Abstract
Objectives
This study aims to investigate the effectiveness of scapular stabilization exercises in patients with chronic neck pain and scapular dyskinesis.
Patients and methods
This single-center, prospective study included a total of 36 patients (17 males, 19 females; mean age: 41±12.8 years; range, 25 to 57 years) with chronic neck pain and scapular dyskinesis between April 2018 and September 2018. The patients were randomly assigned to three treatment groups. Group 1 (n=13) consisted of those receiving scapular stabilization exercises by a physiotherapy specialist control in addition to the routine physiotherapy and rehabilitation program; Group 2 (n=12) consisted of those receiving the routine physiotherapy and rehabilitation program in addition to scapular stabilization exercises in-home training program; and Group 3 (n=11) consisted of those receiving the routine physiotherapy and rehabilitation program alone. The assessments were made using the Visual Analog Scale (VAS) and Northwick Park Neck Pain Questionnaire (NPQ).
Results
Significant differences were found in the pre- and post-treatment VAS scores, and Group 1 and Group 2 created this significant difference (p<0.05). A significant difference was also observed in the pre- and post-treatment NPQ scores among the groups (p<0.05). Group 1 showed the most significant improvement of the NPQ scores (p<0.05).
Conclusion
Our study results suggest that addition of scapular stabilization exercises to the routine physiotherapy components may be an effective method for improving pain and functional results.
Keywords: Chronic neck pain, scapular dyskinesis, scapular stabilization, physiotherapy
Introduction
Neck pain is a musculoskeletal system disorder which causes social and economic loss by reducing the quality of life (QoL) of the individual, and its prevalence varies from 16.7 to 75.1% in the adult population.[1,2] Although a significant proportion of the patients with acute neck pain recover with or without any treatment, the neck pain remains at varying degrees in half of these patients.[3] Chronic neck pain causes limitations in activities of daily living, resulting in impaired QoL.[3] In recent years, neck pain has become a widespread chronic problem, and the problem cannot be completely resolved; therefore, the relationship between the neck region and the shoulder, back, and scapular regions has begun to be emphasized in many studies.[4,5] The cervical and scapular regions are closely associated and, therefore, a problem in one of these two regions can affect the other region. In the studies conducted, scapular kinematics were found to differ among individuals with neck pain, although they did not show a specific pattern.[5]
During the combined scapula humeral movements, the change in the standard position and motion of the scapula is defined as scapular dyskinesis.[4] Some researchers have reported that the impairment in scapular dyskinesis occurs due to the weakness of the scapula thoracic muscles. In contrast, other researchers have advocated that it is due to the imbalance of muscles responsible for the scapular position rather than strength deficits.[6,7] The muscles that adhere to the medial side of the scapula, such as the middle and lower parts of the trapezius muscle, rhomboid major and minor, and serratus anterior, are the critical muscles for stabilization.[8,9] In the literature, the overactivity in the upper part of the trapezius muscle and the decrease in the neuromuscular control in the lower part of the trapezius and serratus anterior muscles have been shown to cause impairment of the scapular motion.[10] Abnormal activity in the trapezius muscle and associated scapular postural changes have been also described in patients with neck pain.[11,12]
Depending on the dysfunction of the scapula, problems occur in the neuromuscular coordination between the cervical and scapular regions, thus providing a basis for both upper extremity and cervical region problems. Studies in which individuals with neck pain were compared to healthy individuals reported that the position of the scapula, the upper extremity natural joint movements, and scapular movements were different in the relaxation position between the two groups.[13] In the literature, it has been reported that scapular stabilization exercises should be added to the treatment program, as they provide mobility and functional gain in patients with neck pain.[12]
Conservative methods are primarily preferred in the treatment of neck pain. Physiotherapy and rehabilitation methods are frequently used in the treatment of chronic neck pain. In recent years, more comprehensive and integrative evaluations and treatment methods have been emphasized.[8,14] Although many studies have examined the effectiveness of scapular stabilization exercises in patients with chronic neck pain, the number of studies evaluating the effects of scapular stabilization exercises in patients with chronic neck pain with scapular dysfunction is limited.[11] In the present study, therefore, we aimed to investigate the effectiveness of the scapular stabilization exercises targeted to the affected scapula thoracic region in chronic neck pain patients with scapular dyskinesis.
