Abstract
Introduction
Although cash transfer programmes are not explicitly designed to improve mental health, by reducing poverty and improving the life chances of children and young people, they may also improve their mental health. This systematic review and meta-analysis assessed the evidence on the effectiveness of cash transfers to improve the mental health of children and young people in low-income and middle-income countries.
Methods
We searched Pubmed, EBSCOhost, Scientific Electronic Library Online, ISI Web of Science and Social Sciences Citation Index and grey literature (from January 2000 to July 2020) for studies which quantitatively assessed the impact of cash transfers on mental health in young people (aged 0–24 years), using a design that incorporated a control group. We extracted Cohen’s d effects size and used a random-effects model for the meta-analysis on studies that measured depressive symptoms, I2 statistic and assessment of study quality.
Results
We identified 12 116 articles for screening, of which 12 were included in the systematic review (covering 13 interventions) and seven in the meta-analysis assessing impact on depressive symptoms specifically. There was high heterogeneity (I2=95.2) and a high risk of bias (0.38, 95% CIs: −5.08 to 5.85; p=0.86) across studies. Eleven interventions (85%) showed a significant positive impact of cash transfers on at least one mental health outcome in children and young people. However, no study found a positive effect on all mental health outcomes examined, and the meta-analysis showed no impact of cash transfers on depressive symptoms (0.02, 95% CIs: −0.19 to 0.23; p=0.85).
Conclusion
Cash transfers may have positive effects on some mental health outcomes for young people, with no negative effects identified. However, there is high heterogeneity across studies, with some interventions showing no effects. Our review highlights how the effect of cash transfers may vary by social and economic context, culture, design, conditionality and mental health outcome.
Keywords: health policy, systematic review, child health, mental health & psychiatry, health economics
Key questions.
What is already known?
Poverty increases vulnerability to mental health problems in children and young people in low-income and middle-income countries.
Prior reviews have examined the impact of cash transfers on the mental health of adults, but none have specifically considered a broad range of mental health outcomes in children and young people.
What are the new findings?
This review, which focused on children and young people, shows that cash transfers may positively impact mental health, with no evidence of negative effects on mental health.
There was significant heterogeneity across studies and mental health outcomes.
What do the new findings imply?
The heterogeneity found across studies suggests that the effects of cash transfers are likely to depend on the social, cultural and economic context in which they are implemented, as well as on their design and the role of conditionality.
There is a need for high-quality randomised controlled trials that assess the impact of poverty reduction interventions on mental health in children and young people.
Introduction
Poverty, defined based on a range of social and economic indicators that capture multiple forms of deprivation,1 2 affects approximately 663 million3 children and young people in low/middle-income countries (LMICs), with potential detrimental effects on their physical and mental health.4–8 Existing frameworks suggest that there is a ‘vicious cycle’ whereby poverty increases the risk of mental illness, while mental illness increases the risk of future poverty.9 Since the late 1990s, cash transfer programmes emerged as a promising approach to reduce poverty, by providing financial resources to alleviate poverty in households, while at the same time stimulating behavioural change and human capital investment.10–12 Cash transfers may be unconditional, which refer to money transfers without any actions required from beneficiaries; or conditional, where money is transferred to beneficiaries that meet specific behavioural requirements. As both conditional and unconditional cash transfer programmes became widespread in many LMICs,13 studies have been conducted to examine their effects on multiple outcomes, such as education, health and nutrition, with some studies showing positive effects,10 12 while others show null or negative effects.14 15
Cash transfer programmes aim to improve outcomes associated with poverty, such as education, health and nutrition.10 16 Although not explicitly designed to improve mental health, there are several mechanisms through which they may also impact the mental health of children and young people living in poverty. Cash transfers increase household income and may thus directly reduce financial strain and increase economic security. They may reduce family conflict associated with poverty and financial stress, thus reducing mental health risks for all family members. Cash transfers may also reduce child labour and related exposures that place young people at risk of mental health disorders. On the other hand, these programmes often involve relatively small cash benefits, which may be insufficient to generate changes in mental health. Improvements in the financial situation of the household may not translate into quality of life improvements for children and young people, thus having limited effects on their mental health. In addition, conditional cash transfers may increase family stress associated with the pressure to meet conditionalities.
Studies on the impact of cash transfers have typically focused on key targeted outcomes such as educational attainment and healthcare use.10 16 Only recently, studies have started to examine the impact of cash transfers on mental health, but the evidence has so far been mixed.8 17 18 While some studies suggest that conditional cash transfers increase psychological distress,19 other studies suggest that they may have positive effects on mental health,20 by increasing social support, reducing exposure to domestic violence and improving physical health. Few studies have assessed their impact on the mental health of children and young people (ages 0–24 years), with most studies focusing on adults.21 Focusing on young people is important because most mental health problems have their origin in adolescence or early adulthood.22 In addition, an extensive literature suggests that mental health problems during adolescence may have profound negative impacts on their educational, social and economic outcomes as they reach adulthood.23 24 Therefore, cash transfers during this period may be critical to breaking the cycle of poverty and mental health that emerges later in life.
A review by Lund and colleagues in 201118 identified only five studies from 2007 to 2009 and concluded that their effect on mental health was mixed. Pega and colleagues concluded that there was insufficient evidence to state that unconditional cash transfers had an impact on depression among children and adults in LMICs.25 However, this review was restricted to studies that measured depressive symptoms only and had the main goal to assess broader results on health services use and health outcomes, rather than mental health specifically. In a recent review of 37 studies, McGuire and colleagues26 reported a positive impact of cash transfers on mental health and well-being, while Ridley and colleagues9 reported positive effects on mental health in a review of 12 cash transfer studies. However, these reviews focused mostly on adults, and no recent review has focused on children and young people in LMICs.
This systematic review and meta-analysis was conducted as part of the CHANCES-6 study, which focuses on understanding the relationship between poverty interventions, mental health and the life chances of children and young people in six LMICs.27 The primary objective of this study was to review the literature on the effect of cash transfers programmes on the mental health of children and young people (0–24 years old) in LMICs. The secondary objective was to understand whether different types of cash transfer programmes have different effects on children and young people’s mental health.
Methods
This review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines,28 and pre-registered on PROSPERO (CRD42020168227).
Inclusion criteria
Our focus was on quantitative studies that assessed the effect of a cash transfer intervention on mental health outcomes in children and young people. We only included papers that reported interventions taking place in an LMIC, as defined by the World Bank at the time the study was published. Studies were included if published in any language from 2000 to the present, as most cash transfer programmes started in the late 1990s and few studies on their impact on mental health were published before 2000.
Intervention
Interventions were only deemed appropriate for inclusion if they (a) were ‘targeted’ anti-poverty interventions, defined as anti-poverty policies that strive to target poor people as the direct beneficiaries to reduce monetary poverty (income or consumption poverty) and/or some dimension of poverty (eg, education, employment or housing materials) and (b) involved a direct cash transfer, such as and including: conditional and unconditional cash transfers, microfinance, loans, debt management and economic streghthening using matched savings. Saving-led economic strengthening interventions differ from traditional cash transfers in that the amount of money transferred depends on how much participants save, whereas, in traditional cash transfer programmes, families do not have to save any money to receive cash transfers. The money from matched-savings interventions is often a smaller amount compared with cash transfers and is typically directed towards specific purposes such as education and family micro-enterprise development.
