Highlights
-
•
In the evaluation of a first seizure, the capture of epileptiform discharges is increased with 24-hour EEG recordings.
-
•
This likely stems from a combination of increased sampling and robust sleep recording.
-
•
Subtle seizures were also recorded by prolonging the EEG in a minority of first seizure presentations.
Abbreviations: VEEG, Video EEG; EDs, epileptiform discharges
Keywords: First unprovoked seizure, 24-Hour video EEG, Epilepsy, Epileptiform discharges, Diagnostic yield
Abstract
Objective
To assess the gain in detection of epileptiform abnormalities in 24-hour EEG recordings following the first seizure.
Methods
We identified patients who underwent 24-hour video EEG (VEEG) with “first seizure” as an indication. We noted the presence or absence of epileptiform discharges (EDs) in the VEEG study and the latency for the appearance of such discharges. We compared the rate of EDs during the initial 60 min with those occurring only later during the recording.
Results
Data from 25 patients, aged 15 to 59, were included. Of the 11 patients with EDs, eight (73%) appeared only after 60 min of recording. This equates to a 32% absolute increase in the detection of EDs across all patients. The latency to first EDs varied from one to 1080 min with a median of 170 min. In four cases, actual subtle seizures were recorded.
Conclusion
This study suggests an increase in the detection of EDs with the 24-hour studies compared to the traditional shorter recordings, in the context of a first seizure.
Significance
A standard EEG can be performed close to the seizure, followed by a longer up to 24-hour recording if the initial shorter study is unrevealing.
1. Introduction
A single unprovoked seizure is a common scenario encountered by practicing neurologists. The ensuing work up aims in part at quantifying the risk of seizure recurrence as a major determinant in the decision of starting an antiepileptic drug. In a published evidence-based guideline, the authors confirmed the following factors to be associated with an increased risk of seizure recurrence: a prior brain insult, an EEG with epileptiform abnormalities, or an epileptogenic lesion on brain imaging (Krumholz et al., 2015). In the absence of an antecedent neurological insult or imaging abnormalities, EEG findings have a decisive role in estimating the risk of seizure recurrence. Epileptiform discharges (EDs) on EEG increase the relative risk for seizure recurrence by a factor of 2.16 (Hauser et al., 1990). This risk applies both to adults and children. After a first unprovoked seizure in adults, epileptiform abnormalities were associated with an increase in seizure recurrence from 27.4% to 49.5%, and in children from 27–42% to 60–71% (Wirrell, 2010). While the role of EEG findings in the management of a single unprovoked seizure is well established, the guidelines do not specify the optimal duration of the EEG recording in this context.
In patients with established epilepsy, the sensitivity of the EEG to detect EDs increases with longer recording time or with repeated studies. Single routine EEGs in epilepsy are often non diagnostic; only 29–55% of patients with epilepsy have EDs on their first EEG. The yield can be increased to 72–90% by performing serial EEG studies (Doppelbauer et al., 1993, Baldin et al., 2014). The sensitivity to detect epileptiform abnormalities is also enhanced by performing extended outpatient EEGs compared to ≤ 30-minute routine recordings (Modur and Rigdon, 2008, Losey and Uber-Zak, 2008, Lee et al., 2013, Burkholder et al., 2016, Tatum et al., 2018), or by performing ≥ 24-hour ambulatory EEG or inpatient studies (Narayanan et al., 2008, Faulkner et al., 2012, Lee et al., 2013). In an outpatient ambulatory EEG study performed on 180 patients with epilepsy, the authors found a median latency to first interictal ED of 316 min. The detection rate of these discharges increased from 44% within four hours of recording to 85% and 95% after 24 and 48 h of recording respectively (Faulkner et al., 2012). Narayanan et al. (2008) reported on 46 patients with epilepsy admitted for EEG monitoring. Only 37% of them had epileptiform activity within the first 20 min of continuous recording (the minimum duration of a routine EEG), compared to 89% exhibiting EDs within the first 24 h. The literature is scarce on the yield of repeated or prolonged EEG recordings in the specific context of a first unprovoked seizure. Baldin et al. (2014) reported a yield of epileptiform abnormalities of 39% with the first EEG, increasing to 68% after the third. We found a single study evaluating the 24-hour video-EEG (VEEG) after a first unprovoked seizure; Chen et al. (2016) reported a rate of 42% of epileptiform abnormalities in 24-hour recordings. However, they did not compare the incremental yield across the recordings progression and did not comment on the latency to first EDs.