Patients and Methods
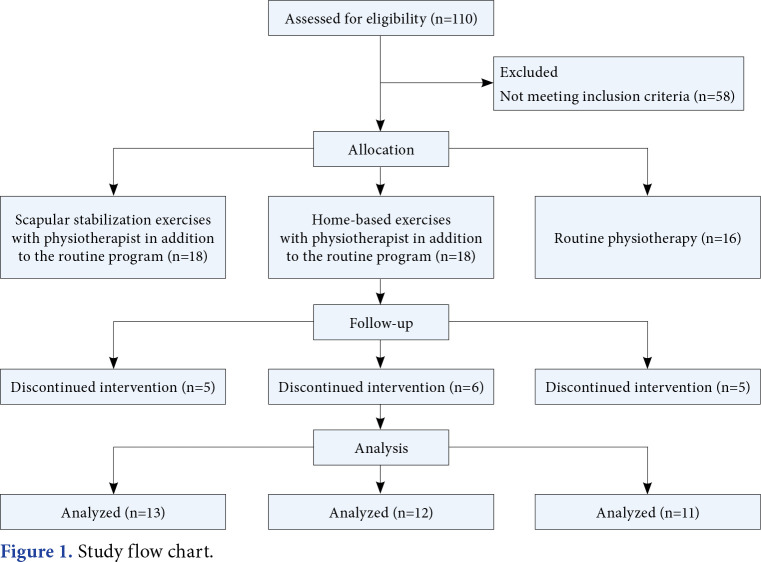
This study was carried out between April 2018 and September 2018 at Inonu University Turgut Ozal Medical Center Physical Therapy and Rehabilitation Department using a pre-treatment/post-treatment quasi experimental study. Patients between 25 and 65 years of age, who agreed to participate in the study, who had complaints of neck pain for at least six months, and who had scapular dyskinesis were included in the study. Those who underwent surgery in the neck and scapular region, who had malignancy, who were treated for neck and back within the past three months, and those with a body mass index of >39 kg/m2 were excluded from the study. Finally, a total of 36 patients (17 males, 19 females; mean age: 41±12.8 years; range, 25 to 57 years) with chronic neck pain and scapular dyskinesis were included. The study flow chart is shown in Figure 1.
Figure 1. Study flow chart.
All patients were examined by a specialist physician for scapular dyskinesis in the outpatient setting. Then, the patients were divided into three groups. Group 1 (n=13) consisted of those receiving scapular stabilization exercises by a physiotherapy specialist control in addition to the routine physiotherapy and rehabilitation program; Group 2 (n=12) consisted of those receiving the routine physiotherapy and rehabilitation program in addition to scapular stabilization exercises in-home training program; and Group 3 (n=11) consisted of those receiving the routine physiotherapy and rehabilitation program alone. None of the patients were allowed to receive any medical treatment for their pain during the treatment period. A written informed consent was obtained from each patient. The study protocol was approved by the Malatya Clinical Research Ethics Committee (date/no: 2018/36). The study was conducted in accordance with the principles of the Declaration of Helsinki.
Assessment and data collection
Data including demographic and clinical characteristics of the patients were recorded at baseline. The Northwick Park Neck Pain Questionnaire (NPQ) was used to evaluate functional status. The NPQ is a tool developed to measure the disability level in neck pain and consists of nine items including neck pain severity, neck pain and sleeping, numbness and tingling in arms in the night, duration of the symptoms and complaints, weight-bearing, reading and watching television, work and home affairs, social activities, and driving. The neck pain total score consists of a maximum of 36 points. If the patient does not drive, the total score is adjusted downward to 32 points. The score is calculated as a percentage of the total NPQ with the following formula: (neck pain score)/36•100%. If the patient does not drive, the formula of (neck pain score)/32•100% is used for the NPQ total percentage calculation. In sum, the percentage range is scored between 0 and 100. High scores indicate a greater disability.[15] The validity and reliability studies of the NPQ have been performed by Kose et al.[16] in the Turkish population.
