Abstract
Background:
Both umbilical and epigastric hernias may be associated with rectus muscle divarication. In such cases, isolated repair of combined hernia defects can have high recurrence rates and poorer cosmetic outcomes, thus the repair of both pathologies ought to be favored. The goal of the study below is to provide detailed technical aspects of the endoscopic retro-rectus mesh repair.
Methods:
We chose a group of 16 patients who underwent the repair of ventral hernias associated with both primary and incisional rectus diastasis, using the extended-view of a totally extraperitoneal Rives-Stoppa repair (eRives) technique. All defects were < 6 cm in width. Our outcome measures perioperative complications and early recurrences.
Results:
The approach used in our study has led to zero cases of perioperative complications and only one early recurrence.
Conclusions:
We believe that the e-Rives repair is the optimal approach for ventral hernias associated with diastasis recti. This technique additionally produces favorable cosmetic outcomes that granted our results a well-deserved recognition in the medical literature.
Keywords: Umbilical hernia, Rectus diastasis, Extended-view totally extraperitoneal, eTEP
INTRODUCTION
Both primary and secondary (incisional) umbilical and epigastric hernias are common in adults. Currently, while there is no standardized surgical approach; there is evidence for both suture and mesh-augmented repair.1 Rectus divarication is a reduced consistency and subsequently increased length of intercrossed fibers of the linea alba that separates both aponeuroses of the rectus abdominis muscles.2 However, umbilical or epigastric hernias are associated with rectus diastasis in some cases.3 In these circumstances, the correction of the ventral hernia defect without the proper treatment of the diastasis may lead to an increased risk of recurrence due to the poor quality of the surrounding tissue.4 Approaches to correct both defects are highly variable in the medical literature, including open, minimally-invasive, and hybrid repairs.5
We describe an endoscopic technique for these patients with midline hernias (both primary and incisional) and co-existing rectus divarication. We consider this entity to be a good indication for the extended-view totally extraperitoneal (eTEP) approach repair, a technique that has been recently published by Igor Belyansky, et al.l for the repair of ventral and incisional hernias.6 According to our experience, some cases did not require the performance of the posterior component separation (eTAR), since the transverse parietal defect does not usually exceed 6 cm. Under these circumstances, we rather use the term “eRives” to name the procedure we employ, than the “eTEP approach”, which is a generic term.
METHODS
We retrospectively analyzed all patients with ventral hernias associated with rectus diastasis operated via an endoscopic retromuscular approach. All patients were administered a general anesthesia.
The retromuscular space was approached with the open technique, through the lateral edge of the left rectus abdominal muscle on the umbilical line. A 10 mm camera port was inserted, and CO2 was used to insufflate to a pressure of 12–14 mmHg. The retromuscular space was bluntly dissected with the aid of the camera (a rigid angled laparoscope). Two 5 mm ports were introduced in the same line with the optic port superior and inferior. After dissecting the left retro-rectal space, the midline was crossed in the plane of the falciform ligament, outside the hernia defect. (Figure 1).
Figure 1.
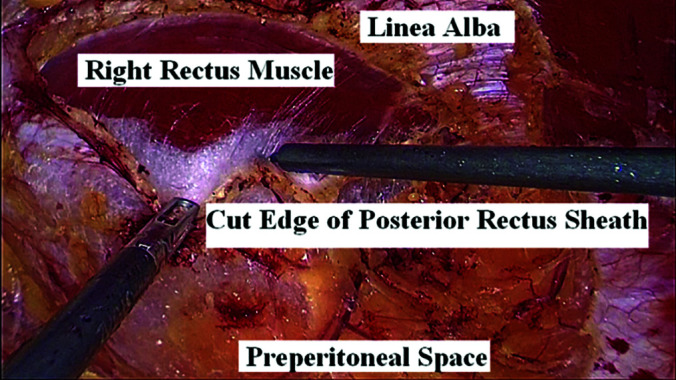
Dissection of the retro-rectus space.
The right side rectus muscle with its sheath was identified and the posterior leaf of the sheath was incised longitudinally on its endo-abdominal surface at 0.5 cm from the medial aspect. The right side retro-rectal space dissection is performed in a similar manner, to the left, being followed by the dissection of the hernia defect (Figure 2).
Figure 2.
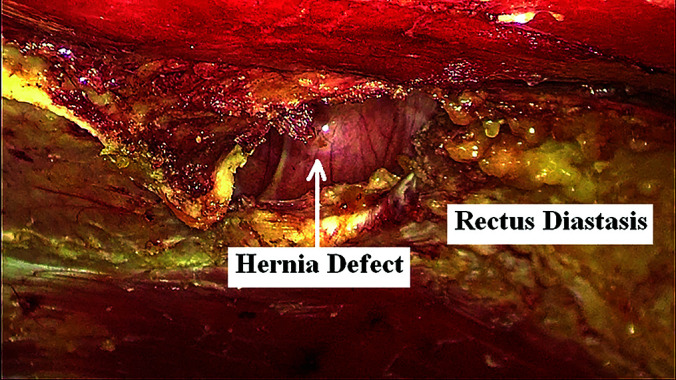
Aspect of hernia defect and diastasis.
