Abstract
Given the scarcity of safe and effective COVID-19 vaccines, a chief policy question is how to allocate them among different sociodemographic groups. This paper evaluates COVID-19 vaccine prioritization strategies proposed to date, focusing on their stated goals; the mechanisms through which the selected allocations affect the course and burden of the pandemic; and the main epidemiological, economic, logistical, and political issues that arise when setting the prioritization strategy. The paper uses a simple, age-stratified susceptible–exposed–infectious–recovered model applied to the United States to quantitatively assess the performance of alternative prioritization strategies with respect to avoided deaths, avoided infections, and life-years gained. We demonstrate that prioritizing essential workers is a viable strategy for reducing the number of cases and years of life lost, while the largest reduction in deaths is achieved by prioritizing older adults in most scenarios, even if the vaccine is effective at blocking viral transmission. Uncertainty regarding this property and potential delays in dose delivery reinforce the call for prioritizing older adults. Additionally, we investigate the strength of the equity motive that would support an allocation strategy attaching absolute priority to essential workers for a vaccine that reduces infection-fatality risk.
Keywords: Vaccine allocation, COVID-19, Equity, SEIR model
1. Introduction
As of February 2021, the novel coronavirus disease 2019 (COVID-19) has caused more than 2.5 million deaths globally [1] and triggered a major recession, with the global economy shrinking by an estimated 4.4% in 2020 [2]. Given the substantial economic, social, emotional, and mental health costs of non-pharmaceutical interventions (e.g., social and physical distancing, mask-wearing, and economic lockdowns), vaccinating a large proportion of the population is considered the best strategy to address this crisis. The race to develop safe and effective COVID-19 vaccines has proceeded at an unprecedented pace [3]. In less than a year, more than 300 candidate vaccines have been developed, with approximately 80 candidates currently in clinical trials and 11 already approved for full or restricted use in several countries, including Canada, China, Russia, the United Kingdom, and the United States [4].
Despite the approval of multiple vaccines, widespread availability and access is not anticipated for at least several more months. The limited supply of vaccine doses at the beginning of the vaccination campaign has raised the question of how best to allocate them among sociodemographic groups. Although vaccine prioritization strategies under constrained resources have previously been established for other outbreak pathogens (e.g., pandemic H1N1 influenza in 2009 [5] and Ebola in 2013–2016 [6]), several characteristics of COVID-19 preclude adoption of these pre-existing frameworks. First, unlike with other respiratory infectious diseases, children have low susceptibility to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the virus that causes COVID-19) infection [7] and low infection-fatality risk [8], although contagiousness in children varies across variants [9]. Therefore, the commonly used strategy of prioritizing children in vaccine allocation [10] (due to either high risk of severe consequences or high risk of transmission to others) may be suboptimal for COVID-19† . In addition, approved COVID-19 vaccines have not yet been adequately tested in children. Second, older adults are at high risk of death from COVID-19 but tend to have fewer social interactions than younger individuals, especially with the implementation of social distancing. In contrast, individuals involved in activities essential for pandemic control and the functioning of society are exposed to a significantly higher risk of infection. Finally, the pandemic has exacerbated pre-existing health and economic inequities, with disproportionate rates of death and severe infection among ethnic minorities and socioeconomically disadvantaged groups [11], [12]. Over-representation in essential jobs, socially determined high prevalence of comorbid conditions, and increased likelihood of living in crowded, intergenerational housing among these groups contribute to these disparities [13].
Many countries have issued or are developing guidelines for COVID-19 vaccine prioritization strategies. These guidelines generally aim to maximize overall good in consideration of both health- and non-health-related outcomes while accounting for the specific epidemiological characteristics of the pandemic (e.g., age differences in transmission and mortality rates). Many of the guidelines also seek to be sensitive to equity concerns related to pre-existing health and economic conditions as well as pandemic-specific differential health and economic impacts across sociodemographic groups. A highly debated issue is whether essential workers should be prioritized over older adults and individuals with serious medical conditions, despite the fact that the latter groups are at considerably higher risk of severe COVID-19-related illness and death [14]. Factors supporting the prioritization of essential workers include their key role in viral transmission due to their relatively high rates of interpersonal contacts and social justice concerns given that a large proportion of essential workers are from socioeconomically disadvantaged and vulnerable populations.
In this paper, we develop an age-stratified susceptible–exposed–infectious–recovered (SEIR) model that differentiates individuals (via contact rates under social distancing) based on their essential worker status. We employ the model to investigate the optimal ranking of alternative vaccine prioritization strategies for minimizing the total number of COVID-19 infections, the number of deaths, or the number of years of life lost over the full course of the pandemic. The model is applied to the United States. We find that prioritizing essential workers minimizes the number of infections, and, if the vaccine is sufficiently effective at blocking transmission, this strategy also minimizes the number of years of life lost. Prioritizing essential workers minimizes the number of deaths in scenarios in which the pandemic is well-controlled, for example, there is a low number of active infections when the vaccine is distributed or non-pharmaceutical interventions are sufficiently stringent to curb transmission. However, in most scenarios, prioritizing the elderly yields the largest reduction in the number of deaths, even with a vaccine that is effective at blocking viral transmission. Uncertainty about this property and potential delays in the delivery of vaccine doses reinforce the call for prioritizing the elderly.
Further, we evaluate the strength of the equity motive required to support prioritization strategies that do not necessarily maximize the selected health objective. In particular, given that many essential workers belong to vulnerable populations, a social justice argument exists for assigning them increased weight in any prioritization strategy [15]. We find that an equity weight of greater than six would have to be assigned to essential workers in comparison with the elderly in order to support the prioritization of essential workers when the vaccine does not curb transmission.
This paper builds on and extends the growing literature on COVID-19 vaccine prioritization strategies. Previous papers have predominantly employed age-stratified deterministic SEIR models and focused on the trade-off between prioritizing high-contact individuals versus high-risk individuals [16], [17], [18], [19], [20], [21]. In contrast, an agent-based model was adopted by Chen et al. [22]. Several studies have included essential workers in their models and considered the relative benefits of vaccinating essential workers prior to vaccinating older adults [23], [24]. Epidemiological differences according to age and occupation were also considered by Babus et al. [25] in a model lacking infection dynamics; the main result of this study was that older individuals with high-risk occupations should be vaccinated first. Moore et al. [26] considered the trade-off between vaccination of older adults and individuals with comorbidities in the United Kingdom and concluded that the former should be prioritized. Some studies have also focused on behavioral changes associated with non-pharmaceutical interventions or fear of infection and the potential relevance of these changes to vaccine prioritization strategies [27], [28], [29]. Finally, Castonguay et al. [30] examined the issue from a spatial perspective and recommended targeting of regions with low initial infection burden.
We contribute to this literature by examining the relative importance of a set of variables in the ranking of socio-demographic groups (including essential workers). These variables include speed of vaccine rollout, initial epidemiological conditions, strength of non-pharmaceutical interventions, and uncertainty over the ability of the vaccine to curb transmission. The main novel contribution of our paper is the analysis of equity weights. The paper is structured as follows: Section 2 discusses prominent guidelines that have been proposed for COVID-19 vaccine allocation, focusing on the underlying ethical goals and their application; Section 3 describes a modeling exercise calibrated to the US population and associated results; and Section 4 summarizes our conclusions.
2. Evaluation of proposed guidelines for COVID-19 vaccine allocation
Table 1 summarizes selected national-level guidelines that have been proposed for COVID-19 vaccine allocation [31], [32], [33], [34], [35], [36], [37]. Most guidelines share the ethical objectives of promoting some form of overall good (e.g., individuals’ aggregate well-being or cumulative health and non-health benefits) and social justice, often in the form of preferring vaccine allocation strategies that prevent harm to the worst-off, however defined. Other social justice considerations include equal concern for all individuals, reducing health disparities, and promoting fairness.
Table 1.
