Abstract
Introduction
Robot‐assisted radical prostatectomy often causes damage to the neurovascular bundle which results in erectile dysfunction and urinary incontinence. Recovery may take months; however, dehydrated umbilical cord allografts appear to offer an advantage in terms of a faster return to continence and potency.
Case presentation
A 67‐year‐old male, who presented with intermediate‐risk prostate cancer, underwent a bilateral nerve‐sparing radical prostatectomy and placement of dehydrated human umbilical cord graft. Four weeks post‐prostatectomy, the patient reported minimal stress urinary incontinence and erections with 75% rigidity. Three months post‐prostatectomy, the patient noted improved continence and erections with 100% rigidity.
Conclusion
To our knowledge, this is the second experience reported in the literature evaluating the use of umbilical cord allograft during robot‐assisted radical prostatectomy, with promising results, and it is the first reported case to analyze potency as an outcome.
Keywords: dehydrated umbilical cord allograft, erectile dysfunction, robot‐assisted radical prostatectomy, urinary incontinence
Abbreviations & Acronyms
- AUA
American Urological Association
- BMI
body mass index
- dHACM
dehydrated human amnion/chorion membrane
- NVB
neurovascular bundle
- PDE‐5i
phosphodiesterase 5 inhibitors
- PSA
prostate‐specific antigen
- RARP
robot‐assisted radical prostatectomy
- RP
radical prostatectomy
- SHIM
Sexual Health Inventory for Men
- SUI
stress urinary incontinence
- UC
umbilical cord
Keynote message.
The anti‐inflammatory properties of the UC allograft provide an optimal environment for healing and recovery of the cavernosal nerves and appears to offer a significant advantage in terms of completing the goal of early incontinence reduction and return to potency.
Introduction
Two complications that arise after RP include erectile dysfunction and urinary incontinence, both of which greatly affect the quality of life and social well‐being of patients. Neuropraxia and trauma to the NVB have been shown to cause an inflammatory response that can lead to damage of the cavernosal nerves. 1 The clinical use of dHACM allografts, containing growth factors and anti‐inflammatory substances for the protection and regeneration of the prostatic NVB, has been show to accelerate early return to continence and potency. 2 , 3 , 4 , 5
Cryopreserved UC allografts appear to offer a slight advantage in terms of a faster return to continence; 6 however, there is a lack of published data illustrating the use of UC allografts in improving potency after RARP. Thus, we describe a case of a 67‐year‐old male who had an accelerated return to continence and potency with the use of a dehydrated human UC allograft at the time of RARP.
Case presentation
We describe a case of a 67‐year‐old male with a BMI of 30.4 who underwent a bilateral nerve‐sparing RARP under Institutional Review Board protocol (Fig. 1) and placement of dehydrated human UC graft from Samaritan Biologics processed in Miami, Florida (Fig. 2). Patient initially presented with clinically localized cT1c Gleason 3 + 4 = 7 prostate cancer with PSA of 4.06 ng/mL. Preoperative SHIM score was 24 with AUA symptom score of 8. An intrafascial nerve sparing, with combined anterograde and retrograde approach, was utilized for this patient. This approach balances oncologic efficacy with adequate functional outcomes. The UC allograft was placed prior to posterior reconstruction with a wraparound technique over the NVB. The dissected vas deferens and seminal vesicles were lifted anteriorly, and Denonvilliers' fascia was then incised to enter the plane between the prostatic capsule and fascia. This dissection was carried antegrade until the apex was reached. The lateral prostatic fascia was then opened sharply to expose the NVB at the mid prostate. The dissection was then carried inferiorly to the posterior plane until releasing the NVB from the prostate pedicle. The pedicle was controlled using Hem–o–lok clips, releasing the entire bundle away from the prostate. It is important to note that during this dissection, electrocautery was avoided to minimize thermal injury, and tension on the NVB was avoided, in order to evade stretch injury. In‐room to out‐of‐room time was 210 min. Estimated blood loss was 50 cc. Final pathology revealed a 36 g 3 + 4 = 7 adenocarcinoma of the prostate negative for seminal vesicle invasion but positive for extra‐prostatic extension, pT3aN0Mx. Final surgical margins were negative. A non‐narcotic protocol was adopted utilizing liposomal bupivacaine and postoperative acetaminophen, gabapentin, and ketorolac. The patient was discharged on postoperative day #1 with a visual analog scale pain score of 0. The patient returned on postoperative day #8 for Foley catheter removal. Postoperative improvements in continence and potency are shown in Table 2.
