Abstract
Aim:
This study aims to evaluate the incidence, indications, management, and long term follow up of cholecystectomy in patients with no gallstones, other than acalculous acute cholecystitis.
Methods:
Prospectively collected data of 5675 patients undergoing laparoscopic cholecystectomy (LC) over 28 years was extracted and analyzed. Patients with biliary symptoms, no stones on ultrasound scans and abnormal hepatobiliary iminodiacetic acid scans, and those with confirmed gallbladder polyps (GBP) were included.
Results:
Two percent of cholecystectomies were performed in patients with acalculous pathology [1.3% functional gallbladder disorder (FGBD) and 0.7% GBP]. The 114 patients were younger, had lower American Society of Anesthesiologists classification, and had fewer previous biliary admissions than those with gallstones (5560). The clinical presentations of FGBD were chronic biliary symptoms (93.1%) and acute biliary pain (6.9%). GBP patients presented with chronic biliary symptoms. LC in 98.6% FGBD and 92.8% GBP were significantly easier than those for gall stones (P < 0.0001). They were significantly (P < 0.0001 FGBD and P < 0.001 GBP) less likely to have adhesions to the gallbladder. This ease was reflected in shorter operation times and lower utilization of abdominal drains. Polyp numbers ranged from 1 to 30 and sizes from 1 mm to 11 mm. No malignant polyps were encountered. In 95.8% FGBD and 95% GBP, patients had a good symptomatic response to LC.
Conclusions:
FGBD and GBP are uncommon in patients undergoing LC. FGBD should be considered during evaluation of right upper quadrant pain with no gall stones. Laparoscopic cholecystectomy may be considered as it achieves long term symptomatic relief in most patients with FGBD and GBP.
Keywords: Gallbladder dyskinesia, Functional gallbladder disease, Gallbladder polyps, Laparoscopic cholecystectomy
INTRODUCTION
The incidence of functional gallbladder disorder (FGBD) as an indication for cholecystectomy is reported to range from 3% to 25%.1–3 Gallbladder polyps (GBP) were an indication for cholecystectomy in 14.3% (516 of 3586 patients) in one series in the Republic of Korea. One hundred and two of these patients were eventually found to have cholelithiasis or cholecystitis with the true incidence of gallbladder polyps being 11.5% (414 patients).4
FGBD is an uncommon but important condition to consider in the evaluation of patients with right upper quadrant pain suggestive of a biliary origin. There is no certain etiology of gallbladder (GB) dyskinesia. However, GB muscular hypertrophy might play an important role in decreasing the contractile activity of the smooth muscle of the GB wall. This hypertrophy is suggested to be secondary to chronic inflammation.5
The Rome IV criteria6 for FGBD requires the presence of biliary pain and the absence of gallstones or other structural pathology. The pain must meet specific criteria (e.g., severe enough to interrupt daily activities or lead to a visit to the emergency department). Low gallbladder ejection fraction (GBEF) on hepatobiliary iminodiacetic acid (HIDA) scan, also known as cholescintigraphy, is considered supportive but not diagnostic of FGBD. However, GBEF is helpful in selecting patients who may benefit from cholecystectomy.6 Although most studies use a cut off level of ≤ 35% ejection fraction on the HIDA scan as diagnostic of GBEF,5 some authors suggested a GBEF of ≤ 50%.7
In addition to the GBEF, the contractility of the gallbladder is evaluated during the HIDA scan by intravenous injection of cholecystokinin (CCK) once filling the gallbladder with radioactive tracer occurred. Poor contractility of the gallbladder may result in abdominal pain, which is normally triggered by fatty meals.7
A thorough history is needed to rule out alternative diagnoses such as peptic ulcer disease, functional dyspepsia, and ischemic heart disease. Additional testing for disorders such as sphincter of Oddi dysfunction or chronic pancreatitis will depend on the patient's history, symptoms, laboratory test findings, and imaging test results.