Selected guidelines for COVID-19 vaccine allocation.
| Proposal/organization | Ethical principles | Goals | Prioritization |
|---|---|---|---|
| US National Academies of Sciences, Engineering, and Medicine [31] |
|
|
Phase 1a (5% of the population): high-risk health workers and first responders Phase 1b (10% of the population): people of all ages with comorbid and underlying conditions that put them at significantly higher risk; older adults living in congregate or overcrowded settings Phase 2 (30%–35% of the population): K–12 teachers, school staff, and childcare workers; critical workers in high-risk settings (e.g., food-processing facilities); all older adults; individuals of all ages with health conditions that put them at moderately higher risk of severe COVID-19 disease; people in homeless shelters, group homes for individuals for disabilities, and correctional facilities, and the staff working in those settings Phase 3 (40%–45% of the population): young adults and children; workers in industries and occupations important to the functioning of society and at increased risk of exposure Phase 4: everyone else Within each specified population group (e.g., “all older adults” or “critical workers in high-risk settings”), a vulnerability index, such as the Centers for Disease Control (CDC). CDC’s Social Vulnerability Index, should be used to identify and prioritize geographic areas that have attributes that are associated with increased vulnerability to severe COVID-19 outcomes. |
| Johns Hopkins Center for Health Security [32] |
|
Tier 1: individuals at greatest risk of severe illness and death and their caregivers; people essential to sustaining the ongoing COVID-19 response; individuals most essential to maintaining core societal functions Tier 2: people at elevated risk of infection; individuals essential to broader health provision and to maintaining other essential services; individuals with least access to healthcare |
|
| US Centers for Disease Control and Prevention interim guidelines, December 22, 2020 [33] |
|
|
Phase 1a: healthcare personnel and residents of long-term facilities Phase 1b: frontline essential workers and adults 75+ Phase 1c: adults with high-risk medical conditions; adults 65+; other essential workers |
| UK Joint Committee on Vaccination and Immunisation [34] | None stated |
|
(1) Residents in a care home for older adults and their caretakers (2) All those 80 years of age and over and frontline health and social care workers (3) All those 75 years of age and over (4) All those 70 years of age and over and clinically extremely vulnerable individuals (5) All those 65 years of age and over (6) All individuals aged 16 years to 64 years with underlying health conditions that put them at higher risk of serious disease and mortality (7) All those 60 years of age and over (8) All those 55 years of age and over (9) All those 50 years of age and over |
| World Health Organization (WHO) COVID-19 Vaccine Global Access Facility (COVAX) guidelines [35] | None stated |
|
|
| WHO Strategic Advisory Group of Experts on Immunization Values Framework [36] |
|
•Contribute significantly to the equitable protection and promotion of human well-being | High risk of severe disease and death; high risk of being infected; high transmission risk; vulnerable groups at risk of disproportionate burden; those who bear significant additional risks and burdens of COVID-19 to safeguard the welfare of others (e.g., health workers and essential workers) |
COVAX is an initiative coordinated by the WHO, Gavi, the Vaccine Alliance, and the Coalition for Epidemic Preparedness Innovations to support the research, development, and manufacturing of COVID-19 vaccine candidates and to promote the fair distribution of vaccines among participating countries.
All guidelines recognize the importance of preserving population health and concur that the foremost aim of an optimal vaccine allocation strategy should be to maximize health outcomes. This translates into selecting prioritization rules that avert, for example, the largest numbers of deaths, cumulative infections, or severe disease cases, depending on the relative importance attributed to nonfatal health conditions and potential long-term sequelae. Two key epidemiological factors determine the variation in these population-wide health outcomes depending on which sub-groups are targeted for vaccination: ① the infection and transmission rates for individuals in each group (i.e., the probability of being infected by the virus and transmitting it), and ② the probable severity of health outcomes given an infection in each group (e.g., the infection-fatality risk or probability of severe symptoms).
Older adults and individuals with serious medical conditions are at greatest risk of severe health outcomes from COVID-19, while essential workers are at greatest risk of infection and subsequent transmission because of their relatively high number of interpersonal contacts during the pandemic. Targeting the latter for vaccination will undoubtedly prevent the greatest number of cumulative infections. However, if the primary goal is to prevent deaths or severe infections, a potential trade-off exists between prioritizing high-severity-risk individuals versus high-contact ones. If the administered vaccines are able to block transmission of SARS-CoV-2, prioritizing high-contact individuals may be the optimal strategy despite their lower risk of severe health sequelae compared to high-severity-risk individuals.
Most published guidelines prioritize high-severity-risk individuals (e.g., older adults and individuals with comorbidities) during the early stages of vaccine allocation. One exception was the initial guidelines issued by the US Centers for Disease Control and Prevention, which prioritized essential workers over older adults and those with pre-existing conditions, with the exception of older adults living in long-term care facilities [37]. On December 22, 2020, these guidelines were partially revised in favor of adults aged 75 years and older and frontline essential workers (e.g., first responders, educators, and grocery store workers), with the latter representing a narrower category than all essential workers [38].
Uncertainty regarding the effectiveness of existing COVID-19 vaccines in blocking transmission provides additional rationale for prioritizing older adults over high-contact individuals if the primary goal is to minimize the number of deaths [39]. Indeed, clinical trials to date have focused on the efficacy of candidate vaccines in preventing cases of COVID-19 among vaccinated individuals as their primary endpoints and have not assessed the candidates’ efficacy in preventing secondary infections. Alternatively, any uncertainty regarding the effectiveness of COVID-19 vaccines in older individuals provides support for prioritizing essential workers.
Of note, the definition of “essential worker” is not uniform across guidelines. For instance, in the United Kingdom, only frontline health and social care workers are prioritized based on their work responsibilities. The definition of “essential” provided by the US Department of Homeland Security (DHS) is broader and encompasses all individuals with a high risk of exposure and those with occupations that are considered crucial for the functioning of society (including healthcare workers, grocery store clerks, educators, accountants, and engineers). Based on this definition, nearly 70% of the US workforce is considered essential [40].
Most guidelines explicitly appeal to the principle of maximizing overall benefits (as opposed to only direct health benefits, such as reductions in COVID-19 deaths or infections). Nevertheless, indirect health and non-health considerations are often overlooked in the concrete recommendations. In principle, at least four such outcomes could affect the selection of the optimal vaccine prioritization strategy. First, the need to preserve health system capacity encourages prioritization of essential workers involved in healthcare activities. Second, permitting certain workers to return safely to their workplace has economic benefits, assuming that the work cannot be effectively performed at home. For example, prioritizing educators (and children) may promote in-person instruction, thereby minimizing educational gaps with pre-pandemic generations and reducing the inequalities in learning between children belonging to high and low socioeconomic groups. Prioritizing the educational sector may also benefit other economic sectors because relieving parents from childcare enables them to work more hours and more productively. Third, specific vaccine allocations may disproportionately reduce the negative social and mental health impacts of the pandemic—for example, by prioritizing the elderly, who are particularly vulnerable to loneliness and isolation due to their smaller social networks. Finally, different allocation strategies may entail different costs, depending on the capacity of healthcare systems to deliver vaccines to various sociodemographic groups (e.g., vaccinating children at school may be easier than vaccinating other age groups) and on vaccine properties (e.g., logistical constraints related to the cold chain required by some vaccines may prevent widespread distribution in remote or under-resourced areas).
In addition to maximizing health and non-health outcomes, ethical considerations may support the prioritization of specific sociodemographic groups. An often-cited ethical issue concerns differences in life expectancy. If accounting not only for the number of avoided deaths, but also for the life expectancy or health-quality-adjusted life expectancy of those saved lives is considered ethically justifiable, vaccinating the young and individuals without serious medical conditions is more of a priority [41]. This may also translate into prioritizing essential workers over the elderly or individuals with comorbidities.
Most guidelines also highlight ethical concerns for prioritizing the worse-off. Structural inequities in society have devalued certain lives, including those of racial and ethnic minorities or socioeconomically vulnerable populations. Moreover, these pre-existing structural inequities have tended to compound the effects of COVID-19 in affected groups, resulting in increased rates of infection and death among already worse-off populations. Therefore, societal interest in not exacerbating (and perhaps even correcting for) existing health, social, and economic inequities may call for additional prioritization of vulnerable populations, beyond what is called for by immediate health concerns.
