Abstract
Background:
Central nervous system (CNS) cryptococcosis is an invasive fungal infection predominantly seen among immunosuppressed patients causing meningitis or meningoencephalitis. Rarely, cryptococcosis can affect immunologically competent hosts with the formation of localized CNS granulomatous reaction, known as cryptococcoma. Common symptoms of CNS cryptococcoma are headaches, consciousness or mental changes, focal deficits, and cranial nerve dysfunction. Rarely, seizures are the only presenting symptom.
Case Description:
We report the case of an immunocompetent patient with a solitary CNS cryptococcoma presenting with a long history of non-responsive generalized seizure who has been successfully operated.
Conclusion:
CNS cryptococcoma is a rare entity, and in immunocompetent patients, its diagnosis can be challenging. The pathophysiology of lesion-related seizure is discussed along with a review of the pertinent literature.
Keywords: Central nervous system, Cryptococcoma, Seizure

INTRODUCTION
Cryptococcosis is an invasive fungal infection caused by two species of Cryptococcus spp. Cryptococcus neoformans is commonly related to immunocompromised patients mainly causing meningitis. Cryptococcus gattii is encountered in immunocompetent population and it is associated with cryptococcoma formation in the brain and lungs.[18] Accordingly, this infection is predominantly seen among immunosuppressed patients, typically those with HIV infection and from less-developed countries with significant morbidity and mortality.[13] Cryptococcosis can also occur in immunologically competent host providing localized reactions.[3] Hence, central nervous system (CNS) cryptococcosis could be meningeal (the most frequent) and/or parenchymal.[18] Cryptococcoma is a chronic granulomatous reaction due to a local inflammatory response in the immunocompetent host. Frequently, it may be misdiagnosed as a malignant lesion, and an accurate diagnosis can be achieved by histology following surgical resection.[19]
Here, we present the case of an intracranial cryptococcoma in a 32-year-old woman with normal immunity. The main mechanisms underlying seizure manifestation along with a review of the pertinent literature are reported.
CASE DESCRIPTION
A 32-year-old Indian woman presented with a history of tonic-clonic seizures since 2013, started during her first pregnancy. In 2016, she underwent electroencephalogram which confirmed the diagnosis of epilepsy. Accordingly, she started antiepileptic treatment with levetiracetam at initial daily dose of 1 g. Due to the recurrence of seizures, the drug was increased till a daily dose of 1.5 g with a poor seizure control. In 2019, a brain magnetic resonance (MR) examination revealed a right temporo-mesial lesion with an irregular peripheral contrast enhancement. The lesion appeared to protrude toward the right cerebral peduncle with brainstem compression, highly suggestive of low-grade glioma. MR spectroscopy supported the suspicion of glioma. The patient underwent functional MR showing anterior dislocation of the inferior longitudinal fasciculus. [Figures 1 and 2] show the main neuroradiological features. At admission, the neurological examination was negative. Her medical history did not reveal significant features, such as recurrent respiratory infection, and contact with pet animals. HIV serology was negative.
Figure 1:

Pre-operative axial (a), coronal (b), and sagittal (c) post-contrast T1-weighted MR showing a right temporo-mesial lesion with an irregular peripheral enhancement.
