Abstract
Infectious cutaneous diseases are very common, especially in certain geographic and tropical regions. Sometimes they may simulate other dermatoses, ordering verification of diagnosis with particular investigations. Dermoscopy is among one of the most important tools readily available in the outpatient setting for the dermatologist to confirm the diagnosis. In this up-to date review, literature concerning the various dermoscopic features of parasitic, viral, dermatophytic and bacterial cutaneous infections is composed. In addition artefacts as well as practical issues in dermoscopy usage are discussed; with the aim to empower dermatologists to promptly and non-invasively diagnose and manage cutaneous infections and infestations.
Keywords: Cutaneous infections, demodex, dermatophyte, dermatoscopy, dermoscopy, entodermoscopy, infestations, mite, molluscum, pediculosis, scabies, tinea, warts
Introduction
Cutaneous infections and infestations are ubiquitous; although some of them demonstrate relative geographic predominance. While the clinical diagnosis of disorders of this category is usually easy, owing to the frequent presentation of the disorder with characteristic lesion(s) with pathognomonic morphology (such as verrucous lesions of common warts, umbilicated papules of molluscum, scaly annular lesions of dermatophytic infection, etc.), occasionally they may simulate other dermatoses, mandating confirmation of diagnosis with specific laboratory investigations including but not limited to microbiological, pathological, serological, and radiological investigations. For example, the flat mildly pigmented lesions of verruca plana may be confused with lichen planus, lichen nitidus, and evolving lesions of seborrheic keratosis; or disseminated annular lesions of steroid-modified tinea corporis may simulate annular psoriasis, granuloma annulare, borderline leprosy, petaloid variant of seborrheic dermatitis, pityriasis rosea, or annular polycyclic variant of subacute cutaneous lupus erythematosus (SCLE). The shortcomings of laboratory investigations [Table 1], especially the delay in availability of results, need for infrastructure and trained personnel, and patient's refusal to undergo invasive investigations like skin biopsy often poses a practical dilemma for the treating specialist, particularly in a resource-constrained healthcare set-up.
Table 1.
Relative limitations of conventional approach to cutaneous diagnosis employing standard* tests and investigations versus the potential of dermoscopy
| Investigation-dependent | Investigator-dependent |
|---|---|
| Typically invasive (skin biopsy) to semi-invasive (e.g., slit skin smears) | Level of training, especially regarding the perfect site for taking the specimen |
| Relative non-compliance of patients to undergo an invasive procedure. Typically difficult in children | Counseling skills of the dermatosurgeon, and skill to produce a scar-less biopsy. Interpretation skill of the Dermatopathologist and Clinical microbiologist |
| Unlike dermoscopy that can provide in-vivo diagnostic clues, the conventional investigations like skin biopsy provide results available from the investigation done in-vitro | The sectioning and slide preparation depend on the skill(s) of the pathologist and technical staff. False negatives may occur if the section examined is relatively peripheral from the main pathology in the specimen |
| Unlike dermoscopy, where the region of suspicion may be repeatedly, and non-invasively evaluated a few number of times as per patient comfort; in case of a non-committal false-negative dermatopathology report, the wrong site and/ or wrong sectioning are responsible. Repeating another biopsy is often fraught with strong patient non-compliance | Same as Above |
| Possibility of local anesthesia-associated rare, but known adverse effects; especially hypersensitivity | Need for an emergency resuscitation kit in the event of a rare anaphylactic reaction to the local anesthetic agent |
| Overall, more time-consuming (results of histopathology and cultures take a week or more) | Skills and efficiency of the pathology/microbiology unit and the reporting specialist |
| Storage of images is tedious, requires specialized equipment, and not feasible for large number of cases | Skills and efficiency of the pathology/microbiology unit and the reporting specialist; willingness to use special equipment for photomicrography to provide images for records |
| Cumbersome with need for specialized infrastructure | Interdepartmental coordination (dermatology, pathology, microbiology) essential for clinicopathological correlation (CPC) or clinicomicrobiological correlation (CMC) for final diagnosis |
| Overall, costlier to the patient | The cost depends on the kind of health-care set-up |
*Skin biopsy and dermatopathology, skin smears for microbiological investigations including wet smears, KOH-based smears, regular and special stains, microbial cultures etc
Dermoscopy, or dermatoscopy, a non-invasive technique, is not a “new” diagnostic modality in cutaneous medicine. The technology that has served for years, and continues to serve the specialized area of cutaneous oncology in the evaluation of the malignant potential of melanocytic lesions typically in susceptible individuals, i.e., those with the lighter skin photo types (SPT I-II), has seen a rapid upsurge in the past decade in the exploration of its diagnostic and extradiagnostic uses in disorders of general dermatology and those involving cutaneous appendages.[1,2,3,4] Its utility has expanded both in terms of the clinicopathological subtypes of dermatoses as well as the diverse ethnicities with different SPTs. Entodermoscopy, a neologism proposed first by Scanni and Bonifazi in 2006 for the dermoscopic diagnosis of ectoparasitosis,[5] was subsequently extended to include superficial skin infections by Zalaudek et al.[6] Ever since, only countable number of review articles have been published on this expanding and niche' topic. Incidentally, majority of their contents focus on the cutaneous infections and infestations in people with lighter SPTs.[4,6,7,8,9] Additionally, anecdotal reports and tiny case series focusing on one particular cutaneous infection/infestation have been published, most of them once again in people with lighter SPTs.[10,11,12,13,14]
This narrative review is different in certain ways. First, it addresses the conditions that are clearly more relevant to population dwelling in South Asia and related developing nations such as Hansen's disease, complicated dermatophytic infections, and scabies among others. Second, it attempts to highlight the subtle differences in the dermoscopic features of the same condition in skin of different ethnic origin, a fact that has been reiterated on several occasions.[15,16,17] Lastly, it dwells on the extra-diagnostic uses of entodermoscopy. However, at the very outset, it must be emphasized that the current evidence on dermoscopic diagnosis of various cutaneous disorders including infections and infestations is not as robust as that of conventional investigations and there are many other factors that limit the utility of dermoscopy for its conventional indication as well as in disorders of general dermatology;[4,6,18] a detailed discussion on which is beyond the scope of this review.
The Mechanism of Dermoscopy—A Quick Revisit
The basic principle of dermoscopy is transillumination of a skin lesion and employing higher magnification to visualize subtle features. The physical properties of the skin influence the fate of light incident on its surface; reflection, refraction, diffraction, and/or absorption [Figure 1a].[3] While a major portion of the light incident on a dry, scaly skin gets reflected, most of the light striking a smooth, oily skin passes through it, reaching the deeper dermis. With the use of a linkage/immersion fluid (such as mineral oil) on the skin, or use of inbuilt crossed-polarizers in the device (that filter out the peripheral scattered light), the translucency of the skin is enhanced, with improved visualization of the substratal structures [Figure 1b]. The two broad categories of dermatoscopes consist of the hand-held dermoscopes (HHD), also referred to as smart dermoscopes, and the videodermoscopes (VD); the latter provide higher magnification as well as evaluation without the need of a contact fluid through its cross-polarizing filters. Practically, most of the newer and evolving dermoscopes are hybrid versions incorporating the best properties of both.
Figure 1.
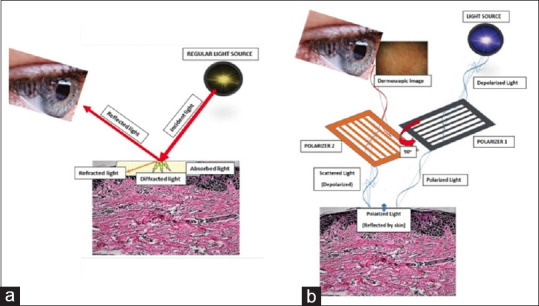
(a) When light is incident on the skin (thick red arrow), it gets reflected back (thin red arrow), while the remaining gets refracted (oblique orange arrow), diffracted (yellow shooting arrows) or absorbed (crimson area). On looking directly at the skin by unassisted eyes, one sees the external image of the skin formed by the reflected light; (b) Working principle of a modern dermoscope. In the polarized mode, the light gets polarized by two cross-polarizers, cutting out the scattered light reflected from the skin, allowing image formation with visualization of substratal structures
There is profound evidence that dermoscopy is a valuable addition to the available tools for the diagnosis of skin infections and infestations. In the ensuing discussion in this narrative review article, we shall dwell upon both the characterizing features (and 'diagnostic clues' of such conditions on dermoscopy, with special emphasis of infections and infestations more pertinent to the developing world as well as touch upon the versatility of dermoscopy in these situations beyond diagnosis. This article summarizes the available extant published literature as well as includes the contributions of the authors.
Prevention of dermoscopy-associated cross-infection
Before we embark upon the role of entodermoscopy, it is paramount to understand the concept of dermoscope-associated cross-infection when the same device is used different patients. As a non-invasive technique, dermoscopy is essentially free of complications. The only issue is the rare but definitive possibility of cross-infection between patients, especially with contact dermoscopy. Dominique et al. reported the contamination of the dermoscopic lens by human papillomavirus (HPV) to be more common than presumed.[19] Their observation revealed that wart-specific HPV DNA is detected with a high frequency (>40%) on a dermoscopic lens before examination and that the detection rate is increased to >75%. In other studies undertaken to review the role of dermatoscopes as vectors for nosocomial infection, confirmed the preventive role of using disposable lens covers, and 70% isopropyl alcohol (both as a contact fluid and as a post-procedure disinfectant) against bacteria including methicillin-resistant S. aureus (MRSA).[20] And while use of disposable covers over the dermatoscope lens, and disinfecting the device with isopropyl alcohol 70% in-between the patients constitute the cornerstone of prevention of cross-infection via dermatoscope,[20,21] many other innovative strategies[3] are being devised. In our personal opinion, however, the assertion about the “dermoscopy-induced COVID-19 spread' in the current pandemic, is not only unfounded and overhyped, but the corresponding suggestions recommended to 'pre-empt the risk” are equally irrational and contradictory.[22,23]
Parasitic Infestations
Pediculosis
Pediculosis capitis and phthiriasis pubis, caused by Pediculus humanus var capitis (head louse), and Pthirus pubis (crab louse) respectively are ectoparasites that cause thousands of infestations worldwide annually. Diagnosis is clinically suspected on patients complaining of severe pruritus, more at the occipital and retro-auricular areas of the scalp, in combination with close examination of the scalp hair for the presence of lice or nits.
Dermoscopic or trichoscopic features that hint towards a strong possibility of pediculosis capitis include focal erythema, erosions and crusting, and sometimes blue-grey macules suggestive of the louse-bite (macula cerulea) suggestive of scalp inflammation (vide infra). Dermoscopy allows a rapid diagnosis of these infestations by permitting the identification of either the nits fixed to the hair shaft in their different stages of maturation/degeneration (more common) [Figure 2a] or rarely, the motile lice/nymphs (owing to the prompt movement of the louse away from light source).[16] Three different stages of the nits [Figure 2b-d] can be easily identified on high magnification in vivo dermoscopy[4,5,6,7,8,9,14,16,24,25,26] – (1) Active viable nits - ovoid, whitish-brown structures (containing eggs/viable embryo) with tense convex walls and an intact closed operculum. They are adherent to the hair shaft and found closest to the scalp surface; (2) Abortive nits – ovoid, relatively translucent, which contain a condensed nonviable embryo surrounded with air spaces with a dehiscing operculum. These may form spontaneously or form the intermediate stage between the active and empty nit following effective pediculocidal treatment; usually found 5 mm or farther away from scalp skin; and (3) Empty nits – translucent whitish crystalline structure that represents the remaining involucrum devoid of operculum (with a plane and a free ending) following the discharge of the embryo (viable or non-viable). They are localized farthest from the scalp— typically more than 1 cm away. It has been reported that the internal nit structure is better visualized at high-magnification polarized mode, typically using a videodermoscope.[25,26]
Figure 2.
