Acute post‐infectious cerebellar ataxia (APCA) is a relatively common cause of acute ataxia among children and usually follows viral or bacterial infections. Recently, various neurological manifestations of Coronavirus Disease‐2019 (COVID‐19) have been described in the literature. Here, we are reporting a pediatric case initially having classical symptoms of COVID‐19 and developed cerebellar ataxia post recovery.
Case Report
A 13‐year‐old child presented with high‐grade fever for 3 days associated with mild respiratory complaints, maintaining arterial oxygen saturation above 96%. His nasopharyngeal swab was positive for severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) done by reverse transcription polymerase chain reaction (RT‐ PCR) and chest X‐ray showed mild basal infiltrates in both lungs. He was managed with tablets paracetamol, vitamin C & E with fever subsiding within 4 days.
Recovery was uneventful over the next 10 days, after which he became less interactive and developed lethargy, headache, and vomiting. Other complaints included clumsiness in both hands causing difficulty while eating food, slurring of speech, and swaying side to side while walking, causing recurrent falls, and requiring ambulatory assistance. There was no history of behavioral changes apart from fatigue. On physical examination he was conscious, alert, oriented and vitals were stable. Central nervous examination revealed intact cognitive function and absence of meningeal signs, saccadic abnormalities, or anosmia. Cranial nerve, motor, and sensory examination was normal. Cerebellar examination showed mild nystagmus, dysarthria, impaired finger nose testing (Video 1, segment 1), dysdiadochokinesia (left > right) (Video 1, segment 2), and impaired tandem walk (Video 1, segment 3). Rest of the systemic examination was normal. There were no notable history and examination findings suggestive of Multisystem Inflammatory Syndrome in Children (MIS‐C) due to Covid‐19.
Video 1.
Segment 1: Showing impaired finger nose finger test, Segment 2: Showing dysdiadochokinesia (left>right), Segment 3: Showing impaired tandem gait.
Blood investigations including complete blood counts, liver and kidney function test were normal. Human Immunodeficiency Virus test was nonreactive. Serum antinuclear antibodies, antinuclear antibodies 3 profile, autoimmune encephalitis panel and thyroid function tests were negative. Repeat nasopharyngeal swab for SARS‐CoV‐2 was negative. His COVID total antibody (Chemiluminescence immunoassay technique) was 46 and IgG antibody was 4 (≥1: positive). Magnetic resonance imaging (MRI) brain was normal (Fig. 1). Cerebrospinal fluid examination (CSF) showed cell count 3/mm3 (lymphocytes count 100%), protein 20.9 mg/dl, glucose 62 mg/dl and negative for Ziehl‐Neelsen, India ink, and Gram stain. GeneXpert for tuberculosis, BIOFIRE FILMARRAY Panel for meningitis/encephalitis (Escherichia coli, Haemophilus influenzae, Neisseria meningitides, Listeria monocytogenes, Streptococcus agalactiae, Streptococcus pneumoniae, Cytomegalovirus, Enterovirus, Herpes Simplex Virus 1 & 2, Human Herpes Virus‐6, Varicella Zoster Virus, Cryptococcal neoformans/gattii) was negative. CSF for SARS‐CoV‐2 RNA was negative, but COVID total antibody was 40 and IgG antibody was 3 (≥1: positive).
FIG. 1.
