A 68-year-old male presented with a 6-month history of a pruritic eruption on the lower extremities. Examination showed multiple papulonodules with central umbilication and firmly adherent keratotic plugs on the extensor surfaces of the legs, predominantly on the right side [Figure 1a and b]. No mucosal lesions were noted. Besides pruritus, the review of systems was innocent for any other associated symptomatology. The patient had been prescribed high potency topical corticosteroids 1 month before, with no significant improvement. His medical history was irrelevant and the patient denied similar complaints in close contacts. General condition was normal. Routine laboratory investigations, including extended biochemistry and autoimmunity, were within normal limits or negative. Skin biopsy showed a well-demarcated crater-like ulcer filled with a thick plug containing fragments of keratin, numerous neutrophils, and transepidermal elimination of degenerated collagen fibers. The underlying dermis exhibited a mixed inflammatory infiltrate of lymphomononuclear cells, occasional neutrophils, and plasma cells [Figure 2a and b]. These findings were consistent with acquired perforating dermatosis. At this point, colchicine 1 mg twice daily was added to the topical corticosteroid. The lesions rapidly improved, with a very significant reduction of the pruritus, subsiding a residual postinflammatory hyperpigmentation after 2 months of treatment [Figure 3].
Figure 1.

Papulonodules with (a) central umbilication on the right leg and (b) closer view of the keratotic plugs (b)
Figure 2.
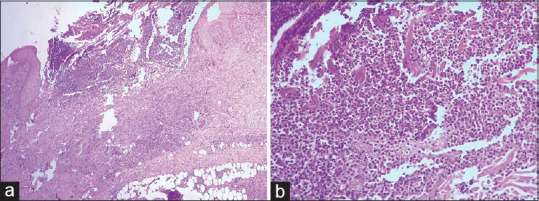
Histological examination with prominent transepidermal defect containing celular debris (a) (H and E, 40×) and higher magnification of the plug, with fragments of keratin, numerous neutrophils, and arrows signaling elimination of degenerated collagen fibers (b) (H and E, 100×)
Figure 3.

Resolution of the papulonodules with postinflammatory hyperpigmentation after 2 months of treatment with colchicine
Perforating dermatoses are a group of uncommon conditions characterized by transepidermal elimination of dermal material (collagen, elastic tissue, or necrotic connective tissue), divided into primary and secondary forms.[1] Primary perforating dermatoses include idiopathic, distinct entities such as elastosis perforans serpiginosa, reactive perforating collagenosis, perforating folliculitis, and Kyrle's disease.[2] A secondary form is acquired perforating dermatosis (APD), characterized clinically by severely pruritic hyperkeratotic papules and nodules, sometimes umbilicated, typically on the hair-bearing limbs of adults, and histopathologically by transepidermal elimination of various substances such as keratin, collagen, and elastic fibers.[1,3] Pruritus is the most prominent feature, and Koebner phenomenon can be observed occasionally.[1,2]
APD arises in adulthood, usually in association with diabetes mellitus or chronic renal failure, but has also been reported in patients with malignant, hepatic and endocrinological disorders, HIV infection, tuberculosis, pulmonary aspergillosis, neurodermatitis, atopic dermatitis, and scabies, although it may develop in patients without any medical problem.[2,3]
Although the pathogenesis of APD is still uncertain, microtrauma, in predisposed patients, can trigger transepidermal elimination and degeneration of the collagen fibers.[4] In addition, insufficient blood supply as a result of microangiopathy may contribute to collagen damage and local inflammatory reactions. Leukocyte infiltration seems to be a predisposing factor for focal necrobiosis of tissue.[2] Increased intralesional TGF-ß3 expression and increased intralesional fibroblast activity have been demonstrated in APD.[5,6]
The differential diagnosis includes prurigo nodularis, folliculitis, arthropod bites, multiple keratoacanthomas, psoriasis, and lichen planus.[1] Diagnostic criteria have been proposed: histopathologic findings of elimination of necrotic basophilic collagen bundles into a cup-shaped epidermal depression, umbilicated papules or nodules with a central adherent keratotic plug, and onset of the lesions after 18 years of age.[7]
