Abstract
Purpose
Previous studies have solely focused on fresh extraction sockets, whereas in clinical settings, alveolar sockets are commonly associated with chronic inflammation. Because the extent of tissue destruction varies depending on the origin and the severity of inflammation, infected alveolar sockets may display various configurations of their remaining soft and hard tissues following tooth extraction. The aim of this study was to classify infected alveolar sockets and to provide the appropriate treatment approaches.
Methods
A proposed classification of extraction sockets with chronic inflammation was developed based upon the morphology of the bone defect and soft tissue at the time of tooth extraction. The prevalence of each type of the suggested classification was determined retrospectively in a cohort of patients who underwent, between 2011 and 2015, immediate bone grafting procedures (ridge preservation/augmentation) after tooth extractions at Seoul National University Dental Hospital.
Results
The extraction sockets were classified into 5 types: type I, type II, type III, type IV (A & B), and type V. In this system, the severity of bone and soft tissue breakdown increases from type I to type V, while the reconstruction potential and treatment predictability decrease according to the same sequence of socket types. The retrospective screening of the included extraction sites revealed that most of the sockets assigned to ridge preservation displayed features of type IV (86.87%).
Conclusions
The present article classified different types of commonly observed infected sockets based on diverse levels of ridge destruction. Type IV sockets, featuring an advanced breakdown of alveolar bone, appear to be more frequent than the other socket types.
Keywords: Alveolar ridge augmentation, Classification, Periodontitis, Socket graft, Tooth socket
Graphical Abstract
INTRODUCTION
After tooth extraction, alveolar sockets undergo major changes, which fall into 2 main categories: quantitative changes, illustrated by the dimensional shrinkage of the ridge; and qualitative alterations, exemplified by erratic healing of the socket.
Ridge dimensional changes following tooth extraction were first reported by Pietrokovski and Massler using cast models [1]. Bone resorption was observed to be more pronounced in the buccal plate than in the palatal/lingual plate in both the maxilla and mandible. This translates into a shift of the central axis of the edentulous ridge toward the palatal/lingual side. In addition, the authors reported that resorption was more severe in the posterior region of the jaw than in the anterior region. Another cast model study by Schropp et al. [2] demonstrated that most of the bone resorption took place during the first 3 months after extraction, resulting in 50% dimensional shrinkage and an average loss of 6.1 mm bucco-lingually. Botticelli reported a horizontal bone loss of 56% buccally and 30% lingually after tooth extraction and immediate implant placement [3]. This was later confirmed by the results by Tan et al., who observed an average bone loss of 3.79 mm horizontally and 1.24 mm vertically within 6 months after extraction in humans [4].
These dimensional alterations might shape the quality of wound repair in the socket. Presuming that the extraction site does not go through intense dimensional changes, the inner-space of the socket should fill with newly formed bone rather than connective tissue. However, connective tissue infiltration of the socket might occasionally take place instead of bone formation, resulting in erratic healing of the extraction site [5].
Both dimensional shrinkage and erratic healing hamper the proper installation of dental implants in post-extraction ridges. On one hand, the insufficient width and height of the ridge entail bone augmentation, a procedure that facilitates achieving a prosthesis-driven position of the fixture, but increases the treatment duration and morbidity. On the other hand, implants installed in sockets with erratic healing often exhibit poor primary stability, therefore requiring a deeper positioning of the fixture to achieve further anchorage from the existing pristine bone. This, in turn, may lead to an unfavorable peri-implant environment, translating into pseudo-pocket formation, esthetic compromise, and difficulty in plaque control [6].
Ridge preservation has been demonstrated to partially prevent dimensional alterations of both soft and hard tissues following tooth extraction [7]. Bone formation is also predictably observed in preserved sockets even if the bone architecture is compromised due to a periodontal/endodontic infection [8,9,10]. Hence, the predictability and the safety of ridge procedures largely relies on proper indications based upon the clinical configuration of the existent tissues following tooth extraction [11].
The objective of the present study is to suggest a classification system of alveolar sockets that takes into account the soft and hard tissue loss subsequent to the extraction of teeth with periodontal and/or endodontic infection. The respective treatment approaches are illustrated by selected clinical cases. In addition, the prevalence of the different classes was retrospectively assessed in a cohort of patients.