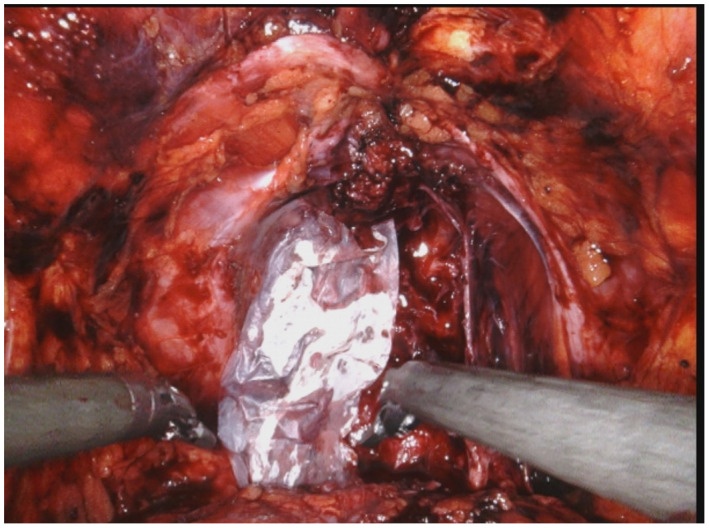
Fig. 1.

Surgical image of RARP before dehydrated UC graft placement.
Fig. 2.
Surgical image of dehydrated human UC graft from Samaritan Biologics placed around NVB.
Table 2.
Postoperative visit improvements in continence and potency
| Postoperative visit | SUI | Potency | PSA (ng/mL) | AUA symptom score |
|---|---|---|---|---|
| Visit #1: 4 weeks post‐prostatectomy | Minimal SUI utilizing 1 pad/day without notable leakage | Erections with 75% rigidity without the use of oral PDE‐5i. Erection satisfactory for penetrative sexual intercourse | N/A | 16 |
| Visit #2: 3 months post‐prostatectomy | Improvement in SUI utilizing 1 pad/multiple days | Erections with 100% rigidity (SHIM score 17) without the use of oral PDE‐5i | Undetectable (<0.01 ng/mL) | 5 |
| Visit #3: 6 months post‐prostatectomy | Improvement in SUI utilizing 0 pads/day | Erections with 100% rigidity (SHIM score 24) without the use of oral PDE‐5i | Undetectable (<0.01 ng/mL) | 5 |
Discussion
The average time for continence recovery post‐RARP is 2.66 months and the average time to recovery of potency is 7.72 months. 7 However, multiple studies demonstrate that the mean time to continence and potency was significantly shorter in patients who were treated with dHACM and UC allografts at the time of prostatectomy as compared to a control group (Table 1). Recovery after RARP is influenced by numerous factors; however, it is evident that the use of the UC allograft significantly enhances early return to potency and continence, as shown in our patient (Table 2). A basic science study using human prostate and bladder cancer cell lines in vitro and in a rat tumor resection model has illustrated the potential for local tumor recurrence when a perinatal tissue allograft is used in patients at high risk of positive margins. 8 However, our patient had negative surgical margins, and no study to date has shown recurrence in patients with organ‐confined disease.
Table 1.
Studies showing improvements in potency and/or continence after allograft placement during RARP
| Publication | Outcome | Results | Type of graft used |
|---|---|---|---|
| Ogaya‐Pinies et al. 2 | Potency | The mean time to potency recovery was enhanced by 0.45 months in the dHACM experimental group | dHACM |
| Razdan et al. 5 | Potency | A faster recovery of erectile function was shown by 2.0 months in the dHACM experimental group | dHACM |
| Barski et al. 4 | Continence and potency | Return to continence was improved by 0.62 months and the mean time to potency was enhanced by 2.2 months in the dHACM experimental group | dHACM |
| Patel et al. 3 | Continence and potency | Return to continence was enhanced by 0.62 months and the mean time to potency was enhanced by 2.05 months in the dHACM experimental group | dHACM |
| Ahmed et al. 6 | Continence | More patients in the UC group became continent at 1 month (65% vs 44%), 3 months (83% vs 70%), 6 months (90% vs 84%) and 12 months (97% vs 87%) | UC |
UC graft is a dehydrated human UC allograft that requires no thawing or special handling. It is ready to use from the package minimizing disruption to the surgical flow. UC allografts have been shown to contain more than 450 bioactive proteins including growth factors and cytokines known to modulate inflammation, support new blood vessel formation, and promote tissue healing while undergoing cell‐mediated resorption. 9 To minimize the potential for disease transmission within perinatal tissue allografts, manufacturer’s rigorously screen the tissue donors. UC is twice as thick as dHACM grafts which yields improved handling characteristics for robotic techniques and the ability to be secured with sutures if desired. 10 Additional characteristics of UC allografts that differ from dHACM grafts are shown in Table 3.