The Visual Analog Scale (VAS) was used to evaluate the neck pain levels of patients before and after treatment. The patients were asked to mark their pain levels on a 0-10-cm visual scale (0= no pain; 10= unbearable pain).[17]
Treatment protocols
Group 1 received the treatment protocol consisting of scapular stabilization exercises (i.e., scapular retraction, lateral pull-down, and push-up exercises) under the supervision of a physiotherapist, in addition to the 15-session routine physiotherapy and rehabilitation program five days a week. The physiotherapist attended to each session. The scapular stabilization exercises constituted the exercise content of the physiotherapy and rehabilitation program to be applied to the participants. The physiotherapist applied scapular stabilization exercises to the patients within the scapular stabilization exercises.
Group 2 received the treatment protocol consisting of scapular stabilization exercises in an in-home training program (30 repetitions a day, five days a week for a total of three weeks), in addition to the routine physiotherapy and rehabilitation program. Scapular stabilization exercises for the patients included in the in-home training program group were the same as the exercises of the group, which applied scapular stabilization exercises in addition to the routine physiotherapy and rehabilitation program applied by a single physiotherapist. The patients were provided with contact details of the researcher by phone in the event of any problem.
Group 3 received the treatment protocol consisting of only the routine physiotherapy and rehabilitation program. The patients in this group were included in the rehabilitation program for five sessions a week for a total of 15 sessions over three weeks. Physiotherapy and rehabilitation were carried out by physiotherapists experienced in their fields. Before the treatment, the specialist physicians and physiotherapists evaluated the functional status of the patient and determined short-term and long-term targets. Each session lasted for 30 to 45 min. Also, each patient worked with the same physiotherapist in each session to maintain the continuity of care.
Routine physiotherapy and rehabilitation program consisted of the use of a superficial heat agent (20 min), conventional transcutaneous electrical nerve stimulation (20 min), and ultrasound (US). The US was administered continuously at a density of 1.5 w/cm2. Treatment duration was set to 7 min.
Statistical analysis
The post-hoc power analysis was performed using the Web-Based Sample Size and Power Analysis Software (WSSPAS) free statistical software.[18] The calculated study power (1-β) was 0.937, considering a type I error (α) of 0.05, a sample size of 11, and effect (d) size of 0.7. Statistical analysis was performed using the IBM SPSS for Windows version 25.0 software (IBM Corp., Armonk, NY, USA). Descriptive data were expressed in mean ± standard deviation (SD), median (min-max) or number and frequency. The Shapiro-Wilk test was used the check the suitability of the variables to normal distribution. The Wilcoxon signed-rank test was performed to compare pre- and post-treatment changes among the groups. The Kruskal-Wallis test was used to compare the groups. Categorical data were analyzed using Chi-square test. The pairwise comparisons of the groups concerning the difference in the scale scores used were performed by the Bonferroni-corrected Mann-Whitney U test. A p value of <0.05 was considered statistically significant.
Results
There was no statistically significant difference in the baseline demographic and clinical characteristics of the patient groups (p>0.05) (Table 1).
Table 1. Demographic and clinical characteristics of study groups.