Performing short EEG studies with low sensitivity to detect abnormalities may be misleading when trying to stratify the risk of seizure recurrence after a first seizure. Thus, normal routine EEGs may be insufficient to reassure patients. Based on this assumption, some patients are now getting 24-hour EEG recordings following a first seizure. At our center, this is at times done after an unrevealing routine EEG or even instead of the routine study. Our study attempts to evaluate this practice and establish the cumulative sensitivity of a 24-hour EEG compared to shorter recordings, calculate the latency to epileptiform abnormalities, and study the effect of this practice on initiation of anti-seizure drugs following a single event.
2. Methods:
The study was approved by the institutional review boards at Hamad Medical Corporation (HMC) and Weill Cornell Medicine-Qatar. As the data was collected retrospectively, informed consent was waived.
2.1. Patients
Study subjects were identified from the epilepsy monitoring unit database at HMC. Patients admitted between May 2016 and January 2020 to investigate a first unprovoked seizure were selected. Two seizures occurring within 24 h were accepted. All subjects underwent a 24-hour VEEG recording. Patients with provoked acute symptomatic seizures or with an established pattern of recurring seizures fulfilling the diagnosis of epilepsy were excluded. We excluded also subjects with obvious abnormalities on neurological examination or neuroimaging studies, and subjects who were initially investigated for a first “unprovoked seizure” but later identified as having an alternative diagnosis to their paroxysmal events. Age and gender were noted for each subject. The specific characteristics of the index event were documented, such as the physical symptoms, loss of consciousness, duration, and timing, in order to reach a gross classification of the seizure.
2.2. EEG
All subjects underwent a 24-hour VEEG recording (Nihon Kohden), some after an unrevealing outpatient EEG. VEEG data was acquired using the standard 10–20 system for electrode placement, in addition to T1 and T2 temporal electrodes. The first 45–60 min of the recording are acquired following our extended EEG protocol and include activation procedures like hyperventilation, photic stimulation and attempted sleep. At the conclusion of the 24-hour recording, the EEG is reviewed page by page by a certified technologist and verified by an electroencephalographer. For the purpose of this study, the results were confirmed later on by another electroencephalographer. The presence or absence of EDs, the latency for the appearance of such discharges, their distribution, and the behavioral state they appear in were noted. EDs could be ictal or interictal. Other less specific EEG abnormalities (slowing, background asymmetry etc.) were also tabulated. The time elapsed from the index seizure to the VEEG study was counted.
2.3. Statistical analysis
Numeric variables are summarized using means ± standard deviations along with medians (Interquartile Range) and minimum/maximum observations. Categorical variables are summarized using frequency distributions. Clopper-Pearson method was used to estimate the 95% confidence interval for the percentage of EDs beyond one hour. The yield of the EEG to detect EDs in the first 60 min of the recording versus the rest of the 24-hour period was calculated. We then deduced the number of patients where these abnormalities would have been missed had the EEG recording been limited to just 60 min. The median latency to the first EDs in patients with such observable discharges was calculated.
3. Results
Data on 25 patients were available for this study. Patients’ age ranged between 15 and 59 years with a median of 32. The male to female ratio was 3/2. Subjects came from several different countries and cultures and were also highly variable in socioeconomic status. All patients except one were investigated for first generalized convulsive events, with only one subject labeled with a likely first focal seizure with impaired awareness. All except one had a single event, with one person experiencing two generalized convulsions within 24 h. There were no cases of status epilepticus. Eighteen patients (72%) had their seizures during wakefulness, while seven had sleep related seizures. Twelve patients (48%) had a previous “unrevealing” outpatient EEG. The VEEG was done two to 180 days after the index seizure episode, with a median of 45 days. Individual demographics, seizure and EEG characteristics are displayed in Table 1.
Table 1.
