Abstract
Purpose
The aim of this study was to compare the efficacy of the tunnel technique for root coverage using a new xenogeneic acellular dermal matrix vs. connective tissue grafting (CTG) for the treatment of multiple maxillary adjacent recessions (recession type 1) at 12 months postoperatively.
Methods
This study enrolled 12 patients with at least 3 contiguous, bilateral, symmetrical maxillary gingival recessions (i.e., at least 6 recessions per patient). In total, 74 recessions were treated using the modified coronally advanced tunnel (MCAT) technique combined with a novel porcine-derived acellular dermal matrix (PADM) at 37 test sites or CTG at 37 control sites. The following clinical parameters were measured: recession height, clinical attachment level, width of keratinized tissue, probing depth, recession width, gingival thickness, mean root coverage (MRC), and complete root coverage (CRC). Comparisons between test and control groups were made for pain visual analog scale scores at 14 days.
Results
At 12 months, the MCAT with PADM (test) yielded a statistically significant improvement in all clinical parameters studied. MRC was significantly higher on the control sides (80.6%±23.7%) than on the test sides (68.8%±23.4%). Similarly, CRC was 48.7%±6.8% on the control sides (CTG), in contrast to 24.3%±8.2% on the test sides (PADM). Statistically significant differences were observed in favor of the control sides for all clinical parameters studied. Nevertheless, the MCAT in adjunction with PADM was clearly superior at reducing mean and maximum patient-reported postoperative pain intensity and pain duration in the first week after surgery.
Conclusions
The use of PADM to treat multiple recessions improved clinical parameters at 12 months, but these outcomes were nevertheless poorer than those observed for CTG. However, PADM reduced morbidity, particularly the pain experienced by patients.
Trial Registration
ClinicalTrials.gov Identifier: NCT03162016
Keywords: Acellular dermis, Connective tissue, Gingival recession, Oral surgical procedures
Graphical Abstract
INTRODUCTION
Connective tissue grafting (CTG) helps to meet patients' needs, particularly in the setting of gingival recession. Good clinical results and the availability of long-term data have made this technique the gold standard for treating periodontal recession [1,2].
However, the need for a second donor site, generally the palate, leads to high morbidity rates. There are risks of donor site necrosis and hemorrhage due to the harvesting procedure and prolonged operative time [3,4]. The risk of developing edema and moderate to severe postoperative pain increases by 3%–4%, respectively, with each minute of the procedure [5]. Moreover, the amount of autologous graft available may be limited for treating multiple recessions [6]. Tissue engineers are now working to help periodontists by attempting to develop alternative materials to autologous CTGs. Allogeneic acellular dermal matrices (ADMs) are currently considered the alternative with the closest clinical results to CTG [7], although their human origin has led to their being banned in some countries or may cause rejection in some patients. Animal-derived materials have therefore been marketed, with an example being xenogeneic bilayer collagen matrices (CMXs). These can be used to increase keratinized tissue (KT) height and to cover single or multiple recessions [3,8], with or without flap coverage. A novel porous porcine collagen matrix has recently been introduced. Since one of its potential advantages is maintaining volume stability, it is referred to as a volume-stable collagen matrix [9]. This matrix must be submerged and has yielded good preliminary tissue augmentation results around teeth and implants [10,11]. Very recently, a new porcine-derived acellular dermal matrix (PADM) (Mucoderm®, Botiss Dental, Straumann Group, Basel, Switzerland) has arrived on the market, which contains elastin and native type I and type III collagen and has undergone no further chemical treatment. Its clinical efficacy has been discussed in case series [12,13] and randomized controlled studies [14] conducted in 2 separate patient groups (a test group and a control group). Only 1 recent split-mouth study has compared the efficacy of this matrix relative to autologous grafts at 12 months, and that study only investigated mandibular recessions [15]. No study has investigated patient pain at a short-term follow-up.
With the above background in mind, this split-mouth prospective randomized study investigated only maxillary recessions and aimed to compare clinical outcomes with the modified coronally advanced tunnel (MCAT) technique combined with the new PADM (test side) or CTG (control) at 12 months. The MCAT is one of the most predictable recession coverage procedures for multiple recessions [16,17]. The secondary aim of our study was to compare patient-reported pain at each site during early wound healing. In this setting, we hypothesized that PADM would yield equivalent clinical outcomes and result in less postoperative pain than CTG in the treatment of contiguous maxillary Cairo recessions of type 1 (RT1: gingival recession with no loss of interproximal attachment) [18].