No therapy for APD is supported by the results of clinical trials.[8] The most commonly used treatment options are topical and intralesional steroids, topical and oral retinoids, and antihistamines.[9] Phototherapy may be helpful for pruritus. Cryotherapy, surgical debridement, and laser therapy have been reported, as well as allopurinol, doxycycline, hydroxychloroquine, dapsone, and methotrexate.[1,5] An important requirement is the management of any associated internal or oncological disease.[5]
The exact mechanisms of action of colchicine remain largely unclear. Current results suggest that colchicine downregulates multiple inflammatory pathways and modulates innate immunity. Colchicine inhibits microtubule formation and interferes with leukocyte migration, adhesion, and degranulation.[10,11] Besides the strong antiinflammatory properties, colchicine also has antifibrotic activities and various effects on endothelial function.[11] Colchicine has increasingly been recognized as a safe and effective treatment for a wide range of cutaneous disorders and novel applications are being explored in dermatology and other fields.[10]
We present the first report of the successful use of colchicine in APD. We speculate that the antiinflammatory and antifibrotic properties of this drug might be of use in this disease. Although none of the typical precipitants of APD was elicited in this particular case, the patient remains under clinical surveillance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lynde C, Pratt M. Acquired perforating dermatosis: Association with diabetes and renal failure. CMAJ. 2009;181:615. doi: 10.1503/cmaj.082013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hinrichs W, Breuckmann F, Altmeyer P, Kreuter A. Acquired perforating dermatosis: A report on 4 cases associated with scabies infection. J Am Acad Dermatol. 2004;51:665–7. doi: 10.1016/j.jaad.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 3.Saray Y, Seckin D, Bilezikci B. Acquired perforating dermatosis: Clinicopathological features in twenty-two cases. J Eur Acad Dermatol Venereol. 2006;20:679–88. doi: 10.1111/j.1468-3083.2006.01571.x. [DOI] [PubMed] [Google Scholar]
- 4.Hong SB, Park JH, Ihm CG, Kim NI. Acquired perforating dermatosis in patients with chronic renal failure and diabetes mellitus. J Korean Med Sci. 2004;19:283–8. doi: 10.3346/jkms.2004.19.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner G, Sachse MM. Acquired reactive perforating dermatosis. J Dtsch Dermatol Ges. 2013;11:723–9. doi: 10.1111/ddg.12131. [DOI] [PubMed] [Google Scholar]
- 6.Fernandes KA, Lima LA, Guedes JC, Lima RB, D'Acri AM, Martins CJ. Acquired perforating dermatosis in a patient with chronic renal failure. An Bras Dermatol. 2016;91:10–3. doi: 10.1590/abd1806-4841.20164619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faver IR, Daoud MS, Su WP. Acquired reactive perforating collagenosis.Report of six cases and review of the literature. J Am Acad Dermatol. 1994;30:575–80. doi: 10.1016/s0190-9622(94)70065-6. [DOI] [PubMed] [Google Scholar]
- 8.Lukács J, Schliemann S, Elsner P. Treatment of acquired reactive perforating dermatosis-A systematic review. J Dtsch Dermatol Ges. 2008;16:825–42. doi: 10.1111/ddg.13561. [DOI] [PubMed] [Google Scholar]
- 9.Lo YP, Snehal D, Deng LH, Chang CH, Shih CJ. Successful treatment of acquired reactive perforating collagenosis induced by pregnancy with allopurinol: A case report with review of literature. Dermatol Sin. 2019;37:162–5. [Google Scholar]
- 10.Robinson KP, Chan JJ. Colchicine in dermatology: A review. Australas J Dermatol. 2018;59:278–85. doi: 10.1111/ajd.12795. [DOI] [PubMed] [Google Scholar]
- 11.Leung Y, Hui L, Kraus V. Colchicine - Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45:341–50. doi: 10.1016/j.semarthrit.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