Individual demographics, seizure and EEG characteristics. L, left. R, right. EDs, epileptiform discharges. W, wakefulness. S, sleep. VEEG, video-EEG.
| Patient | Age (years) | Gender | State at seizure | Prior Routine EEG | Time from seizure to VEEG (Days) | VEEG Findings | Latency to EDs (minutes) |
|---|---|---|---|---|---|---|---|
| 1 | 48 | Female | W | No | 120 | Normal | . |
| 2 | 32 | Female | S | Yes | 105 | L Fronto-temporal slowing | . |
| 3 | 17 | Female | W | No | 75 | Normal | . |
| 4 | 20 | Female | W | No | 4 | Intermittent slowing, bilateral | . |
| 5 | 50 | Male | W | No | 60 | Normal | . |
| 6 | 15 | Female | W | Yes | 180 | R Frontal spike/wave | 2 |
| 7 | 50 | Male | S | No | 45 | Normal | . |
| 8 | 28 | Male | S | No | 30 | Normal | . |
| 9 | 38 | Female | W | No | 7 | L Fronto-temporal sharp waves | 15 |
| 10 | 16 | Male | W | No | 2 | L temporal seizure | 1080 |
| 11 | 37 | Male | W | No | 12 | L temporal seizure & sharp waves | 170 |
| 12 | 55 | Male | S | No | 21 | L Temporal spikes | 134 |
| 13 | 59 | Male | W | Yes | 90 | Normal | . |
| 14 | 32 | Male | W | Yes | 4 | Normal | . |
| 15 | 15 | Female | W | No | 30 | Generalized Spike & wave | 1 |
| 16 | 30 | Female | S | Yes | 60 | L temporal sharp waves | 806 |
| 17 | 52 | Female | W | Yes | 30 | Normal | . |
| 18 | 32 | Male | S | No | 45 | Normal | . |
| 19 | 21 | Male | W | No | 5 | R frontal sharp and slow waves | 660 |
| 20 | 28 | Male | W | Yes | 8 | R frontal seizures | 780 |
| 21 | 26 | Male | W | Yes | 38 | Normal | . |
| 22 | 35 | Male | S | Yes | 65 | L frontal spikes | 785 |
| 23 | 48 | Male | W | Yes | 64 | Multiple electrographic seizures (onset Cz & Fz) | 90 |
| 24 | 38 | Female | W | Yes | 116 | Normal | . |
| 25 | 51 | Male | W | Yes | 82 | Normal | . |
Of the 25 patients, 11 (44%) showed EDs at any time during the VEEG recording, two (8%) had just non-specific abnormalities (EEG slowing), and 12 (48%) had normal studies. All detected EDs were focal, except one case with generalized spike/wave complexes. EDs were exclusively seen during sleep in six of the 11 patients (54.5%) with such VEEG findings, while four showed subtle or pure electrographic seizures (Fig. 1).
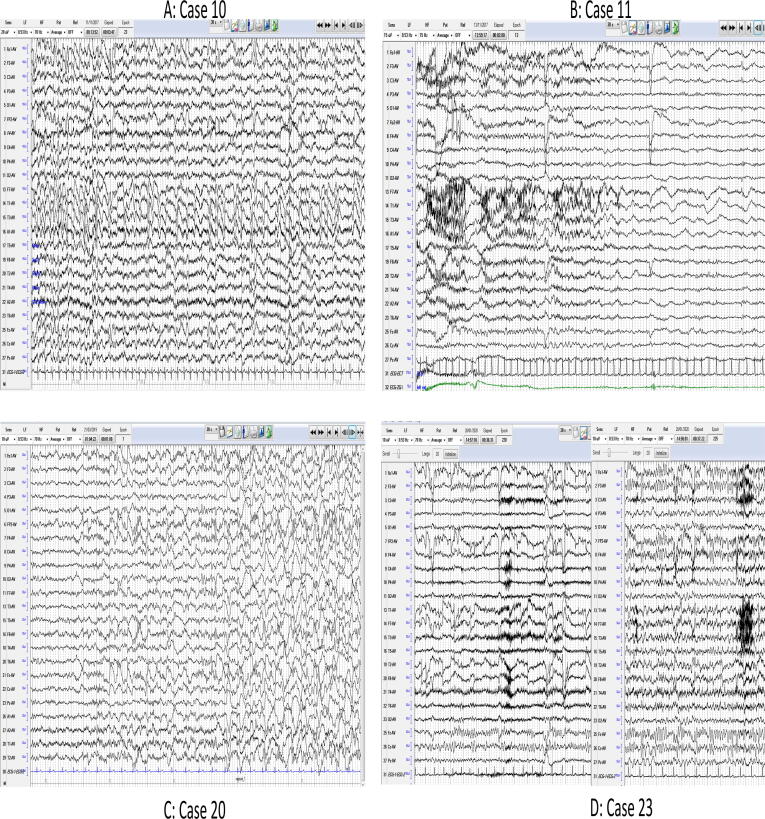
Fig. 1.