Outcomes measures
Studies were considered if they included a measure of: (a) mental health or well-being from parent-reported or self-report questionnaires; (b) a biomarkers associated with mental health (eg, salivary cortisol measures of stress) or (c) diagnoses of mental health conditions, as defined by the WHO International Classification of disease (ICD-11), from either parent-report or self-report questionnaires or psychiatric diagnosis from a medical professional. Mental health and well-being outcomes included but were not limited to symptoms or diagnoses of: mood disorders; anxiety disorders; post-traumatic stress disorder (PTSD); substance-related disorders; feeding and eating disorders; psychotic disorders; personality disorders; behavioural problems; self-esteem; confidence; resilience; self-efficacy; future outlook and hopefulness. Studies were only included if they provided a direct comparison of mental health outcomes for treatment and control groups or pre-intervention and post intervention outcomes.
Participants
As this review aimed to assess the effect of cash transfer interventions on the mental health of children, adolescents and young adults, we only included studies that included an estimate of the impact on mental health for those below 25 years. Given the limited literature on the impact of cash transfers on mental health, we wanted to make sure to include all mental health outcomes for all ages of children and young people. We included programmes where children were either direct beneficiaries (ie, programmes targeted to children) or where they were members of a household that received a transfer (ie, household included at least one person receiving a transfer).
Study design
We included studies that compared cash transfers to an explicit control group, including individual or cluster randomised controlled trials (RCTs) and non-randomised evaluations involving both a control and treatment group. To assess the impact of cash transfers over time, we only included longitudinal studies (with a control group).
Exclusion criteria
Cross-sectional studies and studies that did not include a control group were excluded. We excluded those that did not provide a statistical comparison of interventions, or pre-intervention and post intervention outcomes for non-RCTs. We also excluded studies on interventions that did not involve a cash transfer, even if they involved in-kind transfers, such as food or relief nutrition, employment and educational interventions.
Search strategy
Academic databases
We searched published peer-reviewed journal articles and working papers in the following electronic databases from 2000 to the present: Pubmed (Medline and PubMed Cochrane Central), EBSCOhost (Econlit, the Cumulative Index to Nursing and Allied Health Literature, PsycINFO, Africa Wide Information, Medline), the Scientific Electronic Library Online, ISI Web of Science and Social Sciences Citation Index. We used Medical Subject Heading (MeSH) terms or similar thesaurus/indexing terms in databases that do not use MeSH. We also searched using non-MeSH/other index terms, for recent articles without MeSH/other indexing terms yet, and for articles with misspelt MeSH/other indexing terms. An extensive list of all MeSH and non-MeSH search terms for each concept and database included in the final search is detailed in online supplemental material 1. We screened the reference lists of all included studies and contacted authors of included studies and recent relevant systematic reviews9 25 26 for additional relevant publications.
bmjgh-2020-004661supp001.pdf (207.6KB, pdf)
Grey literature and working papers
We conducted a separate structured search through the EconPapers database via Research Papers in Economics that catalogues journal articles and working papers. In addition, we conducted a specific structured search of Google Scholar between 2000 and 2020. The search strategy was based on similar reviews of the effect of cash transfer interventions on health,12 25 29 and included key terms related to ‘mental disorders’ (including specific disorders, listed above) and ‘mental wellbeing, ‘cash transfer schemes’, ‘low- and middle-income countries’ and ‘randomized controlled trials’.
Post hoc backward and forward citation search
In January 2021, following Cochrane standards,30 we conducted backward and forward citation searches using a manual approach via Google Scholar on all included studies and relevant systematic reviews.9 25 26 This involved assessing reference lists from all studies, and all papers that have since cited these studies.
Selection strategy
The screening tool Covidence was used for the screening and management of articles. Two reviewers (AZ and EG) screened study eligibility and irrelevant peer-reviewed articles were excluded based on title and abstract, while DMD and A-LP screened the titles and abstracts generated from the grey literature search. Full-text articles were subsequently reviewed by AZ and EG to determine eligibility for data extraction. Before proceeding to the full-text review and the data extraction stages, any disagreements on eligibility were discussed and resolved by mutual consent, in consultation with a third author (CL). Reviewers only proceeded to the next stage once 100% agreement was reached. Non-English language papers were only translated after the title and abstract had been tested for inclusion by authors fluent in the language.
Where multiple articles reported data from the same study population, the article with the most comprehensive data was used in the analysis. In cases where the articles reported on the same intervention but with different timeframes or subgroups (eg, by sex or age), all articles were included.
Data extraction
Data extraction was conducted by two reviewers (AZ and EG) using an adapted version of the Cochrane Public Health Group’s data extraction form,31 which was expanded for the intervention perspective involved in this review. The reviewers checked and resolved all discrepancies between their data extraction forms. Details of data extraction can be found in the online supplemental material 1.
Assessment of risk of bias
To assess study quality of RCTs, we used the Cochrane Collaboration’s ‘Risk of Bias’ tool.32 Reviewers judged the overall risk of bias based on a fixed set of domains focusing on different aspects of study design, including selection bias, performance bias, detection bias, attrition bias, reporting bias and other source of bias including misclassification, confounding and reverse causation. Each domain was assigned to have a high, low or unclear risk of bias. The same tool was used for non-RCTs, which were ranked as high risk for selection bias. We used Egger’s test to assess publication bias.33
Data analysis and narrative synthesis
First we used narrative synthesis to present a qualitative report on the effect of cash transfer interventions on mental health outcomes in children and young people. We assessed whether groups of studies differed in relation to outcome, design, conditionality (unconditional vs conditional), age groups (older vs younger children), cash volume, beneficiary (children vs caregiver/household) and country.
Meta-analysis
As there was high heterogeneity between the mental health outcomes used, we decided a priori to only run the meta-analysis on studies that measured the same mental health outcome. A meta-analysis was performed where more than four studies measured the same mental health outcome. Thus, we carried out a meta-analysis on studies that measured depressive symptoms. Seven of the nine interventions that measured depressive symptoms were suitable for inclusion in the meta-analysis. All analyses were conducted using Stata V.16. We converted association parameters and SD into Cohen’s d effect sizes (ES), defined as:
where Ỹt and Ỹc are the mean outcomes of the treatment and control groups, respectively, and Sp is the mean SD from the treatment and control groups. For most studies, the outcome means were not reported and instead the unstandardised treatment effect is reported as a treatment effect parameter estimate; in these cases, D reflects the unstandardised treatment effect estimate.
In studies where the SDs were not reported, SEs were used to calculate SD. When the SEs were not reported, CIs were used to calculate SEs, using the formula:
Heterogeneity was assessed using standardised effect sizes to calculate the I² statistic and χ2 tests. Due to heterogeneity between studies, we used a random-effects approach and performed sensitivity analyses. In the first sensitivity analysis, we excluded studies that were not RCTs; in the second, we excluded studies that were economic strengthening interventions, which involved smaller cash transfers with the aim of encouraging savings using matched savings accounts. Finally, we ran a random-effect meta-regression analysis to evaluate factors (sample size, country, cash volume, programme duration, design or conditionality) that could account for heterogeneity between studies of depressive symptoms only, based on a 5% significance level (p<0.05). Pooled effect sizes for depressive symptoms were then estimated.