Figure 2:
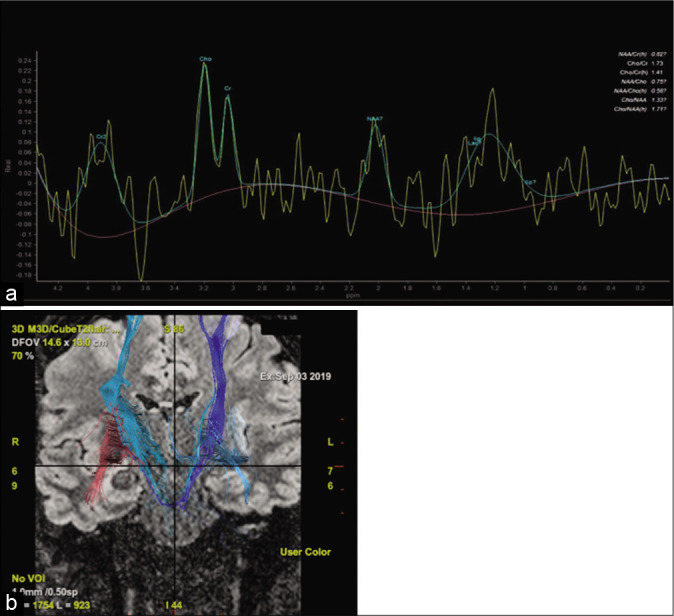
Pre-operative magnetic resonance (MR) spectroscopy (a) depicts a low N-acetylaspartate (NAA) with choline (Cho)/NAA of 1.33 compared to normal brain parenchyma, suggestive for low-grade glioma; functional MR (b) showing the anterior dislocation of the inferior longitudinal fasciculus (ILF) (red tract) and a unaffected corticospinal tracts (blue tracts).
Surgical procedure
The procedure was performed by the use of neuronavigation. A right temporal craniotomy was performed. Through a transulcal approach, the lesion was reached. The lesion appeared as a calcified mass tenaciously attached to the contiguous structures. The lesion was entered, and a yellow-like material was found densely packing the mass. After a careful debulking, the capsule was removed in fragments except for its medial part being strictly adherent to the brainstem [Video 1].
Histopathology
Histopathology showed multiple yeasts consistent with Cryptococcus spp. strongly embedded into an amorphous eosinophilic fibrillar material. Period Acid–Schiff and mucicarmine stain revealed purple organisms and numerous budding yeasts consistent with Cryptococcus spp. [Figures 3 and 4].
Figure 3:
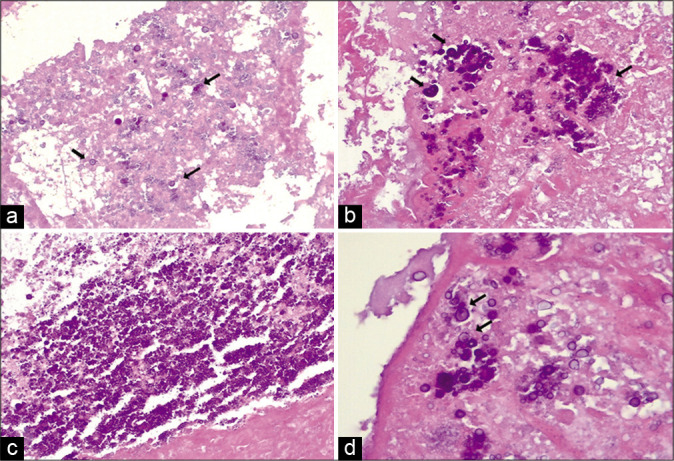
The histopathological findings. (a-c) Cryptococcus embedded in an amorphous eosinophilic fibrillary background. Cryptococcus is a round budding yeast (arrows) that varies in size enveloped by a mucoid capsule (E and E ×20); (d) focus on a cluster of Cryptococcus (arrows) (E and E ×40).
Figure 4:
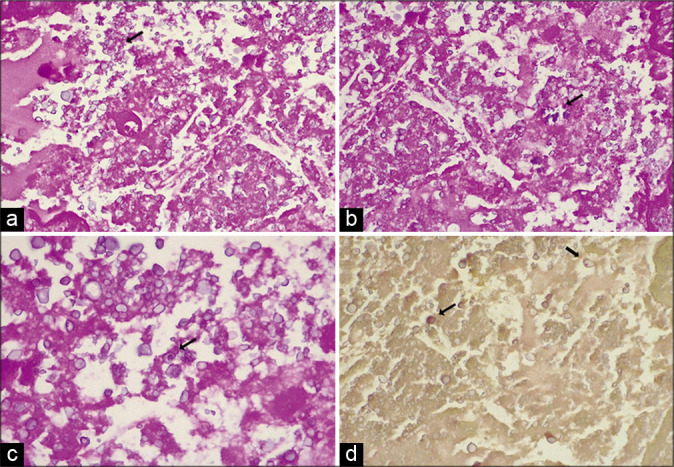
(a-c) Period Acid–Schiff staining the amorphous eosinophilic background and, weakly, the yeasts of Cryptococcus (arrows) (E, F ×20; G ×40); (d) Mucicarmine staining, patchy and weakly, in red the polysaccharide capsule of the yeasts (arrows) (×20).