Samples of ictal EEG collected from four patients. A: Case 10, subtle seizure out of sleep with a left temporal evolving discharge (patient opens eyes and fidgets in bed, amnestic to event). B: Case 11, brief seizure during wakefulness with a left temporal subtle theta/delta rhythmic evolving activity, followed by focal delta slowing (patient exhibits repetitive grimacing and manual automatisms, amnestic to event). C: Case 20, three events during wakefulness and sleep, with a seemingly frontal onset (right) and evolution. No video available for the event during wakefulness, with minor arousal like movements noted during sleep related events. Patient unaware of any events. D: Case 23, multiple EEG seizures during wakefulness and sleep with no clear consistent clinical manifestations, onset at Fz-Cz midline electrodes with bilateral electrographic evolution. The shown sample exhibits discontinuous portions of a seizure to better visually demonstrate the ictal evolution.
The latency to first EDs when present in the VEEG recording varied from one to 1080 min with a median of 170 min.
Of the 11 patients with epileptiform abnormalities, eight (73%, 95% confidence interval 39–94) showed their first discharges only after the initial 60 min of recording, which is well beyond the routine (20–40 min) and even extended (41–60 min) EEG time frame. This means that in patients with EDs, approximately three out of every four patients would have these discharges missed had the recording been shorter than one hour, with a relative yield increase of 73% of the 24-hour VEEG recording compared to the shorter extended EEG. Since eight (32%) of the total study cohort displayed EDs beyond one hour of recording, this translates to the following formula: for each three patients who underwent 24-hour VEEG for a first seizure, roughly one additional patient was identified with epileptiform abnormalities that would have been otherwise missed with just a 60-minute EEG recording.
The 11 patients with ictal and interictal EDs were subsequently started on anti-seizure medications, based mainly on the EEG information.
4. Discussion
The risk of seizure recurrence following a first unprovoked seizure is not uniform and varies across different studies from 40 to 60% with extended follow up (Berg, 2008, Krumholz et al., 2015). Appearance of EDs in corresponding EEG studies grossly doubles the risk of seizure recurrence (Hauser et al., 1990, Krumholz et al., 2015). Single standard EEGs have a relatively low sensitivity at detecting interictal EDs after a first unprovoked seizure, ranging from 21 to 48% (van Donselaar et al., 1992, King et al., 1998, Neufeld et al., 2000, Baldin et al., 2014, Wyman et al., 2017). Repeated EEG studies reveal newer epileptiform abnormalities in many patients, bringing the cumulative sensitivity of serial studies to over 60% (King et al., 1998, Baldin et al., 2014). We found two studies that specifically looked at the yield of repeated sleep-deprived EEG after a first standard EEG without epileptiform abnormalities. Carpay et al. (1997) reported a detection rate of 33% of epileptiform abnormalities in sleep-deprived recordings of children and adolescents with a first seizure and an unrevealing first standard EEG. In a study evaluating 300 adults and children with a first seizure presentation, King et al. (1998) found a cumulative rate of 61% of all patients had generalized or focal epileptiform abnormalities after the second, sleep-deprived EEG. However, repeatedly applying EEG electrodes and repeating studies may be inconvenient and uncomfortable for many patients. An attractive alternative may consist of less numerous but more prolonged recordings. Prolonged EEG monitoring facilities are now readily available. This raises an important management choice since the presence of EDs would influence the decision to start antiepileptic medications to reduce the risk of seizure recurrence. Early therapy with an antiepileptic drug significantly reduces seizure risk recurrence compared to deferred treatment, at least on the short term (First Seizure Trial Group, 1993, Marson et al., 2005, Krumholz et al., 2015, Leone et al., 2016).