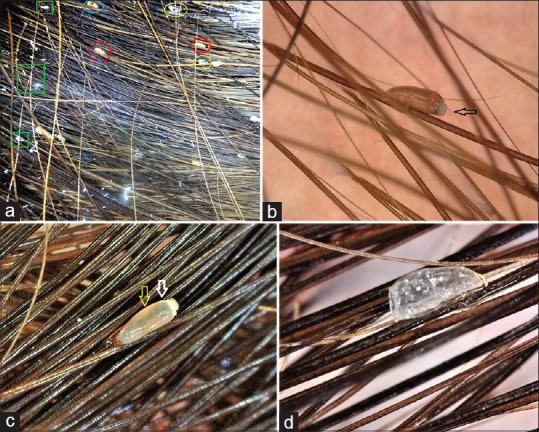
(a) In-vivo appearance of pediculosis capitis with nits in different stages of maturation/degeneration – active/viable (red circled) containing eggs closed with a tough porous operculum, non-viable nit with dead nymph or post-hatching of the nymph, with open operculum (light-blue circled), and empty nit with only air filled shell (yellow circled). Also appreciate 'pseudonits' most commonly seen as dandruff flakes (inside green rectangles), which are of bizarre-shape, and non-adherent to the hair shafts unlike the nits. [Heine Delta Dermoscope, non-polarizing, 20×]. (b) In-vivo high-magnification polarized videotrichoscopic images displaying nits in different stages of maturation/degeneration - (b) Active viable nit- ovoid brown colored structure containing viable embryo with intact operculum (black arrow).(c) Abortive Nit: translucent whitish-brown showing condensed non-viable embryo (yellow arrow) with surrounding air (white arrow). (d) Empty Nit: translucent crystalline-whitish colored open-ended nit without operculum after the discharge of the nymph or abortive embryo. [Dinolite premier AM4113 ZT videodermoscope, Taiwan, polarized, 80×]
Compared to adult lice or nymphs of pediculosis capitis [Figure 3a], in phthiriasis pubis, the smaller body (1.2 x 0.8 mm), lighter color, and less mobility of the parasite renders its visualization by the unaided eye more difficult. Dermoscopy displays the “miniature-crab”-like light greyish-brown louse with six legs, clutching onto the pubic hair shafts with its foreleg-claws[10,11,16,27,28] [Figure 3b]. However, the detection of nits remains the cornerstone of dermoscopic diagnosis of pubic louse.
Figure 3.
Dermoscopic images of adult lice infesting humans: (a) Ex-vivo trichovideoscopic appearance of multiple mature head lice isolated from the patient's scalp that had heavy infestation. A maturing nymph can be seen (red arrow), which is relatively translucent compared to mature lice [Escope videodermoscope, polarized, 10×]. (b) Pubic region of an adult Indian patient showing a 'miniature-crab'-like light greyish-brown louse with six legs, clutching onto the firmly grasped pubic hair shafts with its foreleg-claws. [Escope videodermoscope, polarized, 10×]
Pediculus humanus var. corporis (body louse) is morphologically nearly identical to the head louse. It must be noted that except for the attachment site of the nits (base of the hair in head and pubic lice versus fabric seams in body louse), there is no documented difference in the morphology of nits of the three types of lice.[16,27]
It is important to distinguish any nits from “pseudo-nits”, which can arise from dandruff flakes, hair casts, hair spray or gel residues etc.[29] Unlike nits, the pseudo-nits appear as bizarre-shaped amorphous white structures that are not attached to the hair shaft. Other dermoscopic simulants of nits that may need to be ruled out include the whitish, ovular masses along the hair shafts of white piedra involving the scalp or the pubic region (trichomycosis pubis), or trichorrhexis nodosa (broken hair shafts with a brushed tip).
In case of phthiriasis palpebrarum, lice are sometimes clinically difficult to identify, so the infestation may be misdiagnosed as scales of atopic or seborrheic dermatitis. In these cases, dermoscopy can be of great diagnostic help by revealing the presence of lice and/or nits.[30]
Apart from diagnosis of louse infestation, dermoscopy also aids the clinician to assess the treatment efficacy, corroborate treatment compliance, and to screen household contacts with asymptomatic infestations. Moreover, it also serves as a useful tool for evaluating the efficacy of different pediculocidal topical products through ex vivo evaluation of the movements and physiology of the mite.[25,31]
It is noteworthy, that in contrast to dermoscopy of lice infestation in people with lighter SPTs, appreciation of surrounding erythema, as well as macula cerulae is difficult in dark-skinned individuals.[16,27]
Scabies
Scabies, caused by the mite Sarcoptes scabiei has been identified as a neglected tropical disease responsible for an underestimated and inaccurately quantified level of morbidity and global burden of disease. The diagnosis of scabies is usually made clinically in patients with a highly pruritic papulo-vesicular rash, with characteristic curvilinear burrows and associated secondary lesions visible at sites of predilection, reinforced with a concurrent/recent positive history of similar affection in a household contact. Conventionally, the clinical suspicion of scabies has been confirmed by ex vivo identification of the mite, its eggs, or fecal pellets in skin scrapings seen under light microscopy, a time-consuming procedure with poor patient enthusiasm.
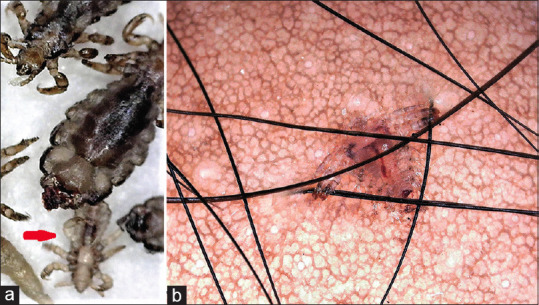
The introduction of both HHD and high-magnification polarized VD has facilitated a much quicker non-invasive in-vivo diagnosis. Various eponymous dermoscopic signs representing different parts of the mite, and the burrow have been described in literature considered pathognomonic of scabies.[6,7,8,9,12,32,33] Small dark brown triangular structures located at the end of whitish structureless, curved or wavy lines, simulating the appearance of 'circumflex accent' (^), popularly known as delta-wing jet with contrail, also called the 'triangle sign' remains one of the oldest described dermoscopic appearance of the burrow with a mite in vivo. Microscopically, the pigmented anterior part of the mite (mouth parts and the two anterior pairs of legs) contributes to the appearance of the brown-colored triangular structure that resembles a delta-glider [another synonym: delta glider sign] triangle, whereas the posterior part composed of translucent abdomen and hind legs evades dermoscopic appreciation. The contrail feature seen on dermoscopy corresponds to the burrow of the mite with some external features and some intrinsic structures. The convoluted burrow (“S” or “Z” shaped, or bizarrely-shaped) is typically scaly, covered with focal whitish-yellow scales, and shows multiple small brown dots within its contents, correlating with the mite's fecal pellets.[16] This trailing burrow follows behind the anterior dark brown triangular structure representing the pigmented anterior part of the mite that looks like a delta-glider in front.
The above features may be detected by an experienced dermoscopist even at a low magnification of 10-20× of a smart HHD [Figure 4a]; visibility of which may be improved by using the digital zoom of the image capturing device, albeit at the cost of compromised resolution [Figure 4b]. However, the dermoscopic morphology of the delta-wing jet with contrail sign is best appreciated at higher optical magnification of 50-150×, using a VD in polarized mode [Figure 5a and b]. It is important to mention that non-specific pigmented structureless areas are often seen surrounding the burrow in scabetic patients who are dark-skinned, owing to the evolving or rapidly settling post-inflammatory hyperpigmentation (PIH)[16] as seen in Figure 5b.
Figure 4.
(a) Low magnification (20×) polarized image of a scabetic burrow from the wrist of a young Indian lady showing a broad view of the delta wing with jet contrail sign. (b) Higher digital magnification (40×) polarized view showing the brown-colored triangular structure (enclosed within the black triangle) that resembles a delta-glider (inset), trailed by the jet contrail (confined by yellow lines). The jet contrail represents the burrow, and often shows whitish-yellow scales, and pigmented dark-brown colored granules and globules suggestive of the fecal pellets (light blue stars) [Heine Delta Dermoscope, polarized, non-contact
Figure 5.
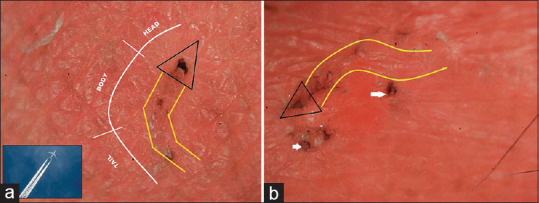
Higher magnification polarized videodermoscopy of scabetic burrows from two Indian children: (a) Appreciate the components of the delta wing jet contrail sign. A schematic diagram of 'jet contrail' can be seen in the inset for morphological comparison. Also appreciate the head, body, tail components of the new anatomo-functional concept called the Mite-Gallery Unit (MGU) proposed to broaden the concept that would consider different albeit related dermoscopic features as additional potential dermocopic clues for diagnosis of scabies with/without the classical clues. (b) In this image that also shows the typical sign as seen in (a), one can also observe the presence of few discreet pigmented structureless areas (white arrows) in the surrounding of the burrow, which is more commonly encountered in scabies patients who are dark-skinned, suggesting simultaneous and/or early development of post-inflammatory hyperpigmentation. [Escope videodermoscope, polarized, non-contact, 80×]
High sensitivity (ranging from 83% to 91%) and acceptable specificities (ranging from 46% to 86%) have been reported for dermoscopic diagnosis of scabies in two large trials comparing the same with conventional methods including microscopic examination of skin smears and the adhesive tape test.[33,34] While the first study confirmed the non-inferiority of standard HHD to microscopic examination, it also showed that the dermoscopic sensitivities were similar for the expert and inexperienced dermoscopists, with enhanced diagnostic accuracy by the dermoscopists with experience.[33] The second study bears special relevance to the resource-constrained developing countries, with suggestion that dermoscopy is a valid tool for diagnosing scabies in such a setting.[34]
Since the abdomen and eggs of mites are transparent, they are hardly visible to dermoscopy, hence, demoscopy can be combined with ink staining to enhance the yield of mites to evaluate and monitor the progression of scabies.[35]
The diagnosis of scabies using optical microscopy until recently has always involved demonstrating the mite and its products outside the human body (on a glass slide) without taking into account exactly what happens within the epidermis. The systematic use of dermoscopy has recently highlighted the morphological complexity of the Sarcoptes tunnel. Previously considered a simple unitary structure, latest insights suggest three separate segments of the burrow conforming to a new anatomo-functional concept called the Mite-Gallery Unit (MGU), composed of three parts, the Head, Body, and Tail. The Mite-Gallery Unit provides a new anatomical and functional explanation of scabies because it provides a more comprehensive in vivo and in situ dermatoscopic diagnosis.[12] This approach, based on the life cycle of the mite and its association with the host's local skin turnover has allowed us to recognize not only Sarcoptes using the gallery, but contributed to novel descriptors including tunnels without Sarcoptes, those with acari alone, and those with associated signs of inflammation.
Recently, the dermoscopic appearance of canine scabies in humans was reported to lack any burrows; rather characterized by presence of curvilinear crusts on most of the papules possibly representing a special pattern of excoriations resulting from tearing of superficially dug tunnels with residual vacant curved linear remnants.[36]
Cutaneous demodicidiosis
Demodex folliculorum is a commensal mite that inhabits the human facial skin; however a heavy infestation by the mite and/or abnormal host inflammatory response is known to cause specific mite-associated dermatoses. Pending confirmation of the exact pathogenic role of human Demodex mites in inflammatory disorders of the facial skin, a higher prevalence of mites has been reported in rosacea, seborrhoeic dermatitis, perioral dermatitis, and blepharitis.[37] The recent recognition of primary demodicidiosis as a primary disease sui generis has been furthered with a working classification based on clinical manifestations into[38] (a) spinulate demodicidiosis (pityriasis folliculorum), involving sebaceous hair follicles without visible inflammation; (b) papulopustular/nodulocystic or conglobate demodicidiosis with pronounced inflammation affecting most commonly the perioral and periorbital areas of the face; (c) ocular demodicidosis, inducing chronic blepharitis, chalazia or, less commonly, keratoconjunctivitis; and (d) auricular demodicidosis causing external otitis or myringitis. Secondary demodicidiosis is usually associated with systemic or local immunosuppression, especially abuse of topical corticosteroids (TCS). Other inflammatory variants include demodex dermatitis, rosacea-like demodicidiosis (RLD) [Figure 6a], pustular folliculitis, among others. Seborrheic dermatitis and different variants of rosacea constitute the most important differentials of primary demodicidiosis.
Figure 6.