| Group 1 (n=13) | Group 2 (n=12) | Group 3 (n=11) | P | |||||||
| n | % | Mean±SD | n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 39.6±13.9 | 40.7±11.4 | 42.8±13.8 | 0.749* | ||||||
| Sex | 0.822† | |||||||||
| Female | 6 | 46.1 | 5 | 41.6 | 6 | 45.4 | ||||
| Male | 7 | 53.9 | 7 | 58.4 | 5 | 44.6 | ||||
| Body mass index (kg/m2) | 26.9±3.5 | 27.11±2.5 | 25±3.4 | 0.684* | ||||||
| Complaint period (month) | 18.4±9.6 | 15.6±3.3 | 17.1±26.6 | 0.718* | ||||||
| * Kruskal Wallis H test; † Chi-square test. | ||||||||||
However, there were statistically significant changes in the pre-and post-treatment VAS scores in all groups (p<0.05). In terms of the NPQ scores, there was also a statistically significant difference between pre- and post-treatment scores in Group 1 and Group 3 (p<0.05). No significant difference was found in Group 2 (p>0.05). There was no significant difference in the pre-treatment VAS scores of the treatment groups (p>0.05). However, we observed a statistically significant difference in the post-treatment VAS scores among the groups (p<0.05). The pre- and post-treatment NPQ and VAS scores of all groups are shown in Table 2.
Table 2. Pre- and post-treatment VAS and NPQ scores.
| Pre-treatment | Post-treatment | |||||||
| Variables | x̄±SD | Median | Min-Max | x̄±SD | Median | Min-Max | z | p |
| VAS (0-10 cm) | ||||||||
| Group 1 | 6.5±1.3 | 7 | 4-8 | 2.8±1.7 | 3 | 0-5 | -3.256 | 0.001* |
| Group 2 | 6.3±1.3 | 6 | 4-8 | 4.1± 1.6 | 4 | 0-7 | -2.958 | 0.003* |
| Group 3 | 6.7±1.1 | 7 | 5-8 | 4.5±1.5 | 5 | 2-7 | -2.961 | 0.003* |
| Pa | 0.773 | 0.020* | ||||||
| NPQ (0-100%) | ||||||||
| Group 1 | 31.9±16.5 | 30.5 | 11.1-68.7 | 16.1±11.2 | 12.5 | 00.0-68.7 | -3.180 | 0.001* |
| Group 2 | 41.3±12.9 | 41.1 | 19.4-61.1 | 36.5±13.1 | 38.5 | 14.1-55.5 | -1.650 | 0.099 |
| Group 3 | 38.8±15.5 | 41.6 | 8.3-65.6 | 33.7±14.2 | 36.1 | 8.3-53.1 | -2.371 | 0.018* |
| Pa | 0.200 | 0.002* | ||||||
| VAS: Visual Analog Scale; NPQ: Northwick Park Neck Pain Questionnaire; SD: Standard deviation; Min: Minimum; Max: Maximum; z: Wilcoxon signed rank test; a: Kruskal Wallis H test; * p<0.05. | ||||||||
In addition, there was a significant difference in the disability status after treatment among the groups (p<0.01). There was a significant difference in the post-treatment VAS-pain scores and, Group 1 and Group 2 created this significant difference (p=0.001 and p=0.019, respectively). A statistically significant improvement was observed in the post-treatment NPQ scores of Group 1, compared to Groups 2 and 3 (p=0.001 and p=0.006, respectively). Group 1 created the significant difference in the improvement of the NPQ scores among the groups (Table 3).
Table 3. Comparisons of post-treatment VAS and NPQ scores among the groups.