Our study is an important step in assessing the value of 24-hour VEEG in the evaluation of the first seizure. We used the first 60 min of the continuous recording as our benchmark, roughly equivalent to the standard “extended” EEG at our institution. This study shows that increasing the duration of the EEG recording close to 24 h increases the relative yield of new EDs by approximately 73%, and the absolute yield by 32%. This implies that almost three quarters of the recordings with EDs would have been missed had the study been limited to one hour or less (the typical recording time for a routine or extended EEG), with the resultant potential delay in the consideration of anti-epileptic treatment. Also, in practical terms, the VEEG recording contributed additional useful information beyond the reach of the shorter routine or extended recording in one of each three performed studies. The improved yield from more prolonged monitoring likely stems from a combination of increased sampling and robust sleep recording. Interictal EDs are often infrequent, and sometimes only occur in sleep (Ferrillo et al., 2000, Tatum et al., 2018). Exclusive activation of such abnormalities during sleep was noted in more than half of our positive recordings. Including a full night of EEG recording in our study protocol likely contributed to improved yield; deep sleep stages may not be reached or sustained in a short standard recording. Additionally, we recorded actual seizures in a small proportion of patients. The seizures were too subtle to be clearly noticed or identified by casual witnesses without EEG data.
Longer recordings may confer a higher confidence in calling interictal epileptiform transients even when they appear early on. The first discharges may be less well formed. The potential recurrence of such discharges throughout the recording would allow better confirmation of their consistent epileptiform morphology and distinction from benign sharply contoured transients.
In our series, the patients with focal EDs outnumbered those with generalized spike/wave complexes by a ratio of 10 to one. This skew towards focal epilepsy is likely multifaceted. First, our group does not include children or adolescents below the age of 15. Genetic or idiopathic generalized epilepsy is often diagnosed in childhood or adolescence (Gallentine and Mikati, 2012, Hantus, 2015, Mullen and Berkovic, 2018). In the same disease context, many generalized epilepsies often start with subtle seizure types (i.e., myoclonus), before the first generalized tonic-clonic event. Thus, what looks like a first generalized convulsion turns out to be not the first seizure upon detailed history (Panayiotopoulos et al., 1994, King et al., 1998, Hantus, 2015). Lastly, most patients end up with a standard EEG first after a single seizure. Generalized EDs tend to appear after a shorter latency compared to focal ones and are likely to be identified more often in routine short EEG recordings (Walczak et al., 1993, Losey and Uber-Zak, 2008, Narayanan et al., 2008, Lee et al., 2013, Tatum et al., 2018). Thus, many of these patients are filtered out as they do not need to progress to longer 24-hour EEG recordings.
Our VEEG studies were performed on an inpatient basis; we lack continuous ambulatory EEG technology at our center. The inpatient setting may permit a better quality recording, but since the duration of each study does not exceed 24 h, an ambulatory continuous EEG alternative may be cheaper and equally adequate as the deterioration of the applied scalp electrodes might not be a problem. Our results can be translated to the outpatient assessment of EDs after a single unprovoked seizure using continuous ambulatory EEG where available.
We found only a single report in the literature on the use of 24-hour VEEG in evaluating a first unprovoked seizure (Chen et al., 2016). The authors recruited 134 patients, included subjects with abnormal brain imaging, and found 42% with epileptiform abnormalities in their 24-hour recording. This is similar to the rate observed in our study. They confirmed a higher seizure recurrence risk in these patients, but did not specify the latency to first epileptiform abnormalities and did not comment on the incremental yield of the continuous recording. None of their patients experienced seizures during the VEEG recording.
Past studies confirmed that, upon further scrutiny, 28–57% of patients presenting for the first time with a seizure have experienced prior typically subtle epileptic events (King et al., 1998, Jallon et al., 2001, Firkin et al., 2015). Our patients were screened repeatedly about such history, and were concluded to have none. However, to our knowledge, the capture of actual seizures in the EEG work up after a first seizure has not been studied in the literature. The capture of such seizures in a minority of our patients is rather unique and warrants emphasis. The events were not recognized by the patients, and lead ultimately to a diagnosis of epilepsy based on evidence of seizure recurrence (Fisher et al., 2014).
