Abstract
ORDINARY HUMAN REASONING MAY LEAD PATIENTS to provide an unreliable history of past experiences because of errors in comprehension, recall, evaluation and expression. Comprehension of a question may change depending on the definition of periods of time and prior questions. Recall fails through the loss of relevant information, the fabrication of misinformation and distracting cues. Evaluations may be mistaken because of the “halo effect” and a reluctance to change personal beliefs. Expression is influenced by social culture and the environment. These errors can also occur when patients report a history of present illness, but they tend to be more prominent with experiences that are more remote. An awareness of these specific human fallibilities might help clinicians avoid some errors when eliciting a patient's past medical history.
Eliciting a patient's past medical history is an essential clinical skill. Doing so is sometimes the only way to determine whether a patient's health is getting worse, what will go wrong next and what has failed in the past. Neglecting the past medical history can cause a physician inadvertently to discontinue important medications, prescribe an incorrect dose of chronic medications, duplicate a low-yield diagnostic test, neglect an earlier directive or disrupt plans made by previous clinicians.1 Problems may become further compounded given that some of the hardest patients to treat are also those with the most complex past medical histories.
Consider a middle-aged woman whom you are treating for a corneal abrasion and who also has a history of chronic fatigue. The fatigue began 1 or 2 years ago and is not worse after exercise. The patient remembers eating some unusual food just before the fatigue started, but she cannot recall anything else even after a detailed review. She has seen other doctors about this problem, but says that they did not take her seriously. She is convinced that something is wrong. She does not seem to be hiding any details, and the privacy of your office has assured her confidentiality.
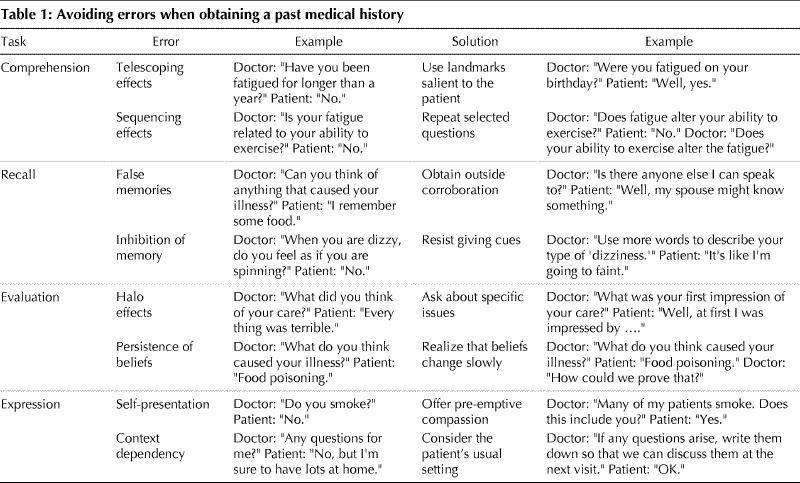
In this article we discuss 8 traps hidden in this past history that could cause a physician to miss the diagnosis. The previous article in this series reviewed observations from psychology relevant to the fallibility of patients' reporting of current symptoms.2 The mistakes stem from 4 tasks that are implicitly imposed on patients when they are asked to describe how they feel: comprehension, recall, evaluation and expression. This framework also applies to how patients report their past medical history. Within this framework, we list further problems that are more important when the experiences are more remote (Table 1).
Table 1
Comprehension
Telescoping effects
One distinctive element in providing a history of past illness relates to the intellectual gymnastics involved in conceptualizing long-term personal information. For example, most patients can tell whether they are currently in pain. Ask the same patient whether he or she was in pain a year ago, however, and an accurate reply is not as easy (especially if the patient is sick right now). Such difficulties in conceptualizing the past can explain, for example, why patients often have trouble determining whether their knee pain has progressed to the point where surgery is warranted.3,4 In general, people are better at remembering events and actions rather than thoughts and intensities.
A particular source of confusion in the past medical history relates to specifying the relevant time interval for the patient. The concept of “the present” is unambiguous, whereas the concept of “the past” can have a murky boundary. Although one might imagine that errors would be symmetrically distributed around the truth, the dominant error is to assign a date to an event that is more recent than the actual occurrence. This bias, called the “telescoping effect,” has the net effect of overestimating the frequency of repeated events and exaggerating the acuteness of unique events. For example, a patient may count a tetanus vaccination from 14 years ago as being within the past decade and may thereby decline a booster dose.
