Abstract
KapWeb is an interactive tool for the determination of cancer survival rates based on case outcomes compiled from more than half a million records from cancer registries all over Japan, and we believe that both the tool and the call for data openness and transparency are important.

Abbreviations
- CSSR
Cancer Survivor's Survival Rate
- JACCC
Japanese Association of Clinical Cancer Centers
Dear Editors,
The year 2020 had been a challenging year especially for the medical community, as the coronavirus pandemic has caused much disruption to key healthcare areas such as cancer care. 1 For cancer patients, survivors and their loved ones, the uncertainty of weathering through the pandemic may compound into frustration and distrust, potentially leading some people to question the opaqueness, openness, and reliability of information such as survival rates and death statistics. The stability of healthcare necessitates a greater level of transparency, especially in key healthcare regions such as cancer. Even during ordinary times, only a minority of cancer patients receive proper information and psychological support about their care, 2 and physicians often overlook their patients’ uncertainties about the future. 3 Cancer incidence will continue to rise as societal demographics become more geriatric; however, are our healthcare systems ready to tackle the issue of transparency and open data in cancer incidence to provide cancer patients/survivors and their loves one the peace of mind they need to improve their quality of life? Although the process of retrospective collection of data for cancer registries may be reasonably mature and has not seen innovative changes, how do we present this information to the public in a directly relevant manner to ensure its usefulness and reliability? Japan, in particular, has a centralized cancer registration system that compiles records of cancer incidence from a number of specialized facilities; we have here developed KapWeb, 4 a companion database of cancer survival statistics, for both researchers and more importantly cancer survivors and their families, to provide a newfound layer of transparency and openness for interpreting cancer survival information.
Cancer survival rates are direct metrics that allow one to examine the probability of survival as the likelihood over time a cancer patient remains alive post‐diagnosis. Although survival rate data in Japan are available in 5‐y statistics from the JACCC as early as 2007, 5 , 6 as a whole these statistics are not centralized or readily curated for rapid visualization and comparison. KapWeb is an interactive database of cancer survival rate statistics for all JACCC member facilities and, after the addition of 10‐y survival rates as an output option, our most recent November 2020 update now incorporates more than half a million case records. To account for compounding effects behind factors such as gender, age, and demographic differences, we have elected to output graphically cancer‐specific relative survival rates, which are normalized by the expected survival rates of cancer‐free individuals in a population to illustrate the relative difference in survival. These relative survival rates are also useful for comparing data with countries around the world, as it removes possible bias as a consequence of difference in demographics. KapWeb statistics can be accessed via 2 data modes (Figure 1A,B): Simple Data generates survival statistics using cancer site, gender, and clinical stages, and Full Data allows additional criteria as filters, such as location of tumors, clinical stages, procedures, and the time elapsed since initial diagnosis. Either interface in KapWeb will generate a survival curve (Figure 1C), along with expert‐generated reports on therapeutic options and relevant summary statistics. Previous KapWeb searches are also cached to minimize recalculation and improve user experience.