MATERIALS AND METHODS
Study design and population
This prospective single-center split-mouth randomized study was conducted in 12 patients (8 women and 4 men) aged 23 to 55 years (mean, 41.2 ± 10.9 years) who were treated in the Periodontics Department of Nice University Hospital, for contiguous, bilateral, symmetrical Cairo RT1 maxillary gingival recessions. Randomization was conducted by the clinical research board of the University Hospital, using a computer-generated program. The random allocation sequence was handed to the surgeon before the procedure and specified the test side and control side. The CTG was harvested from the same palatal site as the control side. All patients signed an informed consent form before entering the study, which complied with the 1975 Declaration of Helsinki as revised in 2000, and which was approved by both the CCP Sud Méditerranée II Institutional Review Board (No. 16.085) and French National Agency for Medicines and Health Products Safety; ClinicalTrials.gov identifier NCT03162016.
The inclusion criteria were as follows: patients aged over 18 years with at least 6 type 1 (RT1) maxillary gingival recessions more than 1 mm high [18], a detectable cementoenamel junction (CEJ: type A), no non-carious cervical lesions (class −: absence of cervical step) [19], non-smokers, a full-mouth plaque score and a full-mouth bleeding on probing score <20%, and no active periodontal disease. Pregnant women, patients with systemic diseases that can affect healing, and those taking medications that interfere with healing (steroids) were not included. A total of 74 recessions were treated (37 test recessions and 37 controls). Treatment procedures were conducted from May 2017 to June 2018.
Patients were educated on oral hygiene and shown how to brush their teeth atraumatically using the roll technique and a soft-bristle brush.
Clinical measurements
The following clinical parameters were recorded before surgery and 12 months after surgery: recession height (RH), which was the distance between the CEJ and the most apical limit of the gingival margin (GM); recession width (RW), as represented by a horizontal measurement of gingival recession at the CEJ; probing depth (PD) as measured using a periodontal probe at the mid-buccal aspect of the tooth from the GM to the bottom of the sulcus; KT width, which was the distance between the most apical point of the GM and the mucogingival junction (MGJ); and gingival thickness (GT), as measured using a needle pierced through the center of a circular-shaped silicone marker measuring 3 mm in diameter. The edge of the marker was positioned at the soft tissue margin, providing a distance from the margin of 1.5 mm; the clinical attachment level (CAL) corresponded to the addition of PD and RH. To evaluate the effectiveness of the treatment, additional calculations were performed: RH reduction was calculated as the difference between RH at baseline and RH at 12 months postoperatively. Mean root coverage (MRC) was calculated by dividing RH reduction by RH at baseline, and multiplied by 100. Complete root coverage (CRC) was determined as the percentage of recession with complete coverage achieved. KT width gain was calculated as the difference between KT width at 12 months postoperatively and KT width at baseline, while GT gain corresponded to the difference between GT at 12 months postoperatively and GT at baseline.
A questionnaire was given to each patient on the day of surgery. It was used to assess pain at each graft site (test or control) using a visual analog scale (VAS) from 0 to 10 over the first 14 days after surgery. To evaluate pain, 3 variables were defined: the number of days with pain: the patient’s total number of days with a pain VAS score >2; the mean pain VAS score (the patient's mean pain VAS score reported during 14 days); and the maximum pain VAS score (the patient's maximum pain VAS score during 14 days).
All measurements were made by the same examiner (S. Vincent-Bugnas). At the end of the study, the investigator who assessed outcomes (G. Borie) was blinded.
Surgical protocol
After a clinical examination and inclusion in the study, the randomization of each patient was sent to the surgeon, specifying the test side to be treated using PADM (Mucoderm®, Botiss Dental, Straumann Group, Switzerland) and the control side to be treated using CTG. Both sides were treated during the same operation.
After local infiltration of articaine hydrochloride (4%) with 1:100,000 epinephrine (Septanest SP®, Septodont, Saint-Maur-des-Fossés, France), exposed root surfaces were cleaned using scalers to remove plaque and any calculus deposits. The surgical technique employed was initially described by Azzi and Etienne [20] and then modified by Aroca et al. [21]. Intrasulcular incisions were made at each recession site on both the test and control sides. Using tunneling instruments (TKN1® and TKN2®, Hu-Friedy Mfg. Co., LLC, Chicago, IL, USA), a full-thickness flap was performed down to the MGJ and beneath each papilla, which remained attached by its tip. Next, a partial thickness flap was made down to the MGJ to ensure tension-free tunnel advancement.
