses. Each day during the pandemic brings new information to the public, which may affect respondent perceptions.
Conclusions
The level of vaccine uptake will likely be a major factor in resolving the COVID-19 pandemic. These findings demonstrate that intention to receive the COVID-19 vaccine varied across demographics, perceived virus severity, and vaccine beliefs. Thus, successful implementation of a COVID-19 immunization campaign by healthcare providers and public health officials will need to incorporate diverse COVID-19 vaccination education strategies tailored to patients' health beliefs that encourage vaccine acceptance and receipt.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Coe: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Supervision, Roles/Writing - original draft, Writing - review & editing.
Elliott: Conceptualization, Data curation, Formal Analysis, Methodology, Roles/Writing - original draft, Writing - review & editing.
Gatewood: Conceptualization, Methodology, Writing - review & editing.
Goode: Conceptualization, Methodology, Writing - review & editing.
Moczygemba: Conceptualization, Methodology, Supervision, Writing - review & editing.
Declaration of competing interest
J-VRG served as an advisor for Valneva, outside of this work. All other authors have no relevant disclosures.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2021.04.023.
Appendix A. Supplementary data
The following are the Smentary data to this article:
References
- 1.World Health Organization Listing of WHO's response to COVID-19. https://www.who.int/news-room/detail/29-06-2020-covidtimeline
- 2.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19) – about COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/cdcresponse/about-COVID-19.html
- 4.Johns Hopkins University Coronavirus Resource Center World map and U.S. Map. https://coronavirus.jhu.edu/map.html
- 5.Schaffer DeRoo S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. J Am Med Assoc. 2020;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 6.Larson H.J., Jarrett C., Eckersberger E., Smith D.M.D., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2020;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- 8.Skinner C.S., Tiro J., Champion V.L. In: fifth ed. Glanz K., Rimer B.K., Viswanath K., editors. Jossey-Bass; San Francisco, CA: 2015. The Health Belief Model; pp. 75–94. (Health Behavior: Theory, Research, and Practice). [Google Scholar]
- 9.Coe A.B., Gatewood S.B.S., Moczygemba L.R., Goode J.V.R. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innov Pharm. 2012;3(2):1–11. doi: 10.24926/iip.v3i2.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kreps S., Prasad S., Brownstein J.S., et al. Factors associated with US adults' likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malik A.A., McFadden S.A.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;Sep;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mercadante A.R., Law A.V. Will they, or Won't they? Examining patients' vaccine intention for flu and COVID-19 using the Health Belief Model. Res Soc Adm Pharm. 2020 Dec 30 doi: 10.1016/j.sapharm.2020.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong M.C.S., Wong E.L.Y., Huang J., et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39:1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tran V.D., Pak T.V., Gribkova E.I., et al. Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia. Pharm Pract. 2021;Jan-Mar;19(1):2776. doi: 10.18549/PharmPract.2021.1.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sadaf A., Richards J.L., Glanz J., Salmon D.A., Omer S.B. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine. 2013;31(40):4293–4304. doi: 10.1016/j.vaccine.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Guidry J.P.D., Laestadius L.I., Vraga E.K., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Contr. 2021;49:137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDonald N.E., Butler R., Dubé E. Addressing barriers to vaccine acceptance: an overview. Hum Vaccines Immunother. 2018;14(1):218–224. doi: 10.1080/21645515.2017.1394533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chu H., Liu S. Integrating health behavior theories to predict American's intention to receive a COVID-19 vaccine. Patient Educ Counsel. 2021 Feb 17 doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomson A., Robinson K., Vallee-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.