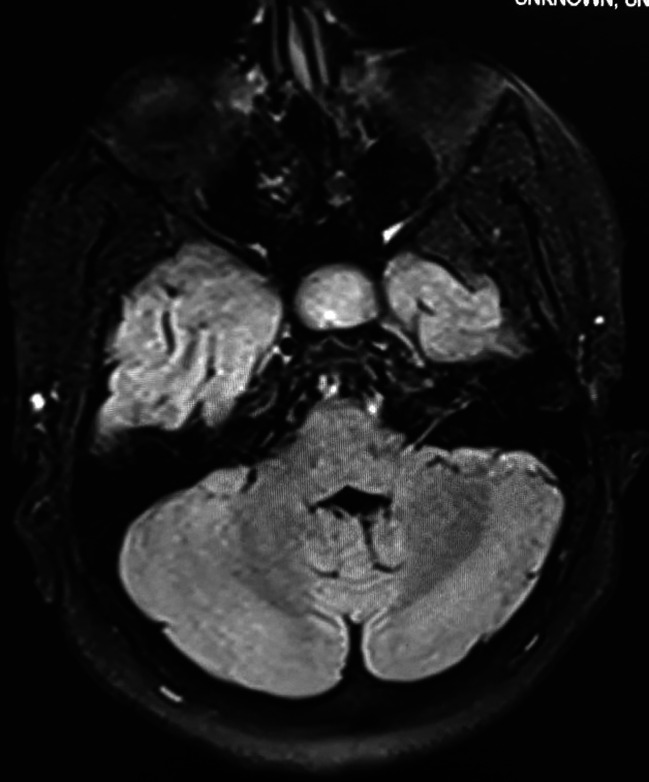
MRI brain T2 FLAIR axial sequence through level of cerebellum showing normal appearance of the cerebellum.
Diagnosis of APCA due to SARS‐CoV‐2 infection was made and pulse therapy of intravenous methylprednisolone 500 mg once daily for 5 days was instituted. The patient's condition improved rapidly, and he was able to ambulate independently after 20 days.
Discussion
Coronavirus Disease‐2019 (COVID‐19) is caused by the novel SARS‐CoV‐2. To date, approximately 83 million cases have been reported globally, accounting for nearly 2 million confirmed deaths. 1
Many neurological manifestations of COVID‐19 have been reported in the literature that range from mild non‐specific features such as headache, lethargy or confusion; isolated focal signs including hyposmia, focal seizures, eye‐movement abnormalities or ataxia; through to severe life‐threatening conditions including status epilepticus, Guillain Barre syndrome, disseminated stroke syndromes and acute haemorrhagic necrotizing encephalopathy. 2 , 3 In addition to these, a newly recognized Kawasaki syndrome‐like hyperinflammatory disorder has been recognized in children called as MIS‐C. This presents with fever, laboratory evidence of inflammation and multisystem (> = 2 organ) involvement, manifesting up to 3–4 weeks following a mild or asymptomatic COVID‐19 illness. 4
APCA in children develops a few days to weeks following viral illness but may follow bacterial infections and vaccinations. Currently, there are four previous reports of isolated cerebellar ataxia manifesting in adults following COVID‐19 infection. 5 , 6 , 7 , 8 In addition to these, Abdel‐Mannan et al., described 27 children with COVID‐19 associated with MIS‐C. In this group, four had new‐onset neurological symptoms, one of whom developed cerebellar ataxia. 9 Our case is the first to describe pediatric post‐infectious ataxia following COVID‐19 without features of MIS‐C, and provides supportive causal evidence with antibody positivity in both serum and CSF.
Neurological manifestations following COVID‐19 can be potentially grouped into three broad categories: direct neurotropic invasion, complications from systemic illness (eg, hyperinflammatory response, coagulopathy, metabolic derangement), or secondary autoimmune phenomena. The presence of angiotensin‐converting enzyme 2 (ACE) on neurons and glia in the hypothalamus, basal ganglia, midbrain, pons, medulla, and cerebellum acts as a possible entry mechanism for SARS‐CoV‐2 to enter directly neuronal cells. 10 Whilst this may represent one potential mechanism underpinning acute infectious cerebellar ataxia, the post infectious manifestations such as the ACPA seen in our patient, more likely represent an autoimmune phenomenon whereby COVID‐19 results in the production of autoantibodies that cross react with cerebellar epitopes. 11 , 12
Our patient developed typical COVID‐19 manifestations initially, followed by a 10‐day asymptomatic period after which he developed symptoms of cerebellar ataxia. Neuroimaging of patients with APCA may show hyperintensities of cerebellar gray matter on T2‐weighted MRI images and lumbar puncture may identify microbial infection and pleocytosis. However, a normal MRI and the absence of pleocytosis and virological markers in CSF do not exclude a post‐infectious autoimmune process. 11 APCA is often a clinical diagnosis, based on history of rapid onset of symptoms following a viral prodrome as well as exclusion of potentially more serious illnesses like toxic ingestions, meningoencephalitis, opsoclonus myoclonus syndrome, acute disseminated encephalomyelitis etc.