The retrospective nature of our study, the selective and relatively small number of patients represent limitations to the generalizability of our results. The wide range of time elapsing between the seizure event and the actual VEEG recording is another limiting factor. Some studies noted significant increased EEG yield if it is done closer to the index first event (King et al., 1998, Sofat et al., 2016, Wyman et al., 2017).
5. Conclusion:
This study was conducted to evaluate the yield of 24 h VEEG in the evaluation of the first unprovoked seizure, particularly in the absence of other high risk factors for recurrence. It suggests an increase in the detection of EDs with the 24-hour studies compared to the traditional shorter recordings. We believe that a routine or extended EEG should be performed close to the seizure, followed by a 24-hour recording if the initial shorter study is unrevealing. This approach will maximize the early identification of subjects with high risk for seizure recurrence, allowing for early intervention. The patients with ictal and interictal EDs would subsequently be counseled about starting anti-seizure medications, based mainly on the EEG information. Future larger studies can verify the current findings and investigate the effect of the time to VEEG from seizure presentation on the recording sensitivity in terms of detecting EDs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
N. Haddad, G. Melikyan, G. Alarcon and A. Alrabi conceived and designed the project. N. Haddad, G. Melikyan, G. Alarcon, A. Alrabi, M. Siddiqi, E. Ali, B. Mesraoua, H AlHail, A Syamala and F. Kazi executed the project and acquired the data. N. Haddad, Y. Shaheen, A. Al-Abdulghani, and Z. Mahfoud performed the analysis and interpretation of data. N. Haddad and Z. Mahfoud drafted the manuscript. All authors critically reviewed and edited the manuscript before approving the final version for submission.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Baldin E., Hauser W.A., Buchhalter J.R., Hesdorffer D.C., Ottman R. Yield of epileptiform electroencephalogram abnormalities in incident unprovoked seizures: a population-based study. Epilepsia. 2014;55(9):1389–1398. doi: 10.1111/epi.2014.55.issue-910.1111/epi.12720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg A.T. Risk of recurrence after a first unprovoked seizure. Epilepsia. 2008;49(Suppl 1):13–18. doi: 10.1111/j.1528-1167.2008.01444.x. [DOI] [PubMed] [Google Scholar]
- Burkholder D.B., Britton J.W., Rajasekaran V., Fabris R.R., Cherian P.J., Kelly-Williams K.M., So E.L., Nickels K.C., Wong-Kisiel L.C., Lagerlund T.D., Cascino G.D., Worrell G.A., Wirrell E.C. Routine vs extended outpatient EEG for the detection of interictal epileptiform discharges. Neurology. 2016;86(16):1524–1530. doi: 10.1212/WNL.0000000000002592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpay J.A., Weerd A.W., Schimsheimer R.J., Stroink H., Brouwer O.F., Peters A.C.B., Donselaar C.A., Geerts A.T., Arts W.F.M. The diagnostic yield of a second EEG after partial sleep deprivation: a prospective study in children with newly diagnosed seizures. Epilepsia. 1997;38(5):595–599. doi: 10.1111/epi.1997.38.issue-510.1111/j.1528-1157.1997.tb01145.x. [DOI] [PubMed] [Google Scholar]
- Chen T., Si Y., Chen D., Zhu L., Xu D.a., Chen S., Zhou D., Liu L. The value of 24-hour video-EEG in evaluating recurrence risk following a first unprovoked seizure: a prospective study. Seizure. 2016;40:46–51. doi: 10.1016/j.seizure.2016.06.005. [DOI] [PubMed] [Google Scholar]
