Abstract
A middle-aged woman with diabetes presented with left-sided facial pain, complete ptosis and fever of short duration. On presentation, she had hyperglycaemia without ketosis. There was total ophthalmoplegia of the left eye with a visual acuity of 6/36. She incidentally tested positive for COVID-19. CT paranasal sinus and MRI brain revealed left-sided pansinusitis with acute infarct in the left parieto-occipital region without angioinvasion. An emergency functional endoscopic sinus procedure was done, which confirmed mucormycosis on histopathological examination. After 1 week of conventional amphotericin B and antibiotics, repeat CT brain showed improvement in mucosal thickening and sinusitis. This case is a rare presentation of mucormycosis associated with rapid progression to orbital apex syndrome with brain infarction in a patient with non-ketotic diabetes and COVID-19. Early diagnosis and treatment are essential to prevent further end-organ damage. It is also interesting that there was no angioinvasion and transient periarterial inflammation was attributed to brain infarction.
Keywords: COVID-19, diabetes, tropical medicine (infectious disease), stroke
Background
Mucormycosis is an angioinvasive disease caused by fungi of the order Mucorales like Rhizopus, Mucor, Rhizomucor, Cunninghamella and Absidia. The prevalence of mucormycosis in India is approximately 0.14 cases per 1000 population, about 80 times the prevalence in developed countries.1 COVID-19 infection has been associated with fungal infections. Mucormycosis is more often seen in immunocompromised individuals, and complications of orbital and cerebral involvement are likely in diabetic ketoacidosis and with concomitant use of steroids. The most common risk factor associated with mucormycosis is diabetes mellitus in India.2 In the background of the COVID-19 pandemic, only a limited number of cases of mucormycosis have been reported, but there are no known documented cases of sudden-onset visual loss with incidental COVID-19 infection in a newly detected young non-ketotic diabetic.3
Case presentation
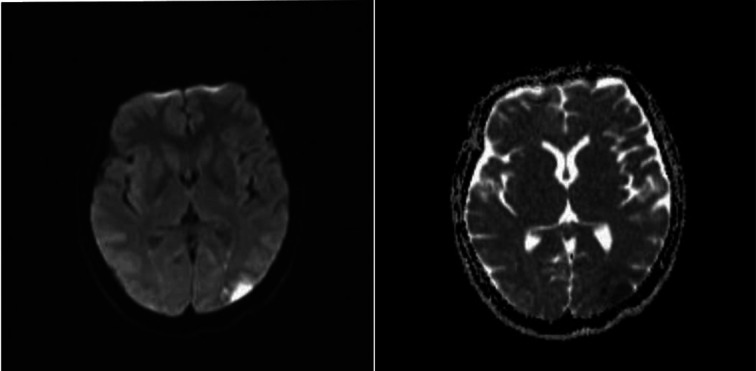
A middle-aged woman, with newly detected diabetes mellitus (haemoglobin A1c: 12.39%), presented with left eye complete ptosis, facial pain for 5 days and preceding fever for 3 days with no symptoms of rhinitis or sinusitis. Clinical examination revealed tenderness of all sinuses on the left side. There was a complete internal and external ophthalmoplegia of the left eye, with absent left eye direct light reflex and left eye visual acuity of 6/36 (figure 1). The right eye movements and vision were normal. The rest of the neurological examination was within normal limits. The patient was afebrile on presentation. Pulse was 78 bpm, blood pressure was 124/80 mm Hg and oxygen saturation was 98% on room air. Systemic examination was unremarkable, and there was no clinical evidence of ketoacidosis.
Figure 1.
Patient presented with left total ophthalmoplegia.