Results
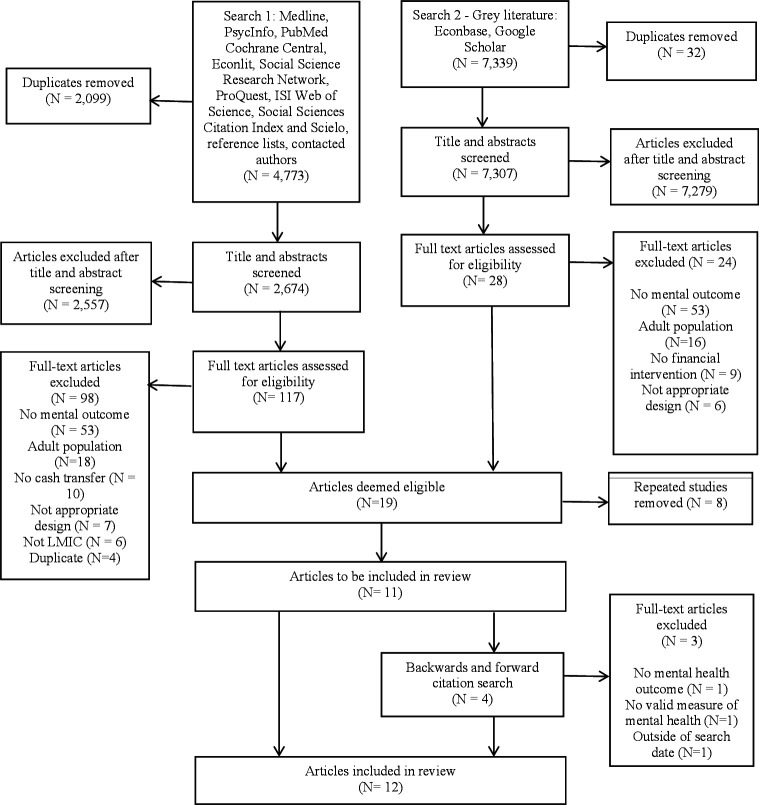
The search of academic databases yielded 4773 papers published in English, Spanish, French and Portuguese, of which 13 were eligible for inclusion in the review (figure 1). In addition, the second search yielded 7339 papers retrieved from the grey literature, of which four studies were included in the review. The backwards and forwards citation searches yielded four papers, of which one was eligible for inclusion in the review. All searches combined resulted in a total of 19 articles on 13 different interventions in nine countries.
Figure 1.
Study selection. LMIC, low/middle-income country.
Where the same intervention and outcomes were reported multiple times, only one paper was included in the analysis. There were six papers generated from the Bridges to Future Intervention in Uganda,34–39 including one paper by Tozan et al,39 which summarised all results from the previous papers, and thus was the only one included in the analysis. Two papers reported on Kenya’s Cash Transfer Programme for Orphans and Vulnerable Children40 41 and both reported the same outcomes in adolescents. We chose to include Kilburn et al40 in the analysis, as they reported the effect size of the cash transfer on depressive symptoms. Two papers presented findings from Atención, a crisis cash transfer in Nicaragua with identical outcomes, so the later one was included (Marcos et al., 2011). Two papers were from the cash transfer programme Oportunidades in Mexico, both were included as they measured different mental health outcomes: behavioural problems42 and cortisol responses to stress.43 Two papers reported the same outcomes from the same interventions in Malawi44 45 and the later paper by Baird et al45 was included as this paper also included longer-term mental health outcomes.
Thus, 12 articles were included in the review, reporting on 13 interventions, as one paper assessed two different interventions (one conditional and one unconditional).45 The key details of each study are listed in table 1. Overall, the included studies involved 43 861 participants from Latin American or African regions: two in Mexico,42 43 Malawi45 46 and Kenya,40 47 and one in Uganda,39 Liberia,48 Ecuador,49 Nicaragua,50 South Africa51 and Cambodia.52 All studies were published in 2007 or later. Eight papers focused on adolescents and young adults aged 11–22 years and four focused on younger children under 5 years. Follow-up varied between 1 and 10 years. Nine studies were cluster or individual RCTs and four were non-randomised evaluations.
Table 1.
Summary of study designs. Age range given where mean age is not provided
| Country | Design | Mean age (years) | Participants | Intervention and control | Conditionality | Mental health outcome | Follow-up (years) | Transfer amount (US$) | |
| Angeles et al46 | Malawi | Cluster RCT | 15–22 | Families defined as ‘ultra-poor’ or labour constrained (n=1336 households) |
Intervention: Malawi Social Cash Transfer Programme Transfer (n=652) Control: no transfer (n=640) |
Unconditional | Center for Epidemiologic Studies Depression Scale: (CES-D-10) | 2 | Variable based on households’ size and composition |
| Baird et al45 | Malawi | Cluster RCT | 15.3 | School-age girls in the low-income Zomba District (n=2049) | Intervention: conditional cash transfer (n=46 enumeration areas) or unconditional cash transfer (n=27 enumeration areas). Control: no transfer (n=15 enumeration areas) |
Conditional (80% school attendance) and unconditional (identical with no requirements on school attendance) | Psychological distress (anxiety, depressive symptoms and social dysfunction): General Health Questionnaire 12 (GHQ-12) | 5 | $1–5 per month to girls $4–10 per month to caregivers |
| Fernald and Gunnar43 | Mexico | Quasi-experimental | 4.0 | Children in households in low-income communities (n=1197) | Intervention: Oportunidades (n=554) Control: no transfer (n=762) |
Conditional: compliance with school and clinic requirements | Baseline and responsivity salivary cortisol | 3.5 | Equivalent to approximentely 20% increase of household income |
| Filmer and Schady52 | Cambodia | Quasi-experimental | 14.0 | Families of children selected for a scholarship (n=3800 scholarships) | Intervention: Scholarship programme cash transfer (n=missing) Control: no transfer (n=missing) |
Conditional: enrollment, regular attendance and satisfactory grade progress | Psychological distress: General Health Questionnaire (GHQ-12) | 1.5 | $45 or $60 three times per year |
| Kilburn et al40 | Kenya | Individual RCT | 16.8 | Poor families taking care of orphans and vulnerable children (n=1540 households) | Intervention: Kenya’s Cash Transfer Programme for Orphans and Vulnerable Children (n=1408). Control: non-cash transfer households from the same sub-location, and non-cash transfer households from a different sub-location control (n=598) |
Unconditional | Depressive symptoms: CES-D-10 | 4 | $10 per month |
| Kilburn et al51 | South Africa | Cluster RCT | 15.5 | Young women between 13 and 20 years old enrolled in high school in low-income study location (n=2537) | Intervention: HIV Prevention Trials Network 068 which provided transfers to young women and their parents (n=1272) Control: no transfer (n=1261) |
Conditional: 80% school days attendance | Depressive symptoms: CES-D-20 Power in relationships: 12-item sexual relationship power scale Hopefulness: 13-item Hope scale |
1–3 | $20 per month |
| Macours et al50 | Nicaragua | Cluster RCT | 3–7 | Children in low-income households between 0 and 83 months (n=4245) | Intervention: Atención a Crisis cash transfer with three arms: cash transfer, cash transfer with vocational training and business skills training, and cash transfer with lump-sum payment toward business development (n=3002 households) Control: no transfer or training (n=1019 households) |
Conditional on regular health check-ups for children ages 0–5 | Behavioural Problems Index Social-personal subscale of the Denver Developmental Screening Test |
0.8 | 15% of per capita expenditures |
| Özler et al48 | Liberia | Quasi-experimental | 13.7 | Adolescent girls and caregivers (n=84 villages, with 1216 eligible girls and 1132 caregivers). | Intervention: Girl Empower (GE), which provides a life skills curriculum to girls (n=393). The GE+ variation includes a cash incentive payment to caregivers for girls’ participation in the programme (n=400) Control: no transfer or programme (n=383). |