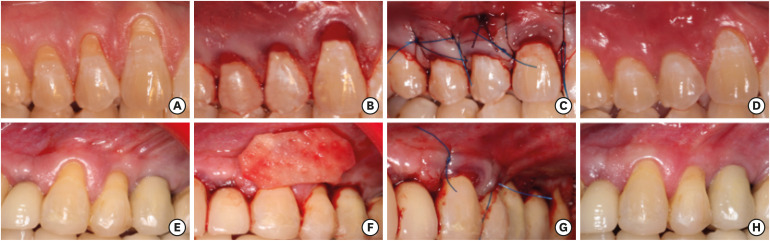
The PADM was then cut to the appropriate size and soaked in a sterile saline solution for 20 minutes in accordance with a previously validated protocol [13]. Meanwhile, the CTG was harvested on the control side using the single-incision technique described by Hürzeler and Weng [22]. A graft approximately 1.5 mm thick was harvested, its thickness being similar to that of the matrix. Manual pressure was then applied to the donor area using a sterile gauze before the site was closed by means of continuous suturing using a 5.0 polyglactin 910 absorbable suture (Vicryl®, Ethicon, Inc., Somerville, NJ, USA). The graft was immediately placed in the tunnel on the control side and stabilized at each end with a suture. In the same way, the matrix was inserted into the tunnel of the test site using mattress sutures and secured mesially and distally. Lastly, the 2 tunnels were advanced coronally to the CEJ of the teeth so as to cover the PADM and CTG. They were then secured using non-absorbable 5.0 polypropylene suspension sutures (Prolene®, Ethicon, Inc.) (Figure 1). Antibiotics were prescribed to all patients for 7 days (2 × 1,000 mg amoxicillin) along with pain relief (paracetamol, 3 g/day). The postoperative instructions were not to brush for the first 10 days, but instead to rinse twice daily with 0.2% chlorhexidine. A questionnaire on postoperative pain on each graft side was also given to patients. They completed it at the end of the procedure and then daily up to day 14 after surgery, when the sutures were removed and gentle brushing resumed. Follow-up appointments were scheduled for 3, 6, and 12 months after surgery. At each appointment, supragingival plaque was removed.
Figure 1. Clinical views of the control side: (A) Preoperative view. (B) Connective tissue graft under the tunnel. (C) Immediate postoperative view. (D) 12-month postoperative view. Clinical views of the test side: (E) Preoperative view. (F) Xenogeneic acellular dermal matrix. (G) Immediate postoperative view. (H) 12-month postoperative view.
Statistical analysis
Descriptive statistics were summarized as mean±standard deviation or the 95% confidence intervals (CIs). The Wilcoxon signed rank test (non-parametric test for paired samples) was used to compare treatments (test vs. control) at baseline and at 12 months.
Comparisons between treatments were then adjusted, using mixed linear regression models, for patient effects (modeled as random effects). The Dunnett-Hsu adjustment was used to adjust the P values in cases of multiple comparisons.
To test the primary hypothesis that PADM would give equivalent clinical results to CTG in the treatment of Cairo RT1 gingival recessions, non-inferiority for PADM was tested using mixed linear regression models adjusting for the same factors as described before. The average effect and its 2-tailed 90% CI (equivalent to a 1-tailed 95% CI, to test for non-inferiority) were calculated. The reason for this was that is not sufficient to conclude that the difference between the treatments was not statistically significant; instead, it was necessary to calculate a measure of the magnitude of difference (a tolerance range) in the percentage of MRC (or other parameters) that would be allowed for PADM to be considered as good as the comparison treatment. The tolerance range is given by the lower bound of the 90% CI.
Postoperative morbidity
To test the secondary hypothesis, which was that patients would experience less pain on the maxilla side treated with PADM than on the side treated with CTG, a non-parametric paired test (the Wilcoxon signed rank test) was used. In addition, the average pain VAS score reported was plotted vs. time.
RESULTS
In the present study, postoperative healing was uneventful in all patients. No complications, such as allergic reactions, infections, or PADM exfoliation, were noted. All patients enrolled fully completed the study follow-up and none withdrew from the study early. A total of 74 recessions were treated in a randomized, split-mouth fashion in 12 patients using the MCAT technique with CTG (control sides; n=37) or PADM (test sides; n=37). For women (8 out of 12), the mean age was 39.5±10.7 years and the median age was 41.5 years. For men (4 out of 12), the mean age was 44.5±12.2 years and the median age was 48 years. The difference in age between men and women was statistically non-significant (P=0.35, Mann-Whitney U test) (data not shown).
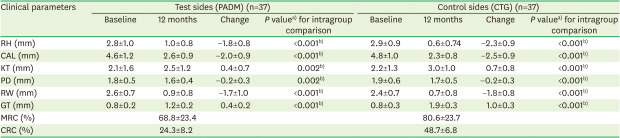
Clinical parameters were evaluated at baseline and at 12 months, and the change in clinical parameters from baseline to 12 months of follow-up are described in Table 1. RH decreased from 2.8±1 mm to 1±0.8 mm on the tunnel + PADM sides (test sides), corresponding to an RH reduction of 1.8 ± 0.8 mm and an MRC of 68.8%±23.4%. On the control sides (tunnel + CTG), RH decreased from 2.9±0.9 mm to 0.6±0.7 mm, reflecting an RH reduction of 2.3±0.9 mm and an MRC of 80.6%±23.7%. A total of 9 (24.3%±8.2%) and 18 (48.7%± 6.8%) recessions exhibited CRC on the test and control sides, respectively. At 12 months, GT had increased by 1±0.3 mm on the control sides and 0.4±0.2 mm on the test sides. At 12 months postoperatively, a statistically significant CAL gain was observed: 2±0.9 mm after applying the PADM and 2.5±0.9 mm after applying GTC.
