Abstract
Background
Despite the COVID-19 pandemic, cardiovascular disease is still the main cause of death in developed countries. Of these deaths, acute coronary syndromes (ACS) account for a substantial percentage of deaths. Improvement in ACS outcomes, are achieved by reducing the time from symptom onset until reperfusion or total ischemic time (TIT). Nevertheless, due to the overwhelming reality at the beginning of the pandemic, acute coronary syndrome (ACS) care may have been compromised.
Objectives
We evaluated delays in TIT based on the date and timing of admissions in patients with STEMI, by a timeline follow-up form, before and during the current COVID-19 pandemic.
Methods
Between July 2018 and June 2020, two hundred and twelve patients diagnosed with ST-segment elevation myocardial infarction (STEMI) were admitted to our medical center. Upon presentation, cases were assigned a timeline report sheet and each time interval, from onset of symptoms to the catheterization lab, was documented. The information was later evaluated to study potential excessive delays throughout ACS management.
Results
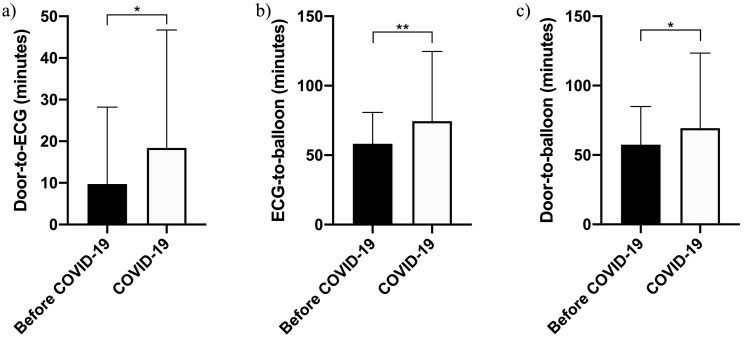
Our data evidenced that during the COVID-19 pandemic ACS admissions were reduced by 34.54%, in addition to several in-hospital delays in patient's ACS management including delays in door-to-ECG time (9.43 ± 18.21 vs. 18.41 ± 28.34, p = 0.029), ECG-to-balloon (58.25 ± 22.59 vs. 74.39 ± 50.30, p = 0.004) and door-to-balloon time (57.41 ± 27.52 vs. 69.31 ± 54.14, p = 0.04).
Conclusions
During the pandemic a reduction in ACS admissions occurred in our hospital that accompanied with longer in-hospital TIT due to additional tests, triage, protocols to protect and prevent infection within hospital staff, and maintenance of adequate standards of care. However, door-to-balloon time was maintained under 90 min.
Keywords: STEMI, COVID-19, SARS-Cov, Time-to-balloon, Ischemia time, Reperfusion strategies, Revascularization, Primary PCI, Care, Management
1. Introduction
Cardiovascular diseases (CVD) are the number one cause of death globally [1]. In Israel, CVD were the second most common cause of death, after cancer, representing 15% of all deaths in 2016 [2]. Considered one of the most representative CVD, acute coronary syndrome (ACS) is characterized by sudden and severe reduction of coronary flow and tissue perfusion followed by cardiomyocytes loss and tissue necrosis [1,3,4]. The total ischemic time (TIT) is one of the most critical parameters that determine patient prognosis defined as the time from symptoms onset until reperfusion [3,5,6]. The underlying ACS perfusion deficit or ischemia can be classified into a ST-segment elevation myocardial infarction (STEMI) and a non-ST-segment elevation myocardial infarction (NSTEMI) by electrocardiographic (ECG) assessment [7,8]. STEMI is the electrical manifestation of transmural ischemia secondary to a complete absence of perfusion to the previously perfused myocardium [5]. Expedited treatment of STEMI with percutaneous coronary intervention (PCI) or thrombolysis, has been shown to improve outcomes [9]. According to the 2018 Acute Coronary Syndrome Israeli Survey (ACSIS), about 36–40% of all ACS were associated with electrocardiographic evidence of STEMI [10,11]. The door-to-balloon time within 90 min of presentation is recommended by the current guidelines [5]. However, the PCI-within-90 min goal is commonly hampered by patient-related factors, delayed presentation, commuting times, and in-hospital system-associated challenges.
The ongoing outbreak of coronavirus disease 2019 (COVID-19), an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has become a rapidly evolving global pandemic that impacted millions of people worldwide. From a clinical standpoint, current reports emphasize that COVID-19 outbreak limit the application of the standards of care for STEMI patients with altered procedures at all levels, unforeseen delays with dramatic consequences in ACS management. Furthermore, during the current pandemic, hospitals around the world have reported a substantial reduction in ACS admissions and reduced number of cardiac procedures [12,13].