- Doppelbauer A., Zeitlhofer J., Zifko U., Baumgartner C., Mayr N., Deecke L. Occurrence of epileptiform activity in the routine EEG of epileptic patients. Acta Neurol. Scand. 1993;87(5):345–352. doi: 10.1111/j.1600-0404.1993.tb04115.x. [DOI] [PubMed] [Google Scholar]
- Faulkner H.J., Arima H., Mohamed A. Latency to first interictal epileptiform discharge in epilepsy with outpatient ambulatory EEG. Clin. Neurophysiol. 2012;123(9):1732–1735. doi: 10.1016/j.clinph.2012.01.023. [DOI] [PubMed] [Google Scholar]
- Ferrillo F., Beelke M., Nobili L. Sleep EEG synchronization mechanisms and activation of interictal epileptic spikes. Clin. Neurophysiol. 2000;111(Suppl 2):S65–S73. doi: 10.1016/s1388-2457(00)00404-1. [DOI] [PubMed] [Google Scholar]
- Firkin A.L., Marco D.J., Saya S., Newton M.R., O'Brien T.J., Berkovic S.F., McIntosh A.M. Mind the gap: multiple events and lengthy delays before presentation with a “first seizure”. Epilepsia. 2015;56(10):1534–1541. doi: 10.1111/epi.13127. Epub 2015 Aug 31. [DOI] [PubMed] [Google Scholar]
- First Seizure Trial Group (FIR.S.T. Group). Randomized clinical trial on the efficacy of antiepileptic drugs in reducing the risk of relapse after a first unprovoked tonic-clonic seizure. Neurology. 1993;43:478‐483. doi:10.1212/wnl.43.3_part_1.478. [DOI] [PubMed]
- Fisher R.S., Acevedo C., Arzimanoglou A., Bogacz A., Cross J.H., Elger C.E., Engel J., Jr, Forsgren L., French J.A., Glynn M., Hesdorffer D.C., Lee B.I., Mathern G.W., Moshé S.L., Perucca E., Scheffer I.E., Tomson T., Watanabe M., Wiebe S. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475–482. doi: 10.1111/epi.12550. Epub 2014 Apr 14. [DOI] [PubMed] [Google Scholar]
- Gallentine W.B., Mikati M.A. Genetic generalized epilepsies. J. Clin. Neurophysiol. 2012;29(5):408–419. doi: 10.1097/WNP.0b013e31826bd92a. [DOI] [PubMed] [Google Scholar]
- Hantus S. Idiopathic generalized epilepsy syndromes of childhood and adolescence. In: Wyllie E., editor. Treatment of epilepsy, principles and practice. Wolters Kluwer; 2015. pp. 248–258. [Google Scholar]
- Hauser W.A., Rich S.S., Annegers J.F., Anderson V.E. Seizure recurrence after a 1st unprovoked seizure: an extended follow-up. Neurology. 1990;40(8):1163–1170. doi: 10.1212/wnl.40.8.1163. [DOI] [PubMed] [Google Scholar]
- Jallon P., Loiseau P., Loiseau J. Newly diagnosed unprovoked epileptic seizures: presentation at diagnosis in CAROLE study. Coordination Active du Réseau Observatoire Longitudinal de l' Epilepsie. Epilepsia. 2001;42(4):464–475. doi: 10.1046/j.1528-1157.2001.31400.x. [DOI] [PubMed] [Google Scholar]
- King M.A., Newton M.R., Jackson G.D., Fitt G.J., Mitchell L.A., Silvapulle M.J., Berkovic S.F. Epileptology of the first-seizure presentation: a clinical, electroencephalographic, and magnetic resonance imaging study of 300 consecutive patients. Lancet. 1998;352(9133):1007–1011. doi: 10.1016/S0140-6736(98)03543-0. [DOI] [PubMed] [Google Scholar]
- Krumholz A., Wiebe S., Gronseth G.S., Gloss D.S., Sanchez A.M., Kabir A.A., Liferidge A.T., Martello J.P., Kanner A.M., Shinnar S., Hopp J.L., French J.A. Evidence-based guideline: management of an unprovoked first seizure in adults: report of the guideline development subcommittee of the american academy of neurology and the american epilepsy society. Neurology. 2015;84(16):1705–1713. doi: 10.1212/WNL.0000000000001487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.H., Lim S.N., Lien F., Wu T. Duration of electroencephalographic recordings in patients with epilepsy. Seizure. 2013;22(6):438–442. doi: 10.1016/j.seizure.2013.02.016. [DOI] [PubMed] [Google Scholar]