Although the clinical significance of GBP is largely related to malignant potential, they may present with biliary symptoms. Most GBP are non-neoplastic or represent lipid deposits (cholesterolosis). The main risk factor for malignant potential is thought to be a polyp size > 1 cm.8
The aim of this study was to evaluate the incidence, indications, and management of cholecystectomy in symptomatic FGBD and GBP patients who have no gallstones. The secondary aim was to examine the long-term outcomes by reviewing follow up data.
METHODS
Review and analysis of prospectively collected data of patients with FGBD or GBP undergoing laparoscopic cholecystectomy (LC) between February 1, 1992 and September 30, 2019 was conducted.
Patients with biliary symptoms who had no gallbladder stones on ultrasonography and an abnormal HIDA scan suggestive of biliary dyskinesia, as well as those with multiple symptomatic GBP, or those > 10 mm were offered LC. Patients who were referred with incidental GBPs on ultrasound scans were investigated to exclude gatroduodenal pathology and managed accordingly. Those who had single GBPs < 1 cm initially had ultrasound scan follow up every 12 months. However, the hospital protocol for radiological follow up is now limited to multiple polyps and those in patients with symptoms suggestive of a biliary origin. A HIDA scan was considered abnormal if the GBEF was < 35%, if no gallbladder filling occurred, or if abdominal pain was reproduced by injecting CCK intravenously during the scan.
Patients who presented with acute biliary pain were admitted and treated conservatively when ultrasound scans showed no gallstones. HIDA scans were carried out as an outpatient investigation. Those who were confirmed to have FGBD were offered a LC. Occasional patients who presented with jaundice or cholecystitis were thoroughly investigated, with repeat ultrasound, computed tomography scans, or magnetic resonance cholangiopancreatography (MRCP). When these investigations did not reveal a calculous cause of jaundice or pancreatitis, the patients underwent laparoscopic cholecystectomy using the standard four port technique in the American position. In our practice, intra-operative cholangiography is obtained routinely. Nassar scale was used to grade the difficulty of the laparoscopic cholecystectomy.9,10 Abdominal subhepatic drain was placed during the operation in some patients with FGBD and GBPs when indicated (e.g., ruptured gallbladder during dissection, gallbladder adhesions dissected and oozing). The high incidence of utilization of abdominal drains in the whole series was influenced by the large biliary emergency workload and the high proportion of bile duct explorations (23%) on this firm.
Early response to treatment was assessed when the patients attended the outpatient clinic within 3 months. No subsequent routine follow up appointments are made for any of our cholecystectomny patients. Long term follow up of our FGBD and GBP patients between 1 and 23 years was carried out in August 2020 by screening hospital records for any outpatient attendances, in-patient admissions, or radiological investigations suggestive of biliary issues. Any investigations for dyspepsia were scrutinized to exclude associations with FGBD, regardless of the time interval between such episodes and the LC. Dyspeptic symptoms were only considered relevant if they occurred as a continuation of the surgical episodes.
Once a diagnosis of FGBD or GBP was made, patients were offered elective LC and informed consent was obtained with emphasis on the rationale and potential results. Ethical approval was not required as management protocols were in line with the recommendations of national and international societies.
SPSS® Statistics 17 was used for statistical analysis. Welch T-test was used to calculate the significance (P-value < 0.05) for continuous data and χ2 with Yates correction for categorical data.