Telescoping effects imply that items that are outside the boundary are inappropriately included in the reference time interval. For example, residents of Seattle were interviewed 6 months after the eruption of the Mount Saint Helens volcano.5 Those asked “In the last 6 months, did anyone try to rob you?” were more likely to report an event than those asked “Since the eruption of Mt. St. Helens, has anyone tried to rob you?” (9.2% v. 1.5%, p < 0.05). Later verification found that almost all the events mentioned by the first group had occurred prior to the designated 6-month interval. This study shows the telescoping effect, namely, a 6-fold overreporting, and also shows that one way to reduce the bias is to avoid calendar dates and use salient landmarks to aid perspective. In medicine, salient landmarks could include major holidays, life events and other milestones meaningful to the patient.
Sequencing effects
Misunderstandings concerning a past medical history may also occur because a lot of questions are asked in an extremely arbitrary order, and the sequence of 2 questions can change a person's responses. In one study, for example, college students were asked how happy they felt and how often they were dating.6 Half were asked about their happiness before the dating question: the responses showed no correlation (r = -0.12, p = 0.33). In contrast, the other half were asked about their happiness after the dating question: their responses showed a high correlation (r = 0.66, p < 0.001). One might draw different conclusions about the link between dating and happiness from these 2 statistics. Similarly, patients' descriptions of their exercise capacity and their fatigue might change depending on which question was asked first.
Several factors can cause a person's interpretation of one question to change depending on prior questions. For example, personal experiences are not always immediately remembered, so that a preceding question might stimulate selective memories that colour subsequent responses. Whatever the explanation, medical histories are vulnerable to similar problems because the physician usually asks many questions and needs to exercise judgement about their sequence. Another physician might obtain different answers simply by phrasing questions slightly differently or by following an alternative line of inquiry. One way to double-check for such interactions is to deliberately ask the same question a few times in different ways at different points in the history.
Textbooks emphasize that questions should be sequenced in a sensible manner. For example, asking about alcohol is difficult at the start or finish of the history. At the start, it creates an image of a physician anxious to find blame. At the finish, it leaves the patient with a disturbing last impression. Asking about alcohol in a few different ways in the middle of an interview is a way to obtain a reliable response. Yet doing so requires tact because the physician's approach can be misconstrued as inattentive or overly suspicious. A failure to check for inconsistencies, however, may be the more common mistake.7
Recall
False memories
Patients' long-term memories often fail through both the loss of relevant information and the fabrication of misinformation. In one study, investigators asked participants to remember events from their childhood.8 A small book of 4 stories had been created for each person: 3 about actual events in the person's life and one about a fictitious event. After each story, the participant was instructed to write what they recalled about the event or to write “I do not remember this.” Surprisingly, many participants remembered the false event, albeit at a lower rate than the real events (29% v. 68% respectively).
Apparently, the landscape of memory is clouded by both fog and mirages. That is, people can be coaxed into remembering events that never happened. Studies suggest that the mirages may intensify with time, can induce people to accept guilt for a crime that they did not commit and may be difficult even for experts to separate from factual accounts.9 In the courtroom, false memories are distinguished from true memories by seeking corroborating information. Yet in medicine, the subjective nature of symptoms makes this standard awkward to apply.10,11 Corroboration can be essential, for example, to verify whether a frail elderly individual living in the community has been eating properly at home.
Some experiences seem impossible to forget. In particular, events are well remembered if they induce strong emotions when they happen, retain their original significance, stay relatively unusual and mark transitional points in life.12 Studies of the reliability of eyewitnesses, however, suggest that memories of emotional events are also prone to distortion because emotional events are discussed with friends, and embellishments to improve the story become incorporated into the memory of the event.13 This difficulty may explain some cases in which patients make false allegations.14,15,16 In medicine, one clue to such embellishments might be if a history seems overly perfect.
Inhibition of memory
Clinicians sometimes provide cues to help patients overcome mild forms of forgetfulness, yet such good intentions can have unintended consequences. Consider a group of students who were asked to memorize a list of 30 words.17 Afterwards, half were given 29 of the words and were asked only to recall the remaining target word. The other half were asked to recall the full list, a much larger task, but were evaluated only on their ability to recall the same target word. Overall, fewer individuals in the prompted than in the unprompted group recalled the target word (20% v. 55%, p = 0.02). Evidently, neutral cues (such as lengthy checklists18) might sometimes inhibit people's ability to remember.