Given that socioeconomically vulnerable populations are disproportionately represented among essential workers, a social justice argument exists for prioritizing this group beyond epidemiological reasons associated with the higher probability of viral infection and transmission among high-contact individuals. Although essential workers may not necessarily be at the highest risk of severe health outcomes and death, prioritizing this group in the allocation of COVID-19 vaccines will adjust for harms they have experienced due to their vulnerable condition and mitigate exacerbation of existing inequities. Additionally, prioritization of essential workers in vaccine allocation may be ethically justifiable based on reciprocity and compensation for their social contribution during the pandemic.
3. Modeling exercise
3.1. Theoretical framework
We evaluated the impacts of alternative vaccine prioritization strategies using a deterministic age-stratified compartmental model. We divided the US population into nine age groups: 0–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80+ years old. We further subdivided each of the 20–29, 30–39, 40–49, and 50–59 years old age groups into two subgroups based on the proportion of essential workers, resulting in a total of 13 sociodemographic groups. Our definition of essential workers includes all workers who are involved in activities considered “essential” by the DHS [40] and are unable to work remotely. These essential workers constitute 42% of the workforce and on average are less educated, have lower wages, and are more likely to come from disadvantaged minority groups compared to the general workforce [42]. The age stratification reflects both epidemiological and behavioral (i.e., associated with social interaction patterns) differences; the main distinction between essential workers and the rest of the population in the model is the ability to practice effective social and physical distancing (i.e., reducing one’s number of contacts).
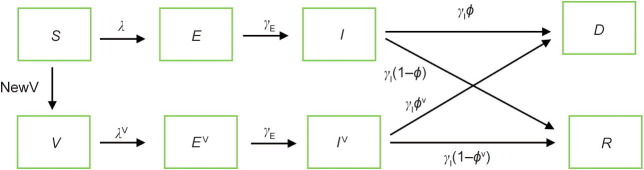
For each sociodemographic group, the model tracks the following health states: susceptible (S), exposed (E), infectious (I), recovered (R), dead (D), vaccinated and potentially susceptible (V), vaccinated and exposed (E V), and vaccinated and infectious (I V). A schematic of this model is presented in Fig. 1 . Model equations and calibration details are presented in Appendix A. All individuals are assumed to be initially susceptible (S) unless they have recovered from an infection or have been effectively vaccinated. Recovered individuals are considered immune to reinfection, and the vaccine, if effective, confers immunity to the disease. Susceptible individuals transition to the exposed state E after contact with an infectious person, provided that the contact transmitted the virus. After a latent period, exposed individuals become infectious (I). After an infectious period, they either recover (R) or die (D).
Fig. 1.
Diagram of the SEIR model with vaccination. The variables next to the arrows denote the probability of transitioning from one compartment to the next. Probabilities marked with the superscript V may have been altered by vaccination. λ and λV represent the probabilities of infection. γE is the probability of transitioning from the exposed to the infectious state. is the probability of exiting the infectious states I and IV. and represent the infection-fatality rates. denotes the number of individuals vaccinated in a single day.
In each period, a proportion of individuals are vaccinated and move from the susceptible to the vaccinated health state (with NewV denoting the number of individuals vaccinated in a period). For two-dose vaccines, such as the BioNTech (Germany)-Pfizer (USA) and Moderna (USA) vaccines currently in use in the United States, the transition from susceptible to vaccinated can be interpreted as the moment when the second vaccine dose takes effect (although, in reality, some protection is offered already after the first dose [43], [44]). We assumed three distinct effects of the vaccine:
(1) The vaccine reduces the susceptibility rate of the vaccinated individual, that is, the probability that the individual becomes infected upon contact with an infectious individual. If the vaccinated individual is infected, then they transition to the exposed state and, after a latent period, to the infectious state . A reduction in the susceptibility rate implies a reduction in the probability of infection , with . After an infectious period, the individual either recovers or dies. If the vaccine is 100% effective at preventing infection, then the probability of being infected and transitioning to the exposed state is zero.
(2) The vaccine reduces the infection-fatality rate of the vaccinated individual, that is, the probability that the vaccinated individual, once infected, transitions to the death state rather than the recovered state. If the vaccine is 100% effective at preventing severe disease (death in this case), vaccinated individuals may still be infected with SARS-CoV-2, but they will not experience further health consequences.
(3) The vaccine reduces the infectiousness of the vaccinated individual, that is, the probability that a vaccinated individual, once infectious, transmits the virus to other individuals. If the vaccine is 100% effective at preventing transmission, vaccinated individuals may still be infected with SARS-CoV-2 and experience severe health consequences from COVID-19 (represented by death in the model), but they will not infect other individuals. This corresponds to a reduction in of other individuals.
A vaccine that reduces the risk of infection will reduce the number of deaths among vaccinated individuals compared to unvaccinated individuals and reduce the number of cases of transmission from a vaccinated infectious individual compared to an unvaccinated infectious individual. A vaccine that only reduces the infection-fatality rate does not prevent individuals from being infected and transmitting the virus but will reduce the number of severe infections among vaccinated individuals compared to unvaccinated individuals. This type of vaccine only confers direct benefits to vaccinated individuals but does not affect disease transmission. Finally, the vaccine may be more effective at reducing the risk of severe health consequences than transmission risk, independent of its effects on initial infection risk.
Modeling these three effects separately enables us to investigate how the optimal allocation of vaccine doses varies according to specific properties of the vaccine. Results from phase III clinical trials have indicated that COVID-19 candidate vaccines are effective at protecting vaccinated individuals from clinical disease, thereby reducing the fatality risk. However, the extent to which approved vaccines reduce risk of infection (including asymptomatic infection) and transmission is unclear [39], [45]. Therefore, in the main analysis, we focused on two types of vaccines: ① a vaccine that reduces infection risk that, consequently, also reduces the number of fatalities and transmissions and ② a vaccine that reduces the risk of transmission and risk of death at different rates.
In the model, an individual’s age is correlated with their daily number of contacts, their susceptibility rate, and their infection-fatality rate. Older adults have fewer contacts on average. Therefore, susceptible older adults are less likely to meet an infectious person compared to younger individuals, and infectious older adults have a lower probability of transmitting the virus to others. However, both susceptibility to infection and infection-fatality rate increase with age. Therefore, older adults are more likely to become infected upon contact with an infectious individual and to experience severe consequences.
We also assumed that essential workers have more contacts than nonessential workers of the same age throughout the immunization campaign (i.e., nonessential workers adhere to some form of social and physical distancing). The number of social interactions among children, adolescents, and older adults was also considered to decrease during the immunization campaign. We employed mobility patterns based on cellphone data to calibrate the reduction in contacts among nonessential workers and non-working-age individuals (see Section S1, Tables S1 and S2 in the Appendix A for details). Additionally, we assumed the implementation of non-pharmaceutical interventions (NPIs) (e.g., mask use) that further reduce individuals’ susceptibility. To be conservative, we assumed that NPIs were lenient in the baseline specification; when combined with the impact of reduced contact rates among children, adolescents, older adults, and nonessential workers, this reduction in susceptibility resulted in a reproductive number of 1.8 [46] † .
Vaccine administration was assumed to occur at a constant daily rate of 1% of the population. The first doses of the vaccine were assumed to be administered in the middle of the pandemic, when 15% of the population had already been infected, and the number of active infections was equal to 1% of the population. The corresponding numbers of daily infections and deaths in the absence of vaccine distribution are presented in Fig. S1 in the Appendix A. We also assumed that the vaccine was perfectly safe and that the distribution was independent of infection-acquired immunity. This is a suboptimal but realistic feature of the vaccine distribution process, accounting for a lack of widespread serological testing and a cautionary approach due to uncertainty regarding the duration of infection-acquired immunity.
We considered seven simple vaccine prioritization strategies: ① no age prioritization, that is, proportional allocation of the vaccine to all age groups according to the size of each group (“age proportional”); ② allocation of the vaccine to individuals aged 60 years and older first (“elderly”), followed by proportional allocation to the rest of the population according to the size of each group; ③ allocation to essential workers first independently of age due to their high-contact rate (“essential workers”), followed by proportional allocation to the rest of the population according to the size of each group; ④ allocation to children and teenagers first (“youth”), followed by proportional allocation to the rest of the population according to the size of each group; ⑤ allocation to essential workers first and elderly second, followed by the rest of the population (“essential/elderly”); ⑥ allocation to the elderly first and essential workers second, followed by the rest of the population (“elderly/essential”); and ⑦ allocation to the elderly and essential workers simultaneously, followed by the rest of the population (“elderly & essential”). These seven strategies account for the major sociodemographic differences in probability of infection and disease severity. Further, these strategies highlight the trade-offs between prioritization of individuals with the highest risk of severe outcomes (the elderly) and those with the highest risk of infection and transmission (essential workers).
