Abbreviation
- PBC
primary biliary cholangitis
Hepatitis at its basic definition simply means inflammation of the liver. The term hepatitis may also be used when there is injury to hepatocytes without significant inflammation. Numerous conditions lead to hepatitis. The pattern and composition of the inflammation seen in the liver often is associated with a differential diagnosis. This article focuses on common patterns seen in adults. The patterns seen in the pediatric population vary significantly. Most patterns are not specific and should be correlated with the clinical situation. Serological testing for viral infection and autoimmune conditions are routine in defining the probable etiology of liver abnormalities. Four common patterns of inflammation are discussed in this article. Each of these patterns prompts a differential diagnosis that is discussed later (Table 1).
TABLE 1.
Principle Histologic Features and Associated Differential Diagnosis of Hepatitis and Cholangitis
| Patterns of Hepatitis and Cholangitis | Main Histology Features | Associated Diseases |
|---|---|---|
| Portal and lobular hepatitis | Variable amounts of lobular and portal inflammation with associated hepatocyte damage | Viral hepatitis |
| Drug‐induced injury | ||
| Autoimmune hepatitis | ||
| Chronic biliary cholangitis (PBC) | ||
| Steatohepatitis | Steatosis with ballooning degeneration with one or more of the following: Mallory hyaline, lobular neutrophilic inflammation, and sinusoidal fibrosis | Alcoholic steatohepatitis |
| Nonalcoholic steatohepatitis (metabolic syndrome) | ||
| Amiodarone toxicity | ||
| Granulomatous hepatitis | Collections of macrophages often with multinucleated giant cells; granulomas may be necrotizing or nonnecrotizing | Infections (usually necrotizing) (bacterial, viral, mycobacterial, and fungal) |
| Sarcoidosis (usually nonnecrotizing) | ||
| PBC (usually duct centered) | ||
| Cholangitis | Inflammation of the bile ducts; this may be neutrophilic or lymphocytic or granulomatous | Obstructive cholangitis |
| Ascending or infectious cholangitis | ||
| Cholangitis lenta (nonsuppurative cholangitis) |
Portal and Lobular Hepatitis
The most common pattern of hepatitis is an infiltrate of inflammatory cells that involves the portal tracts with a variable level of lobular inflammation. Lobular inflammation may include interface hepatitis 1 , 2 , 3 (portal inflammation that is associated with damage to adjacent hepatocytes), spotty necrosis (necrosis or loss of small groups of hepatocytes within the lobules associated with inflammation), apoptosis, or individual cell necrosis with or without associated inflammation, sinusoidal inflammation (diffuse infiltrate within the sinusoids) or pericentral (often accompanied with hepatocyte lose).
This common pattern of portal and lobular hepatitis was originally described as and is commonly associated with viral hepatitis (Fig. 1). Hepatitis B and C are the most common types. This pattern is also seen in primary biliary cholangitis (PBC), autoimmune hepatitis, and drug toxicity. Although this pattern is nonspecific, there are features that are characteristic of some diseases. Hepatitis C tends to have a monomorphic (lymphocyte‐rich) infiltrate. Hepatitis B has ground‐glass hepatocytes and tends to have more pleomorphic infiltrate with plasma cells and eosinophils. PBC is duct centered and is associated with epithelioid granulomas. Autoimmune hepatitis tends to be plasma cell rich. Drug toxicity often is associated with cholestasis but, depending on the drug, can vary substantially.
FIG 1.

Four examples of portal and lobular hepatitis. (A) Drug‐induced hepatitis with lobular and portal mononuclear inflammation. The star identifies the portal tract. (B) Predominantly portal hepatitis with fibrosis in a patient with hepatitis C. (C) Lobular hepatitis with ground‐glass hepatocytes (arrows) in a patient with hepatitis B. (D) Cytomegaloviral hepatitis demonstrating a localized area of neutrophilic inflammation with an associated characteristic viral inclusion (arrow).