RESULTS
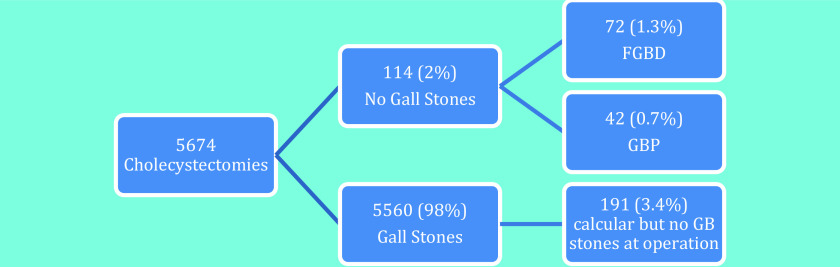
The distribution of the indications for which the 5674 cholecystectomies were performed is illustrated in Figure (1). Two percent of all cholecystectomies were performed in patients who had acalculous pathology (10.3% FGBD and 00.7% GBP). The remainder had undergone pre-operative investigation demonstrating gallstones or were found to have bile duct stones at the time of surgery. This group was therefore considered to have had calculous gallbladder disease.
Figure 1.
Distribution of the calcular and non-calcular cases in 5674 cholecystectomies.
The demographics and pre-operative data for FGBD and GBP are shown in Table (1). The FGBD cohort were younger than that of the gall stone disease group (P < .0001) but the gender distribution was similar. Consequently, the American Society of Anasthetsiologists classification I in the FGBD and GBP patients was more common than in the calculous disease group (P < .0001 and P < .001; respectively).
Table 1.
Demographics and Pre-operative Data
| Demographics/ Pre-operative Data |
|||||
|---|---|---|---|---|---|
| LC for FGBD (n = 72) | LC for GBP (n = 42) | LC for Gallstones (n = 5560) | P-Value Gallstone vs FGBD | P-Value Gallstone vs GBP | |
| Female gender | 60 (83%) | 28 (66.7%) | 4115 (74%) | 0.147 | 0.366 |
| Age mean (SD) | 44 (13) | 49 (11) | 51 (16) | < 0.0001 | 0.227 |
| ASA ASAI ASA II ASAIII ASAIV No record: |
42 (58.3%) 25 (34.7%) 3 (4.1%) 0 (0%) 2 (2.7%) |
22 (52.4%) 15 (35.7%) 3 (7.1 %) 0 (0%) 2 (4.8%) |
1949 (35.1%) 2263 (40.7%) 725 (13.1%) 20 (0.4%) 603 (10.8%) |
< 0.0001 0.386 0.073 0.608 0.068 |
< 0.001 0.426 0.518 0.698 0.405 |
| Previous admission | 2 (2.7%) | 1 (2.3%) | 1290 (22%) | < 0.0001 | 0.003 |
| Previous pre-operative MRCP/ ERCP∼ | 4 (5.6%) | 0 (0%) | 353 (6.3%) | 0.951 | 0.171 |
LC, laparoscopic cholecystectomy; FGBD, functional gallbladder disorder; GBP, gallbladder polyps; SD, standard deviation; ASA, American Society of Anesthesiologists; MRCP, magnetic resonance cholangiopancreatography; ERCP, endoscopic retrograde cholangiopancreatography.
Although patients with FGBD and GBP were investiagted for longer periods pre-operatively, very few previous admission episodes were recorded before their LC when compared to those with gallstone disease (P < .0001 and P = .003; respectively).
Pre-operative MRCP was used on very few occasions in the FGBD group to exclude bile duct stones as it is not part of our routine investigation protocol for suspected ductal stones. MRCP utilization was therefore similar to that of the gallstone cohort. We also used intra-operative cholangiography and single session bile duct exploration rather than relying on pre-operative endoscopic clearance by endoscopic retrograde cholangiopancreatography (ERCP), hence the low incidence of ERCP in this series.
At operation most cholecystectomies (98.6% FGBD and 92.8% GBP) were found to be relatively easy; grades I and II on the Nassar difficulty grading scale for LC, significantly easier than with gall stones (P < .0001). Operative difficulty grades IV and V do not exist in FGBD and GBP (Table 2). The only patient in the FGBD group with a difficulty grade IV had adhesions resulting from a previous open right hemicolectomy. They were significantly (P < .0001 FGBD and P < .001 GBP) less likely to have adhesions between the omentum or the duodenum and the gallbladder or to have a cholangiography. The easier procedures were reflected in a shorter operation time and lower use abdominal drainage.