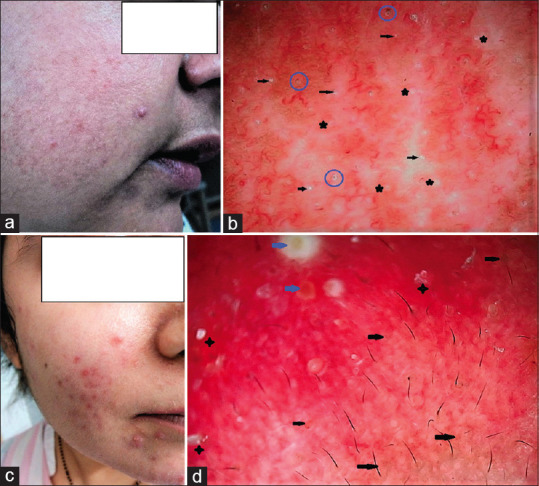
Clinicodermoscopic differentiation of Rosacea-like demodiciodosis (RLD) from papulopustular rosacea: (a) Clinical mage of the muzzle area of the face of a middle-aged lady with intolerance to photoexposure, off- and on itchy and scaly papular eruption over the muzzle area diagnosed with RLD. (b) Dermoscopy from the cheek revealed pinkish red background, with multiple demodex tails (black arrows), and demodex follicular openings (black asterisks). The blue circles have been drawn to surround comedones. Additionally, horizontally-to-haphazardly oriented reticular red dilated blood vessels can be seen, tending to form vascular polygons at places. But other features such as additional scale-crusts, follicular pustules are absent. (c) Facial image of a young lady suffering from chronic papulopustular rosacea with break through lesions. (d) Dermoscopy of the patient's cheek reveals dense erythema in the background, linear vessels characteristically arranged in a polygonal network (vascular polygons) follicular plugs, whitish-yellowish scales (black stars), orange-yellowish areas, pigmentation structures (black arrows), dilated follicles and follicular pustules (blue arrows), clues almost confirmatory of papulopustular rosacea [Escope videodermoscope, polarized, non-contact, 50×]
Conventional methods for the examination and quantification of human Demodex mites include the cellophane tape method (CTP), squeezing method, skin scrapings, Standardized Skin Surface Biopsy (SSSB), and rarely a skin punch biopsy.[37] Of these SSSB remains the most commonly used approach to compare densities of mites between patients with mite-associated dermatoses and healthy controls; >5 mites per cm2 is considered a positive diagnosis of demodicidiosis. However, of the several limitations of this method, the arbitrary choice of this threshold and weak evidence constitute the major deterrents. Thus, qualitative and semi-quantitative dermoscopic features have been suggested and being evolved for hopefully, a more sensitive and specific diagnosis of cutaneous demodicidiosis and its differentiation from conditions simulating or significantly overlapping with this diagnosis.[39]
The dermoscopic hallmarks of all clinical subtypes of demodicidosis include two specific and few non-specific features. The most specific clues include the “Demodex tails,” which look like whitish creamy gelatinous threads, 1–3 mm in length [Figure 6a], result from the presence of follicular inhabitation with a mixture of keratotic material and mites, and are most commonly seen in spinulosis of the face or pityriasis folliculorum-variant. The other specific clue refers to “Demodex follicular openings,” which represent the dilated follicular openings containing round, amorphous grayish/light brown plugs surrounded by an erythematous halo. Horizontally positioned reticular red dilated blood vessels constitute the third common but non-specific dermoscopic finding, which is observed more often in inflammatory variants such as demodex dermatitis and RLDs [Figure 6b].[39,40] Additional non-specific dermoscopic features such as diffuse erythema, scaling, and pustules are present in variable amounts according to the subtype of demodicidiosis.
The “demodex tails” should be distinguished from other scales (more irregular and whiter) and beard hair (regular in size, shape and diameter). Similarly, demodex follicular openings' need to be differentiated from open comedones (more uniformly distributed, darker in colour with a delicate hyperpigmented ring). Dermoscopy can also aid in the detection and quantification of demodex mites per follicle per evaluated area, and also useful for demonstration of early response to anti-mite therapy.
It is possible to dermoscopically differentiate demodex disorders from their main differential diagnosis like seborrheic dermatitis (comprises of dotted vessels in a patchy distribution and fine yellowish scales), erythematotelangiectatic rosacea (shows linear vessels arranged in a polygonal network) and papulopustular rosacea [Figure 6c and d] (shows linear vessels arranged in a polygonal network along with follicular pustules).[40] In the context of South Asia and neighbouring developing countries, where the facial abuse of TCS owing to their over-the-counter-availability is very common, topical steroid-damaged face (TSDF) must be considered as an additional differential of cutaneous demodicidiosis. Dermoscopically, this condition is characterized by multiple tortuous and branching linear vessels over a pinkish-red background with ivory white-to-strawberry ice cream colored patches (suggestive of cutaneous atrophy) in addition to conspicuous hypertrichosis.[41]
Cutaneous larva migrans
Cutaneous larva migrans (CLM), or “creeping eruption” represents a parasitic infestation commonly encountered in tropics and subtropics, most commonly caused by larva of Ancylostoma brasiliense and Ancylostoma caninum.
Minor skin abrasions are the commonest portals of entry into the human cutis, followed by the larvae burrowing intraepidermally. Lesions are typically raised, very itchy, skin-to-tan-to-reddish in color, and form linear, curvilinear, serpentine, and bizzare patterns both discreetly as well as in clusters., with the dorsum of feet and buttocks being the most common sites of involvement [Figure 7a].[42] Dermoscopic examination reportedly reveals translucent brownish structureless areas in a segmental arrangement, corresponding to the larva body. Moreover, red dotted vessels that correspond with the empty burrow have also been reported.[43] On high magnification polarized VD, we observed reddish-brown streaky thick lines (linear & curvilinear) and structureless areas in a segmental pattern representing burrows with larva, with red dotted vessels seen scattered around these structures in the empty burrows. Additionally, the presence of focally present bizarre pigmented structures around the main lesion may be seen, especially in dark-skinned individuals [Figure 7b].
Figure 7.
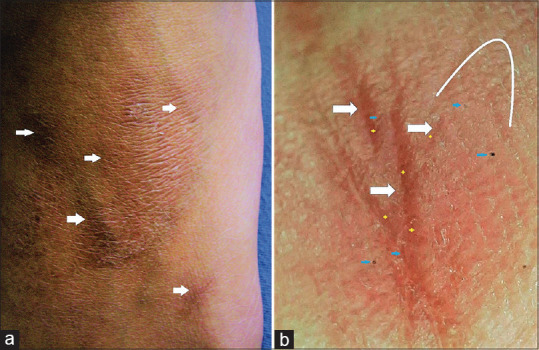
Cutaneous Larva Migrans (CLM) involving the dorsum of one foot in an adult Indian man: (a) Clinical image showing the burrows as raised, skin-to-tan- coloured discreet-to-coalescing linear, and curvilinear lesions (white arrows) with focal erythema and mild scaling. (b) Dermoscopy of the CLM lesions showing reddish-brown streaky thick lines (linear & curvilinear) and structureless areas in a segmental pattern (white arrows & arc) representing burrows with larva, and multiple red dotted-to-curved vessels (yellow crosses) scattered around these structures, i.e., remnants in the empty burrows. Additionally note the presence of focally present bizarre pigmented structures (light blue arrows) typical of darker skin types. [Escope videodermoscope, polarized, non-contact, 80×]
Bed bugs
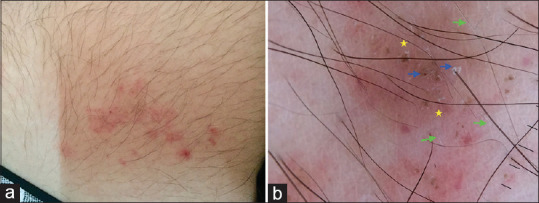
Cimex lectularius commonly known as bed bugs are blood-feeding insects (Order: Hemiptera) around 5-mm in-size that feed on mammalian hosts, including humans. Although visible withy naked eyes, their nocturnal feeding habits, and strong aversion to light render their direct detection nearly impossible. Bed bugs are typically acquired by hosts staying in different hotel rooms with compromised bed hygiene, and their infestation of the host's personal bedding often leads to persistent and recurrent bites. Bed bug bites present as pruritic maculopapules with central haemorrhagic punctum, and targetoid lesions resembling erythema multiforme [Figure 8a]. Dermoscopic findings reported mention the presence of haemorrhagic clod(s) (bite spot) and telangiectasias.[44] Figure 8b demonstrates high-magnification polarized VD image of a tiny region showing multiple bites suggestive of bed bugs; characteristics being similar to those reported till now,[44] i.e., closely placed multiple hemorrhagic clods, interspersed with telangiectasias over a pinkish background.
Figure 8.
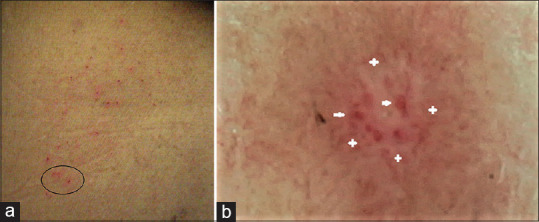
Bed Bug bites in a frequently travelling Indian businessman: (a) Clinical image showing multiple discreetly scattered maculopapules with central haemorrhagic punctum, and erythema-multiforme-like targetoid lesions over the back. (b) Dermoscopic observation (from the black circled region of image (a)) showing multiple haemorrhagic clodS (white arrows) signifying bite spots, and interspersed telangiectasias (white-colored + symbols) over a pinkish-background [Escope videodermoscope, polarized, non-contact, 150×]
Cydnidae pigmentation
Burrowing bugs, are in general considered harmless to humans. Recently, asymptomatic transient non-inflammatory hyperpigmentation caused by the bug Chilocoris spp (family, Cydnidae; order, Hemiptera; suborder, Heteroptera; superfamily, Pentatomoidea) has been reported.[45] These tiny insects proliferate in vegetation-rich areas and adjoining human dwellings especially during the monsoon season. Although essentially harmless to humans, their odorous secretions may stain the human skin, producing oval-to-lanceolate to bizarre-shaped pigmented macules [Figure 9a] that typically show self-resolution within a week and may be wiped out with acetone.[45,46] However, the abrupt appearance of asymptomatic pigmented macules with clustering typically seen in families and people staying in crowded dwellings can be perplexing and may be a source of anxiety for both the patient and the physician. The author(s) of this review were the first to report the dermoscopic appearance of this condition that includes the presence of cluster of numerous oval to shiny brown globules, granules, and bizarre-shaped pigmented structures that demonstrate a superficial “stuck-on” appearance.[46] Additionally, a recent report suggests that the pigmentation is accentuated along the skin furrows and around the eccrine openings [Figure 9b][47]; a logical outcome of the insect's secretions accumulating along the creases and periappendageal openings. The 'acetone test' is sufficient to rule out cydnidae pigmentation from other disorders of hyperpigmentation, especially idiopathic eruptive macular pigmentation (IEMP).[46]
Figure 9.
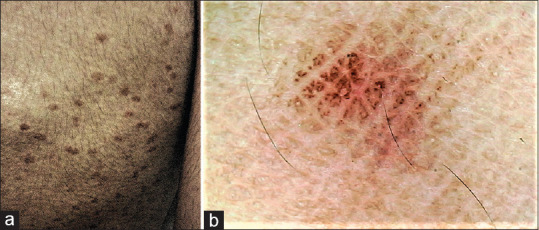
Burrowing bug (Cydnidae) pigmentation: (a) Clinical image showing oval-to-lanceolate to bizarre-shaped pigmented macules scattered over the trunk and limbs of the affected adult. (b) Dermoscopy showing of cluster of numerous oval to shiny brown globules, granules, and bizarre-shaped pigmented structures that demonstrate a superficial “stuck-on” appearance and accentuation along the skin furrows and around the eccrine openings [Escope videodermoscope, polarized, non-contact, 80×]
Cutaneous myiasis
Myiasis is an infestation of the skin caused by the larval stage of different botflies, of the order Diptera, family Calliphoridae (Dermatobia hominis in the Americas, Chrysomya bezziana in the Indian subcontinent; others being Cochliomyia hominivorax, and Cordylobia anthropophaga among others). It occurs due to the larval infestation (maggots) of fly species within the arthropod order that feed on the host's dead or living tissue, body substances, or ingested food. Of the three major clinical types of cutaneous myiasis, furuncular is the most common [Figure 10a],[48] followed by wound myiasis and migratory/creeping variant. Dermoscopy descriptions of furuncular myiasis reported in the literature include a central opening, surrounded by dilated blood vessels, containing a yellowish structure with black spines. Also reported were structures described as 'bird's feet'-like, corresponding to respiratory spiracles and 'thorn-crown'-like due to black dots on the outer edge of the larva [Figure 10b].[48,49,50,51] Unlike furuncular myiasis, wound myiasis is more commonly encountered in the developing world, typically arising from the fly larval infestation of the dead necrotic tissue of non-healing wounds such as diabetic and trophic ulcers of leprosy, neglected ulcers etc.[13] Although these can be visualized through unaided eyes [Figure 11a], dermoscopy facilitates the visualization of multiple live larvae in the ulcer, as well as species identification [Figure 11b].[13]
Figure 10.