We evaluated vaccine prioritization strategies based on three health outcomes: number of infections, number of deaths, and number of years of life lost† . The number of infections is a crude metric used to assess the overall impact of COVID-19, including mortality, morbidity, hospitalizations, and costs to the healthcare system and economy. The number of deaths accounts for the severity of potential outcomes and places equal value on all deaths, regardless of remaining life expectancy. The number of years of life lost accounts for differences in the age of decedents, attaching higher value to deaths in the young.
3.2. Results
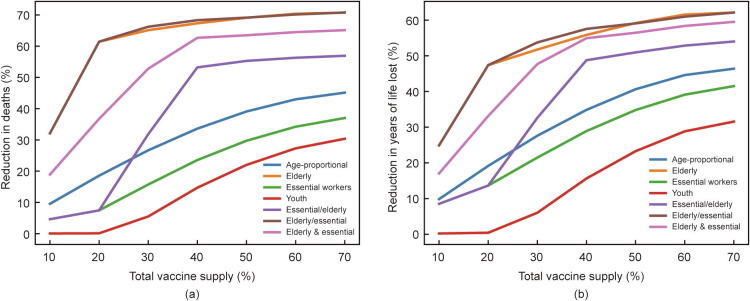
We first considered a vaccine that only produces direct effects on immunized individuals by reducing the infection-fatality risk but does not impact susceptibility or transmission rates. The health outcomes of the seven alternative prioritization strategies as a function of total vaccine supply when assuming the vaccine is 90% effective for all sociodemographic groups are summarized in Fig. 2 . The largest reduction in number of deaths compared with that in a no-vaccination scenario was achieved when the elderly were prioritized (“elderly” or “elderly/essential”). For a goal of reducing the number of years of life lost, the elderly would still be prioritized, but the relative benefits of prioritizing the elderly rather than essential workers decreased. Prioritizing individuals younger than 20 years old was the least effective strategy for reducing the numbers of deaths and years of life lost. Because the elderly are at the highest risk of severe disease and death, a vaccine that exclusively reduces the fatality risk conferred the greatest benefit when the elderly were prioritized. However, when decreasing life expectancy with age was factored in (i.e., using years of life lost as a metric), prioritizing essential workers and the elderly together was almost as beneficial as prioritizing the elderly if vaccine supply was high. Given that the vaccine was assumed to be distributed during the pandemic, at most 70% of deaths and 60% of years of life lost could be averted‡ . Similar results were observed for vaccines with lower effectiveness, although the shares of lives and years of life saved were lower (Appendix A Fig. S2).
Fig. 2.
Impact of a vaccine that is 90% effective at reducing infection-fatality risk as a function of total vaccine supply. The y-axis represents (a) the percentage reduction in deaths and (b) the percentage reduction in years of life lost compared to a scenario with no vaccine. The x-axis represents the percentage of the population that would eventually be vaccinated.
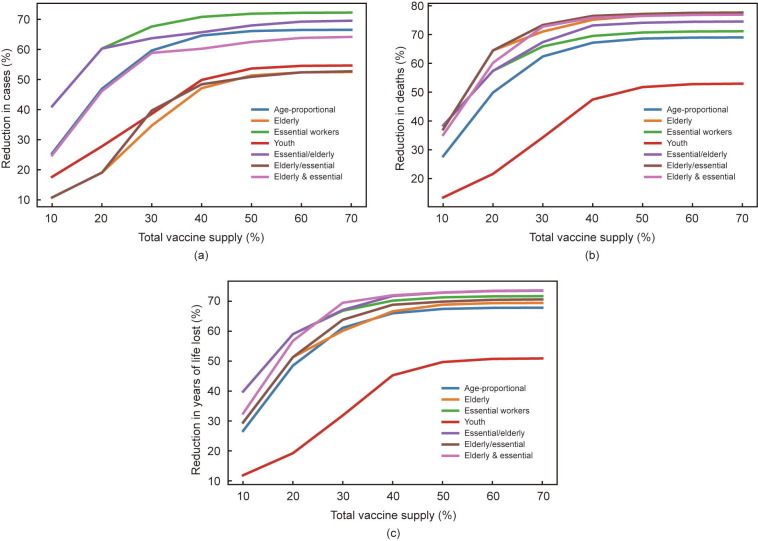
If a vaccine reduces the susceptibility rate, it will also reduce the number of fatalities and the rate of transmission. For a vaccine 90% effective at reducing infection risk, the largest reduction in number of cases was achieved by prioritizing essential workers due to their high contact rates (Fig. 3 ). Prioritizing the elderly or children and adolescents yielded the least reductions in number of infections due to the structure of social interactions (with the elderly having few contacts overall and the young having relatively few contacts outside of their age group, which is low-risk). For a goal of reducing the number of deaths, prioritizing the elderly resulted in the largest reduction in number of deaths for most vaccine supply levels, even if the vaccine was effective at reducing transmission risk and prioritizing essential workers would slow down the pandemic† . However, if the vaccine supply was sufficiently large, prioritizing both the elderly and essential workers resulted in comparably large numbers of avoided deaths. In contrast, for a goal of minimizing the number of years of life lost, the optimal strategy for most vaccine supply levels was to prioritize essential workers due to their younger average age. Similar patterns were observed for lower vaccine effectiveness (despite a decrease in the magnitude of benefits) and for vaccines that reduce both infection-fatality risk and transmission risk equally rather than infection risk (Appendix A Figs. S3 and S4).
Fig. 3.
Impact of a vaccine that is 90% effective at reducing infection risk as a function of total vaccine supply. The y-axis represents (a) the percentage reduction in cases, (b) the percentage reduction in deaths, and (c) the percentage reduction in years of life lost compared to a scenario with no vaccine. The x-axis represents the percentage of the population that would eventually be vaccinated.
Model results suggested that prioritizing the elderly was the optimal strategy in most scenarios even if the vaccine were equally effective at reducing the transmission risk and number of fatalities. For a vaccine that is more effective at providing direct benefits rather than indirect benefits via reduced transmission risk, prioritizing the elderly was the optimal strategy for any level of vaccine supply if minimizing the number of deaths was the goal. For example, for a vaccine that is 90% effective at reducing fatality risk but less than 80% effective at reducing transmission, prioritizing the elderly was the optimal strategy for any level of vaccine supply if the goal was to reduce the number of deaths (i.e., the “elderly/essential” strategy averted more deaths than the “essential/elderly” strategy, see Appendix A Table S4). For a goal of reducing the number of years of life lost, any vaccine able to reduce transmission risk by more than 50% would provide the greatest benefit when prioritizing essential workers (i.e., the “essential/elderly” strategy averted more years of life lost than the “elderly/essential” strategy). Similar patterns were observed for less effective vaccines (Appendix A Table S4).
The expected impact of a vaccine that is 90% effective at reducing fatality risk but with an uncertain impact on transmissibility is presented in Fig. 4 . Uncertainty was modeled as a uniform probability distribution of the effectiveness at reducing transmissibility between 0% and 90%. To compute the expected reduction in number of deaths or years of life lost associated with a given prioritization strategy and total vaccine supply, we first determined the reduction in number of deaths and years of life lost for the effectiveness of a specific vaccine at reducing transmission risk, with effectiveness varying in discrete 10-point increments from 0% to 90%. Thus, for each prioritization strategy, we obtained a distribution of the reduction in numbers of deaths and years of life lost, with one value for each possible effectiveness level. We then obtained the average reduction in the number of deaths and years-of-life lost across all model runs, where each run was weighted equally because of the uniform probability distribution assumption. With uncertain transmissibility effects, prioritizing the elderly was always the optimal strategy for maximizing the number of averted deaths (Fig. 4).
Fig. 4.