Unconditional | Self-esteem: 10-item Rosenberg Scale, Depressive symptoms and anxiety: 12-item Short Mood of Feelings Questionnaire PTSS: Children’s Revised Impact of Event Scale |
2 | $2 per month to girls, $1.25 per month to caregivers |
| Ozer et al42 | Mexico | Cluster RCT | 5.2 | Low-income households (n=506 communities) | Intervention: Oportunidades (n=778) Control: no transfer (n=263) |
Conditional; prenatal care, baby care, immunisation, nutrition monitoring and supplementation, and participation in health, hygiene and nutrition education | Behavior Problems Index | 3–5 | $130 (equivalent to appox. 20% increase of household income) every 2 months |
| Paxson and Schady49 | Ecuador | Quasi-experimental | 3.3 | Families with children in the lowest poverty index quintiles with at least one child under the age of 6 and no children ages six or above (n=17 987) | Intervention: Bono de Desarrollo Humano (n=1479) Control: not offered the Bono until several years later (n=384) |
Unconditional | Behavioural problems: Woodcock, Johnson Muñoz, Mccarthy tests Behavioural problems | 2 | $15 per month |
| Shangani et al47 | Kenya | Individual RCT | 14.2 | Low-income households with at least one orphaned and vulnerable child under 17 years (n=665 from 300 households) | Intervention: Kenya’s Cash Transfer Programme for Orphans and Vulnerable Children (n=231). Control: non-cash transfer households from the same sub-location, and non-cash transfer households from a different sub-location Control (n=424) |
Unconditional | Anxiety: 28-item Children’s Manifest Anxiety Scale–Revised Depressive symptoms: 11-item Child Depression Inventory (CDI) PTSS: 28-item PTSD checklist Future outlook: single item question |
3 | $20 per month |
| Tozan et al39 | Uganda | Cluster RCT | 12.0 | Children who identified as an AIDS orphan (lost one or both parents to AIDS); living within a family (broadly defined and not an institution or orphanage); and enrolled in grades 5–6 in a public primary school in the study region. (n=48 primary schools, 1410 children) |
Intervention: Bridges to the Future (n=487) and Bridges to the Future PLUS (n=396). Economic strengthening and asset accumulation with savings matched on 1:1 rate (Bridges) or 2:1 rate (Bridges PLUS). Control: usual care services for school-going AIDS-affected children in the region (n=500) |
Unconditional | Depressive symptoms: 27-item Child Depression Inventory and the 20-item Beck Hopelessness Scale. Self-concept: 20-item Tennessee Self-Concept Scale and the 29-item Youth Self-Efficacy Survey. | 4 | Bridges: 1:1 matched savings Bridges PLUS: 2:1 matched savings |
PTSD, post-traumatic stress disorder; PTSS, post-traumatic stress syndrome; RCT, randomised controlled trial.
There were 11 cash transfers programmes40 42 43 45–47 49–52 and two economic strengthening programmes that matched savings in Uganda and Liberia.39 48 Of the 13 interventions, six were conditional42 43 45 50–52 and seven were unconditional.39 40 45–49
A range of mental health outcomes were assessed among the 13 programmes, nine of which measured depressive symptoms or psychological distress,39 40 42 45–48 51 52 four anxiety,9 31 32 three psychological well-being39 47 51 (including future outlook, well-being, self-concept/esteem and hopefulness), three childhood social or behavioural functioning,42 49 50 two PTSDs,47 48 one hopelessness39 and one stress.43 These outcomes were largely assessed using self-report questionnaires by the child/youth or sometimes by the caregiver in studies of younger children. One study assessed stress using biomarkers.43
Quality of bias assessment
The quality rating of each study is detailed in table 2. We judged the overall risk of bias to be moderately high. The key issues were lack of randomisation and blinding. Allocation concealment and blinding are not feasible for cash transfer studies as adult participants are aware of whether they receive the cash transfer or not, although arguably many children and adolescents may not be aware as the transfer is made to the parents. Selective reporting was often unclear due to lack of published protocols. Several studies were classified as high risk on other sources of bias due to issues involving outcome (eg, number of cortisol measurements), lack of controlling for potential confounders for non-randomised controlled studies,43 use of non-validated questionnaires to measure mental health outcomes39 42 47 48 or exclusion of children with older siblings.49 Egger’s test for studies included in the meta-analysis did not show a significant publication bias (0.38, 95% CIs: −5.08 to 5.85; p=0.86).
Table 2.
The quality rating of each study based on the Cochrane risk of bias assessment
| Random sequence generation | Allocation concealment | Blinding (participants and personnel) | Blinding (outcome assessment) | Incomplete outcome data | Selective reporting | Other sources of bias | |
| Angeles et al46 | Unclear | Unclear | High risk | Unclear | Low risk | Low risk | Low risk |
| Baird et al45 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Low rIsk |
| Fernald and Gunnar43 | High risk | High risk | Unclear | Unclear | Unclear | High risk | High risk |
| Filmer and Schady52 | High risk | High risk | Unclear | Unclear | Low risk | Unclear | Low risk |
| Kilburn et al40 | Unclear | Unclear | Low risk | Unclear | Low risk | Unclear | Low risk |
| Kilburn et al51 | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear |
| Macours et al50 | Low risk | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk |
| Özler et al48 | Unclear | Low risk | Unclear | Unclear | Low risk | Low risk | High risk |
| Ozer et al42 | High risk | High risk | Unclear | Unclear | Low risk | Low risk | High risk |
| Paxson and Schady49 | High risk | High risk | Unclear | Unclear | High risk | Unclear | High risk |
| Shangani et al47 | High risk | High risk | Unclear | Unclear | Unclear | Low risk | High risk |
| Tozan et al39 | Unclear | Unclear | Unclear | Unclear | Unclear | Low risk | High risk |
The mental health effects of these interventions are summarised in table 3. A total of 11/13 (85%) of interventions reported a significant positive effect on at least one measure of mental health,39 40 42 43 45–47 50–52 including one which had a poor quality rating,49 while only two studies, both of which were quasi-experiments found no effect on any measure.48 49 Of the seven studies39 42 45 47 50 51 that measured multiple outcomes, all reported mixed effects of the intervention, with none reporting a positive effect on every mental health outcome. No studies reported a negative effect on mental health.