Table 3.
Characteristics of UC allografts
| Characteristic of UC allograft | Additional information |
|---|---|
| Thickness | UC allograft is approximately 2× thicker than dHACM and can contain higher amounts of ECM proteins including hyaluronic acid, collagen type I, fibronectin, and laminin 9 , 10 |
| Sterilization | UC allografts are terminally sterilized using validated processes which kill living microorganisms and achieve a sterility assurance level of 10−6 |
| Donor screening | Manufacturer’s rigorously screen the tissue donors and perform serological testing for communicable diseases. Manufacturing processes and procedures are established which follow current good tissue practice regulations |
Only one other study has been published looking at UC graft at the time of prostatectomy, as the role of UC in reducing inflammation and promoting healing is relatively new. 6 Our findings indicate utilization of a dehydrated human UC allograft can quicken the return of both sexual function and continence. A major limitation of this paper is the sample size and lack of comparative groups. Further studies are needed in a prospective, randomized fashion to support these results. Additionally, a multivariate analysis of factors influencing continence and sexual rehabilitation, including the use of allografts, should be performed.
Conclusion
Erectile dysfunction and incontinence are common side effects of RARP. Utilization of a dehydrated human UC allograft at the time of prostatectomy can quicken the return of both sexual function and continence. The anti‐inflammatory properties of the UC allograft provide an optimal environment for healing and recovery of the cavernosal nerves.
Informed consent
All informed consent was obtained from the subject(s) and/or guardian(s).
Conflict of interest
The authors declare no conflict of interest.
Krol BC, Hemal AK, Peak T, Liu S, Pathak RA. Early return to continence and potency with use of dehydrated human umbilical cord graft at the time of robot‐assisted radical prostatectomy: A case study and analysis of relevant literature. IJU Case Rep. 2021; 4: 151–153.
References
- 1. Menon M, Kaul S, Bhandari A, Shrivastava A, Tewari A, Hemal A. Potency following robotic radical prostatectomy: a questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J. Urol. 2005; 174: 2291–6. [DOI] [PubMed] [Google Scholar]
- 2. Cadeddu JA. Re: can dehydrated human amnion/chorion membrane accelerate the return to potency after a nerve‐sparing robotic‐assisted radical prostatectomy? Propensity score‐matched analysis. J. Urol. 2019; 201: 423–4. [DOI] [PubMed] [Google Scholar]
- 3. Patel VR, Samavedi S, Bates AS et al. Dehydrated human amnion/chorion membrane allograft nerve wrap around the prostatic neurovascular bundle accelerates early return to continence and potency following robot‐assisted radical prostatectomy: Propensity score‐matched analysis. Eur. Urol. 2015; 67: 977–80. [DOI] [PubMed] [Google Scholar]
- 4. Barski D, Gerullis H, Ecke T et al. Application of dried human amnion graft to improve post‐prostatectomy incontinence and potency: a randomized exploration study protocol. Adv. Ther. 2020; 37: 592–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Razdan S, Bajpai RR, Razdan S, Sanchez MA. A matched and controlled longitudinal cohort study of dehydrated human amniotic membrane allograft sheet used as a wraparound nerve bundles in robotic‐assisted laparoscopic radical prostatectomy: a puissant adjunct for enhanced potency outcomes. J. Robot. Surg. 2019; 13: 475–81. [DOI] [PubMed] [Google Scholar]
- 6. Ahmed M, Esposito M, Lovallo G. A single‐center, retrospective review of robot‐assisted laparoscopic prostatectomy with and without cryopreserved umbilical cord allograft in improving continence recovery. J. Robot. Surg. 2020; 14: 283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Neumaier MF, Segall Júnior CH, Hisano M, Rocha FET, Arap S, Arap MA. Factors affecting urinary continence and sexual potency recovery after robotic‐assisted radical prostatectomy. Int. Braz. J. Urol. 2019; 45: 703–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alvim RG, Hughes C, Somma A et al. The potential risk of tumor progression after use of dehydrated human amnion/chorion membrane allograft in a positive margin resection model. Ther. Adv. Urol. 2019; 11: 1756287219837771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bullard JD, Lei J, Lim JJ, Massee M, Fallon AM, Koob TJ. Evaluation of dehydrated human umbilical cord biological properties for wound care and soft tissue healing. J. Biomed. Mater. Res. B Appl. Biomater. 2019; 107: 1035–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lei J, Priddy LB, Lim JJ, Massee M, Koob TJ. Identification of extracellular matrix components and biological factors in micronized dehydrated human amnion/chorion membrane. Adv. Wound Care 2017; 6: 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]