The inhibition of memory by neutral cues appears to violate common sense and everyday experiences. The easiest explanation is that weaker memories are suppressed by stronger memories.19 In the clinical setting, physicians who wish to facilitate patients' recall must be patient and avoid offering cues for as long as possible. This type of advice often appears in standard medical textbooks as a recommendation against directive cues. The implication from research in psychology, however, is that even neutral cues can interfere with a patient's memory. A silent pause may sometimes help the patient more than any clever words.
Any cue has the potential to cause distortion. Indeed, inadvertent changes in body language or eye contact might also indirectly change a patient's focus. This is one reason, for example, why clinical trials strive for double-blinding in both patients and clinicians. Being a good interviewer requires self-control. Yet even perfect self-control is insufficient when the physician follows others who have recently seen the patient and have offered cues. The situation is perhaps at its worst in a teaching hospital when a staff physician arrives, following other clinicians, and finds the history to be miraculously simple.
Evaluation
Halo effects
Other errors occur because people may be unaware of the mental processes that form the basis of their evaluations. Consider students who were shown a film of a foreign teacher.20 Half were shown the teacher acting in a pleasant, agreeable and enthusiastic way. The other half were shown the teacher acting in an autocratic, rigid and intolerant style. Students who saw the pleasant version gave more positive ratings to the teacher's appearance, mannerisms and accent (p < 0.001 for each) than students who saw the unpleasant version, even though these 3 attributes were the same in both versions.
This demonstration shows that people's subjective evaluations are influenced by extraneous factors. As a consequence, their explanations may be unreliable even when their judgements seem credible. The preceding example shows that evaluations of one attribute (general likeability) often spill over to influence the evaluation of other attributes (accent). This phenomenon is called the “halo effect.” Capable people may be unaware of the influence of such a phenomenon and only infrequently mention the issue in their explanations. This can be one reason, for example, why obstetricians are either loved or despised by patients but rarely remembered as average.21,22
One other result of a halo effect is that patients may exaggerate their descriptions of treatments at the extremes of success (or failure). As a corollary, one complication could undo years of diligent care and lead a patient to view her or his physician as totally incompetent. Because disappointments will generally lead patients to seek care elsewhere, the original physician may never receive feedback (and may miss the opportunity to make corrections) and the next physician may be greeted with inflated hope (and the cycle repeated). Clinicians, therefore, must be a bit sceptical about a patient's report of past care received elsewhere. Clinicians should also know that high praise from patients is no guarantee of their continued satisfaction.23
Persistence of beliefs
Taking a history also involves listening to the patient's beliefs about why the illness has occurred. Such introspection can sometimes be valuable and sometimes misleading, such as a potential misconception about changes in arthritis being related to changes in the weather.24 One explanation is that people focus on coincidences, capitalize on chance and neglect contrary data. For arthritis, doing so leads patients to look for changes in the weather only when they experience increased pain; furthermore, weather patterns have so many components, time lags and combinations that it's not hard to find at least one coincidence. A lifetime of experiences may do nothing to rectify a misconception.
Studies such as these provide a gloomy assessment of human judgement by suggesting that patients' opinions can be mistaken, even when patients have substantial experience of life. Further work indicates that experiences that are mixed or ambiguous are especially prone to entrench people in their views rather than encouraging a neutral position. This phenomenon is especially disturbing when taking a patient's past history because the situations are usually complicated and the data are almost always a bit ambiguous. No wonder, therefore, that sorting out claims about drug allergies or herbal remedies is difficult.
Psychological research also suggests some methods for helping patients change their unfounded beliefs. First, people need to be reminded that the scientific method requires deliberate checking for contradictory evidence (rather than searching for confirmatory evidence). For example, ask the patient who “has never had back pain as bad as this before” to describe the current episode and, in addition, to recall one past episode that was also quite bad. Second, recognize that an anecdote is sometimes more persuasive than a raft of studies, so that one testimonial about a herbal cure may be impossible for the physician to overturn.
Expression
Self-presentation
Sometimes respondents give consistent but inaccurate reports for fear of embarassment. In one study, for example, college students reported higher well-being in personal interviews than in self-administered surveys.25 The difference was more pronounced when the interviewer was of the opposite sex. Apparently, respondents sometimes embellish their position in order to impress others. Public reports of past problems, therefore, may not always match private perceptions even if people are reminded about the importance of honest and complete responses.
