Abstract
Background
The COVID-19 pandemic is spreading all over the world, particularly in developed countries where obesity is also widespread. There is a high frequency of increased BMI in patients admitted to intensive care for SARS-CoV-2 infection with a major severity in patients with an excess of visceral adiposity. Patients at risk of severe SARS-CoV-2 acute respiratory syndrome are characterised by the high prevalence of pre-existing diseases (high blood pressure and cardiovascular disease, diabetes, chronic respiratory disease, or cancer), most of them typically present in severely obese patients. Indeed, the biological role of adipose tissue in sustaining SARS-CoV-2 infection is not completely elucidated.
Summary
The forced isolation due to pandemic containment measures abruptly interrupted the rehabilitation programs to which many patients with severe obesity were enrolled. People affected by obesity, and especially those with severe obesity, should continue clinical rehabilitation programs, taking extra measures to avoid COVID-19 infection and reinforcing the adoption of preventive procedures. In this review, the available data on obesity and COVID-19 are discussed along with evidence-based strategies for maintaining the necessary continuous rehabilitation programs.
Key Messages
Greater attention is needed for obese and severely obese patients in the face of the current COVID-19 pandemic, which represents a huge challenge for both patients and healthcare professionals. The adoption of new strategies to guarantee adequate and continuous multidisciplinary nutritional rehabilitation programs will be crucial to control the severity of SARS-CoV-2 infection in high-risk populations as well as the worsening of obesity-linked complications. Health authorities should be urged to equip hospitals with tools for the diffusion of telemedicine to maintain physician-patient communication, which is fundamental in chronic and complicated obese patients.
Keywords: Obesity, COVID-19 pandemic, Bariatric surgery, Telemedicine, Rehabilitation, Diet, Physical activity, Adipose tissue
Introduction
Obesity is considered a chronic disease state [1] and currently the major strategy to take action regarding the management of obese patients, particularly metabolically unhealthy patients with a body mass index above 40, is to plan long-term rehabilitation programs. Various evidence exists for the benefit of providing continuous multidisciplinary (dietary, psychological, motor/functional) supportive programs to counteract the degenerative effects of chronic obesity, especially for patients not eligible to the available drug therapies or eligible for bariatric surgery procedures.
In December 2019, the novel coronavirus (SARS-CoV-2) pneumonia emerged in Wuhan (China), with cases rapidly increasing worldwide. On March 11, 2020 the World Health Organisation declared the COVID-19 infection a pandemic. In Europe, Italy was certainly one of the first and most affected countries. From March 10 to May 4, 2020 the Italian Government implemented restrictive measures to contain the infection spread. The containment measures consisted of a temporary closure of all non-essential activities, strengthening the measures aimed to increase personal hygiene, symptom monitoring, early diagnosis, and patient isolation. Indeed, all non-urgent medical visits, including clinical practices planned for obesity management, were deferred to ensure social distancing [2] and reduce the virus spread. During this period, a worsening of clinical/functional complaints and nutritional and metabolic status was observed in obese patients due to changes in lifestyle habits and reduction in exercise practice [3]. Many people became stressed and depressed as a result of overexposure to news about the spread of COVID-19 and the “forced” social isolation, which led to an increased incidence of eating disorders, resulting in weight gain [4]. Moreover, patients with severe obesity and those with previous bariatric surgery represent a vulnerable cohort of patients with an increased risk of infection and/or a severe course of COVID-19 [5]. Thus, in response to a possible “phase 2” of the COVID-19 pandemic, and in general to facilitate all those patients who do not have easy access to a long-term rehabilitation program for different reasons (motor disability, residence in a remote area, etc.), it is necessary to encourage innovative strategies for obesity management to avoid nosocomial dissemination of the virus and, at the same time, maintain standard follow-up for patients who require continuous rehabilitative support. Here, we analysed the main negative effects of the COVID-19 pandemic on dietary habits, eating behaviour, and physical activity in severely obese patients, discussing new strategies that could be put into place to counteract them in the future.