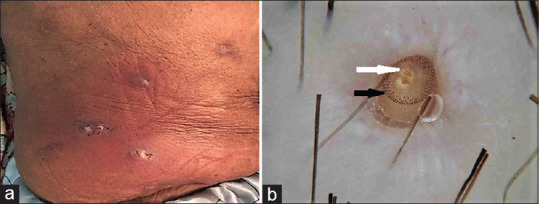
Cutaneous Furuncular Myiasis (a) Clinical image of furuncular myiasis showing erythematous, indurated and tender furuncular nodules induration, over the trunk. Figure courtesy Yusuf et al[48]. (b) Dermoscopic image from another case of furuncular myiasis showing the posterior aspect of the larva. In the center, two bird's feet-like structures (white arrow) correspond to the breathing spiracles. At the periphery of the creamy-white larva, black dots are seen resembling a thorn crown (black arrow) [DermLite handheld II Hybrid dermoscope, polarized, 10×]; Figure courtesy Abraham et al[49]
Figure 11.
Cutaneous Wound Myiasis: (a) Clinical image of wound myiasis showing well-circumscribed tender, boggy scalp ulcer with multiple larvae visible. Figure courtesy Gontijo and Bittencourt[52].(b) Dermoscopic image from the lesion showing numerous yellowish-white larvae with multiple brown dotted rings (green arrow), tracheal tube (blue arrow), and respiratory spiracle (red arrow). Erythema and perifollicular scaling on the scalp can be seen in the periphery. In the center, two bird's feet-like structures (white arrow) correspond to the breathing; Figure courtesy – Gontijo and Bittencourt[52]
Tungiasis
Tungiasis is an infestation caused by the female flea Tunga penetrans, which burrows into the skin. It is endemic in Central and South America, Africa, Pakistan, and India. At first, it appears as a small black dot surrounded by a halo of erythema. With time, it evolves into a pearl-like whitish papule and then into a larger nodule with a well-defined white halo surrounding a black central punctum. The periungual area of the toes is the commonest site.[52]
Dermoscopic examination reveals a whitish homogeneous lesion with a central brown-pigmented ring around a pore, corresponding to the pigmented chitin that surrounds the posterior opening of the flea exoskeleton. The eggs appear as gray-blue blotches or as whitish oval structures linked together to form chain-like structures.[53] Dermoscopy appears to be useful in confirming the diagnosis ex vivo by showing the flea with an inflated jelly sac abdomen full of eggs following the extraction of the intact parasite.[54]
Cutaneous disorders caused by leishmania SPP
Cutaneous Leishmaniasis (CL) is a protozoan skin infection caused by species of the genus Leishmania that are transmitted by Phlebotomus sandflies with a wide clinical spectrum making the diagnosis difficult.[55] In the context of the Indian sub-continent, in addition to the typical presentation of cutaneous leishmaniasis, another entity called the post-kala-azar dermal leishmaniasis (PKDL) with distinctive features is well-known.[56]
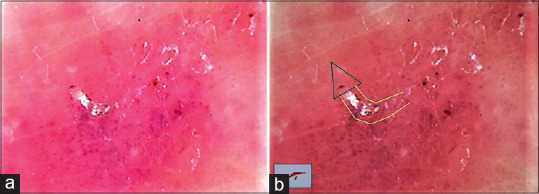
In typical cases of CL, the dermoscopic features vary according to the stage of the lesion - yellow tear-like structures and vessels are seen in early lesions, while central erosion/ulceration combined with scales, a white starburst-like pattern, and vascular structures at the periphery have been detected in late stages of the disease. Generalized erythema, yellow tears, and starburst-like patterns, as well as diverse vascular patterns (dotted, linear-irregular, comma-shaped, polymorphous atypical, hairpin, glomerular-like, corkscrew-like, arborizing vessels) constitute the most commonly detected dermoscopic features of CL lesions.[57] A recent report of two cases from India reiterated these features in Indian patients as well.[58] As CL represents a granulomatous reaction, erythema and yellow to salmon-colored areas are often seen; minimizing their discriminating value for diagnosis of the condition. Other reported features include - milia-like cysts, and a perilesional hypopigmented halo.[58] PKDL is a late cutaneous manifestation of untreated or partially treated visceral leishmaniasis seen typically in the Indian sub-continent.[56] The etiological organism is Leishmania donovani. It characteristically manifests as macules, nodules, plaques, and facial erythema. Mixed/polymorphic form of lesions is the most common, followed by macular lesions, and papulonodular lesions. Dermoscopic features reported from a singular report from India mentions multiple yellow tears and erythema as the prominent features of PKDL [Figure 12a and b].[59] In contrast to lesion of CL, ulcerations and crusting seem to be absent in PKDL lesions.
Figure 12.
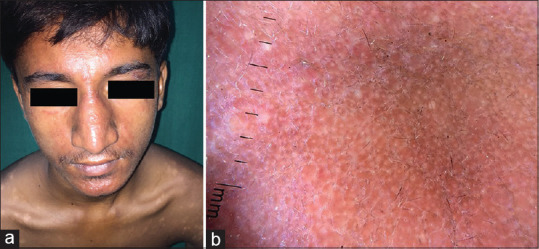
Post-kala azar dermal leishmaniasis (PKDL): (a) Clinical image showing erythematous fleshy papules confined to the chin along with hypopigmented macules involving the trunk; Figures courtesy Jha et al[60]. (b) Dermoscopy of the erythematous papule from the chin revealed erythema, multiple yellow tears with few yellow clods (Dermlite II hybrid m dermoscope, polarized, 10×] [Figures courtesy Jha et al [60]]
Viral Infections
Cutaneous warts
Cutaneous warts are benign proliferations of the epidermis caused by different serotypes of the HPV virus. They may present in different forms, frequently seen as common warts (verruca vulgaris), plane warts (verruca plana or VP), palmar/plantar warts or condyloma acuminata (anogenital warts).[60] They are primarily diagnosed clinically, however in certain situations uncertainty can arise. Flat warts, also known as VP may be mistaken for syringoma, trichoepitheliomas, molluscum, flat or VP-like seborrhoeic keratosis (SK), melanocytic lesions or lichen planus papules. The presence of thrombosed capillaries, a characteristic feature of common and palmoplantar warts that may be visible by naked eye is rarely seen in planar warts. Common wart(s) may be mistaken for hypertrophic actinic keratosis, basal cell carcinomas (BCC), benign appendageal tumors or congenital verrucous epidermal nevi (VEN). Large hyperkeratotic warts may be difficult to distinguish from squamous cell carcinoma (SCC) or related premalignant conditions. This diagnostic confusion is more so in immunocompromised patients who often present with atypical presentations of HPV infection.
Published dermoscopic features of common warts or verruca vulgaris have been divided into two broad categories—surface features, and the vascular component. The externally visible surface morphology better appreciated on dermoscopy has been classified into the certain patterns with the mosaic (or frogspawn) considered the most common. Although the 'frogspawn' pattern characterized by densely packed papillae, each containing red dot or loop and surrounded by a whitish halo[61,62] [Figure 13a] has been conventionally considered as a distinctive surface feature; many argue that both mosaic and frogspawn patterns (the latter appearing as cluster of packed rounded structures resembling a jigsaw puzzle) are non-exclusive.[61] Other surface morphologies include the exophytic keratotic projection [Figure 13b], filiform [Figure 13c], knob-like, daisy flower, and nonspecific patterns.
Figure 13.
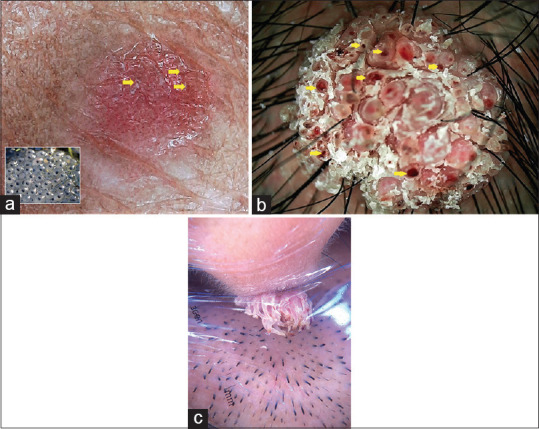
Dermoscopic images of common warts with three different surface morphologies – (a) Raised verrucous surface of a common wart over the neck of an Indian man (appreciate the surrounding acanthosis nigricans) composed of papillary structures, each containing red dot/globule/loop and surrounded by a whitish halo giving a 'frogspawn' appearance (inset); additionally hemorrhagic crusts can be observed focally (yellow arrows) suggesting capillary thrombosis [Escope videodermoscope, polarized, non-contact, 50×]. (b) Florid cauliflower-like exophytic variant of common wart displaying all characteristic dermoscopic features including very densely packed papillae with red centres and whitish halo. Additionally, hemorrhagic crusts (yellow arrows) can be observed practically throughout the wart [Escope videodermoscope, polarized, non-contact, 80×]. (c) Filiform wart showing pink colored papillae with central linear and looped vessels. Also note the 'shriveled effect' produced by the disposable polythene cling film that was placed over the wart during dermoscopy to avoid cross-infection. [Dermlite II hybrid m dermoscope, polarized, 10×]
The vascular structures seen dermoscopically in common warts show polymorphous appearance. Red or black dotted, linear, globular, hairpin, and coiled vessels are typically observed. Of these, hairpin vessels are usually seen in non-wart lesions, although they have also been described in genital warts. Hemorrhages appearing as dark reddish black dots, globules, and streaks corresponding to thrombosed vessels are fairly common and may be considered diagnostic for common and palmoplantar warts.[61,62]
Palmoplantar warts show raised or eroded/perforated yellow-brown structureless areas either devoid of, or with only few appreciable dotted or looped vessels on dermoscopy.[62,63,64] The most characteristic clue is the presence of irregularly distributed hemorrhagic reddish-brown dots (also referred to as 'falooda seeds'),[65] globules, and streaks that represent thrombosed vessels as a result of chronically high vascular pressure at friction-exposed sites [Figure 14a and b]. In contrast, a plantar corn/callosity, is characterized by a transluscent homogenously opaque central core [Figure 14c] that lacks hemorrhagic structures. While high magnification polarized VD allows this distinction without the need of sloughing off the surface, superficial paring followed by dermoscopic evaluation can easily confirm the diagnosis in doubtful cases. Second point of difference between a palmo-plantar wart and corn/callosity is that the skin lines or dermatoglyphics get typically interrupted in warts, but spared or wrap smoothly around the nucleus in the latter. Two pitfalls warrant consideration here. First, the dust particles that tend to stick to the plantar corn may give “pseudo hemorrhagic dots”, which are more brownish-black in color; thus any such lesion especially over the sole should be thoroughly cleansed with alcohol and/or acetone before dermoscopy. Second, after a plantar wart is treated with an ablative procedure like cryotherapy, and post-procedure epithelization is complete, the recovering lesion may not show the typical florid hemorrhagic globules/streaks [Figure 14d].
Figure 14.