Post-operative course
After surgery, the patient presented with a mild left leg coordination impairment which disappeared in a few days. Forty-four hours post-operative MRI showed a residual capsule fragment adherent to the midbrain [Figure 3]. A total body computed tomography (CT) scan and a lumbar puncture were performed without evidence of cryptococcal infection. Accordingly, no antifungal regimen was introduced. The patient was discharged on the 7th post-operative day without post-operative seizures and neurological deficits. At 6-month follow-up, no further seizures were reported.
DISCUSSION
Cryptococcal infection occurs by inhalation of infectious propagules from environmental reservoirs and pulmonary impairment constitutes the first manifestation.[13] Inhaled spores can colonize the host respiratory tract without symptoms leading the infection in a latent form for many times.[7] When local host immunity is suppressed, the fungus can reactivate and widely disseminate to several organs.[13] In immunosuppressed patients, Cryptococcus spp. can cross the blood–brain barrier (BBB) causing meningitis, encephalitis, meningoencephalitis, or ventriculitis. In immunocompetent patient, brain cryptococcal infection can present as single or multifocal granulomatous reaction known as cryptococcoma.[6,7,10,12] To date, only four cases of isolated brain cryptococcoma presenting with seizure have been reported [Table 1].[2,14,17,22] In two cases, seizure was associated with other presenting symptoms.[2] Three cases presented with generalized epilepsy,[2,17,22] as in our report, while one with focal epilepsy.[14] The working diagnosis was mostly brain tumor,[2,17] tuberculoma,[14] or vascular malformation.[22] Complete surgical excision was performed in 1 case,[17] subtotal in 1 case,[22] and stereotactic biopsy in 2 cases.[2,14] Post-operative antifungal drugs (i.e., fluconazole and amphotericin) were administered for the prevention of fulminant cryptococcal meningitis in three cases.[2,14,22] In our case, surgical treatment allowed cryptococcoma resection leaving a small capsule fragment adherent to the midbrain. Furthermore, considering the absence of active infection signs, no therapy was introduced.
Table 1:
Cases of isolated brain cryptococcoma presenting with seizure.

It has been reported that Cryptococcus spp. enters the Virchow–Robin spaces and gives rise to small cysts in the brain parenchyma, inducing a chronic granulomatous reaction composed by macrophages, lymphocytes, and foreign body-type giant cells.[5] Cryptococcus spp. is a facultative intracellular pathogen, and macrophages can act as both a niche for fungal replication and a safe vehicle for spreading into the brain.[12,20] Studies on the pathogenesis of epilepsy due to brain infection distinguish between early and late seizures.[8] Early seizure occurs within the 1st 1–2 weeks after infection and it is considered to be insult related. Late seizure is seen months to years after infections and it occurs following resolution of the active phase.[20] During the phase between the infection and onset of seizures, Cryptococcus spp. induces brain damage and BBB impairment through the release of pro-inflammatory cytokines and activation of downstream signaling promoting the innate immunity reaction and later the adaptive immune response.[12,20,21] The risk for developing epilepsy after infections depends on the severity of brain injury, age, genetic factors, and many other unknown variables.[12,20]
Solitary cryptococcoma is a rare lesion,[7] and the absence of an immunosuppressed history or significant predisposing factors in immunocompetent patients makes the diagnosis challenging. In our case, cryptococcoma presented as a localized tumor-like mass with a 7-year seizures history without other symptoms. Indeed, without a clear clinical history, cryptococcoma can appear radiologically indistinguishable from other CNS lesions.[7,9,11,15,19] Differential diagnosis needs to include other neuroinfectious diseases, such as toxoplasmosis, lymphoma, tuberculoma, and primary or metastatic tumors.[1,4,15] These pathologies can produce similar clinical syndromes and MRI or CT findings to cryptococcoma.