Adipose Tissue and Infection Susceptibilities
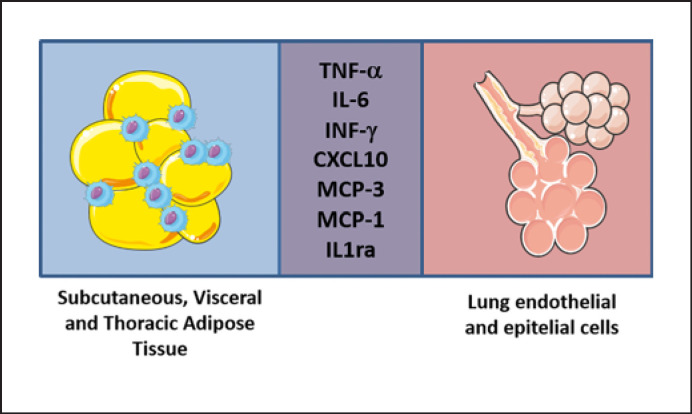
Patients with obesity and morbid obesity have a known increased susceptibility to viral infections [6]. The excess of white adipose tissue and the “low-grade” chronic pro-inflammatory state that characterises obesity are probably the biological basis for a dysregulated immune response as well as for the development of metabolic complications, such as insulin resistance and type 2 diabetes [7]. Adipose tissue is effectively at the interface between metabolism and immunity [8, 9], and immune system cells and adipocytes share numerous similarities in structure and functions, especially in the production of some inflammatory mediators [10]. It is well documented that obese patients have a more intense interleukin-8 release in H1N1 infection as compared with normal-weight individuals [11], and an impaired immune response to influenza vaccination was also described for obese patients [12]. In addition to flu viruses, also the human immunodeficiency virus (HIV) has been described in the literature as an example of a virus capable of interacting with white adipose tissue/adipocytes. HIV evades the immune system by stopping its replication and persisting in latent form in CD4+ T cells and in macrophages. Infected immune cells allow the virus to migrate into non-lymphoid tissues, including white adipose tissue, where it could remain latent or resumes its replication. HIV viral replication can also take place in the white adipose tissue [13] and the adipocyte is a target for HIV infection since it carries on its surface the receptors essential for viral entry (CD4, CXCR4, and CCR5) [13, 14]. Concerning the pathogenesis of SARS-CoV-2 infection, it is almost clear that the viral entry includes the recognition of angiotensin-converting enzyme 2 receptor (ACE2) by the virus spike protein and by the cellular transmembrane protease serine 2 (TMPRSS2) helping host cell viral entry and spread. ACE2 receptors are widely distributed in various organs and cell types, including adipose tissue in which the expression levels reported are higher than in lung tissue [15]. Obese individuals, having an increased adipose mass in the body, possibly increase the number of ACE2-expressing cells, resulting in major infection susceptibility. Recently, a role for human dipeptidyl peptidase 4 (DPP4) was also suggested for SARS-CoV-2 infection. DPP4 expression is higher in visceral adipose tissue and directly correlates with adipocyte inflammation and insulin resistance [16]. Interestingly, the 3 cytokines recently described with an exuberant elevation during the SARS-CoV-2-induced “cytokine storm” (IP-10, also known as CXCL-10, MCP-3, and IL-1ra) [17] are also produced and secreted by adipocytes and adipose tissue-infiltrating immune cells [18] (Fig. 1). Targeted research of SARS-CoV-2 and its role in human adipose tissue is needed, but in the meantime extra preventive measures should be provided during this pandemic period for obese and morbidly obese patients, who represent a group of patients more fragile and susceptible to infections.
Fig. 1.
Inflammatory cytokines upregulated in the “cytokine storm” of SARS-CoV-2 induced in lung cells are also produced and secreted by adipose tissue, adipocytes, and resident immune cells of obese patients, suggesting a potential “addictive” pro-inflammatory effect. Tumour necrosis factor-alpha (TNF-α), interleukin 6 (IL-6), interferon gamma (INF-γ), INF-γ-induced protein 10 (IP-10 or CXCL10), monocyte-chemotactic protein 3 (CCL7 or MCP-3), monocyte-chemotactic protein 1 (CCL2 or MCP-1), and interleukin 1 receptor antagonist (IL-1ra) were associated with an increased viral load, loss of lung function, lung injury, and a fatal outcome. This figure was generated with images from Servier Medical Art (www.servier.com), licensed under the Creative Commons Attribution 3.0 unported license (http://creativecommons.org/license/by/3.0/).