MATERIALS AND METHODS
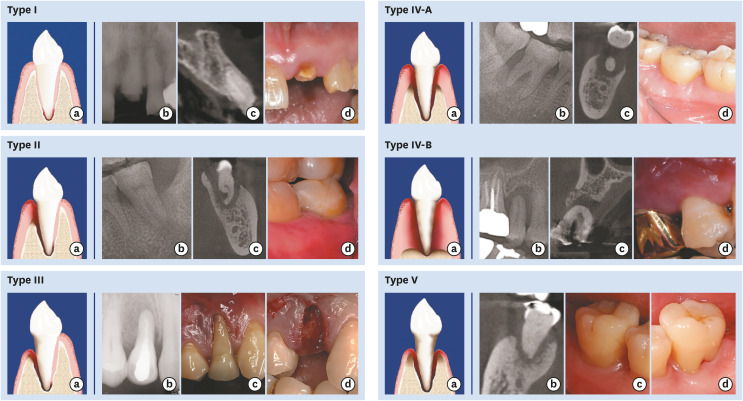
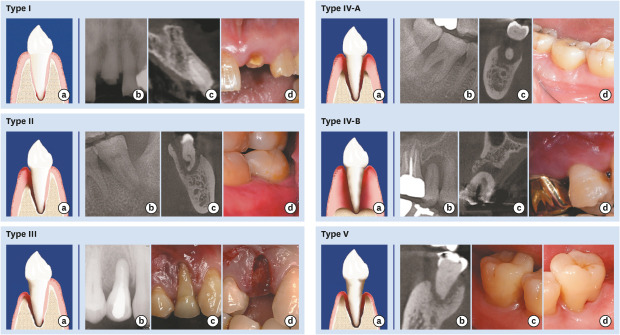
Extraction sockets with chronic pathology are classified into 5 types depending on the morphology of the residual bone and the level of soft tissue breakdown due to infection at the time of extraction. Only single extraction sockets are considered herein, and mesial/proximal bone peaks are assumed to be intact (Figure 1 and Table 1).
Figure 1. Classification of compromised sockets and clinical and radiographic presentation of socket types.
Type I socket. A 4-wall socket without the resorption of the socket wall. Schematic drawing (a), radiographic periapical image (b), computed tomographic image (c) and clinical photo (d) (#21 tooth area).
Type II socket. A 3-wall defect with resorption of either the buccal or palatal (or lingual) wall and no soft tissue recession. Schematic drawing (a), radiographic periapical image (b), computed tomographic image (c), and clinical photo (d) (#37 tooth area).
Type III socket. A 3-wall defect with resorption of either the buccal or palatal (or lingual) wall and soft tissue recession. Schematic drawing (a), radiographic periapical image (b), clinical photo before tooth extraction (c), clinical photo after tooth extraction showing the intact palatal wall and soft tissue (d) (#14 tooth area).
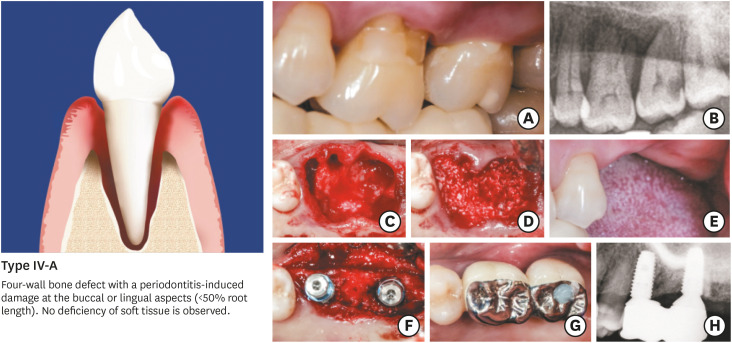
Type IV-A socket. Less than 50% of bone resorption on both buccal and palatal (or lingual) walls and soft tissue in the normal position. Schematic drawing (a), radiographic periapical image (b), computed tomographic image (c), and clinical photo (d) (#47 tooth area).
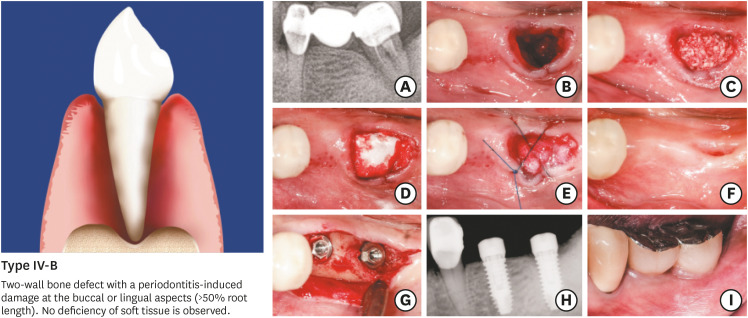
Type IV-B socket. A 2-wall defect with more than 50% buccal and palatal (or lingual) bone loss and soft tissue in the normal position. Schematic drawing (a), radiographic periapical image (b), computed tomographic image (c) and clinical photo (d) (#15 tooth area).