Steatohepatitis
Steatohepatitis is a pattern of hepatitis that is very distinctive and has a limited differential diagnosis that is easily determined with clinical correlation. 4 , 5 The morphology is composed of fatty change with one or more findings of hepatocyte injury, such as ballooning degeneration, Malory hyaline, and inflammation (Fig. 2). With time, this results in sinusoidal fibrosis that is characteristic. Portal inflammation may be seen in many cases but is usually not prominent.
FIG 2.

Steatohepatitis. (A) Hematoxylin and eosin–stained tissue with fatty change, ballooning degeneration of hepatocytes with accumulation of Malory hyaline (arrow). Scattered inflammatory cells are also seen. (B) Trichrome stain highlights sinusoidal fibrosis (arrows) that is characteristic of steatohepatitis.
The differential diagnosis includes alcoholic and nonalcoholic steatohepatitis. There are many publications that try to distinguish between these two entities based on morphological findings, but the differences tend to be qualitative and subjective and not as reliable as good clinical correlation.
Notably, there is a drug toxicity pattern that mimics steatohepatitis. This has been seen in cardiac patients who are taking the drug amiodarone.
Granulomatous Hepatitis
Granulomatous hepatitis is defined as an inflammatory condition involving the liver with a substantial component of granulomas. 6 , 7 Granulomas are a spectrum of findings that are characterized by collections of macrophages. They may be very small, composed of only a few histiocytes. In contrast, granulomas could present as a substantial mass lesion (several centimeters). Although the differential diagnosis for granulomatous inflammation of the liver is wide, they are commonly classified as necrotizing or caseating versus nonnecrotizing (Fig. 3). More commonly, necrosis is seen in infectious conditions. Some infections, however, may be seen with nonnecrotizing granulomas. Lipogranulomas are the most common type of granuloma seen in the liver. They are thought to represent coalescence of macrophages in the elimination of fat from the liver. A condition that commonly affects the liver and has a component of granulomas is PBC. In this condition, small granulomas often are seen involving bile ducts or adjacent to bile ducts. Sarcoidosis is another granulomatous condition that may have characteristic features. Sarcoid granulomas are typically nonnecrotizing and lack a cuff of lymphocytes. This is often referred to as a “naked” granuloma. They may have giant cells and often contain asteroid bodies. With a prolonged duration of sarcoidosis in the liver, granulomas may be seen in a background of fibrosis with minimal other inflammatory cells.
FIG 3.
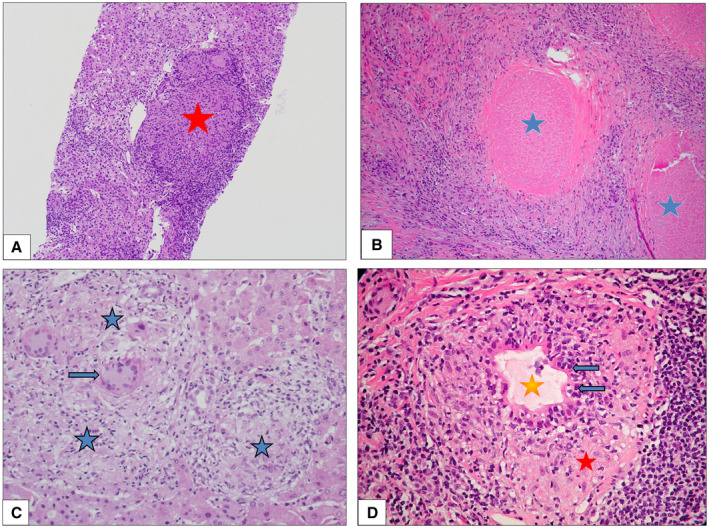
Granulomatous hepatitis is demonstrated. (A) Nonnecrotizing granulomatous hepatitis is present with a well‐formed granuloma (star) that contains a giant cell. (B) Necrotizing granulomatous inflammation with destruction of the hepatic parenchyma (stars identify areas of necrosis). (C) Sarcoidosis occurring in a liver with nonnecrotizing granulomas (stars) containing giant cell (arrow) and lacking a lymphocytic cuff. (D) PBC with granulomatous inflammation (red star) cuffing a bile duct (gold star) that also demonstrates lymphocytic infiltrate (arrows) of the bile duct epithelium.