Outpatient Support
Reduction of Direct Exposure
The management of patients with severe obesity and those after bariatric surgery is often performed in hospitals engaged as COVID-19 hotspots, thus potentially putting obesity-affected outpatients at risk of nosocomial infections. In addition, to maintain social distancing, fewer health services and medical examinations are possible. Prioritisation criteria need to be defined for outpatient contacts to be guaranteed the greatest number of health services in compliance with the local COVID-19 burden and officially implemented rules and regulations. Individual therapy is the basis for obesity treatment, enables physician-patient relationships, and allows physicians to quickly assess the overall condition of the patient. However, due to the number of single contacts, physicians are at high risk of infection and consequently also of virus dissemination. In order to minimise the risk and to protect vulnerable patient cohorts from individuals with potential SARS-CoV-2 infection, physical distancing needs to be implemented through changes to operating procedures for outpatient care, including remodelling of waiting areas to allow sufficient distance between patients, reduction of waiting times, and encouraging changes in the routine of clinical practices to limit the amount of face-to-face contact for patients at risk of a more severe course of infection. Technical solutions for individual protection are available to enable remote physician-patient interactions and their benefits have already been discussed in the context of the COVID-19 pandemic [19]. Group therapy has been a proven strategy to support behavioural changes and greater weight loss than an individual approach. The program generally consists of weekly group meetings, which include psychologists, dietitians, physiotherapists, and physicians. They introduce and explain eating and exercise-related strategies by using a cognitive-behavioural approach [20]. Table 1 presents the main strategies to reduce the risk of virus dissemination the pandemic.
Table 1.
New strategies for obesity management during the COVID-19 pandemic
|
Strategies to reduce direct exposure during group therapy − Limited number of participants − Adequate space/people ratio (2 m2 each) − Priority for access to the most clinically urgent obese patients (eating disorders, need for weight loss prior to surgery, type 2 diabetes decompensated) − No access to patients who are most at risk in the case of SARS-CoV-2 infection (age >70 years, chronic respiratory diseases, oncological diseases in the last 12 months, immunosuppression) − Training patients on the hygiene and health standards to follow during group therapy − Detection of cases of infection by check points at the entrance of the hospital − Security distance of at least 1 m apart between patients both in the waiting area and during group therapy − Sanitising of environments and tools after each use, according to standardised procedures − Use of individual safety devices |
|
Web-based strategies to control eating behaviour − Participation in virtual races or activity challenges (e.g., mindful eating, intuitive eating) − Virtual social support groups − Web-based healthy meal ideas, cooking tips, and ideas for modifying recipes for pantry items |
|
Strategies to maintain adequate food intake and dietary quality − Weighing once a week − Eating vegetables, fruits, and pulses on a daily base − Limit the intake of free sugars and processed/ultra-processed foods − Avoid alcoholic drinks − Prepare a shopping list and a cooking plan − Follow-up by implementation of telenutrition |
|
Strategies to maintain physical activity − Exercise at home (or outside but in respect of safety measures) on a daily base, to counteract sedentary behaviours − Alternation of combined physical activity or concurrent training (a mix of aerobic and rehabilitative exercise on the same day) − Follow-up by new communication technologies |
Support to Control Eating Behaviour
The link between obesity and stress is well known. Stress triggers physiological changes in the hypothalamic-pituitary-adrenal axis, reward processing in the brain, and stimulates the production of biochemical hormones and peptides such as leptin, ghrelin, and neuropeptide involved in the regulation of hunger and satiety [21]. For these reasons stress leads individuals to eat higher quantities of food with a higher tendency to prefer palatable food, to decrease the tendency for physical activity, and to induce shorter periods of sleep, favouring eating disorders. A recent Italian survey reported that during the COVID-19 lockdown, the sense of hunger and satiety changed for more than half of the population: more than half of interviewees reported an increased appetite. The increase in the sense of hunger and the resulting change in eating habits could explain the perception of weight gain observed [3]. These pathways could include increased risks (such as media exposure, disruption to daily activities, social isolation, modified physical activity and sleep, negative effects, and fear of contagion) and lower the protective capacity and access to support programs (such as social support, emotion regulation, and access to clinical treatments), particularly in childhood obesity [22]. Moreover, scheduled follow-up visits for obese patients stopped during the lockdown, so a massive effort to seek new therapeutic strategies is needed.