Table 2.
Operative Data
| LC for FGBD (n = 72) | LC for GBP (n = 42) | LC for Gallstones (n = 5560) | P-Value Gallstone vs FGBD | P-Value Gallstones vs GBP | |
|---|---|---|---|---|---|
| Difficulty grading scale Grade I Grade II Grade III Grade IV Grade V Not recorded |
50 (69.4%) 21 (29.2%) 0 (0%) 1 (1.4%)** 0 (0%) 0 (0%) |
30 (71.4%) 9 (21.4%) 3 (7.1%) 0 (0%) 0 (0%) 0 (0%) |
1796 (32.3%) 1697 (30.5%) 1135 (20.4%) 811 (15.8%) 111 (2.0%) 10 (0.2%) |
< 0.0001 0.347 < 0.001 0.006 0.436 0.717 |
< 0.0001 0.908 0.138 0.025 0.723 0.783 |
| Cholangiography (intraoperative cholangiogram) | 51 (70.1%) | 29 (69%) | 5138 (92.4%) | < 0.0001 | < 0.0001 |
| Adhesions to the gallbladder | 22 (30.6%) | 16 (25.8%) | 3554 (63.9%) | < 0.0001 | < 0.001 |
| Abdominal drains | 11 (15.3%) | 11 (26%) | 2885 (51.9%) | < 0.0001 | 0.002 |
| Length of operation (min): mean (SD)# | 46 (55.4) | 40 (54.7) | 72 (44.9) | < 0.001 | < 0.001 |
| Morbidity | 1 (1.4%): - Bleeding at a 5 mm port site. - Conservative management. |
2 (4.8%): - Wound infection^ -Readmission abdominal pain^. |
297 (5.3%) | 0.284 | 0.992 |
This patient had previous open right colectomy.
LC, laparoscopic cholecystectomy; FGBD, functional gallbladder disorder; GBP, gallbladder polyps; SD, standard deviation.
Symptomatic Response to Surgery
FGBD Patients
The symptomatic response to surgery for each clinical presentation is shown in Table 3. Only 3 patients had a poor response following LC on short term follow up. One patient who had persistent chronic biliary symptoms was ultimately diagnosed with sphincter of Oddi hypertension and underwent botox injection into the sphincter with complete resolution of his symptoms. On long term follow up, all three patients had no biliary symptoms for between 14 to 21 years (Table 4). A quarter of the patients could not be traced and 13% presented with upper GI symptoms from 1 to 18 years after LC. Most were investigated for dyspeptic and reflux symptoms and only two required biliary imaging.
Table 3.
Functional Gallbladder Disorder Clinical Presentations and Short Term Symptomatic Response to Surgery
| Functional Gallbladder Disorder Clinical Presentation | Patients (n = 72) | Symptomatic Response to Surgery No (%) |
|---|---|---|
| Chronic biliary symptoms | 67 (93.1%) | Good response: 64/67 (95.5 %) No response: 3/67 (4.5 %) |
| Acute biliary pain | 5 (6.9%) | Good Response: All (100 %) |
| Total | 72 | Total Good Response: 69 (95.8 %) Total No Response: 3 (4.2 %) |
Table 4.
Pre-operative Investigations and Long-Term Follow Up of Patients with Initial Poor Short Term Response to Laparoscopic Cholecystectomy
| Sex | Age | Pre-operative Investigations/ Ejection Fraction % | Postoperative Investigations/ Follow up | Number of Admission Episodes | |
|---|---|---|---|---|---|
| Case 1 | Male | 65 | Endoscopic retrograde cholangiopancreatography, SOO manometry NAD HIDA Ejection Fraction 17% |
Symptom free 21 years FU. |
2 |
| Case 2 | Female | 52 | Tmax 39 (normal < 20) | OGD NAD, functional dyspepsia, IBS. 18 years FU. |
2 |
| Case 3 | Female | 36 | HIDA Ejection Fraction 22% | OGD healed DU, bile reflux. ERCP and SOO Botox injection. 14 years FU. |
3 |
ERCP, endoscopic retrograde cholangiopancreatography; FU, follow up; HIDA, hepatobiliary iminodiacetic acid; OGD, oesophago-gastro-duodenoscopy; NAD, nicotinamide adenine dinucleotide; SOO, Sphincter of Oddi.