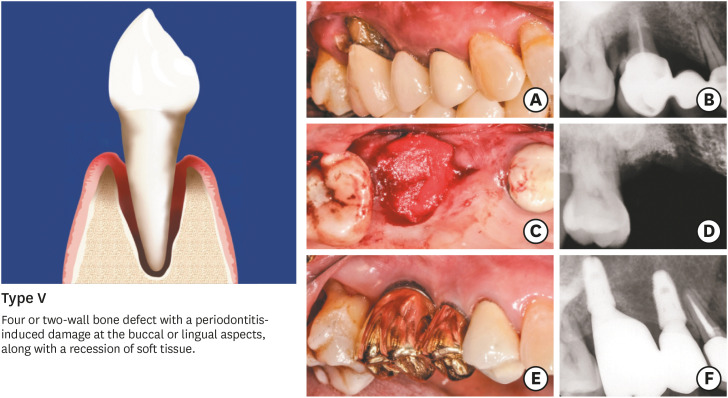
Type V socket. Bone resorption and gingival recession of soft tissue on both buccal and palatal (or lingual) walls. Schematic drawing (a), computed tomographic image (b), clinical photo of the buccal side (c), and clinical photo of the lingual side (d) (#47 tooth area).
Table 1. The proposed classification of infected extraction sockets.
| Type | Residual bone | The level of soft tissue | Defect configuration | Pathology | Healing potential |
|---|---|---|---|---|---|
| Type I | WNL | WNL | 4-wall defect | Endodontic origin, fracture, severe caries | Good |
| Type II | Buccal or palatal/lingual bone loss | WNL | 3-wall defect | Periodontal origin, periodontal-endodontic combined | Good |
| Type III | Buccal or palatal/lingual bone loss | Buccal or palatal/lingual gingival recession | 3-wall defect | Periodontal origin, periodontal-endodontic combined | Poor |
| Type IV-A | Buccal and palatal/lingual bone loss (≤50%) | WNL | 4- or 2-wall defect | Periodontal origin, periodontal-endodontic combined | Poor |
| Type IV-B | Buccal and palatal/lingual bone loss (>50%) | WNL | 2-wall defect | Periodontal origin, periodontal-endodontic combined | Very poor |
| Type V | Buccal and palatal/lingual bone loss | Buccal and palatal/lingual gingival recession | 4- or 2-wall defect | Periodontal origin, periodontal-endodontic combined | Poor |
WNL: within normal limits.
Dental records including patients who received tooth/teeth extraction and immediate ridge preservation were retrospectively assessed to determine the incidence of each socket type.
Suggested classification system
Type I
A type I socket is a 4-wall socket with no resorption of the bony walls. Prior to tooth extraction, the marginal soft tissues are physiologically positioned within the cement-enamel junction and do not exhibit gingival recession. When they exist, pathological processes are limited to the apical region of the tooth at the root apex, and do not trigger a clinically-detectable inflammation of the marginal tissues. Tooth extraction is required due to an extensive loss of tooth substance by caries, and/or crown/root fracture, and/or chronic endodontic infections resistant to conservative treatment. The bone regeneration potential and the treatment predictability are the highest among the different types of compromised sockets (Figure 1 and Table 1).
Type II
A type II socket is a 3-wall defect, where either the buccal plate or the palatal/lingual plate displays bone resorption while no recession of the marginal soft tissue is observed. In the mandible, the resorption of the bony wall is more prevalent from the buccal side than from the palatal/lingual aspect of the socket. In the maxilla, bone destruction limited to the palatal wall can be occasionally observed. Inflammation, mostly observed at the root apex and/or at the margin of socket wall, is triggered by periodontitis or a combined endo-periodontal lesion rather than an endodontic condition alone. The level of bone damage might vary from half to the full length of the buccal or palatal/lingual wall. However, the marginal soft tissues maintain their physiological position, which enhances the possibility of ridge reconstruction (Figure 1 and Table 1).
Type III
In type III sockets, the bone defect configuration and pathology are identical to type II sockets, whereas the soft tissues display recession. The latter feature restrains the possibility for augmentation procedures and reduces the bone regeneration potential and the treatment predictability in comparison to type II (Figure 1, Table 1).
Type IV
The main feature of type IV sockets is bone destruction, which affects both the buccal and palatal/lingual walls, while no recession of the marginal soft tissue is observed. Depending on the resorption level of the buccal and palatal/lingual bony plates, 2 subdivisions of type IV sockets could be described:
Type IV-A: Less than 50% of the buccal and palatal/lingual bony plates are damaged due to periodontitis alone or to combined endo-periodontal lesions. Although the socket morphology involves a 4-wall defect, the cervical part of the buccal and palatal/lingual walls is only composed of soft tissue. The bone damage at the buccal and the palatal/lingual plate hinders the regenerative potential, and the predictability of the treatment aimed at ridge reconstruction is poor (Figure 1 and Table 1).
Type IV-B: This subtype shows the most severe bone breakdown among the different types of infected extraction sockets. Periodontitis or endo-periodontal lesions trigger an inflammatory process that progresses in the marginal bone toward the root apex and radiographically translates into the resorption of a significant height of the buccal and palatal/lingual plates. With bone loss exceeding 50% of the root length at the buccal and palatal/lingual walls and no bone damage proximally, the architecture of type IV-B sockets consists of a 2-wall defect with a very poor bone regenerative potential (Figure 1 and Table 1).