Issues related to self-presentation are clinically important for several reasons. First, the distortions are generally more pronounced in face-to-face interviews (standard for physicians) than in written surveys (standard for researchers). Second, the distortions are worsened when the interviewer is an authority (such as a doctor) rather than a peer (such as a companion). Third, the distortions are exacerbated when respondents believe they share blame instead of just being neutral witnesses. The simplest thing a clinician can do to overcome a patient's inhibitions is to offer pre-emptive compassion; for example, “Everyone has something they do. Which vice do you find hardest to resist?”
No patient wants to appear foolish. To avoid seeming so, individuals sometimes adopt attitudes to match their past actions as a way of appearing consistent. In one experiment, participants were asked to turn wooden knobs for a full hour (a dull task).26 Half were paid $1 and half were paid $20. Contrary to the usual notion that bigger rewards produce bigger effects, those given insufficient payment gave higher ratings for their enjoyment of the task. That is, participants attempted to justify their actions by rationalizing their enjoyment of the activity. A similar paradox might occur in patients who choose to undergo unpleasant surgery, achieve no objective response, but enthusiastically report their improvement.27
Context dependency
Another type of reporting bias relates to context-dependent recall. In a clever demonstration, scuba divers were asked to memorize a list of words either while on land or while underwater.28 Recall was then tested either in the same or in the other setting. As expected, those who both memorized and recalled on land had the best results (38% correct). Those who both memorized and recalled underwater also did fairly well (32% correct). The surprising observation was that those who memorized and recalled in dissimilar settings did particularly poorly (24% correct, in both cases). This effect of context-dependent recall has no simple biologic explanation but may be another reason why patients forget important points when visiting a doctor's office.
The malleable nature of individual reporting calls for specific interventions by physicians. Clinicians should consider the patient's customary setting and recognize that house calls can provide special insights, not only in what the clinician can witness but also in what the patient can recall. Clinicians should recognize that a patient's chief complaint and vital signs in an ambulance may not match the patient's chief complaint and vital signs on arrival at the emergency department, not because of the fallibility of paramedic assessments but because of an abrupt change in the person's surroundings. Finally, clinicians should remember that an awareness of major events in a patient's social situation is both good manners and good science.
Conclusion
This article reviews classic observations from psychology that are relevant when taking a past medical history. The patient case in the introduction describes a situation that contains each of the 8 specific traps: telescoping effects, sequencing effects, false memories, inhibition of memory, halo effects, persistence of beliefs, self-presentation and context dependency (Table 1). Such biases may explain why one of us (D.A.R.) missed the correct diagnosis for this patient who eventually was admitted to hospital because of domestic violence. More generally, problems related to a patient's failure of comprehension, recall, evaluation and expression cause mistakes when a physician is taking a past medical history.
Articles to date in this series .
Redelmeier DA, Ferris LE, Tu JV, Hux JE, Schull MJ. Problems for clinical judgement: introducing cognitive psychology as one more basic science. CMAJ 2001;164(3):358-60.
Redelmeier DA, Schull MJ, Hux JE, Tu JV, Ferris LE. Problems for clinical judgement: 1. Eliciting an insightful history of present illness. CMAJ 2001;164(5):647-51.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Donald A. Redelmeier, Sunnybrook & Women's College Health Sciences Centre, Rm. G151, 2075 Bayview Ave., Toronto ON M4N 3M5; fax 416 480-6048; dar@ices.on.ca
References
- 1.Redelmeier DA. A Canadian perspective on the American hospitalist movement. Arch Intern Med 1999;159:1665-8. [DOI] [PubMed]
- 2.Redelmeier DA, Schull MJ, Hux JE, Tu JV, Ferris LE. Problems for clinical judgement: 1. Eliciting an insightful history of present illness. CMAJ 2001;164(5):647-51. Available: www.cma.ca/cmaj/vol-164/issue-5/0647.htm [PMC free article] [PubMed]
- 3.Wright JG, Hawker GA, Bombardier C, Croxford R, Dittus RS, Freund DA, et al. Physician enthusiasm as an explanation for area variation in the utilization of knee replacement surgery. Med Care 1999;37:946-56. [DOI] [PubMed]
- 4.Redelmeier DA, Kahneman D. Patients' memories of painful medical treatments: real-time and retrospective evaluations of two minimally invasive procedures. Pain 1996;66:3-8. [DOI] [PubMed]
- 5.Loftus EF, Marburger W. Since the eruption of Mt. St. Helens, has anyone beaten you up? Improving the accuracy of retrospective reports with landmark events. Mem Cognit 1983;11:114-20. [DOI] [PubMed]
- 6.Strack F, Martin LL, Schwarz N. Priming and communication: social determinants of information used in judgments of life satisfaction. Eur J Soc Psychol 1988;18:429-42.