FIGURE 1.
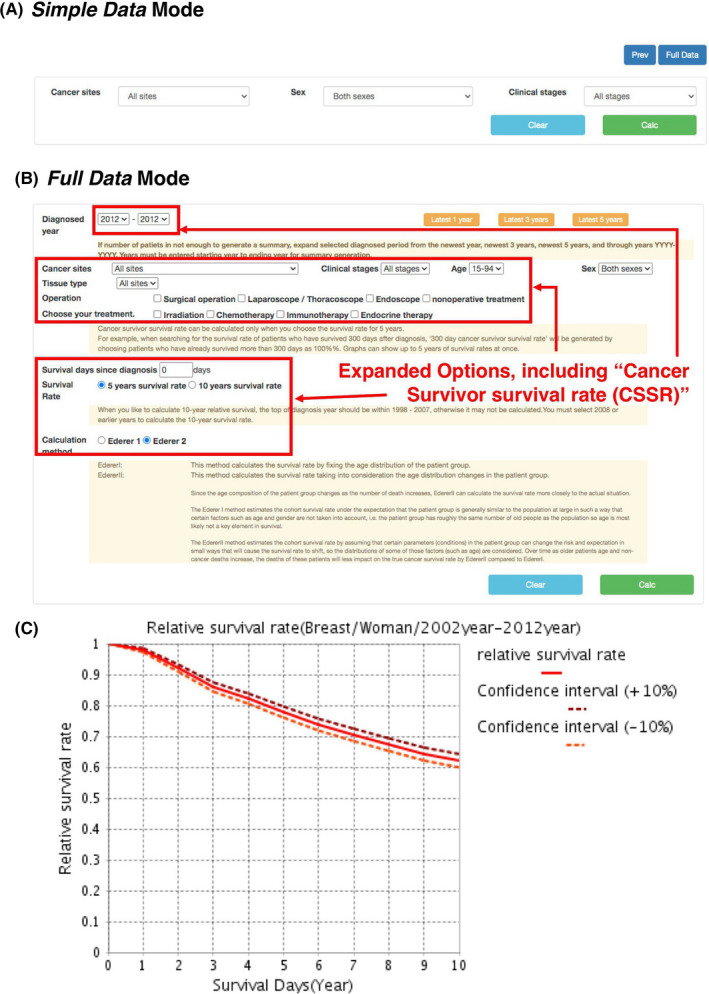
KapWeb interface and sample output. A, “Simple Data” mode parameter selection window. B, “Full Data” access mode parameter options, with expanded options over Simple Data mode highlighted in red. C, Sample relative 10‐y survival rate output for Stage III breast cancer cases (N = 1650) between 2002 and 2012; note that changes in survival rate remain relatively constant over this period
KapWeb also includes a unique feature in generating a conditional survival rate, which we term CSSR, Figure 2A,B), to provide an easier interpretation of how likely a cancer patient remains alive at a certain point in time post‐diagnosis, and a simpler metric for patients to gage and look forward to their recovery hopes; additionally, CSSR is useful for visualizing changes over time, for instance the relative improvement in 5‐y lung cancer survival prognosis over the period of 1997 to 2012 (Figure 2C). CSSR is calculated by specifying a number of days elapsed since diagnosis and either a 5‐y or 10‐y survival period, as well as either Ederer I or II method of estimation. 7 , 8 Ederer I assumes a fixed cohort age structure, while II allows expected survival rate to change as the age structure is altered due to death events. A CSSR, based on either of these reliable and robust estimators, 9 , 10 can provide a net cancer survival measure for patients in the absence of other causes of death, as the rate is normalized to the proportion of expected survivals in a comparable set of cancer‐free individuals.
FIGURE 2.
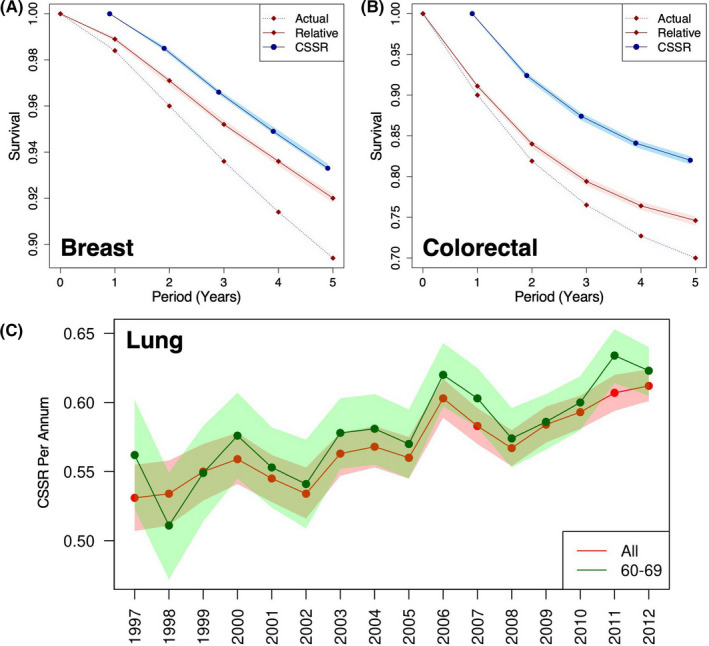
Utility of cancer survivor's survival rate (CSSR). Example comparisons of CSSR and actual survival rates for all stages of (A) breast and (B) colorectal cancers registered between 1997 and 2012 among female patients 15‐94 y of age. Dark blue circle, CSSR (N = 71 465 and 20 827 for breast and colorectal cancers, respectively); dark red diamonds, actual (corrected for demographics, dashed line) and relative (solid line) survival rates (N = 72 697 and 23 012 for breast and colorectal cancers, respectively). C, trends in 5‐y CSSR per annum for lung cancers (1997‐2012). Red, all ages; green, ages between 60 and 69. KapWeb statistics shown were conditionally adjusted to reflect a lapse period of 330 d after the initial diagnosis and rendered in R; shaded regions indicate 90% confidence intervals for the relative rates
Ever since Japan's first cancer registry in the 1950s, cancer registration has been constantly evolving, from the 1970s’ tissue/organ system‐specific approach, to the nationwide consolidation of municipality‐level registries under 2012’s National Cancer Registration Project directives. And now, cancer registration today has accumulated sufficient mass and scale to be meaningfully utilized for big data research and targeted therapeutic studies, as most hosts of cancer registry transform and double in function as biobanks and repositories of patient histories and even sequencing data in a newfound synergy with other modern onco‐therapeutic developments. Nevertheless, to further the goal of maintaining transparency and openness for public health efforts, cancer registries today still require continual improvements, for instance with JACCC the curation of underserved cancer types, eg, childhood cancers, may narrow the gap in a number of statistics and help cancer patients and their physicians chart a better plan for the future.