Type V
Type V refers to alveolar sockets where bone resorption is concomitant with gingival recession on both the buccal and palatal/lingual walls. Hard and soft tissue damage, induced by periodontitis or endo-periodontal lesions, exceeds 50% of the plate height from the buccal and palatal/lingual sides. The predictability of regenerative procedures is therefore very poor (Figure 1 and Table 1).
Incidence of socket types
The dental records of patients treated by tooth extraction and ridge preservation between January 2011 and November 2015 at the Department of Periodontics, Seoul National University Dental Hospital (SNUDH), Seoul, South Korea were examined. The experimental population included patients who underwent extraction of periodontally diseased teeth followed by immediate ridge preservation/augmentation. The following exclusion criteria were implemented: i) ridge preservation at intact extraction sockets where teeth were extracted due to caries or fracture; ii) age <20 years; iii) long-term use of anti-inflammatory drugs (e.g., for rheumatoid disease); iv) pregnancy; and v) a history of autoimmune disease. Complete periodontal data including radiographic records (diagnostically acceptable peri-apical and panoramic radiographs with or without cone-beam computed tomography images), clinical photographs, and records saved in the electronic chart system (Electronic Medical Record System ver. A16.0628.1035. DSGR.SYBASE.FOLDER, ELSA) or written down in paper charts were verified. To determine the level of bone and soft tissue breakdown in line with the suggested classification of compromised sockets, the extracted data for each patient were arranged individually using software (MS Excel; Microsoft Corp., Redmond, WA, USA). Each extraction site was classified in accordance with the bone and soft tissue features of socket types as presented in Table 1. Whenever needed, radiographic records were transferred to a digital image software program (Photoshop; Adobe, San Jose, CA, USA) to assess the height of the bone defect as compared to the respective socket wall.
RESULTS
Selected clinical cases
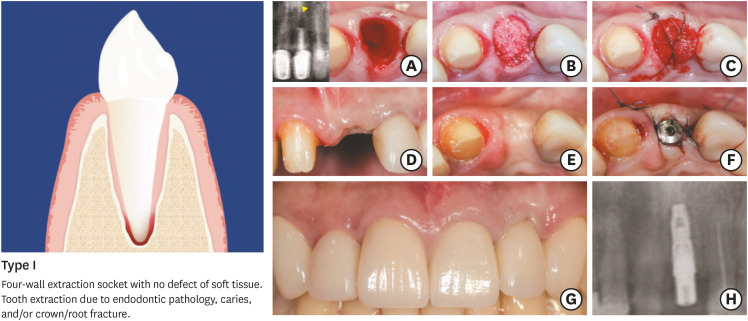
Case 1: Type I extraction socket
The decision was made to perform tooth extraction of a maxillary left central incisor due to apical periodontitis reluctant to endodontic retreatment, as shown in Figure 2. The marginal periodontal tissues did not feature signs of inflammation, and all 4 bony walls of the alveolus were intact. Immediately following extraction of the diseased tooth and a careful debridement of the extraction site, flapless socket grafting was performed using deproteinized bovine bone with 10% collagen covered with a collagen matrix at the socket entrance and secured with a cross-suture. Four months after ridge preservation, the high potential for bone regeneration was facilitated by the socket configuration and minimized dimensional shrinkage. This enabled implant insertion in a prosthetically-optimum position to reach a suitable aesthetic outcome. Overall, this clinical case illustrates the treatment predictability of type I sockets, which is considered to be the highest among all types of compromised sockets.
Figure 2. Type I. (A) Infected extraction socket presenting features of type I: a 4-wall socket without the resorption of socket walls with an endodontic lesion. (B) Application of bone graft after debridement. (C) The socket entrance is sealed with a collagen matrix and secured with sutures. (D) Healing at postoperative week 2. (E) Ridge contour 4 months after ridge preservation. (F) Implant insertion. (G, H) Follow-up at 1 year after prosthesis delivery shows favorable aesthetic results and a stable radiographic level of peri-implant marginal bone.
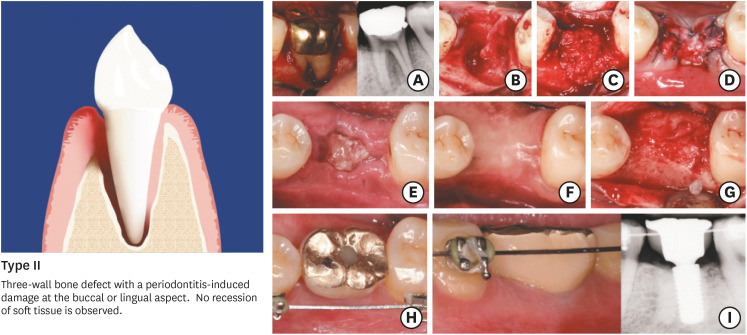
Case 2: Type II extraction socket
Advanced periodontitis affecting the buccal bone wall combined with endodontic involvement justified the extraction of the left mandibular first molar (Figure 3). No recession of soft tissues was observed at baseline. Following flap elevation and tooth avulsion, meticulous debridement clearing all inflammatory tissues in the extraction site was performed under copious saline irrigation. The bone defect was then filled with deproteinized bovine bone with 10% collagen followed by the application of a native collagen membrane on the grafted area and suturing. Although a primary flap closure was not attempted, the extraction site underwent uneventful healing. Soft tissue migration over the exposed area of the barrier device was observed at 2 weeks. A favorable ridge width at re-entry allowed implant installation and subsequent prosthetic restoration. This highlights the favorable bone regeneration potential and the treatment predictability in type II sockets, which, except for type I sockets, remain higher than the other types of compromised sockets.