In order to monitor psychosocial well-being related to body image and eating attitudes, technological devices could be implemented for obese patients as has been done for individuals with subthreshold psychological symptoms during the COVID-19 pandemic [23]. As telemedicine is becoming the “new normal” for healthcare providers, strategies like weekly self-weighing with a bathroom scale and other behaviour modifications able to favour the maintenance of adequate food intake and dietary quality may be adapted by dieticians/nutritionists to provide virtual counselling and healthy weight management practices at home. The time for using virtual strategies/activities and social networks has never been greater and may be used to support healthy behaviour practices [4]. For example, telemedicine could lead to the implementation of mindful eating and a newer concept of intuitive eating through modulating eating habits and emotional eating in response to external cues [24]. The familiar home environment and the absence of external stimuli could in fact allow the application of mindfulness-based approaches that may prevent weight gain, reducing food intake, and working by an increased awareness of internal, rather than external, cues to eat. Telenutrition support involves the interactive use, by a nutritionist, of email or mobile phone text messaging, smartphone applications (apps) or interactive web conferencing to implement the nutrition care process (nutrition assessment, diagnosis, intervention/plan of care, and monitoring and evaluation) with patients at a remote location, within the provisions of their state licensure as applicable [25, 26, 27]. So, the physician can verify the subject's adherence to diet and exercise, recommend therapeutic adjustments, and provide a set of strategies to promote alternative behaviours during critical situations or negative mood states. Moreover, telenutrition leads patients to follow the social pages of nutritional science that offer nutritional advice and nutritional news in simple language. Online support groups can be helpful in maintaining motivation and mitigating stress, especially in patients with eating disorders. It might be a useful tip to motivate daily change and exploit the sense of group and peer imitation, providing advice and exchanging recipes and experiences, besides helping patients to recognise official social pages and limit exposure to fake news. Web-based supporting technologies useful to counteract eating behaviour changes are summarised in Table 1.
Support to Maintain Food Intake and Dietary Quality
Maintaining adequate food intake for severely obese people is hard in normal times, but becomes a huge challenge during extraordinary events, such as the recent COVID-19 pandemic [28]. The fear of food shortages and the need to stock up led individuals to buy large quantities of food and to consequently eat more, together with an increased tendency for storing canned and ultra-processed products due to their secure storage and preparation, as well as the probability of eating while doing other activities. Ultra-processed foods are well known to have a high content of refined carbohydrates, which can lead to a change in insulin response, causing excess nutrient storage in adipose tissue [29], and may affect the brain reward system by leading to addictive-like behaviours and overconsumption.
The boredom, the economic strain, and the continuously hearing or reading about the pandemic could be stressful and inevitably cause overeating and looking for “comfort foods,” such as sweets. As the COVID-19 pandemic continues, the real fear of a decrease in food supplies contributes significantly to increasing the global burden of obesity, with decreased activity and stay-at-home measures. Moreover, as shown by Di Renzo et al. [3], adherence to a Mediterranean diet by Italian people during the COVID-19 pandemic was low, especially in elderly and obese people.
For all these reasons, obese patients need ongoing support to manage the disease during the pandemic [30]. First, we need to remind patients that obesity is a chronic disease and that even a slight weight gain can have consequences on comorbidities, such as a worsening of diabetes, hypertension, or sleep apnoea. Thanks to telemedicine, nutritionists, together with physiatrists/psychologists, could “virtually” enter patients' homes and maintain focus on the daily management of the disease. A virtual link could establish a supportive relationship and tailor-made strategies more oriented to the prevention and treatment of the patient, and not only to the treatment of the disease. It might be helpful to program daily food routines, regularly planning 3 meals and 2–3 snacks a day. Planning of the weekly cooking plan is crucial to optimise time and the need to go out for food purchases. It is important to give space for creativity and to take advantage of the extra time to motivate to cook and to taste new foods, encouraging patients in the adoption healthy recipes. Also, planning daily hydration, providing water in small sips during the day, but also herbal teas and infusions, to modulate the sense of hunger and satiety could be helpful. While nutritional education can benefit from a virtual system, the lack of detection of anthropometric measures useful in evaluating the effectiveness of the diet is on the other hand a limitation of such an application. For this reason, physical consultations must be arranged, for example by reducing their frequency and alternating them with telematic controls. Currently, video support has begun, but the effectiveness of this remote support is still to be determined by longitudinal and well-monitored studies. Table 1 summarise strategies to maintain a correct food intake and dietary quality.
Support to Maintain Adequate Physical Activity
The SARS-CoV-2 pandemic and the related lockdown and social distancing measures have had a tremendous impact on the individual level of habitual physical activity. Isolation has been effective in reducing the spread of SARS-CoV-2, but it also represented a severe limitation of patient movement, thus magnifying, in symptomatic patients, the risk of immobilisation syndromes. Individuals with obesity and chronic diseases are at risk of reduced skeletal muscle mass and function (sarcopenia) and increased body weight during forced inactivity periods [31]. This is a risk for malnutrition conditions with potential negative outcomes in the case of COVID-19 infection [32].