Table 1. Clinical parameters evaluated and their change between baseline and 12 months of follow-up.
| Clinical parameters | Test sides (PADM) (n=37) | Control sides (CTG) (n=37) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 12 months | Change | P valuea) for intragroup comparison | Baseline | 12 months | Change | P valuea) for intragroup comparison | |
| RH (mm) | 2.8±1.0 | 1.0±0.8 | −1.8±0.8 | <0.001b) | 2.9±0.9 | 0.6±0.74 | −2.3±0.9 | <0.001b) |
| CAL (mm) | 4.6±1.2 | 2.6±0.9 | −2.0±0.9 | <0.001b) | 4.8±1.0 | 2.3±0.8 | −2.5±0.9 | <0.001b) |
| KT (mm) | 2.1±1.6 | 2.5±1.2 | 0.4±0.7 | 0.002b) | 2.2±1.3 | 3.0±1.0 | 0.7±0.8 | <0.001b) |
| PD (mm) | 1.8±0.5 | 1.6±0.4 | −0.2±0.3 | 0.002b) | 1.9±0.6 | 1.7±0.5 | −0.2±0.3 | <0.001b) |
| RW (mm) | 2.6±0.7 | 0.9±0.8 | −1.7±1.0 | <0.001b) | 2.4±0.7 | 0.7±0.8 | −1.8±0.8 | <0.001b) |
| GT (mm) | 0.8±0.2 | 1.2±0.2 | 0.4±0.2 | <0.001b) | 0.8±0.3 | 1.9±0.3 | 1.0±0.3 | <0.001b) |
| MRC (%) | 68.8±23.4 | 80.6±23.7 | ||||||
| CRC (%) | 24.3±8.2 | 48.7±6.8 | ||||||
Values are presented as mean±standard deviation.
PADM: porcine-derived acellular dermal matrix, CTG: connective tissue graft, RH: recession height, CAL: Clinical attachment level, KT: keratinized tissue, PD: probing depth, RW: recession width, GT: gingival thickness, MRC: mean root coverage, CRC: complete root coverage.
a)The Wilcoxon signed rank test was used; b)Statistically significant difference (P<0.05).
Significant increases in KT width and GT were revealed on the control side: 0.7±0.8 mm and 1.0±0.3 mm, respectively. Conversely, this increase was small on the test side, with values of 0.4±0.7 mm and 0.4±0.2 mm, respectively.
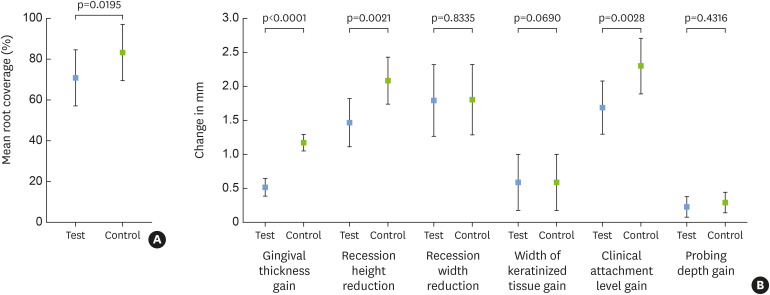
At baseline, no statistically significant difference was found in any clinical parameters between the test and control sides of any patient (except for RW) (Wilcoxon signed rank test, P value) (Table 2). At 12 months follow-up, the difference in RH between the test and control sides was 0.35 mm (indicating that recession was higher in the test group than in the control group by 0.35 mm). This difference was statistically significant (P=0.01). Similarly, statistically significant differences were found between the 2 sides for CAL, RW, and GT, all favoring the control group. KT width was 0.41 mm lower on the test sides than on the control sides (P=0.19). This was also the case for GT. The PD was very similar for both treatments (−0.01 mm lower for the test side; non-significant difference, P=0.87). The associations between the clinical parameters and the treatment (test or control) adjusted for additional covariates (patient's age, patient's sex, side of the maxilla, and tooth type [as fixed effects]) are presented in Figure 2.