Figure 3. Type II. (A) Advanced periodontitis resulting into a substantial defect of the buccal bone wall with endodontic involvement. (B) Damaged extraction socket in line with the presentation of type II. (C) Ridge preservation with deproteinized bovine bone minerals and native collagen membrane. (D) Sutures after socket grafting. (E) Healing at 2 weeks following surgery. (F, G) Ridge preservation allowed implant installation. (H, I) Follow-up at 3 years after prosthesis delivery shows favorable aesthetic results and a stable radiographic level of peri-implant marginal bone.
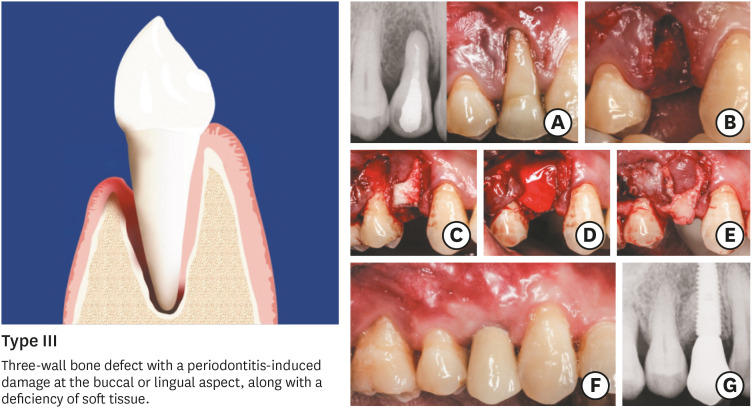
Case 3: Type III extraction socket
Figure 4A and B illustrate the clinical presentation of a Type III compromised socket featuring a periodontitis-induced bone damage at the buccal or palatal/lingual wall, along with a soft tissue deficiency. The reconstruction of the lost tissues was required due to the aesthetic needs. In sequence, following tooth extraction, debridement and flap elevation, ridge preservation/augmentation was conducted through bone grafting using deproteinized bovine bone with 10% collagen covered with a native collagen membrane. A connective tissue graft was then inserted over the barrier device onto the buccal mucosa. This allowed not only to compensate for the soft tissue loss, but also secured the biomaterials underneath. The combination of guided bone regeneration with connective tissue graft minimized post-extraction remodelling an insured proper soft tissue outline for implant-driven prosthetic restoration. In essence, the treatment predictability of Type III socket appears to be lower than Type I and Type II considering the soft tissue deficiency, thus justifying the augmentation of soft tissues in addition to bone grafting.
Figure 4. Type III. (A) Periodontitis-induced bone damage at the buccal wall, along with a recession on tooth #14. (B) A damaged extraction socket shows the presentation of type III marked by a soft tissue deficiency. (C) Socket grafting using deproteinized bovine bone minerals with 10% collagen. (D) Insertion of a native collagen membrane as a barrier device. (E) A connective tissue graft inserted onto the buccal mucosa. (F) Clinical and radiographic outcomes at 1 year after functional loading.
Case 4: Type IV-A extraction socket
Based upon the diagnosis of stage III periodontitis in the maxillary left first and second molars, the choice was made to perform implant-supported restorative treatment (Figure 5). The bone destruction configuration (4-wall socket defect with <50% of the buccal and palatal/lingual wall height) and the absence of soft tissue deficiency were characteristic of type IV-A. Considering the damage shown in the alveolar bone and the condition of the teeth to extract, the ridges were assumed to be at a high risk of shrinkage and required preservation/augmentation procedures. The extraction sockets were grafted using deproteinized bovine bone mineral covered with a native collagen membrane. At postoperative month 4, the dimensional loss in the treated ridge was clear but did not impede implant insertion and the subsequent prosthetic restoration. The observed ridge shrinkage highlights the hindered predictability of preservation/augmentation treatment in type IV-A sockets.