Investigations
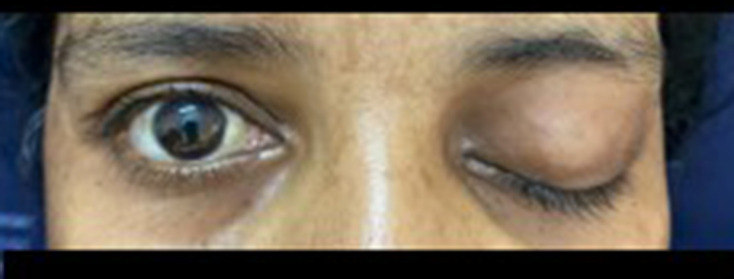
Admission glucose was 378 mg/dL without ketosis. Serum glycated haemoglobin was 12.39%. A CT paranasal sinus showed total opacification of the left ethmoid, maxillary and frontal sinuses (figure 2). An MRI brain showed acute infarct in the left parieto-occipital lobe with a subperiosteal abscess in the superomedial extraconal aspect of the left orbit (figure 3) with thickening and perineural enhancement of the left optic nerve. There was no thrombus in the left internal carotid artery (ICA); however, there was some periarterial inflammation of the left ICA (figure 4). The total leucocyte count was 10.6 × 109/L with a lymphocyte count of 1696 cells/uL. Serial monitoring showed a falling trend of lymphocyte count from 1696 (day 1), to 1246 (day 5), to 924 (day 10), to 666 (day 14) cells/uL. However, CD4 or CD8 testing could not be done. Serum liver biochemistry was within normal limits. Blood urea was 12.3 mg/dL, and serum creatinine was 0.44 mg/dL. The serum electrolytes were within normal limits. She had a B-positive blood type. Inflammatory markers were C reactive protein, 68.35 mg/L (reference range: ≤6 mg/L); procalcitonin, 0.069 ng/mL (reference range: <0.5 ng/mL); D-dimer, 0.80 μg FEU/mL (reference range: <0.5 μg FEU/mL); and serum ferritin, 180.2 mg/dL (reference range for men, 30–400 ng/mL; women, 13–150 ng/mL). She tested positive incidentally for COVID-19 by real-time PCR (nasal and oropharyngeal swab) on day 2 of hospitalisation using TRUPCR SARS-CoV-2 RT qPCR KIT (version 3.2). Chest X-ray (figure 5) was unremarkable, and the patient never required oxygen therapy. She was classified as having a mild COVID-19 infection. Functional endoscopic sinus surgery (FESS) was performed on an emergency basis due to orbital apex syndrome as she fell into group ‘A’ of endonasal surgery indications4 and showed unhealthy, polypoidal mass and slough in the maxillary, anterior and posterior ethmoid sinuses with pus in the frontal sinus and polypoidal mucosa in the sphenoid sinus. Histopathological analysis of the biopsy sample from ethmoid sinus showed fungal colonies of broad aseptate hyphae at an obtuse angle with periodic acid–Schiff stain, which was consistent with mucormycosis. Fungal culture of the sample obtained after sinus debridement in FESS confirmed mucormycosis (Rhizopus species). However, serological fungal markers and fungal culture sensitivity were not tested. The patient was hospitalised for 17 days. Her sugars were well controlled after the initiation of insulin therapy. However, there was no resolution of ophthalmoplegia or ptosis until she was discharged.
Figure 2.

Coronal section of CT paranasal sinus showing left ethmoid sinusitis encroaching on the lamina papyracea.
Figure 3.
Cross-sectional image of MRI brain (DWI and ADC mismatch) showing acute infarct of the parieto-occipital lobe. ADC, apparent diffusion coefficient; DWI, diffusion weighted image.
Figure 4.
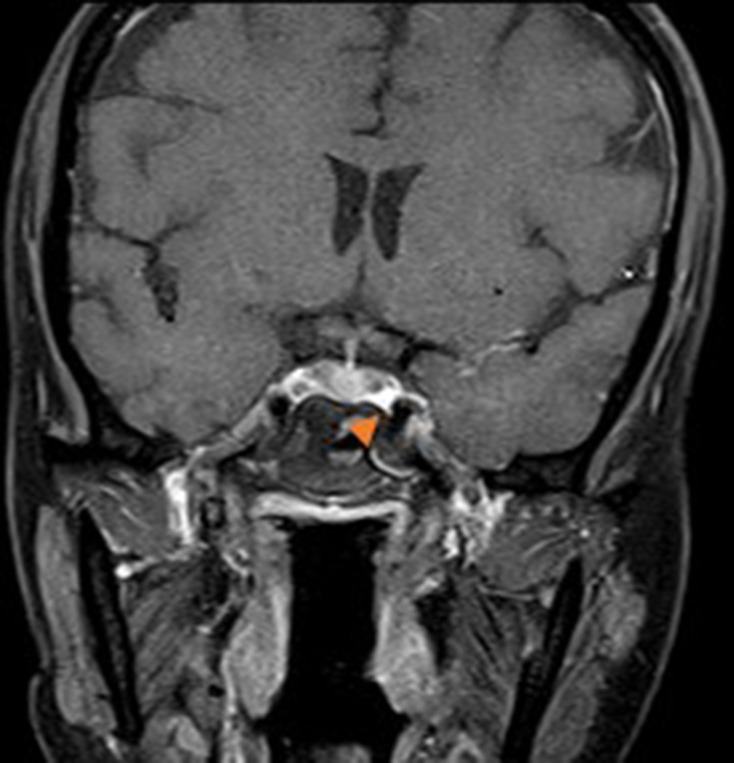
MRI brain showing periarterial inflammation of internal carotid artery (red arrowhead).