In CNS cryptococcal infection, a combined medical and surgical approach is considered the optimal treatment.[18] Systemic antifungal treatment consists of amphotericin B as first-line drug, and flucytosine or fluconazole as second-class agents.[16,18]
According to our experience and based on the few reports available, we speculate that surgical resection should be always attempted to reach a firm diagnosis and brain decompression.[19]
CONCLUSION
CNS cryptococcoma is a rare entity and could affect immunocompetent individuals. It has no specific radiologic findings and can mimic CNS tumors. Our experience suggests that in immunocompetent patients, an isolated intracerebral cryptococcal granuloma can be challenging to diagnose where seizure is the only presenting symptom. In these cases, surgical treatment is mandatory for the diagnosis and seizure resolution.
Supplementary Material
Footnotes
How to cite this article: Brunasso L, Costanzo R, Cascio A, Florena A, Sparacia G, Iacopino DG, et al. Seizure in isolated brain cryptococcoma: Case report and review of the literature. Surg Neurol Int 2021;12:153.
Contributor Information
Laura Brunasso, Email: brunassolara@gmail.com.
Roberta Costanzo, Email: robertacostanzo3@gmail.com.
Antonio Cascio, Email: antonio.cascio03@unipa.it.
Ada Florena, Email: adamaria.florena@unipa.it.
Gianvincenzo Sparacia, Email: gsparacia@ismett.edu.
Domenico Gerardo Iacopino, Email: gerardo.iacopino@gmail.com.
Giovanni Grasso, Email: giovanni.grasso@unipa.it.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Awasthi M, Patankar T, Shah P, Castillo M. Cerebral cryptococcosis: Atypical appearances on CT. Br J Radiol. 2001;74:83–5. doi: 10.1259/bjr.74.877.740083. [DOI] [PubMed] [Google Scholar]
- 2.Batista RR, Gasparetto EL. Uncommon presentation of intracranial cryptococcoma in an immunocompetent patient. AJNR Am J Neuroradiol. 2012;33:E26. doi: 10.3174/ajnr.A2988. author reply E27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beardsley J, Sorrell TC, Chen SC. Central nervous system cryptococcal infections in Non-HIV infected patients. J Fungi (Basel) 2019;5:71. doi: 10.3390/jof5030071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkefeld J, Enzensberger W, Lanfermann H. Cryptococcus meningoencephalitis in AIDS: Parenchymal and meningeal forms. Neuroradiology. 1999;41:129–33. doi: 10.1007/s002340050717. [DOI] [PubMed] [Google Scholar]
- 5.Chen S, Chen X, Zhang Z, Quan L, Kuang S, Luo X. MRI findings of cerebral cryptococcosis in immunocompetent patients. J Med Imaging Radiat Oncol. 2011;55:52–7. doi: 10.1111/j.1754-9485.2010.02229.x. [DOI] [PubMed] [Google Scholar]
- 6.Coppens Y, Kalala JP, van Roost D, van den Broecke C, Vogelaers D. Cryptococcoma unresponsive to antifungal treatment in a 63-year-old non-HIV-infected male. Acta Clin Belg. 2006;61:359–62. doi: 10.1179/acb.2006.057. [DOI] [PubMed] [Google Scholar]
- 7.Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A. Intracranial fungal granuloma: Analysis of 40 patients and review of the literature. Surg Neurol. 2005;63:254–60. doi: 10.1016/j.surneu.2004.04.020. discussion 260. [DOI] [PubMed] [Google Scholar]
- 8.Everitt AD, Sander JW. Classification of the epilepsies: Time for a change? A critical review of the international classification of the epilepsies and epileptic syndromes (ICEES) and its usefulness in clinical practice and epidemiological studies of epilepsy. Eur Neurol. 1999;42:1–10. doi: 10.1159/000008061. [DOI] [PubMed] [Google Scholar]