Figure 5. Type IV-A. (A, B) Clinical and radiographic features of type IV-A in tooth #26: buccal and palatal bone resorption (<50% of root length) with no defect of soft tissues, along with recession on tooth #14. (B) Extraction of teeth #26 and #27 followed by a meticulous debridement under copious saline irrigation. (D) Socket grafting using deproteinized bovine bone mineral with 10% collagen prior to coverage with a native collagen membrane. (E) Ridge healing 3 months following surgery. (F–H) Re-entry for implant insertion into a proper bone envelope, followed by prosthetic treatment and radiographic examination at 1 year following functional loading.
Case 5: Type IV-B extraction socket
Advanced destruction of marginal periodontal tissues (stage IV periodontitis) along with endodontic involvement of the mandibular left second molar necessitated tooth extraction. The buccal and lingual bony walls were missing, while no recession of soft tissue was observed, corresponding to the presentation of type IV-B (Figure 6). The need for restorative treatment justified implant installation. However, the architecture and the extent of the bone defect indicated a delayed approach with immediate ridge preservation/augmentation following tooth extraction. Flapless avulsion of the diseased tooth was performed with meticulous debridement under copious irrigation. Deproteinized bovine bone mineral with 10% collagen was installed in the compromised socket. Without raising a flap, a double-layered native collagen membrane was then positioned over the grafted alveolar bone by gently pushing each layer under the marginal gingiva toward the bone edges of the socket. A cross-mattress suture secured the membrane in place. Despite the hindrance of regenerative potential by the bone defect in type IV-B, the ridge width and height allowed proper implant insertion and subsequent restorative treatment.
Figure 6. Type IV-B. (A) Advanced periodontitis on tooth #37 requiring tooth extraction. (B) The extraction socket displayed features of type IV-B (buccal and palatal bone resorption >50% of the root length, no soft tissue defect). (C) Socket grafting using deproteinized bovine bone mineral with 10% collagen. (D, E) Insertion of a native collagen membrane and sutures. (F) Healing at 3 months following surgery. (G, H) Implant installation. (I) Follow-up at 1 year after prosthesis delivery.
Case 6: Type V extraction socket
As presented in Figure 7, the left maxillary first molar displayed gingival recession and substantial bone resorption, hindering its function as a prosthetic abutment. Ridge preservation/augmentation performed immediately following tooth extraction secured enough bone height for implant insertion without sinus elevation. Although limited regeneration potential was assumed considering the extent of tissue deficiency, ridge preservation/augmentation contributed to minimizing the dimensional loss following tooth extraction.
Figure 7. Type V. (A) Tooth #16 requiring extraction, with bone and soft tissue deficiency corresponding to type V. (B) Radiographic image at baseline. (C) Ridge preservation/augmentation using deproteinized bovine bone mineral with 10% collagen covered with a native collagen membrane. (D) Radiographic follow-up at 4 months after extraction. (E) Clinical situation at 1 year after implant loading. (F) Radiographic view 1 year after implant loading, documenting a stable level of peri-implant marginal bone.
Incidence of socket types
Among a total of 10,060 patients who were treated by dental extractions at the Department of Periodontics at SNUDH between 2011 and 2015, the post-extraction sockets in 297 patients were immediately assigned to ridge preservation/augmentation. Within this group of patients, the prevalence of the extraction socket types were calculated, as presented in Table 2. Type IV was the most common type of extraction socket, accounting for 86.87% of the sockets (258/297). The other types were substantially less frequent and presented similar prevalence rates. The prevalence rate of type II sockets was 4.71% (14 of 297), followed by type V (4.04%; 12 of 297), and type III (2.36%; 7 of 297). Type I was the least frequent, with a prevalence of 2.02% (6 of 297). Notably, type I was the only type that was more prevalent in the anterior region than in posterior region, whereas all the other types were more frequently observed in the posterior areas than in the anterior segment of the jaws.
Table 2. The prevalence of each infected extraction socket type.
| Type | Anterior | Posterior | Total |
|---|---|---|---|
| Type I | 5 (8.20) | 1 (0.42) | 6 (2.02) |
| Type II | 7 (11.48) | 7 (2.97) | 14 (4.71) |
| Type III | 3 (4.92) | 4 (1.69) | 7 (2.36) |
| Type IV-A | 20 (32.79) | 105 (44.49) | 125 (42.09) |
| Type IV-B | 24 (39.34) | 109 (46.19) | 133 (44.78) |
| Type V | 2 (3.28) | 10 (4.24) | 12 (4.04) |
| Total | 61 (100.00) | 236 (100.00) | 297 (100.00) |
Values are presented as number (%).