Physical activity is to be recommended during isolation for several reasons, including psychophysical well-being. Most importantly, moderately intense aerobic exercise is sufficient to improve immune health via enhanced recirculation of immunoglobulins, anti-inflammatory cytokines, neutrophils, NK cells, cytotoxic T cells, and immature B cells, with improved cellular immune function and metabolic health [33]. Also, high-intensity exercise has shown an anti-inflammatory response [34, 35, 36, 37]. However, high-intensity interval training (90% maximum heart rate, 3 times a week) decreased the IFN-γ/IL-4 ratio and increased TNF-α, while moderate-intensity continuous training (70% maximum heart rate, 5 times a week) decreased TNF-α in obese adults [38]; thus, high-intensity exercise may be dangerous in obesity and could help to exacerbate the SARS-CoV-2 virus [39]. Several examples of home exercises have been provided to the general/elderly population during lockdown. Among them, a manual by Ambrose and Verghese [40] provided examples of lying, sitting, and standing exercises with the aim of recommending a self-directed exercise program at home which does not require any special equipment.
Novel Strategies for Physical Activity and Rehabilitation
The European health and care systems are now facing multiple challenges, for which new digital technologies should become solutions to support their sustainability. Inpatient rehabilitation programs have strict inclusion criteria and high costs. Rehabilitation programs are largely performed in an outpatient setting. Home-based supervised programs, conversely, are heavy on logistics on the provider side. To circumvent this, telerehabilitation solutions have been developed and proposed to assist health facilities in the management of their services. Such solutions would allow physiotherapy to be delivered to a greater number of patients, increasing their reach, more quickly, and with comparable clinical results, thus improving the scalability of care.
Digital biofeedback systems for home-based physical rehabilitation have been available since 2016 and have been clinically validated for remote physiotherapy, demonstrating that a digital rehabilitation solution can reduce the dependence on human resources while ensuring better clinical outcomes than conventional rehabilitation, providing objective data for decision-making, but also working in tandem with clinical teams to ensure not only the scalability of care, but also enabling an exponential increase in the active caseload per clinician. A personalised treatment service can be offered through an app providing individualised exercises, activity advice, information, and coaching. The system can retrieve the actual movement data, as provided by motion sensors, as well as processed data, such as the number of correct movements, the reasons behind any wrong movements, and the reported pain and fatigue. An artificial Intelligence engine could check the patient's session data and determine, according to the latter, which changes to that patient's prescription are required to maximise the quality and efficiency of the therapy. The personalisation of the treatment is based on the patient's progress through the rehabilitation, by the feedback gathered through daily reporting, as well as a smart wearable band that captures the individual activity profile. The advantages of such technological solutions for rehabilitation are: (a) not requiring patients to physically be in the health facility to receive physiotherapy, and (b) they can be integrated with a health facility's electronic health record, thus filling the gap between in- and outpatient discontinuity. Moreover, the health system is currently subject to very high pressure and the role of telemedicine could be fundamental to increase the resilience of the system itself. This system is certainly not free from limitations, especially for older people, who might not be familiar with the use of digital tools or have availability of the digital tool itself, especially for those with a low income or socioeconomic status. Clearly telehealth will not replace physical consultations in all scenarios, but it can dramatically streamline quite a few scenarios, improving the lives of patients and reducing overall costs across the system.
Support for Bariatric Patients
Approximately 70% of patients who are candidates for bariatric surgery have a personal history of psychiatric pathology or psychologic distress, which can be exacerbated by the pandemic-induced stress environment before and after bariatric surgery [41, 42, 43, 44].
Bariatric Surgery Candidates
The COVID-19 pandemic has forced the postponement of many elective surgeries, including bariatric and metabolic surgery [41, 45]. Access to bariatric surgery procedures will see everything else gradually return to normal, and this, in addition to the increase in demand due to the temporary interruption of surgery, may lead to a further reduction in the availability/demand ratio of surgical need in this clinical setting [41].
With a view to prioritising candidates for bariatric procedures, the traditional weight-centric criterion, although still commonly used, does not adequately reflect the severity of the disease, and cannot therefore be considered in relation to current clinical needs [41]. In this scenario, a screening for preoperative COVID-19 is mandatory to identify appropriate criteria to prioritise patients in a period of limited capacity [41].