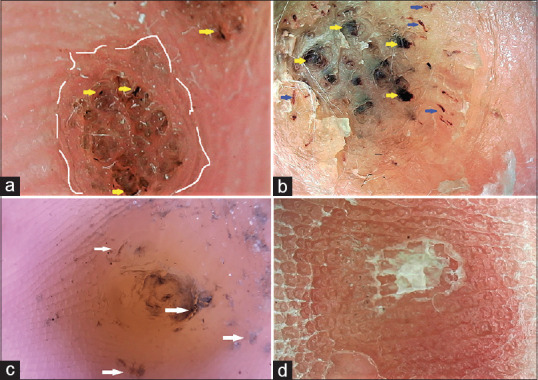
Plantar wart versus callosity: (a) Dermoscopy of a typical plantar wart showing the translucent yellowish-to-light brown packed papillary structures, interspersed with numerous hemorrhagic globules and streaks (yellow arrows). Also appreciate the complete disruption of the normal dermatoglyphics of the involved area of the sole (white broken arcs) by the viral invasion [Escope videodermoscope, polarized, non-contact, 50×]. (b) Higher magnification videodermoscopic view of an older and deeper plantar wart displaying plentiful and large hemorrhagic structures (yellow arrows), as well as streaks (blue arrows) in the periphery [Escope videodermoscope, polarized, non-contact, 150×]. (c) Dermoscopic image of a plantar callosity showing a homogenously opaque central translucent core and lack of vascularity. Appreciate the brownish-black 'pseudo-hemorrhagic structures' that are irregularly scattered (white arrows) and represent artifacts arising from dust and dirt [Dermlite II hybrid m dermoscope, polarized, 10×]. (d) Dermoscopic image of a post-cryoablation plantar wart, taken 2 weeks after the treatment session. Although yellowish-red structureless area can be appreciated, the dermatoglyphics are not as distorted, nor the centre of the lesion show the hemorrhagic crusts typical of an active wart [Escope videodermoscope, polarized, non-contact, 50×]
Tanioka M et al. and Arpaia N et al. have also reported parallel ridge pattern in acral warts.[66,67] The dermoscopic hallmark of plane warts is a skin-colored to crimson-to-yellowish colored background, with regularly distributed, tiny, red dots or globular vessels. The other common pattern described is that of “even-colored light brown to yellow patch without dots or globular vessels”. In certain cases, microkoebnerization may be appreciated. Since VP-like flat SK constitutes one of the most difficult clinical differential of VP lesions, their dermoscopic differentiation merits discussion. In contrast to VP, VP-like SK typically lacks microkoebnerization, has a brownish or brown-predominant background, may have milia-like cysts, comedo-like structures, and an evolving cerebriform structure. Importantly, vascular structures are much less common; even if present, non-uniformly scattered red dots may be seen but globular vessels are typically not seen.
Flat warts dermoscopically show an even colored light or dark brown to yellow background with regularly distributed tiny red dots. These characteristic features help in distinguishing flat warts from close differentials like comedones which show central yellow to white pore of the hair follicle opening. Seborrheic keratosis maybe differentiated dermoscopically by their typical features like cerebriform appearance, milia-like cysts, and comedo-like openings.[68,69]
Dermoscopy of genital warts varies according to their morphology. Papular lesions show features similar to common warts, i.e., whitish areas with central dilated glomerular or dotted vessels. Condyloma accuminata shows multiple whitish fingerlike to knoblike papillae arising from a common base showing elongated and dilated vessels that are more prominent at the periphery. The vessels appear dilated in response to the nitric oxide production from the human papilloma viruses. These features help in differentiating genital warts from pearly penile papules, Fordyce's spots, molluscum contagiosum, vestibular papillae, lymphangiomas, angiokeratomas and other close clinical differentials.[70] The projections of warts have conglomerate vascular structures and are more white and broader than vestibular papillae, which may correlate with the hyperkeratotic and acanthotic features of condyloma acuminata.[71]
The mainstay for dermoscopic diagnosis of the warts has been presence of a vascular component reflecting the dilated and thrombosed vessels within the papillary dermis. However, in Fitzpatrick skin types 4-6, the vascularity maybe difficult to appreciate. A reason for this could be the pigmented nature of lesions obscuring fine vascularity in skin of color population. Secondly, another important tip to diagnose warts dermoscopically is that video and non-contact dermoscopes are recommended as they generally provide greater magnification and eliminate blanching which is helpful in picking fine vascular structures. Moreover, the clinician does not have to go too close to the patient as in cases of hand-held dermoscopes which maybe uncomfortable when dealing with certain infective dermatoses, like genital warts.
Molluscum contagiosum
Molluscum contagiosum is a common and contagious viral infection of the epidermal keratinocytes with characteristic intracytoplasmic inclusions. Lesions are characterized as multiple umbilicated skin-colored papules, with a translucent, glossy appearance.[72]
Clinically molluscum contagiosum is easily diagnosed, but sometimes it may be difficult when there is lack of central umbilication, atypical lesions, single lesion or as several small inflamed lesions.
Dermoscopy of molluscum contagiosum shows the presence of a central yellowish-white structure and vessels around the lesion in various patterns.[73,74] [Figure 15] The central yellowish-white structure appears as polylobular amorphous area. Vascular pattern maybe arranged in a number of ways, with crown vascular pattern/'corona'–like vessels being the most common.[74] In addition to the crown vascular pattern, other reported patterns include vessels that extend through the amorphous structure of the lesions towards their core, without crossing it as a radial pattern.[73] Punctiform vessels, present as small reddish dots inside the lesion, are also seen in molluscum contagiosum, though they have been described in numerous diseases such as melanoma, clear cell acanthoma, lichen planus and eccrine poroma.[75]
Figure 15.

Dermoscopy of molluscum contagiosum showing central yellowish-white polylobular structure [Escope videodermoscope, polarized, non-contact, 50×]
Dermatophytic Infections
Dermoscopy may serve as a rapid diagnostic tool leading to prompt treatment initiation, thereby playing a role in the pandemic of dermatophytosis in India.
Dermoscopic findings in tinea corporis include diffuse erythema, whitish scales, follicular micropustules, brown dots surrounded by a white-yellowish halo, wavy or broken hair. Morse code hairs of vellus hairs can be seen in which there are horizontal white bands related to localized areas of fungal infection. These horizontal white bands are usually multiple and may cause the hair to bend and break.[76] Nicole et al. reported a case of tinea corporis in an infant in whom dermoscopy helped to determine vellus hair involvement, causing treatment to be switched from topical to systemic antifungal therapy[77] [Figure 16a and b].
Figure 16.
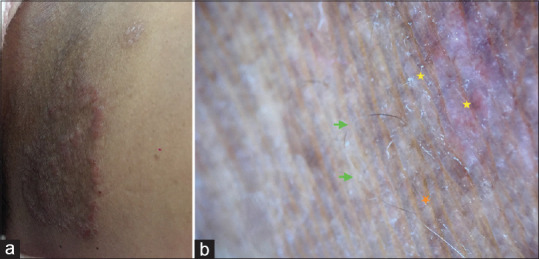
Tinea cruris. (a) clinical picture showing erythematous scaly plaque in the groin. (b) Dermoscopic features suggesting fungal invasion of hair follicle (green arrows), diffuse erythema and scaling (yellow stars) and brownish pigmented blothches (orange star). (Dermlite DL3N 20X, polarized mode)
Tinea manuum and tinea pedis on dermoscopic examination show the whitish scales along the palmar and plantar creases, brownish scales showing dried vesicles and intense erythema, unrelated to that of psoriasis or eczema [Figure 17a and b].
Figure 17.
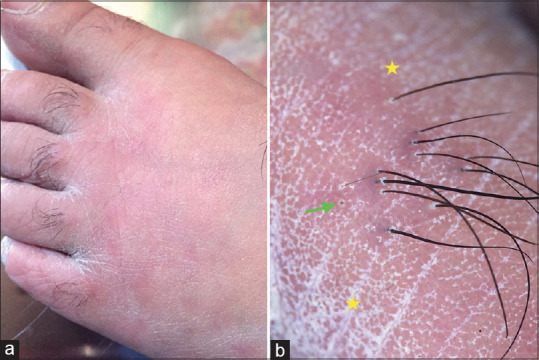
Tinea pedis, (a) Clinical picture depicting erythema and scaling pronounced over the web spaces. (b) Erythema and whitish scaling in the creases (yellow stars), broken hair (green arrow) (Dermlite DL3N 10X, polarized mode)
Dermoscopy of tinea incognito yields morse code hairs of vellus hairs, follicular micropustules, concentric areas of erythema, easily deformable hairs that look weakened and transparent and show unusual bends, in addition to the features of tinea corporis. Glomez Moyano et al. observed scaly, broken, translucent and morse code hairs in an adult with tinea incognito, correlating this finding with direct microscopy[78] [Figure 18a and b].
Figure 18.
Tinea incognito. (a) Ill defined erythematous plaques with excoriations. (b) Translucent hair that looks weakened & shows bends (green arrows), erythema & mild scaling (yellow star), perifollicular scales and pustules (blue arrows) (Dermlite DL3N 20X, polarized mode)
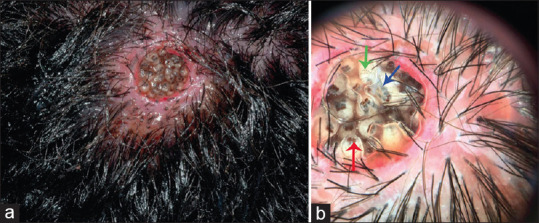
Dermoscopic features of tinea capitis reveal comma, corkscrew and zig-zag hair, black dots, short vellus and bar code (morse code) hairs. Inter-follicular scales and follicular pustules/abscesses can be seen in the kerion type. Cigarette ash hairs can be seen in patients on antifungal treatment. Rafael et al. reported dermoscopic results in 43 patients with tinea capitis in which comma hairs were found in 7 and corkscrew hair in 3 patients[79] [Figure 19a and b].
Figure 19.
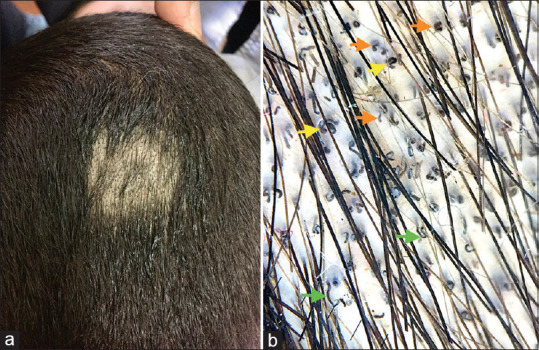
Tinea capitis. (a) Clinical picture of localised patch of alopecia showing black dots and scaling. (b) Comma hairs (orange arrows), corkscrew hairs (yellow arrows), zig-zag hairs (green arrows). (Dermlite DL3N 10X, polarized mode)
Dermoscopic findings in onychomycosis include spikes and longitudinal striations of different colors (aurora borealis pattern), pseudoleuconychia, and melanonychia[80] [Figure 20a and b].
Figure 20.
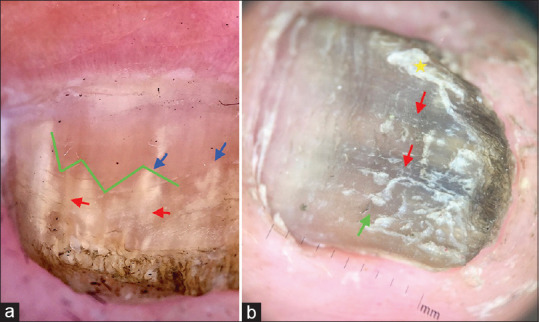
Onychomycosis. (a) Jagged edge of the proximal margin of the onycholytic area (green lines), with sharp structure (spikes) directed to the proximal fold (blue arrows arrow), white- yellow longitudinal striae in the onycholytic nail plate (red arrows). (Dermlite DL3N 10X, polarized mode). (b) Fungal melanonychia: Dull matte black pigmented (red arrow) and yellow areas (green arrows) and pseudoleuconychia (yellow star). (Dermlite DL3N 10X, polarized mode)
A new criterion for systemic antifungal therapy in tinea has been described: the observation of parasitized vellus hairs on direct examination.[81] Dermoscopic examination can predict from the outset which cases of tinea will respond poorly or even not respond at all to topical treatment alone. Dermoscopy is no substitute for mycological study, but rather it complements it, as the parasitism of the vellus hair can be seen only by direct examination or with trichoscopy, but not in culture.[82]
Bacterial Infections
Mycobacterial infections
Dermoscopy has been a very useful tool and plays a significant supportive role in the diagnosis of granulomatous conditions including mycobacterial infections like lupus vulgaris and Hansen's disease.[83]
Dermoscopy of lupus vulgaris shows repetitive pattern of orange to golden background pigmentation along with focused linear telangiectasias and an overlying whitish hue or whitish reticulated streaks.[7] The characteristic yellowish-orange hue corresponds to the dermal granulomatous infiltrate. While it is easily appreciated in lighter skin phototypes, the same is relatively less conspicuous in darker skin. Moreover, pigmented structures are often seen at the periphery of a healed or advanced lesion signifying post-inflammatory pigment incontinence [Figure 21a and b].