DISCUSSION
Various classifications have previously been suggested for extraction sockets [12,13,14,15,16]. Funato et al. [12] considered 4 classes based on the gingival biotype and the severity of buccal bone destruction. Their classification, however, lacked to incorporate important clinical features that might dictate the treatment decisions, such as the position of soft and hard tissues, and the defect configuration from the buccal side as well as from the palatal/lingual side. Elian et al. [13] proposed a simplified classification system for extraction socket defects based on hard and soft tissue deficiencies: type I referred to a situation where there is no bone or soft tissue loss around the tooth, type II involved buccal bone loss without soft tissue breakdown, and type III was characterized by both soft tissue and bone loss on the buccal wall. More recently, Caplanis et al. [14] suggested another classification where additional parameters such as the biotype were taken into consideration to distinguish 4 types, mainly targeting the esthetic area. Whereas the classification systems proposed by Elian et al. [13] and Caplanis et al. [14] focused on the esthetic area and buccal bone, Smith and Tarnow [15] suggested a different classification specifically for the molars. Depending on the anatomical configuration within the extraction sockets, specifically the septal bone, 3 types were proposed. The dimension of the septal bone within the socket is crucial not only for implant stability, but also for the healing pattern when an immediate implant is placed. Accordingly, in type A, where the septal bone completely surrounds the implant surface, high predictability is expected in immediate placement procedures. However, in types B and C, where the buccal plate of the socket is compromised, site preservation rather than an immediate implant procedure should be considered.
The present classification is distinguished from the others in that the extraction sockets are classified according to the destruction of soft and hard tissue as a result of infection rather than the position of the extraction site in the jaw. Furthermore, the inclusion of palatal (lingual) wall destruction in addition to the buccal defect is distinctive. Classifying different types of sockets should not be based only on the location in the arch; instead, information regarding soft and hard tissue breakdown and the remaining walls of the socket should also be provided since it may be crucial for deciding upon the appropriate treatment protocol. The present article classified different types of infected sockets, which are readily observed in clinical situations based on diverse levels of destruction. By accurately understanding the extent of hard and soft tissue resorption based on the classification system, decision-making following tooth extraction and choosing the appropriate timing of implant placement may be facilitated.
Type I sockets display similar features to those of non-infected extraction sockets. Thus, meticulous debridement following tooth extraction is expected to lead to uneventful healing unless hampered by the size of the periapical lesion and/or the acuteness of the inflammatory manifestations. Dimensional shrinkage inevitably occurs in type I sockets, and immediate implant placement might be considered as a proper treatment option to counteract dimensional atrophy and reduce the number of surgical procedures [17,18,19]. Hence, difficulties in achieving primary stability due to tissue breakdown might hinder the proper installation of immediate implants, thereby favoring ridge preservation, particularly in situations where type I sockets display a thin buccal wall. Cardaropoli et al. [20] reported that, in unassisted sockets, the thickness of buccal bone wall was inversely correlated with alveolar bone loss. In the same line, Spinato et al. [21] demonstrated that spontaneously healing sockets with a buccal plate thinner than 1 mm showed more severe height and width loss than sockets with a buccal bone thickness >1 mm. Conversely, the preservation of sockets with a thin buccal wall partially alleviates ridge shrinkage and promotes successful implant placement [21].
In type II sockets, more dimensional alterations are expected to take place following tooth extraction in comparison than in type I sockets due to the breakdown of the buccal or palatal/lingual bone plate. In the anterior region, this shrinkage might seriously affect the aesthetic outcomes when implants are immediately installed. Simultaneous buccal guided bone regeneration (GBR) with an immediate implant placement is often a viable alternative to reconstruct damaged bone walls and to attenuate postoperative dimensional loss. However, when the buccal or palatal/lingual wall suffers extensive damage, immediate implant placement with simultaneous GBR is less predictable. Such clinical configurations are suitable for early implant placement, in which implant installation is delayed until after 4 to 8 weeks of soft tissue healing, as recommended by the third ITI consensus, particularly in the anterior region [22].
In type III sockets, the soft tissue discrepancy in addition to bone damage requires the concomitant preservation of hard and soft tissues. This might be achieved by ridge preservation in conjunction with a connective tissue graft or a free gingival graft. Karaca et al. [23] demonstrated that ridge preservation with a free gingival graft in the anterior maxilla resulted in less dimensional alterations than in unassisted sockets. Soft tissue grafting is believed to incorporate keratinized tissue following the extraction of teeth with gingival recession. However, this treatment alternative requires delaying the implant installation by at least 16 weeks, as recommended in the third ITI consensus report (Table 2) [22].
Type IV sockets feature bone resorption on both the buccal and palatal/lingual walls; therefore, it is necessary to perform ridge augmentation, which consists of grafting beyond the limits of the existing bony envelope [24]. The soft tissues, without any discrepancies, play a critical role in the reconstruction treatment by supporting the grafting material and the barrier device for GBR. In type V sockets, which have defects of both hard and soft tissues, reaching the desirable alveolar height and width following ridge augmentation procedures is not predictable. After 4 to 6 months of healing, complementary ridge augmentation is often needed. In both type IV and V sockets, it is necessary to delay implant installation by at least 16 weeks [22].