Expected impact of a vaccine that is 90% effective at reducing fatality risk but with uncertain effectiveness at reducing transmission risk as a function of total vaccine supply. The y-axis represents (a) the average percentage reduction in the number of deaths and (b) the average percentage reduction in the number of years of life lost compared to a scenario with no vaccine. Thus, a 50% reduction in deaths indicates that the allocation averts 50% of deaths on average. Uncertainty was modeled by assuming that the effectiveness at reducing transmission risk was uniformly distributed between 0% and 90%. The x-axis represents the percentage of the population that would eventually be vaccinated.
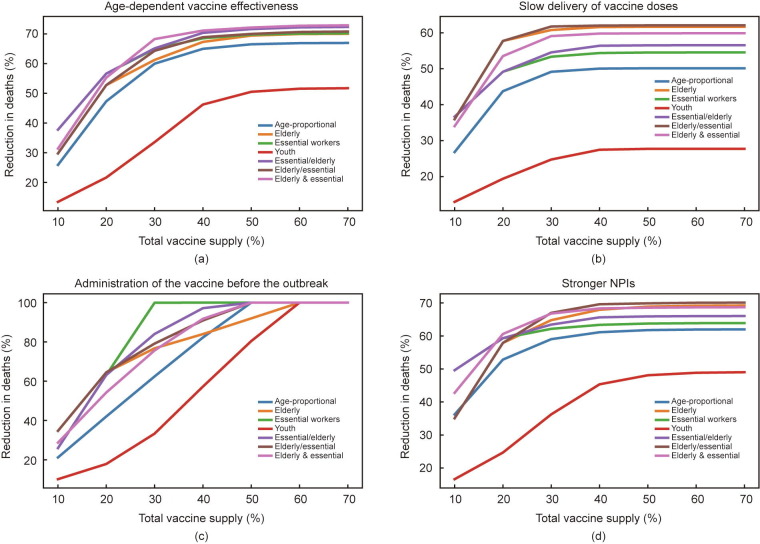
The results of sensitivity analyses for several main model assumptions are summarized in Fig. 5 . For these analyses, we selected minimizing the number of deaths as the outcome of interest because this metric appears to be the most sensitive to variations in vaccine properties. We considered a vaccine that is 90% effective at reducing infection risk but with no additional impact on the risk of death or the risk of transmission for those infected.
Fig. 5.
Sensitivity analysis: percentage reduction in the number of deaths for a vaccine that is 90% effective at reducing infection risk in alternative scenarios as a function of total vaccine supply. (a) Age-dependent vaccine effectiveness: The vaccine was considered 90%, 85%, 80%, 75%, and 70% effective for the 0–49, 50–59, 60–69, 70–79, and 80+ year-old age groups, respectively. (b) Slow delivery of vaccine doses: 0.5% of the population was vaccinated daily, regardless of the total vaccine supply. (c) Administration of the vaccine before the outbreak: The first doses were administered in the absence of infection-acquired immunity and with only one infection per sociodemographic group. (d) Stronger NPIs: The reproductive number was equal to 1.3. The y-axis represents the percentage reduction in number of deaths compared to that in a scenario with no vaccine. The x-axis represents the percentage of the population that would eventually be vaccinated.
Vaccines (e.g., flu vaccines) are often less effective in older adults because the immune system weakens with age. We assessed the impact of age-dependent vaccine effectiveness by assuming that the vaccine is effective at reducing susceptibility in individuals younger than 50 years old and that this effectiveness diminishes by 5 percentage points for every 10 years among those aged 50 years old and older (e.g., the vaccine is 20 percentage points less effective for an 80-year-old than for a 20-year-old). In this scenario, the relative benefits of prioritizing essential workers were greater than under the scenario of uniform effectiveness. Regardless, for large vaccine supply levels, prioritizing older adults alongside essential workers remained the optimal strategy (Fig. 5(a)). Additionally, we examined the implications of increasing the susceptibility rate in children and adolescents to the same level as in adults (Appendix A Fig. S5(a)); this reflects growing evidence of increased susceptibility in children and adolescents to certain novel SARS-CoV-2 variants such as the B.1.1.7 variant. The relative value of prioritizing the young and those with many contacts increased, although no changes were observed in the main results (i.e., prioritizing the elderly remained the optimal strategy). Similarly, we investigated the implications of setting the infection-fatality rate as an increasing function of the total number of active cases to encapsulate potential excess mortality resulting from constraints in healthcare system capacity. This increased the total number of deaths in the absence of vaccination, but no significant change was observed in the priority ranking of alternative strategies compared to the baseline scenario (Appendix A Fig. S5(b)).
We also considered the impacts of supply or logistical constraints in vaccine delivery; here, we assumed that only 0.5% of the population could be vaccinated daily instead of 1%. The achievable reduction in the number of deaths was lower than that in the baseline scenario (60% of deaths could be averted instead of 70%). Additionally, the slower pace of vaccination supported prioritization of the elderly for any level of vaccine supply, owing to a mismatch between the pace of the pandemic and the pace of vaccine administration (Fig. 5(b)). Because the initial vaccine distribution was in the middle of the pandemic, relying on the vaccine to delay transmission became suboptimal if there were constraints in delivery. Thus, the optimal strategy given the uncertainty regarding vaccine supply and delivery was to protect high-risk individuals (i.e., the elderly).
Next, we tested the impact of varying the initial conditions. If the vaccine was distributed before the outbreak (i.e., when the number of active cases was low and there was no infection-acquired immunity in the population), 100% of deaths could be averted by vaccinating only 30% of the population if essential workers were prioritized (Fig. 5(c)). If the pandemic was better controlled when the vaccine was initially distributed (e.g., if the number of active cases corresponded to 0.5% of the population), more than 80% of deaths could be averted, and prioritizing essential workers over the elderly was preferable if vaccine coverage was low (Appendix A Fig. S5(c)). Similarly, the higher the proportion of individuals with infection-acquired immunity at the beginning of the rollout, the better it was to prioritize essential workers when vaccine coverage was low, and the better it was to prioritize the elderly when vaccine coverage was high (Appendix A Figs. S5(d) and (e)). A potential reason for this is that fewer high-fatality-risk individuals had yet to be infected; reducing transmission by prioritizing essential workers would thus be optimal rather than attempting to vaccinate susceptible individuals (considering that vaccination is independent of previous infection in the model). This result could also derive from nonlinear reductions in disease transmission resulting from approaching the herd protection threshold.
Finally, we tested the sensitivity of the results to population compliance with social distancing measures and overall viral transmissibility. If the reproductive number fell to 1.3 (e.g., because of the implementation of stronger NPIs, such as mask wearing, or reduced viral transmissibility), high-fatality-risk individuals were better protected from the negative consequences of the disease. In this scenario, if vaccine coverage was low, the optimal course of action was to curb transmission by prioritizing essential workers, while for high vaccine coverage prioritizing the elderly was optimal (Fig. 5(d)). In contrast, as the reproductive number increased (e.g., because of weaker NPIs or a more transmissible variant of the virus), it was better to protect high-fatality-risk groups for any vaccine supply level (Appendix A Fig. S5(f)). Similar results were observed if, instead of varying the reproductive number† , the level of social interactions was varied: The more contact rates were reduced among individuals who are not essential workers, the larger the relative benefits of prioritizing essential workers if vaccine coverage was low (Appendix A Figs. S5(g) and (h)).
Beyond epidemiological reasons associated with the high risks of exposure and transmissibility, some may consider ethical concerns associated with social justice and fairness as a basis for prioritizing essential workers over the elderly. In the United States, a disproportionate number of essential workers are from racial and ethnic minorities and socioeconomically vulnerable populations, which has resulted in an exacerbation of pre-existing inequalities during the COVID-19 pandemic. Therefore, prioritizing essential workers may be optimal for equity reasons. For example, suppose that two individuals, A and B, would benefit equally from being vaccinated (e.g., they have the same COVID-19 mortality risk). However, B belongs to a socioeconomically vulnerable group and is an essential worker. To adjust for the social injustice faced by B, allocation of the vaccine to B first may be considered optimal, even though both individuals would experience the same health benefits. In contrast, allocating the vaccine to A first may further exacerbate the inequality between A and B. Given sufficient equity motives, prioritizing individual B (the essential worker) may be preferred, even if the expected health benefits of vaccination were higher for individual A.