GBP Patients
All 42 GBP patients presented with chronic biliary symptoms. Polyp numbers ranged from 1 to 30 polyps. Polyp size ranged from 1 mm to 11 mm. No cancer was found in any polyp. Three of 42 (7.0%) GBP patients were found on histological examination of the GB to have small, previously undiagnosed, gallstones in addition to the polyps.
A good symptomatic response to surgery was achieved in 95% of GBP cases. Eight patients (19%) complained of dyspeptic symptoms on follow up of between 1 and 23 years. Two-thirds of patients had no GI symptoms at all over the follow up period and 14% could not be traced.
DISCUSSION
The literature suggests that LC achieves symptom relief in most patients with FGBD. In a study of 256 symptomatic patients with negative ultrasound scans and abnormal GBEF on HIDA scans, 95% of patients reported symptomatic improvement and said they would recommend LC.11,12 A meta-analysis of 29 studies including 2891 patients showed that symptomatic patients with a low GBEF benefit from cholecystectomy.13 Our single surgeon study adopted a similar approach and 95.8% of our FGBD patients had a good response to surgery. Those who reported a continuation of their symptoms during the first few months seem to settle on long term follow up.
Careful clinical assessment is necessary to rule out nonbiliary causes of abdominal pain, especially peptic ulcer disease, functional dyspepsia, gastro-esophageal reflux disease, and inflammatory bowel disease. However, it is widely accepted that biliary dyskinesia can be associated with all these conditions.13 This can be viewed as part of a wider disorder of the gastrointestinal tract14 and may explain the initial poor response to surgery in some patients. This contradicts the old belief that FGBD was a diagnosis of exclusion and the suggestion that FGBD was an isolated entity without associated gastrointestinal disorders.
FGBD patients who do not respond to surgery and no obvious cause is found for their chronic biliary symptoms, may have had false-positive GBEF on HIDA scan.15 These scenarios can be seen in advanced diabetes, celiac disease, obesity, cirrhosis, and with some medications, including calcium channel blockers, oral contraceptives/progesterone and histamine-2 receptor antagonists.
Functional biliary sphincter of Oddi disorder (FBSOD) is also a recognized clinical entity in the Rome IV criteria. FGBD and FBSOD may not present in isolation but occur to variable degrees in the same patient. Some patients may benefit from either a cholecystectomy or a sphincterotomy (or botulinum toxin-induced relaxation of the sphincter of Oddi), while others may require both to get the full relief of biliary symptoms.16 One patient in our study required a botox injection after cholecystectomy, resolving his biliary pain.
Dyskinesia may also involve the pancreatic sphincter. One study showed that two-thirds of patients with sphincter of Oddi dysfunction also have elevated pancreatic basal sphincter pressures. While some patients with suspected or documented sphincter of Oddi dysfunction may respond to sphincterotomy alone, some warrant evaluation of their pancreatic sphincter if symptoms persist after therapy.17
The Rome IV criteria clearly suggest that FGBD may be associated with elevated liver enzymes, conjugated bilirubin and/or amylase/lipase.6 A hypertensive sphincter of Oddi can be associated with elevated liver enzymes and/or a dilated bile duct on ultrasound scanning. Similarly, a hypertensive pancreatic sphincter may be associated with elevated serum amylase or lipase levels with or without a hypertensive dyskinetic sphincter of Oddi. These may be useful markers in patients with equivocal investigations.