Table 2. Paired comparisons of parameters measured for the test (PADM) and control (CTG) sides.
| Follow-up | Clinical parameters | Difference tested | Mean difference±SD | Wilcoxon signed rank test, P value |
|---|---|---|---|---|
| Baseline | RH reduction (mm) | Test-control | −0.14±0.7 | 0.277 |
| CAL (mm) | Test-control | −0.19±0.98 | 0.233 | |
| KT (mm) | Test-control | −0.07±0.79 | 0.472 | |
| PD (mm) | Test-control | −0.05±0.51 | 0.534 | |
| RW (mm) | Test-control | 0.15±0.78 | 0.283 | |
| GT (mm) | Test-control | −0.02±0.16 | 0.228 | |
| 12 months of follow-up | RH (mm) | Test-control | 0.35±0.74 | 0.014a) |
| CAL (mm) | Test-control | 0.39±0.87 | 0.007a) | |
| KT (mm) | Test-control | −0.41±0.94 | 0.190 | |
| PD (mm) | Test-control | −0.01±0.43 | 0.875 | |
| RW (mm) | Test-control | 0.26±0.67 | 0.048a) | |
| GT (mm) | Test-control | −0.68±0.29 | <0.001a) | |
| MRC (%) | Test-control | −12.34±28.2 | 0.005a) |
Values are presented as mean±SD.
PADM: porcine-derived acellular dermal matrix, CTG: connective tissue graft, SD: standard deviation, RH: recession height, CAL: Clinical attachment level, KT: keratinized tissue, PD: probing depth, RW: recession width, GT: gingival thickness, MRC: mean root coverage.
a)Statistically significant difference (P<0.05).
Figure 2. Mean change from baseline to 12 months follow-up, adjusted for additional covariates (patient's age, patient's sex, side of the maxilla, and tooth type). (A) Mean root coverage. (B) Other clinical parameters.
Postoperative morbidity
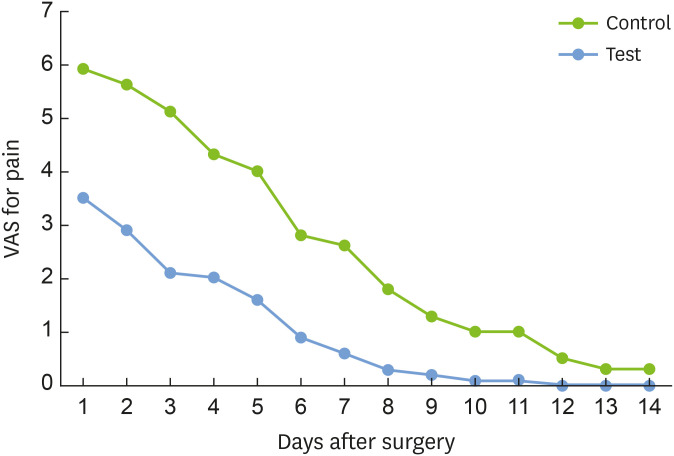
Postoperative VAS values were collected during the first 14 days (Table 3). To test the secondary hypothesis, which was that patients would suffer less pain on the maxilla side treated with PADM than on the side treated with CTG, a non-parametric paired test (the Wilcoxon signed rank test) showed that the test treatment produced less pain than the control treatment. In this case, a mixed linear regression model, with only treatment as a fixed effect and patient effects as random effects, would yield comparable results to those given by the paired test, so this was not calculated.
Table 3. Comparisons of pain VAS scores between the test and control sides during 14 days.
| VAS score | Test (n=12) | Control (n=12) | Mean difference (test-control)±SD | Wilcoxon signed rank test, P value |
|---|---|---|---|---|
| Number of days with pain | 2.3±2.0 | 6.0±2.8 | −3.7±2.0 | <0.001a) |
| Mean pain VAS score | 1.0±0.4 | 2.6±1.0 | −1.6±0.8 | <0.001a) |
| Maximum pain VAS score | 3.5±1.4 | 6.1±1.0 | −2.6±0.4 | <0.001a) |
Values are presented as mean±SD.
SD: standard deviation, VAS: visual analog scale.
a)Statistically significant difference (P<0.05).
In general, significantly less pain was reported on the test side than on the control side. The patients reported on average 3.7 fewer days with pain on the test side than on the control side (P=0.001). Patients also reported a lower mean pain intensity for the test side than for the control side (1.6 VAS points, P<0.001).
The maximum pain felt by patients was higher on the control side than on the test side (on average, 2.6 VAS points less for the test side; P=0.001). The average pain score was plotted vs. time (Figure 3). Then a generalized linear regression model as a function of treatment and time was calculated and indicated that for both treatments, pain decreased in a non-linear way (with an initial rapid decrease followed by a subsequent slower decrease). Pain was higher on the control side than on the test side. Furthermore, the magnitude of decrease in pain depended on the treatment (data not shown).
Figure 3. Course of pain VAS score with time after surgery.
VAS: visual analog scale.