During the dissection of the hernia sac, the peritoneal cavity is usually opened without any notable effect on the procedure. In case of small defects, when the protrusion consists of preperitoneal fat, the peritoneum could be maintained closed. The dissection is completed superiorly under the xyphoid process and inferiorly for minimum 5 cm below the defect.
Two more additional trocars were subsequently inserted: a 10 mm port on the midline in the inferior point of dissection and a 5 mm one in the right upper quadrant. All peritoneal leaks were closed using a barbed absorbable suture (V-Loc 2/0) (Figure 3). If the peritoneal defect is large, the closure is done with running suture; if otherwise, with separate points.
Figure 3.
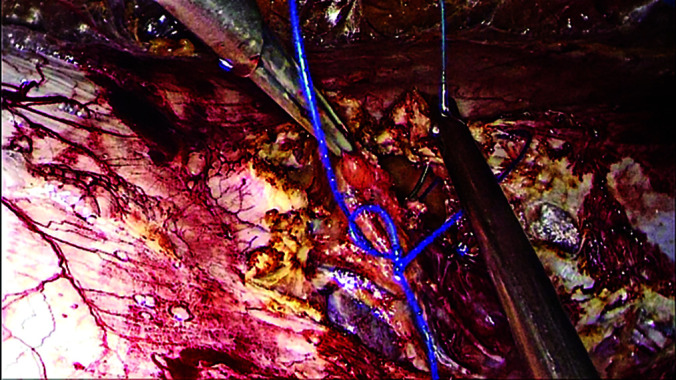
Closure of the posterior layer tears.
The anterior rectus sheath was then closed with the narrowing of the linea alba using a running suture with nonabsorbable barbed suture (V-Loc 0) (Figure 4). The insufflation pressure was dropped to 8 – 9 mmHg, while the anesthetist optimized the muscle relaxation in order to decrease suture tension. The left hand of the operating surgeon gently puts a pressure against the abdominal wall and enhances the application of the surgical sutures.
Figure 4.

Closure of the anterior rectus sheath.
The newly-created retro-muscular space was measured and the mesh was cut to fit the size. The mesh was inserted through the median 10 mm port and arranged in order to keep flat. Usually, the mesh is fixed with one single nonabsorbable 2/0 stitch to the posterior sheath on its upper extremity (Figure 5). Apart from four isolated cases, where the dissection was difficult, no systematic drainage was needed. The final aspect is presented in Figure 6.
Figure 5.
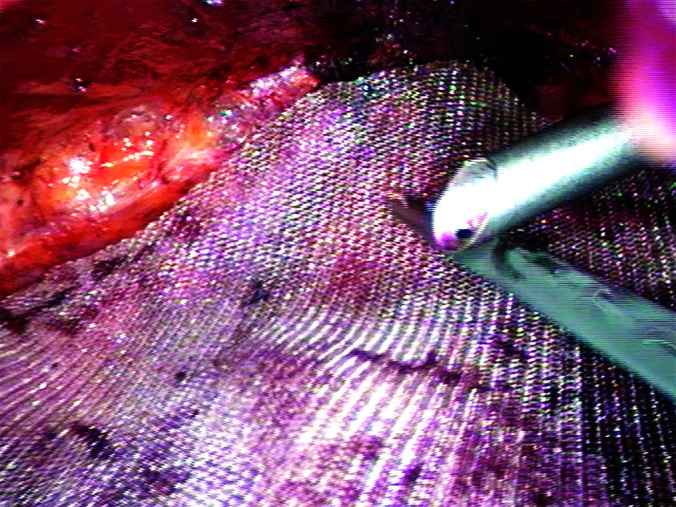
Position of the prothesis.
Figure 6.

Final aspect.
RESULTS
Sixteen patients with associated rectus diastasis and ventral hernias were prospectively evaluated between February 3, 2017 and January 17, 2019. Ten male and six female patients of an age between 39 and 66 years old, formed our cohort study. The operating time ranged from 2 hours and 45 minutes to 5 hours, with 1 to 2 hours for the suture of the anterior sheath. The size of the hernia defect was between 1 and 4 cm, and the maximum size of the diastasis was between 4 and 6 cm, in compliance with the German classification.7
Our preference was for the medium-weight macroporous polypropylene mesh, with dimensions varying between 20 × 12 cm and 35 × 20 cm.
All patients were mobile on postoperative day (POD) 1. The postoperative pain was low, ranging between 1 and 2, in the evening of the procedure, and between 1 and 3 in the POD 1. All patients received nonopioid (Paracetamol) treatment for 1 to 3 days. Patients were typically discharged after an average of 2.53 days (between 1 and 5 days). Patients were able perform their duties after an average of 21 days.
All patients were postoperatively followed up at 1 month, 6 months, and 1 year. There were no postoperative complications, with no disruptions at the level of the diastasis. We had one recurrence at the umbilical level, within six months after surgery. We believe that its occurrence was a result of the prosthesis poorly covering the defect in the lower part.