Post-Operative Bariatric Patients
Restricting access to non-urgent cases could adversely affect the proper monitoring of potential post-operative surgical and nutritional complications. It has proved important to try to avoid the sense of abandonment and isolation that patients often experience during the post-bariatric recovery period to limit the harm during and after the COVID-19 pandemic [46]. Telemedicine consultations, dietary and psychological evaluations in single/multidisciplinary surgery, always remotely, with the creation of a social network and online support, may be a viable solution to support the post-operative period and identify any complications early [45]. Telemedicine strategies supervised by specialised bariatric and metabolic surgery centres have been shown to have positive effects with regard to weight loss and psychosocial goals, comparable to those of in-presence therapy [47]. Remote cognitive behavioural therapy has been shown to be effective in improving mood and eating behaviour (anxiety and depression, emotional eating, and binge eating) in bariatric patients [48]. This approach could be useful also to identify signs and symptoms of potential nutritional deficiencies (decrease in vision, skin rash, easy fatigue, oedema or anasarca, neuropsychiatric signs, nausea, paraesthesia, changes in the bowel, asthenia), and to provide for the possibility of personal visits in urgent cases that suggest severe biochemical deficiencies or surgical complications [41, 45].
Conclusion
The COVID-19 pandemic is a huge challenge for both obese patients and health professionals, but it can also be an opportunity to implement the diffusion of telemedicine and telenutrition to improve the management of obesity, a disease in which physician-patient communication is fundamental and must never be interrupted. Health authorities should be urged to equip hospitals with such systems not only to attend to COVID-19 patients who stay in home isolation, but also to care for patients that need to be protected from a potentially harmful infection and guide them through the pandemic, explaining the future treatment/management, strategies/plan, and provide advice concerning general prevention measures. The current pandemic clearly underlines the importance of making these technical solutions available to healthcare providers to be better prepared for situations like these in the future.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research received no external funding.
Author Contributions
S.B.: conceptualisation. All authors: writing − original draft preparation.
R.D.A. and R.C. contributed equally to this work.
References
- 1.Allison DB, Downey M, Atkinson RL, Billington CJ, Bray GA, Eckel RH, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity (Silver Spring) 2008 Jun;16((6)):1161–77. doi: 10.1038/oby.2008.231. [DOI] [PubMed] [Google Scholar]
- 2.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China Novel Coronavirus Investigating and Research Team A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020 Feb;382((8)):727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020 Jun;18((1)):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhutani S, Cooper JA. COVID-19 related home confinement in adults: weight gain risks and opportunities. Obesity (Silver Spring) 2020 Sep;28((9)):1576–7. doi: 10.1002/oby.22904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussain A, Mahawar K, Xia Z, Yang W, El-Hasani S. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020 Jul-Aug;14((4)):295–300. doi: 10.1016/j.orcp.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 6.Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes. 2013 Mar;37((3)):333–40. doi: 10.1038/ijo.2012.62. [DOI] [PubMed] [Google Scholar]
- 7.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. International Diabetes Federation Task Force on Epidemiology and Prevention. Hational Heart, Lung, and Blood Institute. American Heart Association. World Heart Federation. International Atherosclerosis Society. International Association for the Study of Obesity Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; American heart association; World heart federation; International. Circulation. 2009 Oct;120((16)):1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 8.Lolmède K, Duffaut C, Zakaroff-Girard A, Bouloumié A. Immune cells in adipose tissue: key players in metabolic disorders. Diabetes Metab. 2011 Sep;37((4)):283–90. doi: 10.1016/j.diabet.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Ferrante AW., Jr Macrophages, fat, and the emergence of immunometabolism. J Clin Invest. 2013 Dec;123((12)):4992–3. doi: 10.1172/JCI73658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martí A, Marcos A, Martínez JA. Obesity and immune function relationships. Obes Rev. 2001 May;2((2)):131–40. doi: 10.1046/j.1467-789x.2001.00025.x. [DOI] [PubMed] [Google Scholar]