- Leone MA, Giussani G, Nolan SJ, Marson AG, Beghi E. Immediate antiepileptic drug treatment, versus placebo, deferred, or no treatment for first unprovoked seizure. Cochrane Database Syst Rev. 2016;2016(5):CD007144. doi:10.1002/14651858.CD007144.pub2. [DOI] [PMC free article] [PubMed]
- Losey T.E., Uber-Zak L. Time to first interictal epileptiform discharge in extended recording EEGs. J. Clin. Neurophysiol. 2008;25(6):357–360. doi: 10.1097/WNP.0b013e31818f008a. [DOI] [PubMed] [Google Scholar]
- Marson A., Jacoby A., Johnson A., Kim L., Gamble C., Chadwick D. Immediate versus deferred antiepileptic drug treatment for early epilepsy and single seizures: a randomised controlled trial. Lancet. 2005;365(9476):2007–2013. doi: 10.1016/S0140-6736(05)66694-9. [DOI] [PubMed] [Google Scholar]
- Modur P.N., Rigdon B. Diagnostic yield of sequential routine EEG and extended outpatient video-EEG monitoring. Clin. Neurophysiol. 2008;119(1):190–196. doi: 10.1016/j.clinph.2007.09.128. [DOI] [PubMed] [Google Scholar]
- Mullen S.A., Berkovic S.F. ILAE genetics commission. Genetic Generalized epilepsies. Epilepsia. 2018;59(6):1148–1153. doi: 10.1111/epi.2018.59.issue-610.1111/epi.14042. [DOI] [PubMed] [Google Scholar]
- Narayanan J.T., Labar D.R., Schaul N. Latency to first spike in the EEG of epilepsy patients. Seizure. 2008;17(1):34–41. doi: 10.1016/j.seizure.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Neufeld M.Y., Chistik V., Vishne T.H., Korczyn A.D. The diagnostic aid of routine EEG findings in patients presenting with a presumed first-ever unprovoked seizure. Epilepsy Res. 2000;42(2–3):197–202. doi: 10.1016/s0920-1211(00)00183-2. [DOI] [PubMed] [Google Scholar]
- Panayiotopoulos C.P., Obeid T., Tahan A.R. Juvenile myoclonic epilepsy: a 5-year prospective study. Epilepsia. 1994;35(2):285–296. doi: 10.1111/epi.1994.35.issue-210.1111/j.1528-1157.1994.tb02432.x. [DOI] [PubMed] [Google Scholar]
- Sofat P., Teter B., Kavak K.S., Gupta R., Li P. Time interval providing highest yield for initial EEG in patients with new onset seizures. Epilepsy Res. 2016;127:229–232. doi: 10.1016/j.eplepsyres.2016.08.024. [DOI] [PubMed] [Google Scholar]
- Tatum W.O., Rubboli G., Kaplan P.W., Mirsatari S.M., Radhakrishnan K., Gloss D., Caboclo L.O., Drislane F.W., Koutroumanidis M., Schomer D.L., Kasteleijn-Nolst Trenite D., Cook M., Beniczky S. Clinical utility of EEG in diagnosing and monitoring epilepsy in adults. Clin. Neurophysiol. 2018;129(5):1056–1082. doi: 10.1016/j.clinph.2018.01.019. [DOI] [PubMed] [Google Scholar]
- van Donselaar C.A., Schimsheimer R.J., Geerts A.T., Declerck A.C. Value of the electroencephalogram in adult patients with untreated idiopathic first seizures. Arch. Neurol. 1992;49(3):231–237. doi: 10.1001/archneur.1992.00530270045017. [DOI] [PubMed] [Google Scholar]
- Walczak T.S., Sheuer M.L., Resor S., Pedley T. Prevalence and features of epilepsy without interictal epileptiform discharges. Neurology. 1993;27:330–334. [Google Scholar]
- Wirrell E.C. Prognostic significance of interictal epileptiform discharges in newly diagnosed seizure disorders. J. Clin. Neurophysiol. 2010;27(4):239–248. doi: 10.1097/WNP.0b013e3181ea4288. [DOI] [PubMed] [Google Scholar]
- Wyman A.J., Mayes B.N., Hernandez-Nino J., Rozario N., Beverly S.K., Asimos A.W. The first-time seizure emergency department electroencephalogram study. Ann. Emerg. Med. 2017;69(2):184–191.e1. doi: 10.1016/j.annemergmed.2016.08.004. [DOI] [PubMed] [Google Scholar]