Table 3.
Summary of study outcomes included in review. Findings are unadjusted as presented in the paper and CIs are only included where reported. Effect sizes presented are mean change in outcome
| Change in effect | Psychological distress and depressive symptoms | Psychological well-being | Social/behavioural functioning | |
| Angeles et al46 | Improved | Depressive symptoms (−2.05, p<0.01) and depressive symptoms (−0.15, p<0.01) | ||
| Baird et al45— Conditional | Improved (psychological distress) | Reduction psychological distress (−0.07, SE=0.03, p<0.05) | ||
| Baird et al45—Unconditional | Improved (psychological distress) | Reduction in psychological distress (−0.14, SE=0.05, p<0.01) | ||
| Fernald and Gunnar43 | Improved | Effect on salivary cortisol (−0.12, 95% CI: −0.19 to –0.05; p<0.0001) | ||
| Filmer and Schady52 | Improved | Effect onpsychological distress (0.03, SE: 0.01, p<0.01) | ||
| Kilburn et al40 | Improved | Effect on depressive symptoms (0.79, 95% CI: 0.63 to 0.99; p<0.01) | ||
| Kilburn et al51 | Not improved (depressive symptoms) Improved (power in sexual relationships and hopefulness) in poorest women |
No effect on depressive symptoms (−0.02, SE: 0.03, p>0.05) | Effect on sexual relationship power scores (0.28, SE=0.10, p<0.01), greater hope (0.14, SE: 0.07, p<0.05) in poorest women | |
| Macours et al50 | Improved (socio-emotional functioning) Not improved (behavioural problems) |
Effect of intervention on socio-personal outcomes (0.10, SE: 0.05, p<0.01) No effect on behavioural problems (−0.02, SE: 0.06, p>0.05) |
||
| Özler et al48 | Not improved | No effect on psychosocial outcomes (0.24, SE: 0.64, p>0.05) | ||
| Ozer et al42 | Not improved (anxiety/ depressive symptoms or total effects) Improved (aggressive/ oppositional problems) |
No effect on anxiety/depressive symptoms (−0.29, 95% CI: −0.70 to 0.13; p=0.18) or total symptoms (−0.71, 95% CI: −1.42 to 0.01; p=0.05) | Effect on aggressive/oppositional problems (−0.42, 95% CI: −0.80 to −0.04; p=0.03) | |
| Paxson and Schady49 | Not improved | No effect on behavioural problems (0.11, SE: 0.06, p>0.05) | ||
| Shangani et al47 | Not improved (depressive symptoms) Improved (PTSS, anxiety and future outlook) |
Effect on anxiety (0.57, 95% CI: 0.42 to 0.78; p<0.001), and PTSS (0.50, 95% CI: 0.29 to 0.89; p<0.01). No effect on depressive symptoms (0.77, 95% CI: 0.47 to −1.27, p>0.05) |
Effect on positive future outlook (1.47, 95% CI: 1.08 to 1.99; p<0.01) | |
| Tozan et al39 | Not improved (depressive symptoms) Improved (self-concept, self-efficacy and hopelessness) |
Effect on depressive symptoms (−0.14, 95% CI: −0.32 to 0.03; p=0.10) | Effect on self-concept (0.26, 95% CI: 0.09 to 0.44; p<0.05), self-efficacy (0.26, 95% CI: 0.09 to 0.43; p<0.01) and hopelessness (−0.28, 95% CI: −0.43 to −0.12; p<0.05) |
Of the 10 interventions that measured depressive symptoms, five—of which four were unconditional and one was conditional, and all but one52 were conducted in Africa—reported positive small to large effects (Cohen’s d ranging from 0.02 to 0.76)40 45 46 52 and five—of which three were conditional, two were unconditional and one was conducted in South America—reported no effect.39 42 47 48 51 Two of the studies that reported no effect were matched savings programs,39 48 rather than traditional cash transfers, and the study by Özler and colleagues48 used a quasi-experimental design.
Of the four that measured anxiety,45 47 48 three cash transfer studies—of which one was conditional and two were conditional—reported a positive, small effect (Cohen’s d ranging from 0.06 to 0.28)45 47 and the matched-savings study reported no effect.48 All were conducted in Africa. Of the three studies that measured psychological well-being,39 47 51 all three reported positive small to large effects (Cohen’s d ranging from 0.26 to 0.80). One was unconditional, one was conditional and one was an unconditional matched-savings intervention and all were conducted in Africa. Of the three studies that measured social/behavioural functioning42 49 53 two reported a small positive effect (Cohen’s d ranging from 0.10 to 0.4242 50 and one found no effect,49 although one study used a quasi-experimental design and has a poor quality rating, hence results may indicate bias.
Out of all of the six conditional interventions,42 43 45 50–52 all six reported a positive effect on at least one mental health outcome (Cohen’s d ranging from 0.02 to 0.77), and of the seven unconditional interventions,39 40 45–49 five reported a positive effect on at least one mental health outcome (Cohen’s d ranging from 0.10 to 0.80). Hence, when compared across conditionality, a greater percentage of conditional intervention studies reported a positive effect (100%) than unconditional intervention studies (71%). Likewise, a greater percentage of conditional interventions45 52 (2/3—67%) reported a positive impact on depressive symptoms, compared with unconditional interventions40 45 46 (3/7—43%). By contrast, only one study explicitly compared outcomes between conditional and unconditional cash transfer programmes.45 This study found that unconditional interventions had a greater positive impact on psychological distress than conditional ones. However, effects of both programmes disappeared at the 5-year follow-up after the cash transfer had stopped.45
There were nine studies that reported specific cash volume. Of the three studies with a transfer of $20 per month or higher,42 47 51 all three (100%) reported at least one significant positive effect. In comparison, three40 45 of the five studies (60%) with transfers lower than $20 per month40 45 48 49 reported a positive effect.
Of the five studies in which children were beneficiaries,39 45 48 51 four (80%) reported a positive effect on mental health.39 45 51 Of the seven in which household/caregivers were the beneficiaries,40 42 46 47 49 50 52 six (86%) reported a positive result.40 42 46 47 50 52
Meta-analysis
Seven of the 10 interventions that measured depressive symptoms were suitable for inclusion in the meta-analysis.39 40 42 46–48 51 The two conditional and unconditional programmes reported by Baird et al45 and the study by Filmer and Schady52 could not be included as individual sample sizes in each group were not provided, nor were effect sizes.
Results from the meta-analysis indicated a positive, but non-significant effect of interventions on depressive symptoms: the pooled Cohen’s d effect size from the effects of cash transfer schemes on depressive symptoms was (0.02, 95% CI: −0.19 to 0.23; p=0.85), ranging from −0.24 to 0.40 (figure 2). However, 95% of the variation across estimates was due to heterogeneity between studies (I²=95.2). This suggests that treatment effect differences across studies are not random, which compromises the validity of the summary estimate.