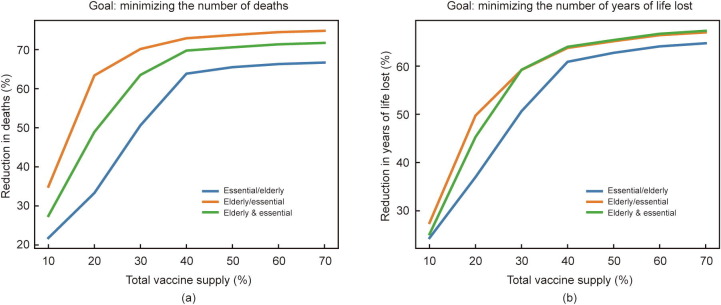
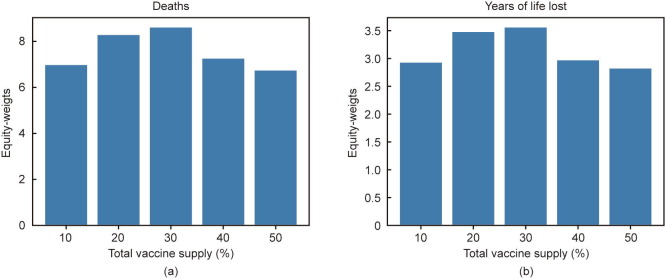
To examine the strength of the equity motive that would attach absolute priority to essential workers, we considered the scenario of a vaccine that only produces direct benefits. For a vaccine that reduces the infection-fatality rate by 90%, prioritizing the elderly resulted in the highest number of deaths averted (Fig. 2). Note that the prioritization strategy also affected the distribution of deaths among different groups in addition to affecting the total number. If the elderly were prioritized over essential workers (i.e., the “elderly/essential” strategy compared to the “essential/elderly” strategy), by construction fewer total deaths would occur and fewer deaths would occur among the elderly, but more deaths would occur among essential workers (because the vaccine has almost exclusively direct benefits, deaths among the rest of the population would be unchanged). We investigated what level of equity-weight for essential workers would be necessary to prioritize them over the elderly in this scenario (i.e., preference of the “essential/elderly” to the “elderly/essential” strategy), despite the higher number of deaths among the elderly, with equity-weight representing the greater value attached to preserving an individual life given their pre-existing social disadvantage.
Fig. 6 depicts the result of such an analysis. If the vaccine supply covered at least 40% of the population and essential workers were prioritized, then saving the life of an essential worker was considered equivalent to saving the life of more than six older adults. Stated differently, the “essential/elderly” allocation would only be selected if preserving the life of an essential worker was equity-weighted at more than six times that of an older person. The same exercise was performed for years of life lost. If the vaccine supply covered at least 40% of the population, the “essential/elderly” allocation would be selected as long as one year of life of an essential worker was equity-weighted to approximately three years of life of an older person. The lower weighting was due to the differences in age and resulting preference for vaccinating essential workers first, based on the higher life expectancy if their lives were saved.
Fig. 6.
Equity-weights attached to preserving (a) the life or (b) the life-years of an essential worker such that essential workers would receive absolute priority in the allocation of a vaccine that is 90% effective at reducing fatalities (the equity-weight attached to preserving the life/life years of an older person is 1). The y-axis represents the equity-weight attached to preserving (a) the life or (b) life years of an essential worker compared to the life or life years of an older adult. For example, a weight of two indicates that preserving the life (a year of life) of an essential worker was equity-weighted to preserving the life of two older adults (two years of life of an older adult). The x-axis represents the maximum percentage of the population that would be vaccinated.
4. Discussion and conclusions
The analysis in this paper highlights that critical considerations for vaccine allocation strategies involve both the stated goal (e.g., minimizing the number of deaths while adjusting for differences in life expectancy or minimizing deaths or years of life lost while promoting social justice) and specific properties of a vaccine. We demonstrate that even if a vaccine is effective at blocking viral transmission, prioritizing the elderly yields the largest reduction in number of deaths in most scenarios. Uncertainty about the effectiveness of a vaccine in blocking transmission and potential constraints in delivery reinforce the relative benefits of prioritizing the elderly. Note that uncertainties or inconsistencies about delivery timing (e.g., interruptions in vaccine supply) are likely to have similar effects on selection of prioritization strategy. Prioritizing essential workers is a viable strategy for reducing the number of infections and years of life lost. It appears also to be a viable strategy for reducing the number of deaths when the pandemic is well-controlled (e.g., under scenarios with a low reproductive number and high compliance with social distancing practices, low number of active cases, or a high level of infection-acquired immunity at the beginning of vaccine rollout), at least if vaccine supply levels are low.
Additionally, we explored the equity implications of relatively broad alternative prioritization strategies for the allocation of limited supplies of COVID-19 vaccine doses. In this regard, we examined the strength of the equity motive that would support prioritization of essential workers (who have the greatest risk of contracting COVID-19 and tend to have disproportionately lower socioeconomic status and to overrepresent racial and ethnic minorities) over older adults (who have the greatest risk of death from COVID-19 but tend to be disproportionately wealthy and white). Our findings suggest that across a range of plausible scenarios, prioritizing older adults would generally yield the greatest reduction in number of deaths. A reasonably strong equity motive (e.g., an equity weight higher than six in our simulation) would therefore be required to favor prioritization of essential workers over older adults, if saving lives were the principal objective.
Nevertheless, more granular methods are available for addressing pre-existing social inequities in the allocation of COVID-19 vaccines. For example, in their Framework for Equitable Allocation of COVID-19 Vaccine published in the fall of 2020, the US National Academies of Sciences, Engineering, and Medicine recommended the use of a social vulnerability index (SVI) to identify and prioritize—within each specified population group (e.g., “all older adults” or “critical workers in high-risk settings”)—geographic areas associated with higher vulnerability to severe COVID-19 outcomes. Such within-group prioritization enables the greatest emphasis to be placed on broad, overarching public health goals (e.g., saving lives), while still giving due attention to longstanding societal inequities. The National Academies’ recommendation to incorporate a vulnerability index was not adopted in the formal national guidelines for phased COVID-19 vaccination from the Centers for Disease Control and Prevention and Advisory Committee on Immunization Practices [33], [38], but several states appear to be employing an SVI in some fashion [47].
It is worth mentioning that the actual implementation of vaccine allocation strategies may have strong equity implications, beyond the impact of the prioritization framework underlying any given strategy. Indeed, several states have paid insufficient attention to the differential abilities of social groups to meet the exigencies of the vaccination registration process. For example, in some cases individuals with lower income may struggle to access online booking systems with limited appointment availability because they have to work blue-collar jobs during the day or lack adequate internet access [48], [49]. Such oversights may precipitate a scenario in which pre-existing social inequities are not only maintained but even exacerbated by the vaccine rollout.
Our analysis has several limitations. We employed a deterministic SEIR model to illustrate the effects of alternative prioritization strategies, but these models, although widely used, are not well-suited to capture disease dynamics that are inherently stochastic and non-linear (e.g., super-spreader events) [50]. In addition, we only considered heterogeneity by age and essential worker status, but other risk factors are correlated with COVID-19 infection risk or the risk of death from COVID-19, including the presence of comorbidities, constraints in healthcare system capacity, sex, race, ethnicity, socioeconomic status, and living arrangements [13], [51], [52], [53], [54]. Further, we did not include geographic variation in the model (e.g., high-density vs low-density areas). Subdividing the population into narrower, more-refined socio-demographic groups would provide a more detailed picture of which groups should be prioritized. Finally, many of the inputs used in the model are subject to uncertainty; new information may thus affect the generalizability of model results. For example, we assumed that, upon recovery, infected individuals are immune and cannot be infected or become infectious again, but future studies may shed light on the duration of natural immunity. In addition, all individuals were considered eligible for the vaccine independently of whether they have been infected and have developed immunity (which is consistent with policy throughout the United States). Finally, the burden of the pandemic and optimal vaccine prioritization strategy depend on the future trajectory of the pandemic, that is the prevalent reproductive number, relative reduction in contacts across ages and socio-economic groups, and dominant variant of the virus in circulation. These features are highly uncertain, and the model relies on best estimates or realistic assumptions.