In this study, we evaluated the impact of COVID-19 on the TIT in patients with STEMI undergoing primary PCI at our hospital.
2. Methods
2.1. Study design
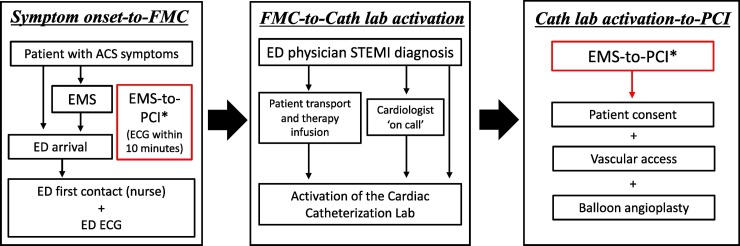
The study was performed at Barzilai Medical Center, a 617-bed hospital, in Ashkelon area in southern Israel. The hospital serves a population of 500,000, with more than 100,000 admissions annually. For this single centered, retrospective study, TIT ACS intervals for STEMI patients were recorded from July 2018 until June 2020 using a pre-determined time report spreadsheet. TIT intervals and delays assessment were simplified by dividing TIT into three different stages 1) symptom's onset-to-first medical contact (FMC), 2) FMC-to-catheter lab activation, and 3) catheter lab activation-to-PCI (Fig. 1 ) [6]. Based on reports by the Ministry of Health, February 2020 was selected as the beginning of the coronavirus outbreak as reports of infected patients were noted from hospitals around the country. The study population included 212 patients with STEMI on which primary PCI was performed. The cohort was further divided into two groups, 176 patients with a conventional STEMI protocol (before COVID-19) and 36 with STEMI protocol during the COVID-19 pandemic (COVID-19).
Fig. 1.
Classification of total ischemic time during COVID-19 pandemic. The different stages of time delays from onset of symptoms until reperfusion therapy. TIT intervals are divided into hospital independent delays (symptom onset-to-FMC) and in-hospital delays (FMC-to-cath lab activation, and cath lab activation-to-PCI). *A clear EMS-STEMI diagnosis even during COVID-19 pandemic mandates direct and immediate catheterization lab activation to minimize total ischemic time at any given time as before COVID-19 pandemic. ECG should be performed within 10 min upon arrival. TIT, total ischemic time. FMC, first medical contact. EMS, emergency medical service. STEMI, ST-segment elevation myocardial infarction. ECG, electrocardiogram. ED, emergency department. PCI, percutaneus coronary intervention.
2.2. Pre-revascularization protocol
We registered TIT intervals from onset of symptoms to PCI procedure. Pre-hospital data was provided by the emergency medical service (EMS) upon patient arrival. Patient admission to the emergency department (ED), and initial evaluation and ECG assessment was performed by the nursing staff. Upon STEMI diagnosis by the ER physician, the on-call cardiologist was notified for further patient evaluation. If the decision to proceed to primary PCI is made, the Cath lab team is activated and assumes the responsibility of recording the time interval information into the time report spreadsheet. The route from the ED to the Cath lab at our hospital is approximately 200 m and involve the use of an elevator in a two stories ride. When a STEMI diagnosis is known prior to hospital arrival, the cardiologist is informed in advance to wait for the patient at the ED. After the procedure, the timeline report spreadsheet is revised and signed by the chief interventional cardiologist and transferred to our institutional quality control department. The study protocol adhered to the declaration of Helsinki and was approved by the institutional review board of Barzilai Medical Center (BRZ-0113-20).
2.3. Statistical analysis
The results are presented as the mean ± standard deviation (SD) for continuous variables with normal distribution, and as number and percentage for categorical data. t-test was used for comparison of continuous variables. Proportions were compared with contingency tables followed by either Fisher's exact test or Chi-square depending of the variable category. A two-sided p-value <0.05 was considered statistically significant. Statistical analysis was performed with GraphPad Prism version 8.4.3 for Mac, GraphPad Software, La Jolla California USA.