Figure 2.
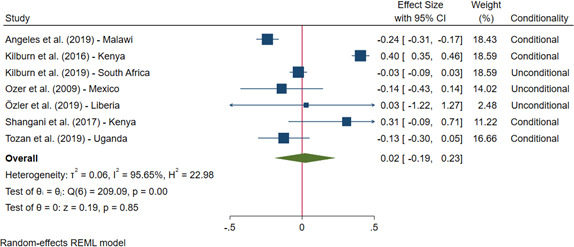
Forest plot comparing studies which used Cohen’s d to assess the effect of cash transfers on depressive symptoms in young people. While the effect size is negative, reflecting a positive impact of the CT on reducing depression is non-significant.
The meta-regression analysis revealed that none of the factors considered on their own (sample size, country, cash volume, programme duration, design or conditionality) explained the high heterogeneity. To remove heterogeneity across studies, we ran a series of sensitivity analyses with subgroups. The first was conducted only among RCTs. A second sensitivity analysis was run among studies that were traditional cash transfers, which involved excluding the two economic strengthening programmes.39 48 The exclusion of these studies did not change the conclusion of the primary meta-analyses (data not shown). We also ran subgroup analyses comparing conditional51 54 and unconditional39 40 46–48 studies. The analysis had no significant subgroup effect (X2=0.38, p=0.54). However, with only two studies contributing to the conditional subgroup, it is unlikely that this analysis can be interpreted with confidence.
Discussion
This study aimed to review the literature on the impact of cash transfers programmes on the mental health of children and young people in LMICs. Twelve articles, which assessed the impact of 13 programmes, were included in the review and narrative synthesis, and seven studies were included in the meta-analysis to assess the effect of cash transfers on depressive symptoms specifically.
Results from the narrative synthesis suggest that cash transfer programmes may improve some mental health outcomes in children and young people. In particular, 11 of 13 (85%) evaluations reported a positive effect on at least one measure of mental health in children and young people. On the other hand, the meta-analysis suggests that cash transfers had no effect on depressive symptoms among children and young people, although the small number of studies and high heterogeneity precludes firm conclusions, and no study found an effect on all mental health outcomes. It is important to note that studies found either positive effect or null effects but none found negative effects on mental health. This is important for policymakers, showing that there is no evidence of negative consequences of cash transfers for the mental health of children and young people. Our findings suggest that social protection programmes can have a positive impact on mental health of young people. Benefits may be optimised through cross-collaboration, such as linking mental health interventions with cash transfers.
While there does not seem to be any difference in findings of studies in which children were beneficieries, as findings were comparable to studies where caregivers with beneficiaries, the volume of cash transferred does seem to be important. Our narrative synthesis showed 100% of studies with transfers at $20 or higher per month reported a positive effect on mental health, whereas only 60% of studies with transfers lower than $20 reported a positive effect. In the meta-analysis, one of the two studies that reported no effect on mental health was a matched-savings programme,48 in which the volume of cash transferred each month for matched-savings programme is often very small ($2), compared with $10–20 per month in traditional cash transfer programmes.39 40 47 51 Further research should investigate whether the impact of cash transfers on youth mental health differs with cash volume, as this has important implications for policy. Policy decisions about the amount, duration and administration of cash transfers could also influence mental health, and optimising their role might benefit from cross-sectoral collaboration. Our findings support recent recommendations27 for relatively low-cost policy changes, such as cash volume, targeting and predictability and duration of payments, which could enhance the mental health impacts of cash transfers for young people.
This review demonstrates the need for research into studies understanding the effects of the conditionality of cash transfers on mental health outcomes. Earlier studies that have directly compared conditional versus unconditional programmes suggest that conditional cash transfers have larger impacts for education, health and nutrition outcomes.13 Research also suggests that conditional cash transfers may be more appropriate in Latin America, and less appropriate in African contexts.55 In contrast, we found that both conditional and unconditional programmes can have positive effects on mental health, but there were null findings from studies in both categories. Except for one study in Malawi,45 none of the studies explicitly incuded multiple arms that directly compared conditional and unconditional transfers. In the one study that did,45 unconditional transfers had a slightly greater positive impact on psychological distress than conditional transfers, but results vanished for both interventions 5 years after the programme had stopped. The majority of conditional cash transfer studies were from Central and South America, whereas studies on unconditional cash transfers and economic strengthening programmes were conducted in Africa. Overall, more research is needed to isolate the impact of conditional and unconditional cash transfer programmes on mental health.
While our findings suggest cash transfers may positively impact the mental health of young people, the meta-analysis found a null effect on depressive symptoms. This is likely to reflect heterogeneity across studies, programmes or regions.
Several differences across both study methods and programme designs may have contributed to the heterogeneity observed in our study. In terms of differences in methods, sample sizes, trial design (cluster, individual RCTs, quasi-experimental), outcomes and outcome measures (eg, self-report, clinician assessed, biomarkers) varied across studies. In terms of differences in the intervention, the amount of money received ranging from $2 to $20 a month, seven studies involved conditionalities, while seven were unconditional cash transfers, and the age of populations studied ranged from 3 to 22 years.48 51
Notewithstanding potential methodological explanations, the heterogeneity across studies may also reflect genuine differences in the impact of cash transfers on mental health across different countries, cultures and mental health outcomes. Transfers may improve some mental health outcomes but not others—for example, there may be effects on childhood externalising conditions such as oppositional behaviour42 but not on internalising conditions such as depression. Cash transfers may also generate inconsistent results depending on whether they successfully improve underlying socioeconomic conditions and life chances for young people, such as improved educational attainment. It may also be that improvements on education, physical health or life chances alone do not consistently translate into mental health improvements,56 and that more explicit components associated with mental health support are required in order to generate mental health improvements in young people.
Overall, results from this review suggest that cash transfers by themselves may not be a magic bullet to improve mental health in children and young people living in poverty, and that effects might be very different for different countries, conditionality, volume of cash, age and mental health outcome. While this was beyond the scope of the current paper, further understanding of the mechanisms by which cash transfers influence mental health is necessary to understand whether these inconsistencies in findings reflect inconsistent effects on mental health, or inconsistent effects on the mechanisms by which changes to mental health occur. For instance, addressing the indirect mechanisms of cash transfers improving mental health through increasing household income, and directly through reducing child labour is an important area for future research.
Our findings reflect that this is a relatively young field of research which still requires considerable attention. While nearly 10 000 titles and abstracts were screened, only 13 papers were eligible for inclusion in this review, despite a our broad inclusion criteria. While there has been an increase in the number of RCTs assessing cash transfers in LMICs since the review in 2011,18 there is a clear need for high-quality randomised controlled trials of poverty reduction interventions to incorporate mental health as part of the oucomes assessed.