APCA generally responds to supportive care with some studies suggesting a beneficial effect of steroids, intravenous immunoglobulin, plasma exchange to counter the autoimmune process. Our patient showed an excellent response to intravenous methylprednisolone, with full recovery of function over 20 days.
While APCA is the most common cause of acute ataxia in children, it's association with the novel SARS‐CoV‐2 highlights the need for awareness of this possible complication in the pediatric age‐group among clinicians. The importance of ruling out more serious causes before reassuring family and initiation of supportive care needs to be emphasized.
Author Roles
(1) Research project: A. Conception, B. Organization, C. Execution; (2) Manuscript Preparation: A. Writing of the first draft, B. Review and Critique.
L.R.T.: 1 A, 1 B, 1C, 2A, 2B
D.J.S.: 2B
U.A.: 2B
A.B.: 1A, 1B, 1C
I.A.: 1A, 1B, 1C
Disclosure
Ethical Compliance Statement: The authors confirm that the approval of an institutional review board was not required for this work. We also confirm that the patient has given written informed consent for the publication of his video. We confirm that we have read the Journal's position on issues involved in the ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflict of Interest: No specific funding was received for this work. The authors declare that there are no conflicts of interest relevant to this work.
Financial Disclosures for the previous 12 months: The authors declare that there are no additional disclosures to report.
References
- 1. WHO Coronavirus Disease (COVID‐19) Dashboard. https://covid19.who.int/. Accessed January 3, 2021.
- 2. Ahmad I, Rathore FA. Neurological manifestations and complications of COVID‐19: a literature review. J Clin Neurosci 2020;77:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stafstrom CE, Jantzie LL. COVID‐19: neurological considerations in neonates and children. Children (Basel) 2020;7:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nakra NA, Blumberg DA, Herrera‐Guerra A, Lakshminrusimha S. Multi‐system inflammatory syndrome in children (MIS‐C) following SARS‐CoV‐2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management. Children (Basel) 2020;7:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mukherjee D, Sarkar P, Dubey S, Ray BK, Pandit A, Lahiri D. Ataxia as a presenting manifestation of COVID‐19: Report of a single case. medRxiv 2020.05.24.20103648; doi: 10.1101/2020.05.24.20103648 [DOI]
- 6. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China JAMA Neurol 2020;77:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Povlow A, Auerbach AJ. Acute cerebellar Ataxia in COVID‐19 infection: a case report. J Emerg Med 2020;60:73–76. 10.1016/j.jemermed.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dijkstra F, Van den Bossche T, Willekens B, Cras P, Crosiers D. Myoclonus and cerebellar ataxia following coronavirus disease 2019 (COVID‐19). Mov Disord Clin Pract 2020;7:974–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abdel‐Mannan O, Eyre M, Löbel U, et al. Neurologic and radiographic findings associated with COVID‐19 infection in children. JAMA Neurol 2020;77:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. MacGregor DP, Murone C, Song K, Allen AM, Paxinos G, Mendelsohn FA. Angiotensin II receptor subtypes in the human central nervous system. Brain Res 1995;675:231–240. [DOI] [PubMed] [Google Scholar]
- 11. Blumkin L, Pranzatelli MR. Acquired ataxias, infectious and Para‐infectious. Handb Clin Neurol 2012;103:137–146. [DOI] [PubMed] [Google Scholar]
- 12. Uchibori A, Sakuta M, Kusunoki S, Chiba A. Autoantibodies in postinfectious acute cerebellar ataxia. Neurology 2005;65:1114–1116. [DOI] [PubMed] [Google Scholar]