- 11.Hagau N, Slavcovici A, Gonganau DN, Oltean S, Dirzu DS, Brezoszki ES, et al. Clinical aspects and cytokine response in severe H1N1 influenza A virus infection. Crit Care. 2010;14((6)):R203. doi: 10.1186/cc9324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheridan PA, Paich HA, Handy J, Karlsson EA, Hudgens MG, Sammon AB, et al. Obesity is associated with impaired immune response to influenza vaccination in humans. Int J Obes. 2012 Aug;36((8)):1072–7. doi: 10.1038/ijo.2011.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hazan U, Romero IA, Cancello R, Valente S, Perrin V, Mariot V, et al. Human adipose cells express CD4, CXCR4, and CCR5 receptors: a new target cell type for the immunodeficiency virus-1? 2002;((4)) doi: 10.1096/fj.01-0947fje. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Desruisseaux MS, Nagajyothi, Trujillo ME, Tanowitz HB, Scherer PE. Adipocyte, adipose tissue, and infectious disease. Infect Immun. 2007 Mar;75((3)):1066–78. doi: 10.1128/IAI.01455-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020 Apr;9((1)):45. doi: 10.1186/s40249-020-00662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iacobellis G. COVID-19 and diabetes: can DPP4 inhibition play a role? Diabetes Res Clin Pract. 2020 Apr;162:108125. doi: 10.1016/j.diabres.2020.108125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Y, Shen C, Li J, Yuan J, Wei J, Huang F, et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J Allergy Clin Immunol. 2020 Jul;146((1)):119–127.e4. doi: 10.1016/j.jaci.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dayer JM, Chicheportiche R, Juge-Aubry C, Meier C. Adipose tissue has anti-inflammatory properties: focus on IL-1 receptor antagonist (IL-1Ra) Ann N Y Acad Sci. 2006 Jun;1069((1)):444–53. doi: 10.1196/annals.1351.043. [DOI] [PubMed] [Google Scholar]
- 19.Järvelä-Reijonen E, Karhunen L, Sairanen E, Muotka J, Lindroos S, Laitinen J, et al. The effects of acceptance and commitment therapy on eating behavior and diet delivered through face-to-face contact and a mobile app: a randomized controlled trial. Int J Behav Nutr Phys Act. 2018 Feb;15((1)):22. doi: 10.1186/s12966-018-0654-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hakala P, Karvetti RL, Rönnemaa T. Group vs. individual weight reduction programmes in the treatment of severe obesity—a five year follow-up study. Int J Obes Relat Metab Disord. 1993 Feb;17((2)):97–102. [PubMed] [Google Scholar]
- 21.Tomiyama AJ. Stress and Obesity. Annu Rev Psychol. 2019 Jan;70((1)):703–18. doi: 10.1146/annurev-psych-010418-102936. [DOI] [PubMed] [Google Scholar]
- 22.Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity (Silver Spring) 2020 Aug;28((8)):1382–5. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mills JP, Kaye KS, Mody L. COVID-19 in older adults: clinical, psychosocial, and public health considerations. JCI Insight. 2020 May;5((10)):10–5. doi: 10.1172/jci.insight.139292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017 Dec;30((2)):272–83. doi: 10.1017/S0954422417000154. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Xue H, Huang Y, Huang L, Zhang D. A Systematic Review of Application and Effectiveness of mHealth Interventions for Obesity and Diabetes Treatment and Self-Management. Adv Nutr. 2017 May;8((3)):449–62. doi: 10.3945/an.116.014100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hutchesson MJ, Rollo ME, Krukowski R, Ells L, Harvey J, Morgan PJ, et al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obes Rev. 2015 May;16((5)):376–92. doi: 10.1111/obr.12268. [DOI] [PubMed] [Google Scholar]
- 27.Peregrin T. Telehealth Is Transforming Health Care: What You Need to Know to Practice Telenutrition. J Acad Nutr Diet. 2019 Nov;119((11)):1916–20. doi: 10.1016/j.jand.2019.07.020. [DOI] [PubMed] [Google Scholar]