DISCUSSION
This study aimed to compare the treatment efficacy of the MCAT with CTG or PADM at 12 months for treating multiple RT1 maxillary gingival recessions. So far, there are very little data in the literature comparing PADM to CTG. Only 1 prospective split-mouth clinical study with 12 months' follow-up employed the same procedure as the one used in our study, but that study only investigated mandibular recessions [15]. At the PADM test sites and CTG control sites, the authors found mean coverage rates of 53.2% and 83.1%, respectively. Their findings corroborate our MRCs of 68.8% on the test sides vs. 80.6% on the control sides; the difference in the coverage rate on the matrix test sides is attributable to a difference in recession location, since the recessions were maxillary in our study and therefore had a better coverage prognosis [15]. CRC was 20% and 67% on the test and control sides, respectively, in the study by Pietruska et al., [15] and 24.3% and 48.7% in our study. This confirms that the results were similar at the PADM graft sites.
Another study with 6 months' follow-up that compared 2 patient groups treated using the same procedure reported MRCs of 95% (control) vs. 91% (test). Those results are higher than the values observed in our study, particularly with regard to our test group, whose MRC was 68.8%. However, the authors did show that, unlike CTG, PADM displayed limited potential regarding CRC (71.4% for CTG vs. 14.3% for PADM) [14], a finding borne out by our results (80.6% for CTG vs. 24.3% for PADM). The data on KT height gains with PADM are similar in most studies: 0.5 mm (our study), 0.52 mm [15], 0.76 mm [12], 0.8 mm [14], and 0.92 mm [13]. In other words, KT height tends to increase by less than 1 mm.
Our study's clinical results on the test sides were lower than those previously reported by our team in a series of 12 patients [13] with 100 Miller class 1 and 2 maxillary recessions [23] treated using the same procedure (MCAT + PADM). At 12 months in that study, MRC was 84.4%, CRC was 43%, the mean RH reduction was 3.2 mm, and the mean RW reduction was 1.7 mm, while CAL gain was 3.26 mm. According to some authors, bilateral treatments such as those performed in the split-mouth setting in this study may increase the risk of failure compared with unilateral treatment [24]. Moreover, in our study, the CEJ of all teeth was well preserved (type A, class −), which had not been taken into consideration in our previous study since it was conducted before the publication of the Chicago classification. The current inclusion of this parameter is therefore worth noting, since it enables a more accurate measurement of recessions [25,26]. Only 4 previous studies used the same xenogeneic matrix as we used in our study. Hence, there are as yet little clinical data on the PADM, which is still a new material. However, other studies have used collagen matrices and have assessed other substitutes.
A recent clinical study with 12 months' follow-up on treating multiple recessions using allogeneic ADMs revealed that recurrence took place within 6 to 12 months if the initial KT height was <2 mm and the KT width was <1.2 mm. If not, the root coverage rate was stable at 12 months and comparable to CTG with this type of human-derived substitute [27]. These conclusions demonstrate that it is worthwhile to consider clinical studies with a follow-up of at least 12 months, like our study, because recurrence—if it takes place at all—will most likely occur within this period.
Of the substitutes available on the market, CMXs have been particularly well studied. They are mostly associated with coronally advanced flap (CAF) techniques to cover multiple recessions. Very recently, some authors found that although at 12 months CAF + CMX did not show any superior benefits compared with CAF alone in terms of MRC, it did significantly increase GT and may be indicated in patients with thin phenotypes [28]. Another study showed that at 6 months, CAF + CMX reduced operative time and recovery time while improving patient-reported pain during the first days after surgery compared with CAF + CTG, even if it was poorer in terms of MRC [3]. Even though CAF cannot be directly compared against the MCAT, it would appear that the clinical benefits of using CTG outweigh those of using CMX regardless of the surgical protocol followed. Conversely, from the patient's perspective, the use of a substitute results in better tolerance both during surgery, since no palatal graft is harvested, and in the early stages after surgery. The same conclusion has been reached by many researchers [3,15,29,30] and was confirmed again in this study. Indeed, patients reported significantly higher mean pain on the control side, where a palatal graft had been harvested homolaterally to the recipient site, than on the test side (mean VAS, 2.6 vs. 1.0, respectively). This tendency applied to maximum pain too, with maximum VAS scores of 6 during the first 6 days on the control side vs. 3.5 during only the first 2 days on the test side.
Within the limits of this study, the novel PADM in combination with the MCAT technique yielded statistically significant improvements in all clinical parameters studied at 12 months postoperatively in the treatment of multiple Cairo RT1 recessions. Although the matrix yielded poorer clinical results overall compared with the gold standard (CTG), especially with regard to MRC and CRC, it was still clearly superior at reducing mean and maximum patient-reported postoperative pain intensity and pain duration in the first week after surgery.
ACKNOWLEDGEMENTS
The authors thank Ms. Leticia Grize from the Department of Epidemiology and Public Health of the Swiss Tropical and Public Health Institute, Basel, Switzerland, for performing the statistical analysis.