- 7.Macleod J. Clinical examination. 6th ed. New York (NY): Churchill Livingstone; 1983. p. 3.
- 8.Loftus EF. Creating false memories. Sci Am 1997;277:70-5. [DOI] [PubMed]
- 9.Loftus EF, Polage DC. Repressed memories. When are they real? How are they false? Psychiatr Clin North Am 1999;22:61-70. [DOI] [PubMed]
- 10.Small GW, Borus JF. The influence of newspaper reports on outbreaks of mass hysteria. Psychiatr Q 1987;58:269-78. [DOI] [PubMed]
- 11.Boakes J. False complaints of sexual assault: recovered memories of childhood sexual abuse. Med Sci Law 1999;39:112-20. [DOI] [PubMed]
- 12.Linton M. Transformations of memory in everyday life. In: Neisser U, editor. Memory observed. San Francisco (CA): U.H. Freeman and Co.; 1982.
- 13.Quas JA, Goodman GS, Bidrose S, Pipe ME, Craw S, Ablin DS. Emotion and memory: children's long-term remembering, forgetting, and suggestibility. J Exp Child Psychol 1999;72:235-70. [DOI] [PubMed]
- 14.Sjoberg RL. False allegations of satanic abuse: case studies from the witch panic in Rattvik 1670-71. Eur Child Adolesc Psychiatry 1997;6:219-26. [DOI] [PubMed]
- 15.Carter RM. Malpractice and avascular necrosis: legal outcomes. Can J Gastroenterol 1999;13:79-84. [DOI] [PubMed]
- 16.Ross SE. “Memes” as infectious agents in psychosomatic illness. Ann Intern Med 1999;131:867-71. [DOI] [PubMed]
- 17.Slamecka NJ. An examination of trace storage in free recall. J Exp Psychol 1968;76:504-13. [DOI] [PubMed]
- 18.Hardy JR, Edmonds P, Turner R, Rees E, A'Hern R. The use of the Rotterdam Symptom Checklist in palliative care. J Pain Symptom Manage 1999;18: 79-84. [DOI] [PubMed]
- 19.Tulving E, Hastie R. Inhibition effects of intralist repetition in free recall. J Exp Psychol 1972;92:297-304.
- 20.Nisbett RE, Wilson TD. Telling more than we can know: verbal reports on mental processes. Psychol Rev 1977;84:231-58.
- 21.Fischhoff B. Hindsight does not equal foresight: the effect of outcome knowledge on judgment under uncertainty. J Exp Psychol Hum Percept Perform 1975;41:288-99.
- 22.Tucker JS, Hall MH, Howie PW, Reid ME, Barbour RS, Florey CD, et al. Should obstetricians see women with normal pregnancies? A multicentre randomised controlled trial of routine antenatal care by general practitioners and midwives compared with shared care led by obstetricians. BMJ 1996;312:554-9. [DOI] [PMC free article] [PubMed]
- 23.Dawson NV, Arkes HR, Siciliano C, Blinkhorn R, Lakshmanan M, Petrelli M. Hindsight bias: an impediment to accurate probability estimation in clinicopathologic conferences. Med Decis Making 1988;8:259-64. [DOI] [PubMed]
- 24.Redelmeier DA, Tversky A. On the belief that arthritis pain is related to the weather. Proc Natl Acad Sci U S A 1996;93:2895-6. [DOI] [PMC free article] [PubMed]
- 25.Strack F, Schwarz N, Chassein B, Kern D, Wagner D. The salience of comparison standards and the activation of social norms: consequences for judgments of happiness and their communication. Br J Soc Psychol 1990;29:303-314.
- 26.Festinger L, Carlsmith JM. Cognitive consequences of forced compliance. J Abnorm Soc Psychol 1959;58:203-10. [DOI] [PubMed]
- 27.The EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med 1985;313:1191-200. [DOI] [PubMed]
- 28.Godden DR, Baddeley AD. Context-dependent memory in two natural environments: on land and underwater. Br J Psychol 1975;66:325-31.