- 9.Ho CL, Chang BC, Hsu GC, Wu CP. Pulmonary cryptococcoma with CD4 lymphocytopenia and meningitis in an HIV-negative patient. Respir Med. 1998;92:120–2. doi: 10.1016/s0954-6111(98)90043-9. [DOI] [PubMed] [Google Scholar]
- 10.Jung A, Korsukewitz C, Kuhlmann T, Richters M, Fischer B, Niederstadt T, et al. Intracerebral mass lesion diagnosed as cryptococcoma in a patient with sarcoidosis, a rare opportunistic manifestation induced by immunosuppression with corticosteroids. J Neurol. 2012;259:2147–50. doi: 10.1007/s00415-012-6473-y. [DOI] [PubMed] [Google Scholar]
- 11.Li Q, You C, Liu Q, Liu Y. Central nervous system cryptococcoma in immunocompetent patients: A short review illustrated by a new case. Acta Neurochir (Wien) 2010;152:129–36. doi: 10.1007/s00701-009-0311-8. [DOI] [PubMed] [Google Scholar]
- 12.Liu TB, Perlin DS, Xue C. Molecular mechanisms of cryptococcal meningitis. Virulence. 2012;3:173–81. doi: 10.4161/viru.18685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maziarz EK, Perfect JR. Cryptococcosis. Infect Dis Clin North Am. 2016;30:179–206. doi: 10.1016/j.idc.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadkarni TD, Menon RK, Desai KI, Goel A. A solitary cryptococcal granuloma in an immunocompetent host. Neurol India. 2005;53:365–7. doi: 10.4103/0028-3886.16950. [DOI] [PubMed] [Google Scholar]
- 15.Paiva AL, Aguiar GB, Lovato RM, Zanetti AV, Panagopoulos AT, Veiga JC. Cryptococcoma mimicking a brain tumor in an immunocompetent patient: Case report of an extremely rare presentation. Sao Paulo Med J. 2018;136:492–6. doi: 10.1590/1516-3180.2017.0046210417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 Update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salvador GL, Castanho GF, Yokoo P, Teixeira BC. Cryptococcoma in an immunocompetent patient-simulating neoplasia. Eur Neurol. 2019;81:188–9. doi: 10.1159/000501852. [DOI] [PubMed] [Google Scholar]
- 18.Santander XA, Gutierrez-Gonzalez R, Cotua C, Tejerina E, Rodriguez GB. Intraventricular cryptococcoma mimicking a neoplastic lesion in an immunocompetent patient with hydrocephalus: A case report. Surg Neurol Int. 2019;10:115. doi: 10.25259/SNI-104-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ulett KB, Cockburn JW, Jeffree R, Woods ML. Cerebral cryptococcoma mimicking glioblastoma. BMJ Case Rep. 2017;2017:bcr2016218824. doi: 10.1136/bcr-2016-218824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vezzani A, Fujinami RS, White HS, Preux PM, Blumcke I, Sander JW, et al. Infections, inflammation and epilepsy. Acta Neuropathol. 2016;131:211–34. doi: 10.1007/s00401-015-1481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walenkamp AM, Chaka WS, Verheul AF, Vaishnav VV, Cherniak R, Coenjaerts FE, et al. Cryptococcus neoformans and its cell wall components induce similar cytokine profiles in human peripheral blood mononuclear cells despite differences in structure. FEMS Immunol Med Microbiol. 1999;26:309–18. doi: 10.1111/j.1574-695X.1999.tb01403.x. [DOI] [PubMed] [Google Scholar]
- 22.Zhu JQ, Tao XF, Bao WQ, Hao NX, Wu XR. Calcified cerebral cryptococcal granuloma. Indian J Pediatr. 2013;80:345–8. doi: 10.1007/s12098-012-0758-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