3. Results
We analyzed data from 212 patients further divided into two groups, 176 patients with STEMI before the COVID-19 (Before COVID-19 group) and 36 with STEMI during the COVID-19 pandemic (COVID-19 group). Patients in both groups were predominantly male (83% vs. 89%), and older (61 vs. 59 years old). No significant differences between the two groups were observed in gender, age, BMI or comorbidities including hyperlipidemia, past cardiac family history, smoking, past ischemic heart disease or cerebrovascular accident, hypertension, diabetes mellitus, peripheral vascular disease, and Troponin T negative results at admission (Table 1 ). During the COVID-19 pandemic, we observed a significant increase in STEMI hospitalizations during the morning shift, however, before the pandemic hospitalizations were evenly distributed throughout the day (p = 0.043, Table 2 ). STEMI cases were also evenly distributed throughout the week, with a slightly increased percentage of STEMI cases on Thursdays (p = 0.69). The time interval from symptom onset to hospital arrival, obtained during history taking in the ED, accounted for an average of 174.6 ± 213.8 min compared to 158.5 ± 162.3 min during the COVID-19 pandemic. Despite a reduction in 16 min, no significant statistical differences were observed (p = 0.698). Time from symptoms onset to PCI was 231 ± 199 min compared to 229 ± 157.4 min recorded during COVID-19 pandemic (p = 0.949). In-hospital time intervals indicated a 9 min delay in door-to-ECG time (9.43 ± 18.21 vs. 18.41 ± 28.34, p = 0.029, Table 2, Fig. 2 ). The average time-interval from ECG-to-balloon increased by 16 min (58.25 ± 22.59 vs. 74.39 ± 50.30, p = 0.004, Table 2, Fig. 2). In addition, the door-to-balloon time experienced a 12 min delay (57.41 ± 27.52 vs. 69.31 ± 54.14, p = 0.04, Table 2, Fig. 2). No increased mortality, from admission to PCI, was observed when both time periods were compared (15 vs. 0, p = 0.08).
Table 1.
Characteristics of patients admitted to the emergency department with STEMI before and during the COVID-19 pandemic.
| Before COVID-19 |
COVID-19 |
p-value | |
|---|---|---|---|
| (n = 176) | (n = 36) | ||
| Male gender | 146 (83) | 32 (89) | 0.46 |
| Age (mean ± SD) | 61 ± 12.9 | 59 ± 11.73 | 0.62 |
| BMI (mean ± SD) | 27.67 ± 4.55 | 27.67 ± 4.15 | 0.99 |
| Hyperlipidemia | 82 (46.5) | 13 (36) | 0.27 |
| Past family history | 22 (12.5) | 5 (14) | 0.78 |
| Smoking (Current) | 77 (44) | 12 (33) | 0.27 |
| Past CAD or cerebrovascular accident | 45 (25.5) | 5 (14) | 0.19 |
| Hypertension | 86 (49) | 13 (36) | 0.20 |
| Diabetes mellitus | 60 (34) | 9 (25) | 0.33 |
| Peripheral vascular disease | 9 (5) | 0 (0) | 0.36 |
| Troponin T negative at admission | 30 (17) | 6 (17) | 0.99 |
SD, standard deviation. BMI, body mass index. CAD, coronary artery disease.
Table 2.
Comparison of time intervals in STEMI patients before and during the COVID-19 pandemic.
| Before COVID-19 | COVID-19 | p-value | |
|---|---|---|---|
| Time of day (daytime), n (%) | 0.043 | ||
| AM | 87 (49%) | 24 (66%) | |
| PM | 89 (51%) | 11 (33%) | |
| Day of the week | 0.69 | ||
| 1 | 26 (15%) | 7 (19%) | |
| 2 | 22 (13%) | 5 (14%) | |
| 3 | 27 (15%) | 2 (5%) | |
| 4 | 23 (13%) | 3 (8%) | |
| 5 | 30 (17%) | 8 (22%) | |
| 6 | 25 (14%) | 5 (14%) | |
| 7 | 23 (13%) | 6 (17%) | |
| Time from symptoms onset to first medical contact/nurse, minutes±SD, (95% CI) | 174.6 ± 213.8 (95% CI, 135.4–213.7) | 158.5 ± 162.3 (CI, 99.02–218.1) | 0.698 |
| Time from symptoms onset to PCI, minutes±SD, (95% CI) | 231.1 ± 199 (CI 198.1–264.1) | 229 ± 157.4 (CI 181.2–276.9) | 0.949 |
| Door-to-ECG time, minutes±SD, (95% CI) | 9.43 ± 18.21 (CI 6.19–12.67) |
18.41 ± 28.34 (CI 8.95–27.85) |
0.029 |
| ECG-to- ballon time, minutes±SD, (95% CI) | 58.25 ± 22.59 (CI 54.37–61.12) |
74.39 ± 50.30 (CI 58.51–90.27) |
0.004 |
| Door-to-balloon time, minutes±SD, (95% CI) | 57.41 ± 27.52 (CI 53.06–61.76) | 69.31 ± 54.14 (CI 54.09–84.54) | 0.04 |
1, Sunday. 2, Monday. 3, Tuesday. 4, Wednesday. 5, Thursday. 6, Friday. 7, Saturday. PCI, percutaneous coronary intervention. ECG, electrocardiogram. SD, standard deviation. 95% CI, confidence interval.