Cholangitis
Cholangitis simply defined is inflammation of the bile ducts (Fig. 4). 8 , 9 Cholangitis could also be defined by its associated inflammation (i.e., neutrophilic, lymphocytic, or granulomatous). The term, when used by itself, most commonly is used with reference to neutrophilic cholangitis (bacterial infection or obstruction of the biliary system). Other associated findings, such as portal edema and ductular proliferation at the periphery of the portal tract, are often present. Lymphocytic cholangitis is most often seen in PBC andPrinciple Histologic Features and Associated Differential Diagnosis of Hepatitis and Cholangitis in acute cellular rejection. PBC may be purely lymphocytic or, as described earlier, may be associated with granulomas and usually affects small intrahepatic ducts. Lymphocytic or mononuclear cholangitis of large (hilar and extrahepatic) ducts is characteristic of primary sclerosing cholangitis. When the inflammation involves larger ducts and damage occurs, it will result in obstruction and infection, leading to neutrophilic cholangitis of the smaller ducts.
FIG 4.

Two examples of cholangitis are shown. (A) Acute or ascending bacterial cholangitis is present with a neutrophilic infiltrate seen with the bile duct (arrow). Associated ductular proliferation is also seen. (B) An example of cholangitis lenta (nonsuppurative cholangitis), ductular proliferation is present in the periphery of the portal tracts with bile plug (arrows). Note the lack of inflammatory infiltrate.
Nonsuppurative cholangitis, also known as cholangitis lenta, is a condition that is characterized by ductular proliferation with bile plugs seen within the ductules. The background liver is typically cholestatic, but the portal inflammation is usually lacking. This condition is seen in association with systemic or peritoneal infections, as well as other systemic conditions.
Potential conflict of interest: Nothing to report.
References
- 1. Denk H. What is expected from the pathologist in the diagnosis of viral hepatitis. Vichows Arch 2011;458:377‐392. [DOI] [PubMed] [Google Scholar]
- 2. Batts KP, Ludwig J. Chronic hepatitis: an update on terminology and reporting. Am J Surg Pathol 1995;19:1409‐1417. [DOI] [PubMed] [Google Scholar]
- 3. Bach N, Thung SN, Schaffner F. The histological features of chronic hepatitis C and autoimmune chronic hepatitis: a comparative analysis. Hepatology 1992;15:572‐577. [DOI] [PubMed] [Google Scholar]
- 4. Burt AD, Mutton A, Day CP. Diagnosis and interpretation of steatosis and steatohepatitis. Semin Diagn Pathol 1998;15:246‐258. [PubMed] [Google Scholar]
- 5. Brunt EM. Nonalcoholic steatohepatitis: pathologic features and differential diagnosis. Sem Diagn Pathol 2005;22:330‐338. [DOI] [PubMed] [Google Scholar]
- 6. Kleiner DE. Granulomas in the liver. Semin Diagn Pathol 2006;23:161‐169. [DOI] [PubMed] [Google Scholar]
- 7. Valla DC, Benhamou JP. Hepatic granulomas and hepatic sarcoidosis. Clin liver Dis 2000;4:269‐285. [DOI] [PubMed] [Google Scholar]
- 8. Gonzalez R. Large duct obstruction. PathologyOutlines.com website. Available at: http://www.pathologyoutlines.com/topic/liveracutelargeductob.html. Accessed June 13, 2020.
- 9. Lefkowitch JH. Bile ductular cholestasis: an ominous hispathologic sign related to sepsis and “cholangitis lenta”. Hum Pathol 1982;13:19‐24. [DOI] [PubMed] [Google Scholar]