Other relevant considerations for vaccine allocation strategies were beyond the scope of this analysis. The capacity of the health system to deliver the vaccine to different sociodemographic groups may be relevant to the selection of vaccine prioritization strategy. In addition to logistical constraints and differences in the distribution of costs among sociodemographic groups, vaccine hesitancy may play a role in the final allocation. If a prioritized group refuses to receive the vaccine, it makes sense to rapidly allocate the vaccine to the next group. In this regard, attaching equal priority to elderly and essential workers (as in the “elderly & essential” strategy) may avoid delays in vaccine rollout. Alternatively, many US states have addressed this issue by allowing overlap in the timing of vaccination across priority groups [55]. Moreover, some vaccine allocation strategies may either diminish or amplify vaccine hesitancy. For example, the general public may be more likely to accept a vaccine if they witness its effectiveness in healthcare workers who also endorse its use; conversely, they may be less likely to accept the vaccine if immunosenescence substantially undermines its effectiveness in older adults who are early recipients [56] †.
Throughout the paper, we have assumed that a single vaccine is to be distributed. Availability of multiple vaccines with different levels of effectiveness, dosage, safety profiles, and costs is likely to affect the selected allocation strategy. This raises the complex question of which vaccine is appropriate for each sociodemographic group and when each group should be vaccinated under different conditions of uncertainty. For example, if a more effective vaccine than the one available is expected, which group should receive available doses of the less-effective vaccine? Non-health considerations are important here as well because delaying vaccine distribution implies that physical and social distancing measures must remain in place for longer, thereby delaying economic recovery and prolonging social hardship. Due to the interplay between NPIs and vaccination strategies, the optimal vaccine prioritization rule should be selected in conjunction with the optimal intensity of NPIs (e.g., the rule may depend on economic sectors for which relaxation of NPIs is most desired).
Potential unintended consequences of vaccination should also be considered. The introduction of a vaccine may confer a sense of protection in immunized individuals, who may behave less cautiously with regards to practicing social and physical distancing. This may be an issue if the vaccine turns out to be less effective than expected, especially at reducing transmission.
In sum, the optimal vaccine allocation strategy depends on various factors, including COVID-19 epidemiology, vaccine characteristics, and economic, social, and ethical considerations. Analyses of the full value of COVID-19 vaccines and alternative prioritization strategies will promote preparedness for future pandemics and improve the distribution and logistical management of vaccines for endemic diseases.
Acknowledgments
Acknowledgements
This work was supported by the Value of Vaccination Research Network (VoVRN) through a grant from the Bill & Melinda Gates Foundation (OPP1158136). The content is solely the responsibility of the authors and does not necessarily reflect the views of the VoVRN or the foundation.
Compliance with ethics guidelines
Maddalena Ferranna, Daniel Cadarette, and David E. Bloom declare that they have no conflict of interest or financial conflicts to disclose.
Footnotes
Evidence suggests that some of the novel variants, for example, the B.1.1.7 variant, are more contagious and more likely to infect children compared to the non-variant virus [9]. Although COVID-19 vaccines are generally expected to be effective against these novel variants, differential susceptibility across age groups may affect optimal vaccine allocation.
The basic reproductive number for COVID-19 (i.e., in a fully susceptible population in the absence of any intervention) is reported to fall in the range of 2.0 to 3.0 [46]. For the purpose of our baseline analysis, we assumed that the reproductive number during the vaccine rollout was 1.8, reflecting mild forms of social and physical distancing.
Analysis based on the number of quality-adjusted years of life lost is presented in Section S2 and Table S3 in the Appendix A, as no significant differences were observed with respect to the number of years of life lost.
Because the vaccine does not affect the risk of infection in this scenario, the impact on the number of cases is minimal and stems from the difference in the number of individuals that are alive (i.e., the more individuals that are still alive, the lower the probability of encountering an infectious person for any given contact rate and number of infections in the population, see Appendix A Fig. S2).
If a hypothetical vaccine that was effective at preventing transmission but was ineffective at preventing death existed (i.e., if vaccinated individuals could be infected and experience severe health outcomes as much as unvaccinated individuals but were less infectious than unvaccinated individuals), prioritizing essential workers would lead to the largest number of avoided deaths.
Note that in our framework, varying the reproductive number is equivalent to varying the (average) susceptibility rate, with contact rates kept constant.
Another issue is whether the vaccine allocation strategy is affected by the number of doses required per individual (i.e., single-dose vs two-dose vaccines). Logistical barriers and hesitancy issues are increased with multi-dose vaccines, which may delay distribution and the resulting reduction in infections (e.g., the decision by the UK to postpone the administration of the second dose of the BioNTech-Pfizer and AstraZeneca-University-of-Oxford vaccines, thereby vaccinating a larger group with one dose rather than a smaller group with two doses [56]).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eng.2021.03.014.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.coronavirus.jhu.edu [Internet]. Baltimore: Johns Hopkins University & Medicine; 2020 [cited 2020 Dec 14]. Available from: https://coronavirus.jhu.edu/map.html.
- 2.International Monetary Fund. World Economic Outlook, October 2020: a long and difficult ascent [Internet]. Washington, DC: International Monetary Fund 2020 [cited 2020 Dec 13]. Available from: https://www.imf.org/en/Publications/WEO/Issues/2020/09/30/world-economic-outlook-october-2020.
- 3.Bloom D.E., Cadarette D., Ferranna M., Hyer R.N., Tortorice D.L. How new models of vaccine development for COVID-19 have helped address an epic public health crisis. Health Aff. 2021;40(3):410–418. doi: 10.1377/hlthaff.2020.02012. [DOI] [PubMed] [Google Scholar]
- 4.Zimmer C., Corum J., Wee S.L. The New York Times Company; New York: 2020. Coronavirus vaccine tracker [Internet] [cited 2021 Feb 24]. Available from: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html. [Google Scholar]
- 5.Institute of Medicine . The National Academy Press; Washington, DC: 2010. The 2009 H1N1 influenza vaccination campaign: summary of a workshop series. Available from: http://www.ncbi.nlm.nih.gov/books/NBK54185/ [PubMed] [Google Scholar]
- 6.Skrip L.A., Galvani A.P. Next steps for Ebola vaccination: deployment in non-epidemic, high-risk settings. PLoS Negl Trop Dis. 2016;10(8) doi: 10.1371/journal.pntd.0004802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viner R.M., Mytton O.T., Bonell C., Melendez-Torres G.J., Ward J., Hudson L. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2021;175(2):143–156. doi: 10.1001/jamapediatrics.2020.4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahase E. COVID-19: what have we learnt about the new variant in the UK? BMJ. 2020;371 doi: 10.1136/bmj.m4944. [DOI] [PubMed] [Google Scholar]
- 10.Medlock J., Galvani A.P. Optimizing influenza vaccine distribution. Science. 2009;325(5948):1705–1708. doi: 10.1126/science.1175570. [DOI] [PubMed] [Google Scholar]
- 11.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. Lancet Respir Med. 2020;8(6):547–548. doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with COVID-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown C, Ravallion M. Inequality and the coronavirus: socioeconomic covariates of behavioral responses and viral outcomes across US counties. NBER working paper. 2020 Jul. No.: w27549.
- 14.Goodnough A, Hoffman J. The elderly vs. essential workers: who should get the coronavirus vaccine first [Internet]. New York: The New York Times Company; 2020 [cited 2020 Dec 6]. Available from: https://www.nytimes.com/2020/12/05/health/covid-vaccine-first.html.
- 15.Persad G., Peek M.E., Emanuel E.J. Fairly prioritizing groups for access to COVID-19 vaccines. JAMA. 2020;324(16):1601–1602. doi: 10.1001/jama.2020.18513. [DOI] [PubMed] [Google Scholar]
- 16.Matrajt L, Eaton J, Leung T, Brown ER. Vaccine optimization for COVID-19: who to vaccinate first? Sci Adv 2021;7(6):eabf1374. [DOI] [PMC free article] [PubMed]
- 17.Rodríguez J, Patón M, Acuña JM. Prioritisation of population groups with the most interactions for COVID-19 vaccination can substantially reduce total fatalities. 2020. medRxiv:2020.10.12.20211094v3.