- 28.Bracale R, Vaccaro CM. Changes in food choice following restrictive measures due to Covid-19. Nutr Metab Cardiovasc Dis. 2020 doi: 10.1016/j.numecd.2020.05.027. (xxxx). DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019 Jul;30((1)):67–77.e3. doi: 10.1016/j.cmet.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Frühbeck G, Baker JL, Busetto L, Dicker D, Goossens GH, Halford JC, et al. European Association for the Study of Obesity Position Statement on the Global COVID-19 Pandemic. Obes Facts. 2020;13((2)):292–6. doi: 10.1159/000508082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morley JE, Kalantar-Zadeh K, Anker SD. COVID-19: a major cause of cachexia and sarcopenia? J Cachexia Sarcopenia Muscle. 2020 Aug;11((4)):863–5. doi: 10.1002/jcsm.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, et al. endorsed by the ESPEN Council ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020 Jun;39((6)):1631–8. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019 May;8((3)):201–17. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): does workout intensity matter? (A mini review of some indirect evidence related to obesity) Obes Med. 2020 Sep;19((Apr)):100245. doi: 10.1016/j.obmed.2020.100245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khaleghzadeh H, Afzalpour ME, Ahmadi MM, Nematy M, Sardar MA. Effect high-intensity interval training along with Oligopin supplementation on some inflammatory indices and liver enzymes in obese male Wistar rats with non-alcoholic fatty liver disease. Obes Med. 2020;17((October 2019)):100177. [Google Scholar]
- 36.TaheriChadorneshin H Cheragh-Birjandi S, Goodarzy S, Ahmadabadi F. The impact of high intensity interval training on serum chemerin, tumor necrosis factor-alpha and insulin resistance in overweight women. Obes Med. 2019;14((January)):100101. [Google Scholar]
- 37.de Souza DC, Matos VA, Dos Santos VO, Medeiros IF, Marinho CS, Nascimento PR, et al. Effects of high-intensity interval and moderate-intensity continuous exercise on inflammatory, leptin, IgA, and lipid peroxidation responses in obese males. Front Physiol. 2018 May;9((MAY)):567. doi: 10.3389/fphys.2018.00567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gerosa-Neto J, Antunes BM, Campos EZ, Rodrigues J, Ferrari GD, Rosa Neto JC, et al. Impact of long-term high-intensity interval and moderate-intensity continuous training on subclinical inflammation in overweight/obese adults. J Exerc Rehabil. 2016 Dec;12((6)):575–80. doi: 10.12965/jer.1632770.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Campbell JP, Turner JE. Debunking the Myth of Exercise-Induced Immune Suppression: Redefining the Impact of Exercise on Immunological Health Across the Lifespan. Front Immunol. 2018 Apr;9:648. doi: 10.3389/fimmu.2018.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ambrose A, Verghese J. Patient and Caregiver guide to managing covid-19 patients at home. 2020 Mar; DOI: [Google Scholar]
- 41.Rubino F, Cohen RV, Mingrone G, le Roux CW, Mechanick JI, Arterburn DE, et al. Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes Endocrinol. 2020 Jul;8((7)):640–8. doi: 10.1016/S2213-8587(20)30157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parmar C. Bariatric and Metabolic Surgery Can Prevent People with Obesity from COVID-19 Infection. Obes Surg. 2020;••• doi: 10.1007/s11695-020-04843-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sockalingam S, Leung SE, Cassin SE. The Impact of Coronavirus Disease 2019 on Bariatric Surgery: Redefining Psychosocial Care. Obesity (Silver Spring) 2020 Jun;28((6)):1010–2. doi: 10.1002/oby.22836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shakory S, Van Exan J, Mills JS, Sockalingam S, Keating L, Taube-Schiff M. Binge eating in bariatric surgery candidates: the role of insecure attachment and emotion regulation. Appetite. 2015 Aug;91:69–75. doi: 10.1016/j.appet.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 45.Yeo C, Ahmed S, Oo AM, Koura A, Sanghvi K, Yeo D. COVID-19 and Obesity-the Management of Pre- and Post-bariatric Patients Amidst the COVID-19 Pandemic. Obes Surg. 2020 Sep;30((9)):3607–9. doi: 10.1007/s11695-020-04670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coulman KD, MacKichan F, Blazeby JM, Donovan JL, Owen-Smith A. Patients' experiences of life after bariatric surgery and follow-up care: a qualitative study. BMJ Open. 2020 Feb;10((2)):e035013. doi: 10.1136/bmjopen-2019-035013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang CD, Rajaratnam T, Stall B, Hawa R, Sockalingam S. Exploring the Effects of Telemedicine on Bariatric Surgery Follow-up: a Matched Case Control Study. Obes Surg. 2019 Aug;29((8)):2704–6. doi: 10.1007/s11695-019-03930-4. [DOI] [PubMed] [Google Scholar]
- 48.David LA, Sijercic I, Cassin SE. Preoperative and post-operative psychosocial interventions for bariatric surgery patients: A systematic review. Obes Rev. 2020 Apr;21((4)):e12926. doi: 10.1111/obr.12926. [DOI] [PubMed] [Google Scholar]