Figure 21.
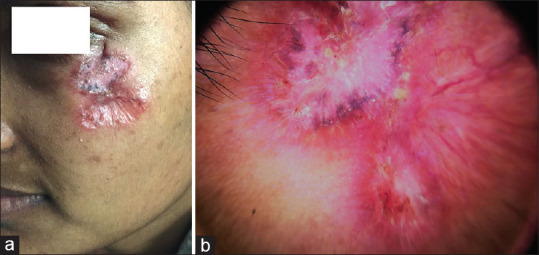
Lupus vulgaris. (a) Clinically erythematous atrophic plaque with scarring extending from the left lower canthus to the cheek. (b) Dermoscopy revealing crimson-red to faint orangish background with yellowish structureless areas (black arrows), multiple linear branching vessels (white stars), and few whitish streaks (yellow diamonds). In addition, a pink scar surrounded by few brown to blue-grey pigmented globules and clods (green arrows) can be appreciated in the upper andcentral field. [DermLite II hybrid m; polarized, 10×]
Dermoscopic imaging of the lesions of borderline tuberculoid (BT) leprosy demonstrates white areas, yellow globules, linear branching telangiectasia, and decreased white dots as well as hairs. White areas correspond to a decrease in the number of melanocytes in BT leprosy. The yellow globules with telangiectasia are generally considered a hallmark of granulomas, present in the dermis. Yellow globules, however, are not observed in all lesions of BT leprosy. They show subtle presence in infiltrated areas of hypopigmented patches but are prominent in facial areas. This may be attributed to thin epidermis on the face that enhances the visibility of yellow globules in the infiltrated lesions[83] [Figure 22].
Figure 22.
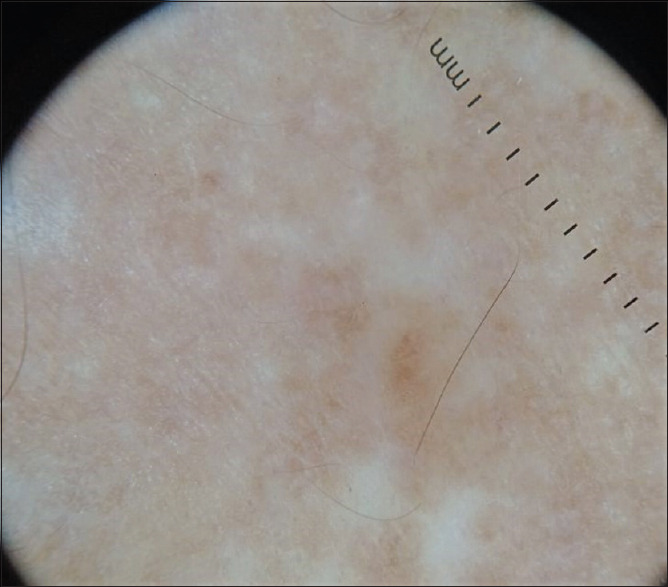
Dermoscopy of hypopigmented macule of borderline Hansen's disease showing scattered dull-white structureless areas with accentuation along skin markings, reduced white dots of eccrine and follicular ostia, and a significant amount of residual pigment network visible [Dermlite 4, polarized, 10X]
Dermoscopy of histoid leprosy (HL) demonstrates whitish-yellow structureless area and linear branching vessels. The whitish-yellow structureless area corresponds to granuloma and whitish color is suggested to correspond to whorled arrangement of spindle-shaped histiocytes in the granuloma in HL. Vessels are in accordance to the vessels noted in other granulomatous conditions.[84]
Pseudomonas infections
Pseudomonas folliculitis (PF) is a community-acquired infection typically resulting from the bacterial colonization of hair follicles after direct exposure to contaminated fomites. Lesions begin as pruritic; erythematous macules that progress to erythematous papules, some of which form folliculo-centric pustules.[85] Dermoscopy has been used to differentiate PF from insect bites and nodular scabies. PF shows presence of vellus hair at the center of the lesion, not otherwise visible through naked eye. Lesions of insect bites and nodular scabies are not centered on the hair follicle. Moreover, the oedema from the pseudomonal infections gives a pale hue to the lesion under dermoscopy.[86]
Corynebacterium infections
Gram-positive bacteria, mainly Corynebacterium species, cause pitted keratolysis. On dermoscopy, the periphery of the crater shows heterogeneous architecture suggesting random dissolution of stratum corneum by the bacterial colonies.[87]
Trichobacteriosis, mostly caused by Corynebacterium tenuis, is a bacterial infection limited to the hair shaft. The dermoscopic characters described in this condition are: concretions and nodules along the length of the hair shaft, cottony structures, flame-like pale yellowish adherent nodules, plume sign and skewer sign.[88,89]
Others
Dermoscopy has been used as an adjunct to the clinical and microbiological diagnosis of some other bacterial infections like buruli ulcer (caused by M. ulcerans), staphylococcal folliculitis, to differentiate staphylococcal scalded skin syndrome from toxic epidermal necrolysis, however they need further validation.[90,91,92]
Artefacts and Practical Issues
Artefacts are common observations in dermoscopy examination. Since artefacts may interfere with evaluation and diagnosis of different dermatological disorders, every dermatologist should be well aware with their presence and their types so that correct dermoscopic evaluation can be done. Dermoscopy being well known to improve the diagnostic accuracy in dermatology can also help in detecting those artefacts that are not visible or distinguishable by naked eye.[93]
Artefacts may arise due to various reasons like external applications, seasonal effects, and cultural practices. Face and hair being the most exposed parts of the body, exogenous particles (personal application and foreign material) have the highest tendency to come in contact with them and thus produce higher chances of application related artefacts. Season related artefacts commonly seen are dirt, henna, holi color and sunscreen while vermillion and hair oil application are related with the local cultural practices. In context to entodermoscopy, two important infestations seen over face and hair are demodex folliculitis and pediculosis capitis.[94,95] Artefacts can obscure the visualization and create difficulties in diagnosing these infestations.
Sunscreen is one of the commonest artefacts on the face which may be attributed to the fact that it is the most prescribed treatment in select facial pigmentary disorders. Presence of sunscreen causes obliteration of sebaceous openings and thus can obscure the erythema and scaling caused by demodex folliculitis. It can also cause difficulty in visualizing the tail of demodex mite which is pathognomonic for diagnosis.[39] Similar difficulty in visualization over face can be encountered due to another artefact, i.e., face powder which is commonly applied by women particularly in rural areas. Dirt and camouflage agents are among the less common agents seen over face but can give rise to similar problems for diagnosis.
Diagnosis of Pediculosis capitis is based on dermoscopic visualization of nits, mite, and nymph containing eggs.[95] These can be masqueraded by various agents applied over hair in different situations. Minoxidil crystals represent a major artefact over hair. These crystals appear as shiny crystals enclosing the hair root sheath and give a false perception of scales of psoriasis or seborrheic dermatitis, and they can easily mask the appearance of nits of pediculosis capitis.
Both vermillion and red Holi color produce a background of false erythema, which can be easily confused for inflammatory scalp disorders. Similarly, hair dye application which is a common practice in middle aged group, presents as an important artefact by imparting a brownish-black hue to the scalp. Hair dye can cause difficulty in visualization of nits and eggs. Hair fibers used nowadays as a camouflaging agent also appear as a prominent artefact. Application of hair oil and hair gel also appears as artefacts because of their ability to differentially reflect and refract light. Therefore, artefacts should always be kept in mind when the dermoscopy findings mismatch with clinical suspicion. Thorough cleansing of the area with spirit or acetone and calling the patient after a proper head wash with shampoo is definitely useful to minimize artefact-related outcomes.
Conclusion
The diagnostic and other uses of dermoscopy have been rapidly expanding across practically all groups of cutaneous disorders. There has been a growing body of evidence for the use of this technique in the diagnosis of cutaneous infections and infestations. While the conventional methods like microscopy, including the use of special stains, microbial cultures, histopathology, and molecular detection methods continue to serve as the gold standard for diagnosis and/or reference for comparison against other and emerging modalities like dermoscopy, for an experienced dermoscopist, the use of this technology offers several advantages over the conventional gold standards. The key dermoscopic findings for cutaneous infections and infestations are summarized in Table 2. A thorough knowledge of entodermoscopy will empower dermatologists to promptly, non-invasively, and confidently diagnose and manage cutaneous infections and infestations, both as a lone modality, as well as in facilitating patient approval for an invasive diagnostic test, if required.
Table 2.