Footnotes
- Conceptualization: Séverine Vincent-Bugnas, Gwenaël Borie.
- Formal analysis: Eve Naman, Mathieu Charbit.
- Investigation: Jonathan Laurent, Eve Naman.
- Methodology: Gwenaël Borie, Jonathan Laurent.
- Project administration: Séverine Vincent-Bugnas.
- Writing - original draft: Séverine Vincent-Bugnas, Mathieu Charbit, Jonathan Laurent, Eve Naman, Gwenaël Borie.
- Writing - review & editing: Séverine Vincent-Bugnas, Gwenaël Borie.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Zucchelli G, Tavelli L, McGuire MK, Rasperini G, Feinberg SE, Wang HL, et al. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J Periodontol. 2020;91:9–16. doi: 10.1002/JPER.19-0350. [DOI] [PubMed] [Google Scholar]
- 2.Chambrone L, Salinas Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018;10:CD007161. doi: 10.1002/14651858.CD007161.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tonetti MS, Cortellini P, Pellegrini G, Nieri M, Bonaccini D, Allegri M, et al. Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: randomized trial assessing non-inferiority in root coverage and superiority in oral health-related quality of life. J Clin Periodontol. 2018;45:78–88. doi: 10.1111/jcpe.12834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aguirre-Zorzano LA, García-De La Fuente AM, Estefanía-Fresco R, Marichalar-Mendía X. Complications of harvesting a connective tissue graft from the palate. A retrospective study and description of a new technique. J Clin Exp Dent. 2017;9:e1439–45. doi: 10.4317/jced.54337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griffin TJ, Cheung WS, Zavras AI, Damoulis PD. Postoperative complications following gingival augmentation procedures. J Periodontol. 2006;77:2070–2079. doi: 10.1902/jop.2006.050296. [DOI] [PubMed] [Google Scholar]
- 6.Cairo F. Periodontal plastic surgery of gingival recessions at single and multiple teeth. Periodontol 2000. 2017;75:296–316. doi: 10.1111/prd.12186. [DOI] [PubMed] [Google Scholar]
- 7.Chambrone L, Ortega MA, Sukekava F, Rotundo R, Kalemaj Z, Buti J, et al. Root coverage procedures for treating single and multiple recession-type defects: an updated Cochrane systematic review. J Periodontol. 2019;90:1399–1422. doi: 10.1002/JPER.19-0079. [DOI] [PubMed] [Google Scholar]
- 8.Cairo F, Barbato L, Tonelli P, Batalocco G, Pagavino G, Nieri M. Xenogeneic collagen matrix versus connective tissue graft for buccal soft tissue augmentation at implant site. A randomized, controlled clinical trial. J Clin Periodontol. 2017;44:769–776. doi: 10.1111/jcpe.12750. [DOI] [PubMed] [Google Scholar]
- 9.Thoma DS, Zeltner M, Hilbe M, Hämmerle CH, Hüsler J, Jung RE. Randomized controlled clinical study evaluating effectiveness and safety of a volume-stable collagen matrix compared to autogenous connective tissue grafts for soft tissue augmentation at implant sites. J Clin Periodontol. 2016;43:874–885. doi: 10.1111/jcpe.12588. [DOI] [PubMed] [Google Scholar]
- 10.Thoma DS, Naenni N, Benic GI, Hämmerle CH, Jung RE. Soft tissue volume augmentation at dental implant sites using a volume stable three-dimensional collagen matrix - histological outcomes of a preclinical study. J Clin Periodontol. 2017;44:185–194. doi: 10.1111/jcpe.12635. [DOI] [PubMed] [Google Scholar]
- 11.Zeltner M, Jung RE, Hämmerle CH, Hüsler J, Thoma DS. Randomized controlled clinical study comparing a volume-stable collagen matrix to autogenous connective tissue grafts for soft tissue augmentation at implant sites: linear volumetric soft tissue changes up to 3 months. J Clin Periodontol. 2017;44:446–453. doi: 10.1111/jcpe.12697. [DOI] [PubMed] [Google Scholar]
- 12.Cosgarea R, Juncar R, Arweiler N, Lascu L, Sculean A. Clinical evaluation of a porcine acellular dermal matrix for the treatment of multiple adjacent class I, II, and III gingival recessions using the modified coronally advanced tunnel technique. Quintessence Int. 2016;47:739–747. doi: 10.3290/j.qi.a36565. [DOI] [PubMed] [Google Scholar]
- 13.Vincent-Bugnas S, Borie G, Charbit Y. Treatment of multiple maxillary adjacent class I and II gingival recessions with modified coronally advanced tunnel and a new xenogeneic acellular dermal matrix. J Esthet Restor Dent. 2018;30:89–95. doi: 10.1111/jerd.12337. [DOI] [PubMed] [Google Scholar]