GBPs tend to be misreported by radiologists and sonographers and managed with different protocols by surgeons. This seems to contribute to further biliary presentations and can delay definitive treatment by LC. One study reported that only 43 of 244 patients (18%), who had GBPs detected on ultrasound, underwent cholecystectomy. A quarter of the patients in this series presented at a later date with biliary symptoms and 21% were eventually offered surgery.18 In our study, all symptomatic GBP patients with polyps larger than 10 mm or those with multiple polyps underwent cholecystectomy. Those who had gastroduodenal pathology on gastroscopy were managed accordingly and were offered cholecystectomy only if they remained symptomatic. Patients who did not meet the above criteria were either discharged or follow up was arranged. Only those undergoing LC are included in our study. Long term follow up, over 10 years in half of the cases, showed no symptoms.
Another study showed that 66% of patients who had cholecystectomy for symptomatic gallbladder polyps with no stones were completely pain free after surgery. The remainder, however, experienced infrequent moderate episodes of pain on eating. The authors concluded that surgery was effective in controlling symptoms and allowing patients to return to normal lifestyle.19 Jones-Monahan et al. demonstrated that among 45 symptomatic patients with GBPs and no stones who underwent cholecystectomy, 93% reported relief of symptoms.20,21 The remaining two patients experienced dyspepsia that did not interfere with daily activity. These results are very similar to those in our study where 95% of patients had a good response to surgery.
The incidence of malignant polyps in patients who underwent cholecystectomy for ultrasound detected gallbladder polyps, ranged from 5% to 15%.22 Our study did not show malignancy in any of the 43 GBP patients. Polyps were relatively small in size, the largest measuring 11 mm.
CONCLUSION
Although the incidence of FGBD and GBP is relatively small, the diagnosis can be challenging and management decisions need careful consideration. Definitive treatment with LC may be offered as it achieves long term symptomatic relief in most patients.
Contributor Information
Haitham Qandeel, Hashemite University, Zarqa, Jordan..
Ahmad H. M. Nassar, Laparoscopic Biliary Service, University Hospital Monklands, Lanarkshire, Scotland, UK..
Hwei J. Ng, Royal Alexandra Hospital, NHS Greater Glasgow and Clyde, Scotland, UK..
Hisham El Zanati, University Hospital Hairmyres, Lanarkshire, Scotland, UK..
References:
- 1. Thiels C, Hanson K, Chawla K, et al. Functional gallbladder disease: operative trends and short-term outcomes. Surgery. 2016;160(1): 100–105. [DOI] [PubMed] [Google Scholar]
- 2. Barbara L, Sama C, Labate AM, et al. A population study on the prevalence of gallstone disease: the Sirmione Study. Hepatology. 1987;7(5):913–917. [DOI] [PubMed] [Google Scholar]
- 3. Al-Azzawi H, Nakeeb A, Saxena R, Maluccio M, Pitt H. Cholecystosteatosis: an explanation for increased cholecystectomy rates. J Gastrointest Surg. 2007;11(7):835–843. [DOI] [PubMed] [Google Scholar]
- 4. Lee S, Kim H, Shin J. Reasonable cholecystectomy of gallbladder polyp – 10 years of experience. Asian J Surg. 2019;42(1):332–337. [DOI] [PubMed] [Google Scholar]
- 5. Lim J, Joo K, Won K, Lim S, Joo S, Yang Y. Predictor of abnormal gallbladder ejection fraction in patients with atypical biliary pain: histopathological point of view. Medicine (Baltimore). 2017;96(51):e9269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cotton P, Elta G, Carter C, Pasricha P, Corazziari E, Rome IV. Gallbladder and sphincter of Oddi disorders. Gastroenterology. 2016(16):224–229. S0016-5085 [DOI] [PubMed] [Google Scholar]