DISCUSSION
According to the latest Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias,8 the eTEP ventral hernia repair may be used to correct ventral hernias and co-existing diastasis with wide extraperitoneal mesh augmentation and minimal fixation, with favorable early outcomes regarding pain, infection, and recurrence. We applied this technique with caution, avoiding large defects where cosmetic aspect might have suffered.
The procedure combines the advantages of the minimally invasive approaches with retrorectal mesh placement, restoration of the linea alba, avoiding mesh contact with abdominal viscera or subcutaneous space, and offering a wide space with a larger mesh surface.9
The reason we restored the linia alba in these situations was not due to aesthetics, but rather to neccessarily lower the risk of a potential ventral hernia recurrence.
Limitations of the eTEP procedure include prolonged operative time and technical difficulties.9 The suture of the anterior rectus sheath on the roof of the rectus space can be particularly difficult. Based on the gained experience, we concluded that the long duration of the procedure may be reduced especially by decreasing the time to complete the suture of the anterior sheath.
The laparoscopic extraperitoneal approach still sets limitations and ergonomic challenges to both the available degrees of freedom and the significance of the operating surgeon, while requiring extensive technical and minimally invasive surgical expertise for proper execution.10
The position or number of ports as well as the positioning of the operating team may be modified in order to minimize the technical drawbacks.
No additional expenditures were necessary, as this method uses standard laparoscopic instruments and meshes.
Recent studies have found ergonomic benefits in the use of a robotic platform compared to the traditional laparoscopy, while the operative time and intra-operative expenditures have significantly increased.11
Although we did not have a controlled trial, comparing pain scores between our intraperitoneal onlay mesh and eRives patients, we have found that the latter had lower need of analgesics. In these cases,12 this may be due to our application of the minimal fixation outside the peritoneal cavity.
We chose to study the eRives technique only for ventral hernias associated with rectus diastasis in order to have a cohort of patients who were likely to exhibit similar parietal defects. When the abdominal wall defect is larger than 5 or 6 cm in width, the cosmetic result is not so good because of the postoperative occurrence of disturbing protuberances under the skin, after the suture of the midline. We prefer the open approach in cases of ventral hernias associated with a diastasis larger than 6 cm.
We consider that the procedure should consist in the eTEP approach of ventral hernias. After the learning curve has been achieved, more complex cases may be approached.13
CONCLUSIONS
We believe that the eRives procedure is the optimal choice for ventral hernias with associated diastasis recti. The technique should be promoted for its cosmetic results, the reproducibility rate, and for acquiring the principles of modern hernia surgery.
Contributor Information
Doru Moga, Military Hospital Sibiu, Department of Surgery, Romania..
Florin Buia, Military Hospital Cluj-Napoca, Department of Surgery, Romania..
Valentin Oprea, Military Hospital Cluj-Napoca, Department of Surgery, Romania..
References:
- 1. Kohler G, Luketina RR, Emmanuel K. Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg. 2015;39(1):121–126. [DOI] [PubMed] [Google Scholar]
- 2. Bellido Luque J, Bellido Luque A, Valdivia J, et al. Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia. 2015;19(3):493–501. [DOI] [PubMed] [Google Scholar]
- 3. Privett BJ, Ghusn M. Proposed technique for open repair of a small umbilical hernia and rectus divarication with self-gripping mesh. Hernia. 2016;20(4):527–530. [DOI] [PubMed] [Google Scholar]
- 4. Radu VG, Lica M. The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia. 2019;23(5):945–955. [DOI] [PubMed] [Google Scholar]
- 5. Mommers EHH, Ponten JEH, Al Omar AK, et al. The general surgeon's perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc. 2017;31(12):4934–4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Belyansky I, Daes J, Radu VG, et al. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32(3):1525–1532. [DOI] [PubMed] [Google Scholar]
- 7. Reinpold W, Köckerling F, Bittner R, et al. Classification of rectus diastasis – a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg. 2019;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bittner R, Bain K, Bansal VK, et al. Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)). Surg Endosc. 2019;33(11):3511–3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Penchev D, Kotashev G, Mutafchiyski V. Endoscopic enhanced-view totally extraperitoneal retromuscular approach for ventral hernia repair. Surg Endosc. 2019;33(11):3749–3756. [DOI] [PubMed] [Google Scholar]
- 10. Belyansky I, Reza Zahiri H, Sanford Z, Weltz AS, Park A. Early operative outcomes of endoscopic (eTEP access) robotic-assisted retromuscular abdominal wall hernia repair. Hernia. 2018;22(5):837–847. [DOI] [PubMed] [Google Scholar]
- 11. Lu R, Addo A, Ewart Z, et al. Comparative review of outcomes: laparoscopic and robotic enhanced-view totally extraperitoneal (eTEP) access retrorectus repairs. Surg Endosc. 2020;34(8):3597–3605. [DOI] [PubMed] [Google Scholar]
- 12. Baig SJ, Priya P. Extended totally extraperitoneal repair (eTEP) for ventral hernias: short-term results from a single centre. J Minim Access Surg. 2019;15(3):198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moga DF, Buia F, Oprea V. Endoscopic repair of ventral hernia and rectus diastasis. (preprint) https://doi:10.21203/rs.2.11743/v1. [DOI] [PMC free article] [PubMed]