| Variables | Post-treatment | ||
| U | z | p | |
| VAS (0-10 cm) | |||
| Group 1-2 | 61.000 | -1.036 | 0.300 |
| Group 1-3 | 17.500 | -3.403 | 0.001 |
| Group 2-3 | 31.000 | -2.344 | 0.019 |
| NPQ (0-100%) | |||
| Group 1-2 | 19.500 | -3.188 | 0.001 |
| Group 1-3 | 24.000 | -2.754 | 0.006 |
| Group 2-3 | 58.000 | -0.496 | 0.620 |
| VAS: Visual Analog Scale; NPQ: Northwick Park Neck Pain Questionnaire; z: Bonferroni-corrected Mann-Whitney U test. | |||
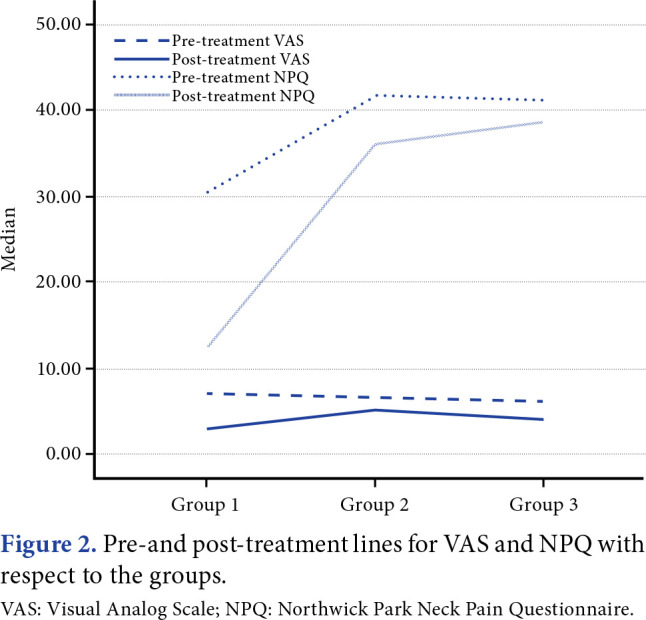
The pre-and post-treatment lines for VAS and NPQ according to the groups are depicted in Figure 2.
Figure 2. Pre-and post-treatment lines for VAS and NPQ with respect to the groups. VAS: Visual Analog Scale; NPQ: Northwick Park Neck Pain Questionnaire.
Discussion
In this study, the effectiveness of the scapular stabilization exercises targeted to the affected scapula thoracic region in chronic neck pain patients with scapular dyskinesis were investigated. The patients with chronic neck pain accompanied by scapular dyskinesis were randomly assigned to one of three groups: When the pre-treatment and post-treatment VAS and NPQ scores were compared in the group in which scapular stabilization exercises in addition to the routine physiotherapy and rehabilitation program were applied, a statistically significant difference was observed.
Home-based exercise programs are practical, economic, and effective treatment modalities for chronic pain management.[19] Previous studies have shown that these programs are as effective as standard physical treatment methods, although the exercises performed with the physiotherapist are more effective.[20] Similar to the literature, in our study, we found that the exercises carried out under the supervision of a physiotherapist were more effective.
In recent years, some researchers have examined the effectiveness of addition of scapular stabilization exercises to the routine treatment program along with the cervical region exercises in patients with neck and back pain.[21] As there can be changes in the muscle imbalance and mobilization around the scapula in patients with scapular dyskinesis, relevant exercises should be added to the neck pain treatment program.[12] Therefore, a dynamic program was developed consisting of both cervical and scapula thoracic stabilization exercises and exercises for the muscles around the scapula in our study.
Review of the literature reveals studies supporting the methodology and results of our study. Dusunceli et al.[22] compared the cervical and scapular stabilization exercises with physical therapy agents in patients with chronic neck pain and showed that the frequency of drug use in the stabilization exercise group was reduced. In another study, Jull et al.[23] randomly divided women with chronic neck pain into two groups and applied proprioceptive exercises to the first group and craniocervical flexion exercise training to the second group. Although there was a significant decrease in the severity of pain for both exercise groups, there was no other statistically significant difference between the groups. Similarly, Andersen et al.[24] divided office workers with chronic neck pain into two groups as the training group receiving random scapular training and the control group. In the training group, two exercises were used: press-up and push-up plus. The authors concluded that there was a decrease in the pain severity and an increase in the pain threshold in the training group, compared to the control group. Likewise, Zhang et al.[25] reported that scapular stabilization exercises in scapular dyskinesis patients were effective in acquiring normal scapula position and shoulder joint movements, and avoiding pain. Consistent with these data, we observed a statistically significant decrease in the VAS scores of Group 1, compared to the other groups. However, there was no significant change in Group 2 in which home-based exercises were provided. This can be attributed to the possibility of non-adherence of Group 2 patients to the given exercise program and non-allowance of taking advantage of pain-relieving effects of the conventional PM&R agents in our study.