- 18.Bubar K.M., Reinholt K., Kissler S.M., Lipsitch M., Cobey S., Grad Y.H. Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science. 2021;371(6532):916–921. doi: 10.1126/science.abe6959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gallagher M.E., Sieben A.J., Nelson K.N., Kraay A.N.M., Orenstein W.A., Lopman B. Indirect benefits are a crucial consideration when evaluating SARS-CoV-2 vaccine candidates. Nat Med. 2021;27(1):4–5. doi: 10.1038/s41591-020-01172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen X, Li M, Simchi-Levi D, Zhao T. Allocation of COVID-19 vaccines under limited supply. 2020. medRxiv:2020.08.23.20179820.
- 21.Forslid R, Herzing M. Whom to vaccinate first—some important trade-offs. CEPR discussion paper. 2021 Feb. No.: DP15800.
- 22.Chen JZ, Hoops S, Marathe A, Mortveit H, Lewis B, Venkatramanan S, et al. Prioritizing allocation of COVID-19 vaccines based on social contacts increases vaccination effectiveness. 2021. medRxiv:2021.02.04.21251012.
- 23.Buckner JH, Chowell G, Springborn MR. Dynamic prioritization of COVID-19 vaccines when social distancing is limited for essential workers. 2020. medRxiv:2020.09.22.20199174. [DOI] [PMC free article] [PubMed]
- 24.Biggerstaff M. Modeling strategies for the initial allocation of SARS-CoV-2 vaccines [Internet]. 2020 [cited 2020 Oct 30]. Available from: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-10/COVID-Biggerstaff-508.pdf.
- 25.Babus A, Das S, Lee SM. The optimal allocation of COVID-19 vaccines. 2020. medRxiv:2020.07.22.20160143. [DOI] [PMC free article] [PubMed]
- 26.Moore S, Hill EM, Dyson L, Tildesley MJ, Keeling MJ. Modelling optimal vaccination strategy for SARS-CoV-2 in the UK. 2020. medRxiv:2020.09.22.20194183. [DOI] [PMC free article] [PubMed]
- 27.Jentsch P, Anand M, Bauch CT. Prioritising COVID-19 vaccination in changing social and epidemiological landscapes. 2020. medRxiv:2020.09.25.20201889. [DOI] [PMC free article] [PubMed]
- 28.Rahmandad H. Behavioral responses to risk promote vaccinating high-contact individuals first. 2021. medRxiv:2021.02.05.21251215. [DOI] [PMC free article] [PubMed]
- 29.Vellodi N., Weiss J. Optimal vaccine policies: spillovers and incentives. Covid Econ. 2021;65:1–46. [Google Scholar]
- 30.Castonguay FM, Blackwood JC, Howerton E, Shea K, Sims C, Sanchirico JN. Spatial allocation of scarce vaccine and antivirals for COVID-19. 2021. medRxiv:2020.12.18.20248439.
- 31.National Academy of Sciences Engineering and Medicine . The National Academy Press; Washington, DC: 2020. Framework for equitable allocation of COVID-19 vaccine. [PubMed] [Google Scholar]
- 32.Toner E, Barnill A, Krubiner C, Bernstein J. Interim framework for COVID-19 vaccine allocation and distribution in the United States [Internet]. Baltimore: The Johns Hopkins Center for Health Security; 2020. Available from: https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2020/200819-vaccine-allocation.pdf.
- 33.Centers for Disease Control and Prevention. How CDC is making COVID-19 vaccine recommendations [Internet]. Washington, DC: Centers for Disease Control and Prevention; 2020 [cited 2021 Jan 4]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html.
- 34.Joint Committee on Vaccination and Immunisation. Priority groups for Coronavirus (COVID-19) vaccination: advice from the JCVI, 2 December 2020 [Internet]. London: Joint Committee on Vaccination and Immunisation; 2020 [cited 2020 Dec 2]. Available from: https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-2-december-2020/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-2-december-2020.
- 35.World Health Organization (WHO). Fair allocation mechanisms for COVID-19 vaccines through the COVAX facility [Internet]. Geneva: World Health Organization; 2020 [cited 2020 Sep 9]. Available from: https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility.
- 36.WHO Strategic Advisory Group of Experts. Values framework for the allocation and prioritization of COVID-19 vaccination [Internet]. Geneva: WHO; 2020 [cited 2020 Sep 14]. Available from: https://apps.who.int/iris/bitstream/handle/10665/334299/WHO-2019-nCoV-SAGE_Framework-Allocation_and_prioritization-2020.1-eng.pdf.
- 37.Advisory Committee on Immunization Practices (ACIP). Phased allocation of COVID-19 vaccines [Internet]. Washington, DC: Centers for Disease Control and Prevention; 2020 [cited 2020 Dec 15]. Available from: https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/COVID-02-Dooling-508.pdf.
- 38.Dooling K., Marin M., Wallace M., McClung N., Chamberland M., Lee G.M. The advisory committee on immunization practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69(5152):1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peiris M., Leung G.M. What can we expect from first-generation COVID-19 vaccines? Lancet. 2020;396(10261):1467–1469. doi: 10.1016/S0140-6736(20)31976-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.www.cisa.gov [Internet]. Washington, DC: Cybersecurity & Infrastructure Security Agency; 2020 [cited 2020 Dec 14]. Available from: https://www.cisa.gov/publication/guidance-essential-critical-infrastructure-workforce.
- 41.Emanuel E.J., Wertheimer A. Who should get influenza vaccine when not all can? Science. 2006;312(5775):854–855. doi: 10.1126/science.1125347. [DOI] [PubMed] [Google Scholar]
- 42.Blau FD, Koebe J, Meyerhofer PA. Who are the essential and frontiline workers? [Internet]. NBER Working Paper n. 27791: 2021. Available from: https://www.nber.org/system/files/working_papers/w27791/w27791.pdf.
- 43.Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. In press. [DOI] [PMC free article] [PubMed]
- 44.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rasmussen A.L. The New York Times Company; New York: 2021. Does the vaccine stop transmission? [Internet] [cited 2021 Feb 23]. Available from: https://www.nytimes.com/2021/02/23/opinion/covid-vaccines-transmission.html. [Google Scholar]
- 46.Bauch C.T. Estimating the COVID-19 R number: a bargain with the devil? Lancet Infect Dis. 2021;21(2):151–153. doi: 10.1016/S1473-3099(20)30840-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmidt H., Weintraub R., Williams M.A., Buttenheim A., Sadecki E., Wu H. SSRN; Rochester: 2021. Equitable allocation of COVID-19 vaccines: an analysis of the initial allocation plans of CDC’s jurisdictions with implications for disparate impact monitoring [Internet] Available from: https://ssrn.com/abstract=3740041. [Google Scholar]
- 48.NPR. Early data shows striking racial disparities in who’s getting the COVID-19 vaccine [Internet]. NPR; 2021 Jan 28 [cited 2021 Jan 28]. Available from: https://www.npr.org/transcripts/961703505.
- 49.Zhang C, Bushey C. Racial inequality plagues US vaccine rollout [Internet]. The Financial Times Ltd.; 2021 [cited 2021 Feb 20]. Available from: https://www.ft.com/content/7b0db882-a369-4e32-a86a-eb7fda2a0da0.
- 50.Roberts M., Andreasen V., Lloyd A., Pellis L. Nine challenges for deterministic epidemic models. Epidemics. 2015;10:49–53. doi: 10.1016/j.epidem.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takahashi T., Ellingson M.K., Wong P., Israelow B., Lucas C., Klein J. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588(7837):315–320. doi: 10.1038/s41586-020-2700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chow N, Fleming-Dutra K, Gierke R, Hall A, Hughes M, Pilishvili T, et al.; CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep 2020;69(13):382–6. [DOI] [PMC free article] [PubMed]
- 54.Wu X, Nethery RC, Sabath MB, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci Adv 2020;6(45):eabd4049. [DOI] [PMC free article] [PubMed]
- 55.See how the vaccine rollout is going in your state [Internet]. New York: The New York Times Company; 2021 [cited 2021 Feb 23]. Available from: https://www.nytimes.com/interactive/2020/us/covid-19-vaccine-doses.html.
- 56.Public Health England. COVID-19: The Green Book, Chapter 14a [Internet]. London: Public Health England; 2020 [cited 2021 Feb 20]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/948757/Greenbook_chapter_14a_v4.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.