Key dermoscopic findings of various cutaneous infections and infestations
| Infection/infestation | Key dermoscopic findings |
|---|---|
| Parasitic infections | |
| Pediculosis capitis | Viable nits: brown, translucent, ovoid eggs with convex extremity firmly attached to the hair shaft |
| Empty nits: translucent with a plane and fissured free ending. | |
| Phthiriasis pubis | Lice adherent to the pubic hair (conical shape of the operculum and the wide fixing sleeve of egg to hair) |
| Scabies | Mite appear as ‘circumflex accent’ like image/“triangle sign” |
| Burrows appear as “S” or “Z” shaped structures (“the delta glider” or “jet with contrail” sign) | |
| Demodex folliculorum | Demodex tails- gelatinous, whitish 1-3 mm creamy thread protruding from skin surface |
| Demodex follicular openings - round, amorphic, grayish/light brown plugs surrounded by an erythematous halo | |
| Cutaneous larva migrans | Translucent brownish structureless areas in a segmental arrangement |
| Tungiasis | Well-defined white halo surrounding a black central punctum. |
| Cutaneous Leishmaniasis | Early lesions: yellow tear-like structures and vessels |
| Later stages: central erosion/ulcerations combined with scales, a white starburst-like pattern, and vascular structures. | |
| Viral infections | |
| Viral warts | Irregular whitish structures, white haloes, or densely packed papillae with central vascular structures |
| Molluscum contagiosum | Central yellowish-white polylobular amorphous structure with surrounding vessels |
| Fungal infections | |
| Tinea corporis | Diffuse erythema, whitish scales, follicular micropustules, brown dots surrounded by a white-yellowish halo, wavy/broken hair. Vellus and morse code hairs. |
| Tinea manuum and tinea pedis | Whitish scales along the palmar & plantar creases |
| Tinea capitis | Comma, corkscrew and zig-zag hair, black dots, short vellus and bar code (morse code) hairs |
| Onychomycosis | Spikes and longitudinal striations of different colors (aurora borealis pattern), pseudoleuconychia and melanonychia |
| Bacterial infections | |
| Lupus vulgaris | Repetitive pattern of orange to golden background pigmentation along with focused linear telangiectasias |
| Tuberculoid leprosy | White areas, yellow globules, linear branching telangiectasia, and decreased white dots as well as hairs |
| Histoid leprosy | Whitish-yellow structureless areas and linear branching vessels |
| Pseudomonas folliculitis | Pale hue, central vellus hair |
| Pitted keratolysis | Heterogeneous architecture at the periphery of the craters |
| Trichobacteriosis | Concretions and nodules along the length of the hair shaft, cottony structures, flame-like pale yellowish adherent nodules, plume sign and skewer sign |
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sonthalia S, Pasquali P, Agrawal M, Sharma P, Jha AK, Errichetti E, et al. Dermoscopy update: Review of its extradiagnostic and expanding indications and future prospects. Dermatol Pract Concept. 2019;9:253–4. doi: 10.5826/dpc.0904a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sonthalia S, Errichetti E. Dermoscopy—not just for diagnosis and not just for dermatologists! Kathmandu Univ Med J (KUMJ) 2017;15:1–2. [PubMed] [Google Scholar]
- 3.Sonthalia S, Yumeen S, Kaliyadan F. Dermoscopy Overview and Extradiagnostic Applications. [Updated 2020 Aug 13]. In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2020. Jan, [PubMed] [Google Scholar]
- 4.Errichetti E, Stinco G. Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb) 2016;6:471–507. doi: 10.1007/s13555-016-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scanni G, Bonifazi E. Viability of the head louse eggs in pediculosis capitis. A dermoscopy study. Eur J Pediat Dermatol. 2006;16:201–4. [Google Scholar]
- 6.Zalaudek I, Giacomel J, Cabo H, Di Stefani A, Ferrara G, Hofmann-Wellenhof R, et al. Entodermoscopy: A new tool for diagnosing skin infections and infestations. Dermatology. 2008;216:14–23. doi: 10.1159/000109353. [DOI] [PubMed] [Google Scholar]
- 7.Verzì AE, Lacarrubba F, Dinotta F, Micali G. Dermatoscopy of parasitic and infectious disorders. Dermatol Clin. 2018;36:349–58. doi: 10.1016/j.det.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Micali G, Verzì AE, Lacarrubba F. Alternative uses of dermoscopy in daily clinical practice: An update. J Am Acad Dermatol. 2018;79:1117–32e1. doi: 10.1016/j.jaad.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 9.Piccolo V. Update on dermoscopy and infectious skin diseases? Dermatol Pract Concept. 2019;10:e2020003. doi: 10.5826/dpc.1001a03. doi: 10.5826/dpc. 1001a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scanni G. Human phthiriasis. Can dermoscopy really help dermatologists? Entodermoscopy: A new dermatological discipline on the edge of entomology. G Ital Dermatol Venereol. 2012;147:111–7. [PubMed] [Google Scholar]
- 11.Criado PR. Entodermoscopy: Dermoscopy for the diagnosis of pediculosis. An Bras Dermatol. 2011;86:370–1. doi: 10.1590/s0365-05962011000200027. [DOI] [PubMed] [Google Scholar]
- 12.Scanni G. The mite-gallery unit: A new concept for describing scabies through entodermoscopy. Trop Med Infect Dis. 2019;4:48. doi: 10.3390/tropicalmed4010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gontijo JRV, Bittencourt FV. Wound myiasis: The role of entodermoscopy. An Bras Dermatol. 2018;93:746–8. doi: 10.1590/abd1806-4841.20188043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cinotti E, Labeille B, Bernigaud C, Fang F, Chol C, Chermette R, et al. Dermoscopy and confocal microscopy for in vivo detection and characterization of Dermanyssus gallinae mite. J Am Acad Dermatol. 2015;73:e15–6. doi: 10.1016/j.jaad.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 15.Sonthalia S, Gupta A, Jha AK, Sarkar R, Ankad BS. Disorders of pigmentation. In: Lallas A, Errichetti E, Ioannides D, editors. Dermoscopy in General Dermatology. 1st ed. London: CRC Press; 2018. pp. 282–94. [Google Scholar]
- 16.Gupta V, Sonthalia S, Bhat YJ, Langar S, Bosseila M. Inflammatory and infectious conditions. In: Lallas A, Errichetti E, Ioannides D, editors. Dermoscopy in General Dermatology. 1st ed. London: CRC Press; 2018. pp. 295–309. [Google Scholar]
- 17.Sonthalia S, Jha AK, Goldust M, Omchery A, Dayrit JF. Dermoscopic characterization in pigmented skin: Interpret “pigmented” structures carefully. Dermatol Pract Concept. 2019;9:211–3. doi: 10.5826/dpc.0903a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papageorgiou V, Apalla Z, Sotiriou E, Papageorgiou C, Lazaridou E, Vakirlis S, et al. The limitations of dermoscopy: False-positive and false-negative tumours. J Eur Acad Dermatol Venereol. 2018;32:879–88. doi: 10.1111/jdv.14782. [DOI] [PubMed] [Google Scholar]
- 19.Penso-Assathiany D, Gheit T, Prétet JL, Aubin A, Massimo T, Mougin C, et al. Presence and persistence of human papillomavirus types 1, 2, 3, 4, 27, and 57 on dermoscope before and after examination of plantar warts and after cleaning. J Am Acad Dermatol. 2013;68:185–6. doi: 10.1016/j.jaad.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 20.Chattopadhyay M, Blackman Northwood M, Ward B, Sule J, Burrows NP. Are dermatoscopes a potential source of nosocomial infection in dermatology clinics.? Clin Exp Dermatol. 2014;39:401–4. doi: 10.1111/ced.12277. [DOI] [PubMed] [Google Scholar]
- 21.Mun JH, Park SM, Ko HC, Kim BS, Kim MB. Prevention of possible cross-infection among patients by dermoscopy: A brief review of the literature and our suggestion. Dermatol Pract Concept. 2013;3:33–4. doi: 10.5826/dpc.0304a07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jakhar D, Bhat YJ, Chatterjee M, Vinay, Ankad BS, Jha AK, et al. Dermoscopy practice during COVID-19 pandemic: Recommendations by SIG dermoscopy (IADVL Academy) Indian Dermatol Online J. 2020;11:343–4. doi: 10.4103/idoj.IDOJ_231_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jakhar D, Kaur I, Kaul S. Art of performing dermoscopy during the times of coronavirus disease (COVID-19): Simple change in approach can save the day! J Eur Acad Dermatol Venereol. 2020;34:e242–4. doi: 10.1111/jdv.16412. [DOI] [PubMed] [Google Scholar]
- 24.Badri T, Hammami H, Benmously R, Mokhtar I, Fenniche S. Dermoscopic diagnosis of pediculosis capitis. Acta Dermatovenerol Alp Pannonica Adriat. 2010;19:45–6. [PubMed] [Google Scholar]
- 25.Di Stefani A, Hofmann-Wellenhof R, Zalaudek I. Dermoscopy for diagnosis and treatment monitoring of pediculosis capitis. J Am Acad Dermatol. 2006;54:909–11. doi: 10.1016/j.jaad.2005.11.1083. [DOI] [PubMed] [Google Scholar]
- 26.Nikam VV, Mehta HH. A nonrandomized study of trichoscopy patterns using nonpolarized (contact) and polarized (noncontact) dermatoscopy in hair and shaft disorders. Int J Trichology. 2014;6:54–62. doi: 10.4103/0974-7753.138588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sonthalia S, Varma S, Jha AK. Dermoscopy of pubic louse. Indian Dermatol Online J. 2019;10:90–1. doi: 10.4103/idoj.IDOJ_35_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang Q, Ran X, Ran YP. Cover image: Dermoscopy in vivo for the life cycle of Phthirus pubis. Br J Dermatol. 2017;176:279. doi: 10.1111/bjd.15049. [DOI] [PubMed] [Google Scholar]
- 29.Zalaudek I, Argenziano G. Dermoscopy of nits and pseudonits. N Engl J Med. 2012;367:1741. doi: 10.1056/NEJMicm1103059. [DOI] [PubMed] [Google Scholar]
- 30.Lacarrubba F, Micali G. The not-so-naked eye: Phthiriasis palpebrarum. Am J Med. 2013;126:960–1. doi: 10.1016/j.amjmed.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 31.Lacarrubba F, Nardone B, Milani M, Botta G, Micali G. Head lice: Ex vivo videodermatoscopy evaluation of the pediculocidal activity of two different topical products. G Ital Dermatol Venereol. 2006;141:233–5. [Google Scholar]
- 32.Prins C, Stucki L, French L, Saurat JH, Braun RP. Dermoscopy for the in vivo detection of Sarcoptes scabiei. Dermatology. 2004;208:241–3. doi: 10.1159/000077310. [DOI] [PubMed] [Google Scholar]
- 33.Dupuy A, Dehen L, Bourrat E, Lacroix C, Benderdouche M, Dubertret L, et al. Accuracy of standard dermoscopy for diagnosing scabies. J Am Acad Dermatol. 2007;56:53–62. doi: 10.1016/j.jaad.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 34.Walter B, Heukelbach J, Fengler G, Worth C, Hengge U, Feldmeier H. Comparison of dermoscopy, skin scraping, and the adhesive tape test for the diagnosis of scabies in a resource-poor setting. Arch Dermatol. 2011;147:468–73. doi: 10.1001/archdermatol.2011.51. [DOI] [PubMed] [Google Scholar]
- 35.Ma Y, Hu w, Wang P, Bian K, Liu Z. Dermoscopy combined with ink staining as one more method to diagnose nodular scabies. Indian J Dermatol Venereol Leprol. 2019;85:324–5. doi: 10.4103/ijdvl.IJDVL_516_18. [DOI] [PubMed] [Google Scholar]
- 36.Aydıngöz IE, Mansur AT. Canine scabies in humans: A case report and review of the literature. Dermatology. 2011;223:104–6. doi: 10.1159/000327378. [DOI] [PubMed] [Google Scholar]
- 37.Litwin D, Chen W, Dzika E, Korycińska J. Human permanent ectoparasites; recent advances on biology and clinical significance of demodex mites: Narrative review article. Iran J Parasitol. 2017;12:12–21. [PMC free article] [PubMed] [Google Scholar]
- 38.Chen W, Plewig G. Human demodicosis: Revisit and a proposed classification. Br J Dermatol. 2014;170:1219–25. doi: 10.1111/bjd.12850. [DOI] [PubMed] [Google Scholar]
- 39.Segal R, Mimouni D, Feuerman H, Pagovitz O, David M. Dermoscopy as a diagnostic tool in demodicidosis. Int J Dermatol. 2010;49:1018–23. doi: 10.1111/j.1365-4632.2010.04495.x. [DOI] [PubMed] [Google Scholar]