Figure 5.
Chest X-ray (PA view). PA, posteroanterior.
Treatment
She was initiated on conventional amphotericin B (given for 11 days) and aspirin for acute cerebral infarct. Post FESS, CT paranasal sinus imaging was done after 1 week of treatment with antifungal therapy and showed a reduction in the diffuse opacification of the left ethmoid, frontal and maxillary sinuses (figure 6).
Figure 6.

Coronal section of CT paranasal sinus showing reduced opacification of the left ethmoid sinus.
Discussion
An active search of literature reviewed few reported rhino-orbitary cases associated with COVID-19.3 5 6 Diabetes mellitus is an independent risk factor for rhino-orbital–cerebral mucormycosis in a meta-analysis of 600 series with 851 cases. The most common species isolated was Rhizopus species, with an overall mortality of 46%.7
A case of COVID-19 with rhino-orbital mucormycosis coinfection associated with ketoacidosis was reported in a patient with recent-onset diabetes mellitus.8 Pathogenic mechanisms involved in fungal aggressiveness include decreased phagocytic activity, accessible amounts of iron due to the displacement of protons by transferrin in diabetic ketoacidosis and fungal heme oxygenase, which promotes iron absorption for its metabolism.
In a case described of severe COVID-19 associated with fungal coinfection, cell counts revealed that there was a progressive increase in white blood cell count and neutrophils while lymphocytes progressively decreased.9 It is hypothesised that SARS-CoV-2 infection may affect CD4+ and CD8+ T-cells, which are highly involved in the pathological process of COVID-19 infection. It has been shown that in severe COVID-19 cases, there is a reduction in the absolute number of lymphocytes and T-cells, which is associated with the worst outcomes. Mucorales-specific T-cells (CD4+ and CD8+) produce cytokines such as interleukin (IL) 4, IL-10, IL-17 and interferon-gamma (IFN-γ) that damage the fungal hyphae. Such specific T-cells were seen only in patients affected by invasive mucormycosis, and they concluded that they could be a useful surrogate diagnostic marker of an invasive fungal disease. It might be speculated that lymphopenia could increase the risk of developing invasive mucormycosis, while the recovery of lymphocyte count could improve the adaptive immune system and induce the production of Mucorales-specific T-cells, which might have a role in controlling the invasive infection.
There are a significant number of reports showing alterations in cell-mediated immunity, such as chemotaxis, phagocytosis and cytokine secretion in both type 1 and type 2 diabetics. Individuals with diabetes have been described to have alterations in innate immune system components. Natural killer cell activity is reduced in individuals with diabetes, and more pro-inflammatory M1 macrophages are present. Furthermore, T-cell activity is skewed. Disease severity in patients is due to not only the viral infection but also the host response. Elevated glucose levels may also suppress the antiviral response. In the context of COVID-19, severe disease progression is described by a delay in IFN-γ response with a prolonged hyperinflammatory state and lower CD4 and CD8 cell numbers. Regardless of the involvement of the endothelial cells, the initial delay in IFN-γ response together with the hyperinflammatory response in individuals with diabetes may exacerbate the ‘cytokine storm’ and increase COVID-19 severity. Increased vascular lesions, endothelial inflammation and vasoconstriction associated with endothelial dysfunction put individuals with diabetes at a greater risk for endotheliitis in several organs. Change of vascular tone towards more vasoconstriction can lead to subsequent organ ischaemia, tissue oedema and a procoagulant state. Finally, dysregulated immune cell populations and activity observed in individuals with diabetes play a critical role in aggravating the severity.10
A case series in the Indian subcontinent reported six cases of rhino-orbital–cerebral mucormycosis following COVID-19 infections.11 The mean duration between the diagnosis of COVID-19 and the development of symptoms of mucormycosis was 15.6±9.6 days. Control of hyperglycaemia, early treatment with liposomal amphotericin B and surgery are essential for the successful management of mucormycosis. Thus, the use of glucocorticoids in mild COVID-19 cases (without hypoxaemia) or the utilisation of higher doses of glucocorticoids should be avoided. Further, in the absence of a clear benefit, drugs targeting immune pathways such as tocilizumab should be discouraged. For successful management of mucormycosis, a high index of clinical suspicion, low threshold for diagnosis in patients with risk factors, neuroimaging and specific diagnostic tests with a coordinated effort from a multidisciplinary team including ophthalmology, otorhinolaryngology, infectious diseases, neurosurgery, critical care, microbiology and pathology department are crucial. A delay of even 6 days in initiating treatment doubles the 30-day mortality from 35% to 66%.11
Simple tests like vision, pupil, ocular motility and sinus tenderness can be part of routine physical evaluation of a patient with COVID-19 hospitalised with moderate to severe infection or diabetics with COVID-19 or those receiving systemic corticosteroids. Visual prognosis, however, continues to remain poor.