- 7. Canfield A, Hetz S, Schriver J, et al. Biliary dyskinesia: a study of more than 200 patients and review of the literature. J Gastrointest Surg. 1998;2(5):443–448. [DOI] [PubMed] [Google Scholar]
- 8. Sun Y, Yang Z, Lan X, Tan H. Neoplastic polyps in gallbladder: a retrospective study to determine risk factors and treatment strategy for gallbladder polyps. Hepatobiliary Surg Nutr. 2019;8(3):219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nassar A, Ashkar K, Hafiz AA, Mohamed AY. Is laparoscopic cholecystectomy possible without video technology? Min Invas Ther. 1995;4(2):63–65. [Google Scholar]
- 10. Griffiths EA, Hodson J, Vohra RS, et al. Utilisation of an operative difficulty grading scale for laparoscopic cholecystectomy. Surg Endosc. 2019;33(1):110–121; Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dwivedi A, Shetty A, Sanghavi P, Phan T, Lakra Y, Silva Y. Efficacy of laparoscopic cholecystectomy in acalculous gallbladder disease: long-term follow-up. JSLS. 2004;8(2). [PMC free article] [PubMed] [Google Scholar]
- 12. Steele J, Wayne H, Iskandar M, Wolmer T, Bratcher J, Cooperman A. Biliary pain, no gallstones—remove the gallbladder, anyway? J Fam Pract. 2014;63(8). [PubMed] [Google Scholar]
- 13. Vineet S, Gudsoorkar A, Oglat A, Jain, et al. Systematic review with meta-analysis: cholecystectomy for biliary dyskinesia—what can the gallbladder ejection fraction tell us? Aliment Pharmacol Ther. 2019;49(6):654–663. Mar. [DOI] [PubMed] [Google Scholar]
- 14. Penning C, Gielkens H, Delemarre J, Lamers C, Masclee A. Gall bladder emptying in severe idiopathic constipation. Gut. 1999;45(2):264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tulchinsky M. Applied hepatobiliary scintigraphy in chronic gallbladder diseases. Appl Radiol. 2016;45(9):16–25. [Google Scholar]
- 16. Murray W. Botulinum toxin-induced relaxation of the sphincter of Oddi may select patients with acalculous biliary pain who will benefit from cholecystectomy. Surg Endosc. 2011; 25(3):813–816. [DOI] [PubMed] [Google Scholar]
- 17. Lehman G, Sherman S. Hypertensive pancreatic sphincter. Can J Gastroenterol. 1998;12(5):333–337. [DOI] [PubMed] [Google Scholar]
- 18. Abdullah A, Rangaraj A, Rashid M, Puw-Jones R, Rasheed A. Gallbladder polypoid lesions are inaccurately reported and undermanaged: a retrospective study of the management of gallbladder polypoid lesions detected at ultrasound in symptomatic patients during a 36-month period. Clin Radiol. 2019;74(6):489.e17–e23. [DOI] [PubMed] [Google Scholar]
- 19. Ahmed M, Diggory R. Acalculous gallbladder disease: the outcomes of treatment by laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2011;93(3):209–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jones-Monohas K, Gruenberg J, Finer J, Tong G. Isolated small gallbladder polyps: an indication for cholecystectomy in symptomatic patients. Am Surg. 2000;66(8):716–719. [PubMed] [Google Scholar]
- 21. Wiles R, Thoeni R, Barbu S, et al. Management and follow-up of gallbladder polyps: joint guidelines between the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), European Association for Endoscopic Surgery and other Interventional Techniques (EAES), International Society of Digestive Surgery - European Federation (EFISDS) and European Society of Gastrointestinal Endoscopy (ESGE.). Eur Radiol. 2017;27(9):3856–3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pickering O, Pucher P, Toale C, et al. Prevalence and sonographic detection of gallbladder polyps in a Western European Population. J Surg Res. 2020;250:226–231. [DOI] [PubMed] [Google Scholar]