The pain, which causes motor control to change by affecting motor unit activation and the sense of proprioception, also adversely affects functions. [26] Pain in the neck region limits the functions of the affected region. In a randomized-controlled study by Yildiz et al.,[5] the effects of cervical and scapular stabilization exercises on nonspecific neck pain were examined and the patients were randomly allocated to one of two groups as the intervention group receiving neck-focused exercise and scapular stabilization training and the control group receiving neck-focused exercise training only. Although a significant improvement was observed in the VAS and Neck Disability Index scores after six weeks of training in both groups, there was no significant difference in scapula kinematics between the intervention and control groups. In our study, a statistically significant decrease in the NPQ scores of Group 1 was observed, compared to the other groups. This supports the opinion that the decrease in pain severity is significantly correlated with the improved functional status. However, although there are several studies examining the effect of scapular stabilization exercises and scapula thoracic muscle training on pain and QoL in patients with scapular dyskinesis or chronic neck pain in the literature, the number of studies investigating these effects on functional status is still scarce. We, therefore, believe that our study would contribute to the literature in this area of research.
Nonetheless, there are some limitations to this study. The diagnosis of scapular stabilization was made only based on the clinical examination of the physician. In addition, the number of patients with scapular dyskinesia and chronic neck pain recruited during the study period was limited.
In conclusion, the treatment of scapular dyskinesis requires correction of the general body biomechanics, not just a local segment, such as the shoulder or neck, where the pain is felt more intensely. Since the human body is a kinetic chain and neck and scapular regions are involved in this kinetic chain, it may be useful to consider the scapular biomechanics for scapular region treatment. The treatment method in which the exercises are taught individually by a physiotherapist and supported by conventional physiotherapy agents has a positive effect on the pain and functional status of patients. We believe that the mechanism of scapular dysfunction would improve with longer treatment duration and longer follow-up, and the effects of exercise would be more beneficial in the long-term.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Coşkun ME. Neck pain and treatment. Turkiye Klinikleri J Surg Med Sci. 2006;2:43–47. [Google Scholar]
- 2.Genebra CVDS, Maciel NM, Bento TPF, Simeão SFAP, Vitta A. Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther. 2017;21:274–280. doi: 10.1016/j.bjpt.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taş S, Erden Z. Kronik boyun ağrılı bireylerde postüral kontrol ve dengenin incelenmesi. JETR. 2017;4:97–104. [Google Scholar]
- 4.Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142–151. doi: 10.5435/00124635-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Yildiz TI, Turgut E, Duzgun I. Neck and scapula-focused exercise training on patients with nonspecific neck pain: A randomized controlled trial. J Sport Rehabil. 2018;27:403–412. doi: 10.1123/jsr.2017-0024. [DOI] [PubMed] [Google Scholar]
- 6.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 7.Phadke V, Camargo P, Ludewig P. Scapular and rotator cuff muscle activity during arm elevation: A review of normal function and alterations with shoulder impingement. Rev Bras Fisioter. 2009;13:1–9. doi: 10.1590/S1413-35552009005000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castelein B, Cools A, Parlevliet T, Cagnie B. Are chronic neck pain, scapular dyskinesis and altered scapulothoracic muscle activity interrelated. : A case-control study with surface and fine-wire EMG. J Electromyogr Kinesiol. 2016;31:136–143. doi: 10.1016/j.jelekin.