Thus, it is important to have a high index of suspicion for fungal coinfection in patients with COVID-19 presenting with comorbidities. Further, they should undergo immediate imaging studies with an emphasis on the requirement of surgical intervention. There is a need to stress on the judicious use of steroids to avoid flaring up of the fungal infection.
Learning points.
This case is an unusual presentation of rapidly developing fungal infection in a patient with non-ketotic diabetes in the background of COVID-19. Severe disease progression in the absence of use of immunosuppressants makes it a rare case.
An alteration in the T-cell population in COVID-19 infection is linked to the pathogenesis of fungal infection.
Early diagnosis and treatment of mucormycosis that involve antifungal therapy and surgical debridement are necessary to reduce mortality and prevent end-organ damage.
Judicial use of immunosuppressive therapy in COVID-19 infection should be considered particularly in regard to treatment of fungal coinfections.
Footnotes
Twitter: @ShwetaMR
Contributors: All four authors were involved in patient care directly. Writing the initial manuscript was done by SMR. Selecting appropriate image templates was done by VVK. The necessary corrections and final outcome of the article were done under the guidance of SPS and LS.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: an update. J Fungi 2020;6:265. 10.3390/jof6040265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prakash H, Chakrabarti A. Global epidemiology of mucormycosis. J Fungi 2019;5:26. 10.3390/jof5010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta S, Pandey A. Rhino-Orbital mucormycosis associated with COVID-19. Cureus 2020;12:e10726. 10.7759/cureus.10726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radulesco T, Verillaud B, Béquignon E, et al. COVID-19 and rhinology, from the consultation room to the operating theatre. Eur Ann Otorhinolaryngol Head Neck Dis 2020;137:309–14. 10.1016/j.anorl.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mekonnen ZK, Ashraf DC, Jankowski T, et al. Acute invasive rhino-orbital mucormycosis in a patient with COVID-19-associated acute respiratory distress syndrome. Ophthalmic Plast Reconstr Surg 2021;37:e40–80. 10.1097/IOP.0000000000001889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med. In Press 2021;42:264.e5–264.e8. 10.1016/j.ajem.2020.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeong W, Keighley C, Wolfe R, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect 2019;25:26–34. 10.1016/j.cmi.2018.07.011 [DOI] [PubMed] [Google Scholar]
- 8.Waizel-Haiat S, Guerrero-Paz JA, Sanchez-Hurtado L, et al. A case of fatal rhino-orbital mucormycosis associated with new onset diabetic ketoacidosis and COVID-19. Cureus 2021;13:e13163. 10.7759/cureus.13163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pasero D, Sanna S, Liperi C, et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection 2020:1–6. 10.1007/s15010-020-01561-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erener S. Diabetes, infection risk and COVID-19; molecular metabolism 39, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sen M, Lahane S, Lahane TP, et al. Mucor in a viral land: a tale of two pathogens. Indian J Ophthalmol 2021;69:244–52. 10.4103/ijo.IJO_3774_20 [DOI] [PMC free article] [PubMed] [Google Scholar]