- 14.Cieślik-Wegemund M, Wierucka-Młynarczyk B, Tanasiewicz M, Gilowski Ł. Tunnel technique with collagen matrix compared with connective tissue graft for treatment of periodontal recession: a randomized clinical trial. J Periodontol. 2016;87:1436–1443. doi: 10.1902/jop.2016.150676. [DOI] [PubMed] [Google Scholar]
- 15.Pietruska M, Skurska A, Podlewski Ł, Milewski R, Pietruski J. Clinical evaluation of Miller class I and II recessions treatment with the use of modified coronally advanced tunnel technique with either collagen matrix or subepithelial connective tissue graft: a randomized clinical study. J Clin Periodontol. 2019;46:86–95. doi: 10.1111/jcpe.13031. [DOI] [PubMed] [Google Scholar]
- 16.Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi GE, Stavropoulos A, et al. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions--a systematic review. Quintessence Int. 2012;43:545–554. [PubMed] [Google Scholar]
- 17.Graziani F, Gennai S, Roldán S, Discepoli N, Buti J, Madianos P, et al. Efficacy of periodontal plastic procedures in the treatment of multiple gingival recessions. J Clin Periodontol. 2014;41(Suppl 15):S63–S76. doi: 10.1111/jcpe.12172. [DOI] [PubMed] [Google Scholar]
- 18.Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol. 2011;38:661–666. doi: 10.1111/j.1600-051X.2011.01732.x. [DOI] [PubMed] [Google Scholar]
- 19.Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S204–S213. doi: 10.1002/JPER.16-0671. [DOI] [PubMed] [Google Scholar]
- 20.Azzi R, Etienne D. Recouvrement radiculaire et reconstruction papillaire par greffon conjonctif enfoui sous un lambeau vestibulaire tunnélisé et tracté coronairement. J Parodontol Implant Orale. 1998;17:71–77. [Google Scholar]
- 21.Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, et al. Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol. 2010;37:88–97. doi: 10.1111/j.1600-051X.2009.01492.x. [DOI] [PubMed] [Google Scholar]
- 22.Hürzeler MB, Weng D. A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent. 1999;19:279–287. [PubMed] [Google Scholar]
- 23.Miller PD. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8–13. [PubMed] [Google Scholar]
- 24.Clauser C, Nieri M, Franceschi D, Pagliaro U, Pini-Prato G. Evidence-based mucogingival therapy. Part 2: ordinary and individual patient data meta-analyses of surgical treatment of recession using complete root coverage as the outcome variable. J Periodontol. 2003;74:741–756. doi: 10.1902/jop.2003.74.5.741. [DOI] [PubMed] [Google Scholar]
- 25.Zuhr O, Bäumer D, Hürzeler M. The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol. 2014;41(Suppl 15):S123–42. doi: 10.1111/jcpe.12185. [DOI] [PubMed] [Google Scholar]
- 26.Zuhr O, Rebele SF, Schneider D, Jung RE, Hürzeler MB. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes. J Clin Periodontol. 2014;41:582–592. doi: 10.1111/jcpe.12178. [DOI] [PubMed] [Google Scholar]
- 27.Tavelli L, Barootchi S, Di Gianfilippo R, Modarressi M, Cairo F, Rasperini G, et al. Acellular dermal matrix and coronally advanced flap or tunnel technique in the treatment of multiple adjacent gingival recessions. A 12-year follow-up from a randomized clinical trial. J Clin Periodontol. 2019;46:937–948. doi: 10.1111/jcpe.13163. [DOI] [PubMed] [Google Scholar]
- 28.Rotundo R, Genzano L, Patel D, D'Aiuto F, Nieri M. Adjunctive benefit of a xenogenic collagen matrix associated with coronally advanced flap for the treatment of multiple gingival recessions: a superiority, assessor-blind, randomized clinical trial. J Clin Periodontol. 2019;46:1013–1023. doi: 10.1111/jcpe.13168. [DOI] [PubMed] [Google Scholar]
- 29.Cieślik-Wegemund M, Candotto V, Wierucka-Młynarczyk B, Tanasiewicz M, Gilowski L, Duda M, et al. Coverage of multiple recessions using the tunnel technique and a collagen matrix in the maxilla or mandible: a 6-month study. J Biol Regul Homeost Agents. 2018;32:1–10. [PubMed] [Google Scholar]
- 30.Tavelli L, McGuire MK, Zucchelli G, Rasperini G, Feinberg SE, Wang HL, et al. Extracellular matrix-based scaffolding technologies for periodontal and peri-implant soft tissue regeneration. J Periodontol. 2020;91:17–25. doi: 10.1002/JPER.19-0351. [DOI] [PubMed] [Google Scholar]