There are several ways that future studies in this field of research could be improved. First, studies should unpack the mechanisms that link cash transfers to mental health. Given that the mechanisms by which cash transfers affect mental health are currently unclear, further RCTs should seek to address this by exploring whether cash transfers causally impact mental health, and measuring the direct and indirect mechanisms by which changes occur. Second, we recommend that future trials include a conditional and unconditional arm to directly compare the effects of conditionality on mental health among children and young people. Efficiency and administrative costs associated with conditional versus unconditional programmes also need to be considered to inform future policies on poverty reduction and mental health. Third, little qualitative research or process evaluation findings were reported in the papers included in this review. Yet, mixed methods are essential to understand the role of culture and other local, contextual factors. Longitudinal qualitative methods should be applied alongside RCTs to provide in-depth understanding of how cash transfers impact the mental health and stress of recipients and their children. Finally, following recommendations by Pega and colleagues,25 steps must be taken to reduce the risk of bias in the field. Future studies should pre-register protocols to reduce potential selective reporting. It is important that studies provide detailed assessments of the quality of evidence so risk of bias can be reliably assessed.
Strengths of this review include the fact that we reviewed a broad range of academic databases and grey literature, with no restrictions on publication format, period of time or language. However, there are several limitations to this review. For most mental health outcomes, a narrative synthesis was performed as less than four studies measured the same mental health outcome. It was challenging to assess differences across studies of a small number, hence meta-analyses could not be carried out for specific mental health oucomes other than depressive symptoms. The financial poverty reduction schemes assessed in this review may also be heterogeneous in their focus on different aspects of poverty and target beneficiaries. Poverty is complex and multidimensional, and evidence suggests that the strength and direction of the relationship between poverty and mental health differs across poverty dimensions.4 As concluded in the recent review by Pega and colleagues,25 interventions that tackle only one dimension of poverty may not substantially improve mental health, particularly when not targeted to specific subgroups.
Footnotes
Handling editor: Seye Abimbola
Contributors: AZ designed the study, conducted the review and analysis and prepared the manuscript. EG conducted the review and analysis and helped design the study and advise on the manuscript. CL designed the study and supervised the review, analysis and write-up. DMD and A-LP conducted the grey literature review and advised on the manuscript. MA-P and RA supervised the review, analysis and write-up. SEL PH, YD, AM, AB, CSP and CZ helped design the study and all authours red and commented on the the manuscript.
Funding: This study is an output of the CHANCES-6 study. This work was supported by the UKRI’s Global Challenges Research Fund (ES/S001050/1). The support of the Economic and Social Research Council (ESRC) is gratefully acknowledged. MA-P is additionally supported by the ESRC Centre for Society and Mental Health at King's College London (ESRC Reference: ES/S012567/1).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. Data extracted from studies are available directly from published work. Data extraction tables generated for the purposes of this review are available upon request.
References
- 1.Toye JI M. Social inclusion and community economic development: literature review. The Canadian CED Network 2004;4:Cd008137. [Google Scholar]
- 2.Lund C, Cois A. Simultaneous social causation and social drift: longitudinal analysis of depression and poverty in South Africa. J Affect Disord 2018;229:396–402. 10.1016/j.jad.2017.12.050 [DOI] [PubMed] [Google Scholar]
- 3.Unicef . Child poverty UNICEF, 2020. Available: https://www.unicef.org/social-policy/child-poverty
- 4.Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med 2010;71:517–28. 10.1016/j.socscimed.2010.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 6.Ozer EJ, Fernald LCH, Weber A, et al. Does alleviating poverty affect mothers' depressive symptoms? A quasi-experimental investigation of Mexico's Oportunidades programme. Int J Epidemiol 2011;40:1565–76. 10.1093/ije/dyr103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ensminger ME, Hanson SG, Riley AW, et al. Maternal psychological distress: adult sons' and daughters' mental health and educational attainment. J Am Acad Child Adolesc Psychiatry 2003;42:1108–15. 10.1097/01.CHI.0000070261.24125.F8 [DOI] [PubMed] [Google Scholar]
- 8.Hanandita W, Tampubolon G. Does poverty reduce mental health? an instrumental variable analysis. Soc Sci Med 2014;113:59–67. 10.1016/j.socscimed.2014.05.005 [DOI] [PubMed] [Google Scholar]
- 9.Ridley M, Rao G, Schilbach F, et al. Poverty, depression, and anxiety: causal evidence and mechanisms. Science 2020;370:w27157. 10.1126/science.aay0214 [DOI] [PubMed] [Google Scholar]
- 10.Baird S, Ferreira FHG, Özler B, et al. Conditional, unconditional and everything in between: a systematic review of the effects of cash transfer programmes on schooling outcomes. J Dev Effect 2014;6:1–43. 10.1080/19439342.2014.890362 [DOI] [Google Scholar]
- 11.Owusu-Addo E, Renzaho AMN, Smith BJ. The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: a systematic review. Health Policy Plan 2018;33:675–96. 10.1093/heapol/czy020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA 2007;298:1900–10. 10.1001/jama.298.16.1900 [DOI] [PubMed] [Google Scholar]
- 13.Bastagli F, Hagen-Zanker J, Harman L. Cash transfers: what does the evidence say. A rigorous review of programme impact and the role of design and implementation features. ODI Briefing London: Overseas Development Institute, 2016. [Google Scholar]
- 14.Behrman JR. Medium-term impacts of the oportunidades conditional cash transfer program on rural youth in Mexico” 219–70. Discussion papers//Ibero America Institute for Economic Research 2009;122:219–70. [Google Scholar]
- 15.Santos MCS, Delatorre LR, Ceccato MdasGB, et al. Programa Bolsa Família E indicadores educacionais em crianças, adolescentes E escolas no Brasil: revisão sistemática. Ciênc. saúde coletiva 2019;24:2233–47. 10.1590/1413-81232018246.19582017 [DOI] [PubMed] [Google Scholar]
- 16.Leroy JL, Ruel M, Verhofstadt E. The impact of conditional cash transfer programmes on child nutrition: a review of evidence using a programme theory framework. J Dev Effect 2009;1:103–29. 10.1080/19439340902924043 [DOI] [Google Scholar]
- 17.Wahlbeck K, Cresswell-Smith J, Haaramo P, et al. Interventions to mitigate the effects of poverty and inequality on mental health. Soc Psychiatry Psychiatr Epidemiol 2017;52:505–14. 10.1007/s00127-017-1370-4 [DOI] [PubMed] [Google Scholar]
- 18.Lund C, De Silva M, Plagerson S, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet 2011;378:1502–14. 10.1016/S0140-6736(11)60754-X [DOI] [PubMed] [Google Scholar]
- 19.Fernald LCH, Hamad R, Karlan D, et al. Small individual loans and mental health: a randomized controlled trial among South African adults. BMC Public Health 2008;8:409. 10.1186/1471-2458-8-409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaarder MM, Glassman A, Todd JE. Conditional cash transfers and health: unpacking the causal chain. J Dev Effect 2010;2:6–50. 10.1080/19439341003646188 [DOI] [Google Scholar]