The shakeup of 2020 is irreversibly transforming our lives, as we become acquainted with mask wearing and social distancing. Certainly, these changes will affect how the medical community provides cancer care, as we move forward and readjust to a new normal. Cancer will always be a public health issue, and a key element in maintaining order with public health problems is the instillation of confidence, which can only come with greater transparency and openness. In this grand scheme, while tools such as KapWeb may seem inconsequential, but just like the simple act of wearing masks as a COVID‐19 countermeasure, when every little incremental step helps, then as the English writer Charles Dicken may have said, “it [shall be] a far, far better thing that [we] do than [we] have ever done [in the end].”
CONFLICT OF INTEREST
The authors have no conflict of interest.
ACKNOWLEDGMENTS
Collection, statistical analysis and reporting of the Japanese Association Clinical Cancer Centers survival data for KapWeb is partly supported by the Cancer Research and Development Fund (2020‐A‐20) of the National Cancer Center Japan.
Contributor Information
Haruo Mikami, Email: hmikami@chiba-cc.jp.
Hiroki Nagase, Email: hnagase@chiba-cc.jp.
REFERENCES
- 1. Maringe C, Spicer J, Morris M, et al. The impact of the COVID‐19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population‐based, modelling study. Lancet Oncol. 2020;21:1023‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. All.Can Initiative . Patient insights on cancer care: opportunities for improving efficiency; 2019. www.all‐can.org/what‐we‐do/research/patient‐survey/. Accessed December 21, 2020.
- 3. Chandwani KD, Zhao F, Morrow GR, et al. Lack of patient‐clinician concordance in cancer patients: Its relation with patient variables. J Pain Symptom Manage. 2017;53(6):988‐998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. KapWeb . kapweb.chiba‐cancer‐registry.org. Accessed November 19, 2020.
- 5. Saruki N, Mikami H. Survival statistics publication and web‐based calculation publication of survival rates by the Japanese Association of Clinical Cancer Centers. JACR Monogr. 2012;17:22‐27. [Google Scholar]
- 6. Higashi T, Nakamura F, Saruki N, Sobue T. Establishing a quality measurement system for cancer care in Japan. Jpn J Clin Oncol. 2013;43(3):225‐232. [DOI] [PubMed] [Google Scholar]
- 7. Ederer F, Axtell LM, Cutler SJ. The relative survival rate: a statistical methodology. Natl Cancer Inst Mongr. 1961;6:101‐121. [PubMed] [Google Scholar]
- 8. Ederer F, Heise H. Instructions to IBM 650 Programmers in Processing Survival Computations. Methodological note no. 10. End Results Evaluation Section. Bethesda, MD: National Cancer Institute; 1959. [Google Scholar]
- 9. Lambert PC, Dickman PW, Rutherford MJ. Comparison of different approaches to estimating age standardized net survival. BMC Med Res Methodol. 2015;15:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hakulinen T, Seppa K, Lambert PC. Choosing the relative survival method for cancer survival estimation. Eur J Cancer. 2011;47(14):2202‐2210. [DOI] [PubMed] [Google Scholar]