Fig. 2.
Comparison of In-hospital times before the pandemic (Before COVID-19) and during the pandemic (COVID-19). ECG, electrocardiogram. *p < 0.05. **p < 0.005.
4. Discussion
The impact of COVID-19 on ACS presentation and management has shaped the clinical scenario in our daily hospital practice. In line with other hospitals worldwide [[12], [13], [14]], we observed a reduction of hospitalization for STEMI, which in our hospital accounted for a 34.54% reduction. In this new clinical scenario, we hypothesized that the reduction in STEMI is caused by a less stressful home-based work environment and a patient's fear of being admitted to the hospital, especially during lockdown.
The best ACS clinical outcomes are achieved by reducing the time from symptom onset until reperfusion or TIT. TIT is one of the most critical parameters that strongly correlated with infarct size and mortality [6,15,16]. The current guidelines of the European Society of Cardiology (ESC) and the American Heart Association (AHA) for the management of patients with STEMI emphasize the importance in TIT reduction strategies [5,17]. In particular, the ESC guidelines advocate for an ECG diagnosis within 10 min upon chest pain presentation, and a door-to-balloon time within 90 min of STEMI diagnosis [5]. In fact, TIT can be divided into three different stages 1) symptom's onset-to-FMC, 2) FMC-to-catheter lab activation, and 3) catheter lab activation-to-PCI [6]. Despite that our study did not show an overall reduction in TIT, no substantial delays were evidenced during the COVID-19 pandemic. As far as stage 1 is concerned, our study evidenced significant delays from symptoms onset to first medical contact. Despite a 16-min reduction in stage 1 delays during COVID-19, the results did not prompt statistically significant outcomes. The shorter symptom-to-FMC time observed during COVID-19 is in sharp contrast to data reported from US and Europe where this time interval was excessively prolonged [14,[17], [18], [19], [20]]. This reduction can be explained by a relatively milder impact of the pandemic medium-sized metropolis, combined with a faster commuting times caused by ‘lock-down’ restrictions issued by the government inviting citizens to stay at home, unless urgent needs should arise. Nevertheless, stage 1 still continues to be a major player in increased TIT interval overall. As far as the stage 2 delays are concerned, our catheterization lab is within walking distance to the ED, hence no significant delays were noted. Interestingly, our study shows that COVID-19 pandemic caused significant delays in stage 3, including ECG-to-balloon and door-to-balloon time. This fact can be explained by the additional tests carried out, the extra time for staff preparation to protect themselves with personal protection equipment against COVID-19, and delays on PCI-related activities. Detailed analysis of the three stages evidenced that despite no substantial delays were observed in stage 1, the delays accounted in stages 2 and 3 delays were due to COVID-19 protocols set in place at our facility which maintained TIT as before the pandemic. In addition, we maintained a door-to-balloon time under 90 min as prior to the pandemic hence, no increase primary PCI procedure time or increased mortality was observed and the quality of care was preserved. One of the reasons for this success is based on the ‘STEMI code’ set in place at our facility, thus when a STEMI diagnosis is made in the ER, a direct activation of the Cath lab team can be made by the ED physician [[21], [22], [23]]. The readiness of the patient for transport to the catheterization lab begins shortly after diagnosis, concomitantly to treatment in the ED. When the lab is ready, the ED is notified and the patient is urgently transferred, accompanied by a cardiologist (Fig. 1).
CRediT authorship contribution statement
Sharon Bruoha: Investigation, Methodology, Data curation, Visualization, Writing - review & editing. Chaim Yosefy: Supervision, Funding acquisition, Writing - review & editing. Enrique Gallego-Colon: Investigation, Writing - original draft, Formal analysis. Jonathan Rieck: Supervision, Writing - review & editing. Yan Orlov: Resources, Writing - review & editing. Azriel Osherov: Validation, Data curation, Writing - review & editing. Abu Hamed Jihad: Validation, Data curation, Writing - review & editing. Yaniv Sherer: Resources, Data curation, Writing - review & editing. Nasi Viki: Methodology, Writing - review & editing. Jamal Jafari: Conceptualization, Project administration, Writing - review & editing.