- 40.Friedman P, Sabban EC, Cabo H. Usefulness of dermoscopy in the diagnosis and monitoring treatment of demodicidosis. Dermatol Pract Concept. 2017;7:35–8. doi: 10.5826/dpc.0701a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sonthalia S, Jha AK, Sharma R. The role of dermoscopy in a topical steroid-damaged face. Dermatol Pract Concept. 2018;8:166–7. doi: 10.5826/dpc.0803a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aljasser MI, Lui H, Zeng H, Zhou Y. Dermoscopy and near-infrared fluorescence imaging of cutaneous larva migrans. Photodermatol Photoimmunol Photomed. 2013;29:337–8. doi: 10.1111/phpp.12078. [DOI] [PubMed] [Google Scholar]
- 43.Crocker-Sandoval AB, Sánchez-Dueñas LE, Quiñones-Venegas R, González-Ramírez RA, Orendain-Koch N. Hallazgos dermatoscópicos en larva migrans. Dermatol Rev Mex. 2015;59:98–101. [Google Scholar]
- 44.Shirato T, Iwata H, Yoshimoto N, Nomura Y, Yamane N, Shimizu H. Dermoscopy is useful for bed bug (Cimex lectularius) bites. J Eur Acad Dermatol Venereol. 2016;30:539–40. doi: 10.1111/jdv.12938. [DOI] [PubMed] [Google Scholar]
- 45.Malhotra AK, Lis JA, Ramam M. Cydnidae (burrowing bug) pigmentation: A novel arthropod dermatosis. JAMA Dermatol. 2015;151:232–3. doi: 10.1001/jamadermatol.2014.2715. [DOI] [PubMed] [Google Scholar]
- 46.Sonthalia S. Dermoscopy of cydnidae pigmentation: A novel disorder of pigmentation. Dermatol Pract Concept. 2019;9:228–9. doi: 10.5826/dpc.0903a15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poojary S, Baddireddy K. Demystifying the stinking reddish brown stains through the dermoscope: Cydnidae pigmentation. Indian Dermatol Online J. 2019;10:757–8. doi: 10.4103/idoj.IDOJ_346_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yusuf MA, Pritt BS, McMichael JR. Cutaneous myiasis in an elderly woman in Somaliland. Int J Womens Dermatol. 2019;5:187–9. doi: 10.1016/j.ijwd.2019.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abraham LS, Azulay-Abulafia L, Aguiar Dde P, Torres F, Argenziano G. Dermoscopy features for the diagnosis of furuncular myiasis. An Bras Dermatol. 2011;86:160–2. doi: 10.1590/s0365-05962011000100027. [DOI] [PubMed] [Google Scholar]
- 50.Silva de Lima A, Rovere RK. Furuncular myiasis: Dermoscopic features using a cross-polarized device without contact. J Am Acad Dermatol. 2015;72(1 Suppl):S6–7. doi: 10.1016/j.jaad.2014.02.045. [DOI] [PubMed] [Google Scholar]
- 51.Bernardes Filho F, Martins G, Barbará EF, Paiva ML, Coelho Filho RL, Nery JA. Dermoscopy as an auxiliary tool for the diagnosis of furuncular myiasis. An Bras Dermatol. 2014;89:663–5. doi: 10.1590/abd1806-4841.20142975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen CW, Thong HY, Jee SH. Tungiasis: A case report and review of the literature. Dermatol Sinica. 2011;29:29–31. [Google Scholar]
- 53.Criado PR, Landman G, Reis VM, Belda W., Jr Tungiasis under dermoscopy: In vivo and ex vivo examination of the cutaneous infestation due to Tunga penetrans. An Bras Dermatol. 2013;88:649–51. doi: 10.1590/abd1806-4841.20132071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abarzua A, Cataldo K, Alvarez S. Dermoscopy in tungiasis. Indian J Dermatol Venereol Leprol. 2014;80:371–3. doi: 10.4103/0378-6323.136980. [DOI] [PubMed] [Google Scholar]
- 55.Torres-Guerrero E, Quintanilla-Cedillo MR, Ruiz-Esmenjaud J, Arenas R. Leishmaniasis: A review. F1000es. 2017;6:750. doi: 10.12688/f1000research.11120.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zijlstra EE, Kumar A, Sharma A, Rijal S, Mondal D, Routray S. Report of the Fifth Post-Kala-Azar Dermal Leishmaniasis Consortium Meeting, Colombo, Sri Lanka, 14–16 May 2018? Parasites Vectors. 2020;13:159. doi: 10.1186/s13071-020-04011-7. doi: 10.1186/s13071-020-04011-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Serarslan G, Ekiz Ö, Özer C, Sarıkaya G. Dermoscopy in the diagnosis of cutaneous leishmaniasis. Dermatol Pract Concept. 2019;9:111–8. doi: 10.5826/dpc.0902a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bhat YJ, Yaseen A, Sheikh S, Hassan I. Dermoscopy of two cases of cutaneous leishmaniasis. Indian J Dermatol. 2020;65:232–4. doi: 10.4103/ijd.IJD_284_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jha AK, Sonthalia S, Lallas A. Dermoscopy of post Kala-Azar dermal leishmaniasis. Indian Dermatol Online J. 2018;9:78–9. doi: 10.4103/idoj.IDOJ_49_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cliffe J, Morris-Jones R. Management of cutaneous viral warts. BMJ. 2014;348:g3339. doi: 10.1136/bmj.g3339. [DOI] [PubMed] [Google Scholar]
- 61.Li X, Yu J, Thomas S, Lee K, Soyer HP. Clinical and dermoscopic features of common warts. J Eur Acad Dermatol Venereol. 2017;31:e308–10. doi: 10.1111/jdv.14093. [DOI] [PubMed] [Google Scholar]
- 62.Lallas A, Giacomel J, Argenziano G, García-García B, González-Fernández D, Zalaudek I, et al. Dermoscopy in general dermatology: Practical tips for the clinician. Br J Dermatol. 2014;170:514–26. doi: 10.1111/bjd.12685. [DOI] [PubMed] [Google Scholar]
- 63.Bae JM, Kang H, Kim HO, Park YM. Differential diagnosis of plantar wart from corn, callus and healed wart with the aid of dermoscopy. Br J Dermatol. 2009;160:220–2. doi: 10.1111/j.1365-2133.2008.08937.x. [DOI] [PubMed] [Google Scholar]
- 64.Lee DY, Park JH, Lee JH, Yang JM, Lee ES. The use of dermoscopy for the diagnosis of plantar wart. J Eur Acad Dermatol Venereol. 2009;23:726–7. doi: 10.1111/j.1468-3083.2009.03184.x. [DOI] [PubMed] [Google Scholar]
- 65.Nirmal B, George R, Kodiatte TA. Dermatoscopy of palmar wart with falooda seed appearance. Australas J Dermatol. 2018;59:155–6. doi: 10.1111/ajd.12676. [DOI] [PubMed] [Google Scholar]
- 66.Tanioka M, Nakagawa Y, Maruta N, Nakanishi G. Pigmented wart due to human papilloma virus type 60 showing parallel ridge pattern in dermoscopy. Eur J Dermatol. 2009;19:643–4. doi: 10.1684/ejd.2009.0781. [DOI] [PubMed] [Google Scholar]
- 67.Arpaia N, Filotico R, Mastrandrea V, Cassano N, Vena GA. Acral viral wart showing a parallel ridge pattern on dermatoscopy. Eur J Dermatol. 2009;19:381–2. doi: 10.1684/ejd.2009.0670. [DOI] [PubMed] [Google Scholar]
- 68.Kim WJ, Lee WK, Song M, Kim HS, Ko HC, Kim BS, et al. Clinical clues for differential diagnosis between verruca plana and verruca plana-like seborrheic keratosis. J Dermatol. 2015;42:373–7. doi: 10.1111/1346-8138.12760. [DOI] [PubMed] [Google Scholar]
- 69.Hui D, Hong-Yan J, Ai-E X. Evaluation of verruca plana by in vivo reflectance confocal microscopy and dermoscopy. Skin Res Technol. 2017;23:437–40. doi: 10.1111/srt.12336. [DOI] [PubMed] [Google Scholar]
- 70.Lacarruba F, Verzi AE, Dinotta F, Micali G. Cutaneous and anogenital warts. In: Micali, editor. Atlas of Pediatric Dermatoscopy. Springer. 2018. p. 35. [Google Scholar]
- 71.Kim SH, Seo SH, Ko HC, Kwon KS, Kim MB. The use of dermatoscopy to differentiate vestibular papillae, a normal variant of the female external genitalia, from condyloma acuminata. J Am Acad Dermatol. 2009;60:353–5. doi: 10.1016/j.jaad.2008.08.031. [DOI] [PubMed] [Google Scholar]
- 72.Brown J, Janniger CK, Schwartz RA, Silverberg NB. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93–9. doi: 10.1111/j.1365-4632.2006.02737.x. [DOI] [PubMed] [Google Scholar]
- 73.Ianhez M, Cestari Sda C, Enokihara MY, Seize MB. Dermoscopic patterns of molluscum contagiosum: A study of 211 lesions confirmed by histopathology. An Bras Dermatol. 2011;86:74–9. doi: 10.1590/s0365-05962011000100009. [DOI] [PubMed] [Google Scholar]
- 74.Zaballos P, Ara M, Puig S, Malvehy J. Dermoscopy of molluscum contagiosum: A useful tool for clinical diagnosis in adulthood. J Eur Acad Dermatol Venereol. 2006;20:482–3. doi: 10.1111/j.1468-3083.2006.01480.x. [DOI] [PubMed] [Google Scholar]
- 75.Vázquez-López F, Kreusch J, Marghoob AA. Dermoscopic semiology: Further insights into vascular features by screening a large spectrum of nontumoral skin lesions. Br J Dermatol. 2004;150:226–31. doi: 10.1111/j.1365-2133.2004.05753.x. [DOI] [PubMed] [Google Scholar]
- 76.Lacarrubba F, Verzì AE, Micali G. Newly described features resulting from high-magnification dermoscopy of tinea capitis. JAMA Dermatol. 2015;151:308–10. doi: 10.1001/jamadermatol.2014.3313. [DOI] [PubMed] [Google Scholar]
- 77.Knopfel N, del Pozo LJ, Escudero Mdel M, Martin-Santiago A. Dermoscopic visualization of vellus hair involvement in tinea corporis: A criterion for systemic antifungal therapy? Pediatr Dermatol. 2015;32:e226–7. doi: 10.1111/pde.12648. [DOI] [PubMed] [Google Scholar]
- 78.Gomez-Moyano E, Crespo-Erchiga V, Martinez Pilar L, Martinez Garcia S. Correlation between dermoscopy and direct microscopy of morse code hairs in tinea incognito. J Am Acad Dermatol. 2016;74:e7–8. doi: 10.1016/j.jaad.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 79.Isa R, Amaya B, Pimentel M, Arenas R, Tosti A, Cruz A. Dermoscopy in tinea capitis: A prospective study on 43 patients. Med Cutan Iber Lat Am. 2014;42:18–22. [Google Scholar]
- 80.Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2013;27:509–13. doi: 10.1111/j.1468-3083.2011.04323.x. [DOI] [PubMed] [Google Scholar]
- 81.Gomez-Moyano E, Crespo-Erchiga V. Tinea of vellus hair: An indication for systemic antifungal therapy. Br J Dermatol. 2010;163:603–6. doi: 10.1111/j.1365-2133.2010.09811.x. [DOI] [PubMed] [Google Scholar]
- 82.Gomez-Moyano E, Crespo-Erchiga V, Leandro-Martinez P, Silvestre-Martinez G, Martin-Gonzalez T, Godoy-Diaz DJ, et al. Using dermoscopy to detect tinea of vellus hair. Br J Dermatol. 2016;174:636–8. doi: 10.1111/bjd.14085. [DOI] [PubMed] [Google Scholar]
- 83.Ankad BS, Sakhare PS. Dermoscopy of borderline tuberculoid leprosy. Int J Dermatol. 2018;57:74–6. doi: 10.1111/ijd.13731. [DOI] [PubMed] [Google Scholar]
- 84.Ankad BS, Sakhare PS. Dermoscopy of histoid leprosy: A case report. Dermatol Pract Concept. 2017;7:63–5. doi: 10.5826/dpc.0702a14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zacherle BJ, Silver DS. Hot tub folliculitis: A clinical syndrome. West J Med. 1982;137:191–4. [PMC free article] [PubMed] [Google Scholar]
- 86.Errichetti E, Stinco G. Dermoscopy: A useful tool for assisting the diagnosis of Pseudomonas folliculitis. An Bras Dermatol. 2016;91:835–6. doi: 10.1590/abd1806-4841.20165382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lockwood LL, Gehrke S, Navarini AA. Dermoscopy of pitted keratolysis. Case Rep Dermatol. 2010;2:146–8. doi: 10.1159/000319792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Almazan-Fernandez FM, Fernandez-Crehuet Serrano P. Trichomycosis axillaris dermoscopy. Dermatol Online J. 2017;23:15. [PubMed] [Google Scholar]
- 89.Guiotoku MM, Ramos PM, Miot HA, Marques SA. Trichobacteriosis: Case report and dermosocpic study. An Bras Dermatol. 2012;87:315–6. doi: 10.1590/s0365-05962012000200023. [DOI] [PubMed] [Google Scholar]
- 90.Hu R, Queen CM, Zouridakis G. Lesion border detection in Buruli ulcer images. In annual international conference of the IEEE Engineering in Medicine and Biology Society (EMBC), IEEE. 2012:5380–3. doi: 10.1109/EMBC.2012.6347210. [DOI] [PubMed] [Google Scholar]
- 91.Durdu M, Errichetti E, Eskiocak AH, Ilkit M. High accuracy of recognition of common forms of folliculitis by dermoscopy: An observational study. J Am Acad Dermatol. 2019;81:463–71. doi: 10.1016/j.jaad.2019.03.054. [DOI] [PubMed] [Google Scholar]
- 92.Miyashita K, Ogawa K, Iioka H, Miyagawa F, Okazaki A, Kobayashi N, et al. Adult case of staphylococcal scalded skin syndrome differentiated from toxic epidermal necrolysis with the aid of dermoscopy. J Dermatol. 2016;43:842–3. doi: 10.1111/1346-8138.13281. [DOI] [PubMed] [Google Scholar]
- 93.Sonthalia S, Tiwary P. Colored dots on trichoscopy-beware of artifacts. J Am Acad Dermatol. 2019;80:e143–4. doi: 10.1016/j.jaad.2018.11.052. [DOI] [PubMed] [Google Scholar]
- 94.Rather PA, Hassan I. Human Demodex mite: The versatile mite of dermatological importance. Indian J Dermatol. 2014;59:60–6. doi: 10.4103/0019-5154.123498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coates SJ, Thomas C, Chosidow O, Engelman D, Chang AY. Ectoparasites: Pediculosis and tungiasis. J Am Acad Dermatol. 2020;82:551–69. doi: 10.1016/j.jaad.2019.05.110. [DOI] [PubMed] [Google Scholar]