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Lee ST, Moon J, Lee SH, Cho KH, Im SH, Kim M, et al. Changes in activation of serratus anterior, trapezius and latissimus dorsi with slouched posture. Ann Rehabil Med. 2016;40:318–325. doi: 10.5535/arm.2016.40.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. doi: 10.4085/1062-6050-44.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozünlü Pekyavaş N, Kunduracılar Z, Ersin A, Ergüneş C, Tonga E, Karataş M. The relationship between scapular dyskinesia, pain, range of motion, and flexibility in patients with neck and shoulder problems. Agri. 2014;26:119–125. doi: 10.5505/agri.2014.55486. [DOI] [PubMed] [Google Scholar]
- 12.Zakharova-Luneva E, Jull G, Johnston V, O’Leary S. Altered trapezius muscle behavior in individuals with neck pain and clinical signs of scapular dysfunction. J Manipulative Physiol Ther. 2012;35:346–353. doi: 10.1016/j.jmpt.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Cagnie B, Struyf F, Cools A, Castelein B, Danneels L, O’leary S. The relevance of scapular dysfunction in neck pain: a brief commentary. J Orthop Sports Phys Ther. 2014;44:435–439. doi: 10.2519/jospt.2014.5038. [DOI] [PubMed] [Google Scholar]
- 14.O'Riordan C, Clifford A, Van De Ven P, Nelson J. Chronic neck pain and exercise interventions: frequency, intensity, time, and type principle. Arch Phys Med Rehabil. 2014;95:770–783. doi: 10.1016/j.apmr.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Leak AM, Cooper J, Dyer S, Williams KA, Turner-Stokes L, Frank AO. The Northwick Park Neck Pain Questionnaire, devised to measure neck pain and disability. Br J Rheumatol. 1994;33:469–474. doi: 10.1093/rheumatology/33.5.469. [DOI] [PubMed] [Google Scholar]
- 16.Kose G, Hepguler S, Atamaz F, Oder G. A comparison of four disability scales for Turkish patients with neck pain. J Rehabil Med. 2007;39:358–362. doi: 10.2340/16501977-0060. [DOI] [PubMed] [Google Scholar]
- 17.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) S240-52Arthritis Care Res (Hoboken) 2011;63 Suppl 11 doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 18.Arslan AK, Yaşar Ş, Çolak C, Yoloğlu S. WSSPAS: An interactive web application for sample size and power analysis with r using shiny. Turkiye Klinikleri Journal of Biostatistics. 2018;10:224–246. [Google Scholar]
- 19.Ay S, Koldaş Doğan Ş, Evcik D. Is there an effective way to prescribe a home-based exercise program in patients with knee osteoarthritis. A randomized controlled study. Turk J Phys Med Rehab. 2013;59:1–6. [Google Scholar]
- 20.Anar SÖ. The effectiveness of home-based exercise programs for low back pain patients. J Phys Ther Sci. 2016;28:2727–2730. doi: 10.1589/jpts.28.2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Celenay ST, Akbayrak T, Kaya DO. A comparison of the effects of stabilization exercises plus manual therapy to those of stabilization exercises alone in patients with nonspecific mechanical neck pain: a randomized clinical trial. JOSPT. 2016;46:44–55. doi: 10.2519/jospt.2016.5979. [DOI] [PubMed] [Google Scholar]
- 22.Dusunceli Y, Ozturk C, Atamaz F, Hepguler S, Durmaz B. Efficacy of neck stabilization exercises for neck pain: a randomized controlled study. J Rehabil Med. 2009;41:626–631. doi: 10.2340/16501977-0392. [DOI] [PubMed] [Google Scholar]
- 23.Jull G, Falla D, Treleaven J, Hodges P, Vicenzino B. Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res. 2007;25:404–412. doi: 10.1002/jor.20220. [DOI] [PubMed] [Google Scholar]
- 24.Andersen CH, Andersen LL, Zebis MK, Sjøgaard G. Effect of scapular function training on chronic pain in the neck/ shoulder region: a randomized controlled trial. J Occup Rehabil. 2014;24:316–324. doi: 10.1007/s10926-013-9441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang M, Zhou JJ, Zhang YM, Wang JH, Zhang QY, Chen W. Clinical effectiveness of scapulothoracic joint control training exercises on shoulder joint dysfunction. Cell Biochem Biophys. 2015;72:83–87. doi: 10.1007/s12013-014-0408-4. [DOI] [PubMed] [Google Scholar]
- 26.Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361–370. doi: 10.1016/s1050-6411(03)00042-7. [DOI] [PubMed] [Google Scholar]