5. Conclusion
During the COVID-19 pandemic, we observed a reduction in STEMI hospitalizations. Despite the delays observed throughout patient's cardiovascular care along with the additional extraordinary measures to protect staff and patients from viral transmission, the delays were within the 90 min door-to-balloon window with no associated increased mortality.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Virani S.S., Alonso A., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P., et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141 doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Israel Central Bureau of Statistics. Causes of death in Israel . 2016. State of Israel, 2020. [Google Scholar]
- 3.Brodie B.R., Webb J., Cox D.A., et al. Impact of time to treatment on myocardial reperfusion and infarct size with primary percutaneous coronary intervention for acute myocardial infarction (from the EMERALD trial) Am J Cardiol. 2007;99(12):1680–1686. doi: 10.1016/j.amjcard.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 4.Gallego-Colon E., Oliver E. Stem Cell Genetics for Biomedical Research: Past, Present, and Future. Springer International Publishing; 2018. Cardiac stem cells: a plethora of potential therapies for myocardial regeneration within reach; pp. 135–171. [Google Scholar]
- 5.Ibanez B., James S., Agewall S., et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 6.Denktas A.E., Anderson H.V., McCarthy J., Smalling R.W. Total ischemic time. JACC Cardiovasc Interv. 2011;4:599–604. doi: 10.1016/j.jcin.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Kumar A., Cannon C.P. Acute coronary syndromes: diagnosis and management, part I. Mayo Clin Proc. 2009;84(10):917–938. doi: 10.1016/S0025-6196(11)60509-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collet J.-P., Thiele H., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 9.Gibson C.M., Pride Y.B., Frederick P.D., et al. Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1035–1044. doi: 10.1016/j.ahj.2008.07.029. [DOI] [PubMed] [Google Scholar]
- 10.ACSIS . 2018. Acute Coronary Syndrome Israeli Survey. [Google Scholar]
- 11.Porter A., Paradkar A., Goldenberg I., Shlomo N., Cohen T., Kornowski R., et al. Temporal trends analysis of the characteristics, management, and outcomes of women with acute coronary syndrome (ACS): ACS Israeli survey registry 2000-2016. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.014721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashraf S., Ilyas S., Alraies M.C. Acute coronary syndrome in the time of the COVID-19 pandemic. Eur Heart J. 2020;41(22):2089–2091. doi: 10.1093/eurheartj/ehaa454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pessoa-Amorim G., Camm C.F., Gajendragadkar P., De Maria G.L., Arsac C., Laroche C., et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Hear J - Qual Care Clin Outcomes. 2020;6:210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020 May 15 doi: 10.1093/eurheartj/ehaa409. ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 16.Tarantini G., Cacciavillani L., Corbetti F., et al. Duration of ischemia is a major determinant of transmurality and severe microvascular obstruction after primary angioplasty: a study performed with contrast-enhanced magnetic resonance. J Am Coll Cardiol. 2005;46(7):1229–1235. doi: 10.1016/j.jacc.2005.06.054. [DOI] [PubMed] [Google Scholar]
- 17.ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction. Circulation. 2004;110 doi: 10.1161/circ.110.9.e82. [DOI] [Google Scholar]
- 18.McNair P.W., Bilchick K.C., Keeley E.C. Very late presentation in ST elevation myocardial infarction: predictors and long-term mortality. Int J Cardiol Heart Vasc. 2019;22:156–159. doi: 10.1016/j.ijcha.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mafham Marion M., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet (Lond Engl) 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roffi Marco, et al. The obstacle course of reperfusion for ST-segment-elevation myocardial infarction in the COVID-19 pandemic. Circulation. 2020;141(24):1951–1953. doi: 10.1161/CIRCULATIONAHA.120.047523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koh J.Q., Tong D.C., Sriamareswaran R., et al. In-hospital ‘CODE STEMI’ improves door-to-balloon time in patients undergoing primary percutaneous coronary intervention. Emerg Med Australas. 2018;30(2):222–227. doi: 10.1111/1742-6723.12855. [DOI] [PubMed] [Google Scholar]
- 22.Ahmar W., Quarin T., Ajani A., Kennedy M., Grigg L. Improvement in door-to-balloon times in management of acute ST-segment elevation myocardial infarction STEMI through the initiation of ‘Code AMI’. Intern Med J. 2008;38(9):714–718. doi: 10.1111/j.1445-5994.2007.01476.x. [DOI] [PubMed] [Google Scholar]
- 23.Bajaj S., Parikh R., Gupta N., et al. “code STEMI” protocol helps in achieving reduced door-to-balloon times in patients presenting with acute ST-segment elevation myocardial infarction during off-hours. J Emerg Med. 2012;42(3):260–266. doi: 10.1016/j.jemermed.2011.03.014. [DOI] [PubMed] [Google Scholar]