- 21.Samuels F, Stavropoulou M. ‘Being able to breathe again’: the effects of cash transfer programmes on psychosocial wellbeing. J Dev Stud 2016;52:1099–114. 10.1080/00220388.2015.1134773 [DOI] [Google Scholar]
- 22.Jones PB. Adult mental health disorders and their age at onset. British Journal of Psychiatry 2013;202:s5–10. 10.1192/bjp.bp.112.119164 [DOI] [PubMed] [Google Scholar]
- 23.Knapp M, King D, Healey A, Thomas C, et al. Economic outcomes in adulthood and their associations with antisocial conduct, attention deficit and anxiety problems in childhood. J Ment Health Policy Econ 2011;14:37–47. [PubMed] [Google Scholar]
- 24.McCrone P, Knapp M, Fombonne E. The Maudsley long-term follow-up of child and adolescent depression. Eur Child Adolesc Psychiatry 2005;14:407–13. 10.1007/s00787-005-0491-6 [DOI] [PubMed] [Google Scholar]
- 25.Pega F, Liu SY, Walter S, et al. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database Syst Rev 2017;11:Cd011135. 10.1002/14651858.CD011135.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGuire J, Kaiser C, Bach-Mortensen A. The impact of cash transfers on subjective well-being and mental health in low-and middle-income countries: a systematic review and meta-analysis. SocArXiv 2020. 10.31235/osf.io/ydr54 [DOI] [PubMed] [Google Scholar]
- 27.Bauer A, Garman E, McDaid D, Aea B, et al. Integrating youth mental health into cash transfer programmes in response to the COVID-19 crisis in low-income and middle-income countries. Lancet Psychiatry 2021:S2215-0366(20)30382-5. 10.1016/S2215-0366(20)30382-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lagarde M, Haines A, Palmer N, et al. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database Syst Rev 2009;67:Cd008137. 10.1002/14651858.CD008137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Briscoe S, Bethel A, Rogers M. Conduct and reporting of citation searching in Cochrane systematic reviews: a cross-sectional study. Res Synth Methods 2020;11:169–80. 10.1002/jrsm.1355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JP, Thomas J, Chandler J, et al., . Chapter 5: collecting data. Cochrane handbook for systematic reviews of interventions. Hoboken: John Wiley & Sons, 2019. [Google Scholar]
- 32.Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ssewamala FM, Ismayilova L. Integrating Children’s Savings Accounts in the Care and Support of Orphaned Adolescents in Rural Uganda. Social Service Review 2009;83:453–72. 10.1086/605941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ssewamala FM, Neilands TB, Waldfogel J, et al. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. J Adolesc Health 2012;50:346–52. 10.1016/j.jadohealth.2011.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han C-K, Ssewamala FM, Wang JS-H. Family economic empowerment and mental health among AIDS-affected children living in AIDS-impacted communities: evidence from a randomised evaluation in southwestern Uganda. J Epidemiol Community Health 2013;67:225–30. 10.1136/jech-2012-201601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karimli L, Ssewamala FM, Neilands TB, et al. Poverty, economic strengthening, and mental health among AIDS orphaned children in Uganda: mediation model in a randomized clinical trial. Soc Sci Med 2019;228:17–24. 10.1016/j.socscimed.2019.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karimli L, Ssewamala FM. Do savings mediate changes in adolescents' future orientation and health-related outcomes? findings from randomized experiment in Uganda. J Adolesc Health 2015;57:425–32. 10.1016/j.jadohealth.2015.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tozan Y, Sun S, Capasso A, et al. Evaluation of a savings-led family-based economic empowerment intervention for AIDS-affected adolescents in Uganda: a four-year follow-up on efficacy and cost-effectiveness. PLoS One 2019;14:e0226809. 10.1371/journal.pone.0226809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kilburn K, Thirumurthy H, Halpern CT, et al. Effects of a large-scale unconditional cash transfer program on mental health outcomes of young people in Kenya. J Adolesc Health 2016;58:223–9. 10.1016/j.jadohealth.2015.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Handa S, Martorano B, Halpern C. The impact of the Kenya CT–OVC on parents' wellbeing and their children. Social Science & Medicine 2014;141:36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ozer EJ, Fernald LCH, Manley JG, et al. Effects of a Conditional Cash Transfer Program on Children’s Behavior Problems. Pediatrics 2009;123:e630–7. 10.1542/peds.2008-2882 [DOI] [PubMed] [Google Scholar]
- 43.Fernald L, Gunnar MR. Effects of a poverty-alleviation intervention on salivary cortisol in very low-income children. Social Sciences and Medicine 2009;68:2180–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. Q J Econ 2011;126:1709–53. 10.1093/qje/qjr032 [DOI] [Google Scholar]
- 45.Baird S CM, Özler B. When the money runs out: evaluating the longer-term impacts of a two year cash transfer program. World Bank Policy Research Working Paper 2016;7901. [Google Scholar]
- 46.Angeles G, de Hoop J, Handa S, et al. Government of Malawi's unconditional cash transfer improves youth mental health. Soc Sci Med 2019;225:108–19. 10.1016/j.socscimed.2019.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shangani S, Operario D, Genberg B, et al. Unconditional government cash transfers in support of orphaned and vulnerable adolescents in Western Kenya: is there an association with psychological wellbeing? PLoS One 2017;12:e0178076. 10.1371/journal.pone.0178076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Özler B, Hallman K, Guimond M-F, et al. Girl Empower - A gender transformative mentoring and cash transfer intervention to promote adolescent wellbeing: Impact findings from a cluster-randomized controlled trial in Liberia. SSM Popul Health 2020;10:100527. 10.1016/j.ssmph.2019.100527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paxson C, Schady N. Does money matter? the effects of cash transfers on child health and cognitive development in rural Ecuador. Washington DC: Processed World Bank, 2008. [DOI] [PubMed] [Google Scholar]
- 50.Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. Am Econ J Appl Econ 2012;4:247–73. 10.1257/app.4.2.247 [DOI] [Google Scholar]
- 51.Kilburn K, Hughes JP, MacPhail C, et al. Cash transfers, young women's economic well-being, and HIV risk: evidence from HPTN 068. AIDS Behav 2019;23:1178–94. 10.1007/s10461-018-2329-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Filmer D, Schady N. School enrollment, selection and test scores: school enrollment, selection and test scores. Washington, DC: The World Bank, 2009. [Google Scholar]
- 53.Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. Washington, DC: Processed World Bank, 2008. [Google Scholar]
- 54.Ozer EJ, Fernald LCH, Manley JG, et al. Effects of a conditional cash transfer program on children's behavior problems. Pediatrics 2009;123:e630–7. 10.1542/peds.2008-2882 [DOI] [PubMed] [Google Scholar]
- 55.Schubert B, Slater R. Social cash transfers in low-income African countries: conditional or unconditional? Development Policy Review 2006;24:571–8. 10.1111/j.1467-7679.2006.00348.x [DOI] [Google Scholar]
- 56.Courtin E, Nafilyan V, Glymour M, et al. Long-term effects of compulsory schooling on physical, mental and cognitive ageing: a natural experiment. J Epidemiol Community Health 2019;73:370–6. 10.1136/jech-2018-211746 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-004661supp001.pdf (207.6KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. Data extracted from studies are available directly from published work. Data extraction tables generated for the purposes of this review are available upon request.