In order to assess the prevalence of each of the socket types considered in the present classification, radiographic data from a cohort of patients who underwent to ridge preservation/augmentation immediately following tooth extraction were examined. Type IV sockets, featuring extensive resorption of the buccal and palatal/lingual bony wall with no recession of the marginal soft tissues, were most frequently observed, in 86.87% of the included extraction sites. In contrast, the proportion of type I sockets, with an intact/slightly affected bone and soft tissue architecture, was only 2.02%. This observation demonstrates that alveolar sockets chosen for ridge preservation, commonly suffer an advanced breakdown, whereas the current evidence on socket preservation procedures only concerns sockets with intact hard and soft tissue architecture. The limited number of clinical studies does not provide enough data to draw robust conclusions on the outcomes of ridge preservation procedures specifically in the setting of compromised extraction sockets [25].
Another finding that arises from the retrospective data in the present study is the higher frequency of preservation procedures in posterior ridges in comparison to anterior sites. One exception to this observation is type I sockets, which were more frequent in the anterior area. It is clear that aesthetic demands motivate the need for site preservation in the anterior segment of the arch. Yet, in the molar sites with a low priority for aesthetics, the need for ridge preservation might be questioned. The decision to graft the socket or to immediately place an implant following tooth extraction is directed by 3 considerations: i) minimizing bone loss, ii) shortening the overall treatment duration, and iii) maximizing the treatment predictability. From this perspective, the aim of Tarnow's classification was to help clinicians properly select whether to perform immediate implant placement in molar sites assuming that this procedure would enable a shorter treatment time [26]. Hence, the specificity of compromised sockets in the molar area poses doubts regarding the validity of the indication for immediate implants. On one hand, posterior ridge shrinkage is more extensive than the dimensional loss observed in the anterior segment of the arch [27]. On the other hand, the risk of proximity to the maxillary sinus or nerve structures is real when an implant is immediately installed in a post-extraction ridge with a limited height. The primary stability of immediate implants is another matter of concern in posterior sockets [28]. Depending on the extent of the periodontal and/or endodontic infection, immediate implant placement could be even more challenging. Therefore, a sequence involving immediate ridge preservation and delayed implant placement appears to be suitable for posterior sockets where infections compromise the natural architecture of alveolar bone and/or soft tissue, corresponding to type II, type III, and type IV in the present classification. This assumption is reinforced by recent data suggesting that, in compromised molar sites of the maxilla, ridge preservation immediately following tooth extraction might reduce the need for an ancillary sinus lift prior to implant installation [29].
The classification of infected sockets in this study did not include any reference to acute infections of the periodontium. Clinical reality suggests that acute infections need to be managed through antibiotic medication and temporization prior to any treatment modality, either implant placement or ridge preservation. Consequently, only sockets where infections fulfill the characteristics of chronic lesions were considered in this classification.
The present classification only encompasses single tooth extraction sockets. Therefore, it was hypothesized that mesial or distal proximal walls do not exhibit a significant breakdown. In the situation of adjacent multiple extraction sockets, however, proximal wall destruction is a common feature and site preservation/reconstruction procedures become more challenging. Apart from the preclinical data by Al-Askar et al. [30], who reported that contiguous teeth extraction led to more intense bone destruction than single tooth extraction, evidence on the healing fate of adjacent multiple tooth extraction sockets is weak. As highlighted by a recent consensus report [26], further studies on adjacent multiple extraction sockets are required to draw conclusions regarding the appropriate treatment strategies specific to this distinctive clinical presentation.
In conclusion, type IV sockets were the most frequent type identified in a retrospective cohort. The evaluation of the extent of hard and soft tissue resorption using the present classification might facilitate the selection of a suitable treatment option with regard to the regenerative potential of the extraction site.
Footnotes
- Conceptualization: Jung-Ju Kim, Heithem Ben Amara, Ki-Tae Koo.
- Formal analysis: Jung-Ju Kim, Heithem Ben Amara, Inna Chung.
- Investigation: Jung-Ju Kim, Heithem Ben Amara.
- Methodology: Jung-Ju Kim, Heithem Ben Amara, Ki-Tae Koo.
- Project administration: Inna Chung, Ki-Tae Koo.
- Writing - original draft: Jung-Ju Kim, Heithem Ben Amara.
- Writing - review & editing: Heithem Ben Amara, Jung-Ju Kim, Ki-Tae Koo.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967;17:21–27. doi: 10.1016/0022-3913(67)90046-7. [DOI] [PubMed] [Google Scholar]
- 2.Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313–323. [PubMed] [Google Scholar]
- 3.Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31:820–828. doi: 10.1111/j.1600-051X.2004.00565.x. [DOI] [PubMed] [Google Scholar]
- 4.Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(Suppl 5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 5.Kim JH, Susin C, Min JH, Suh HY, Sang EJ, Ku Y, et al. Extraction sockets: erratic healing impeding factors. J Clin Periodontol. 2014;41:80–85. doi: 10.1111/jcpe.12173. [DOI] [PubMed] [Google Scholar]
- 6.Yi Y, Koo KT, Schwarz F, Ben Amara H, Heo SJ. Association of prosthetic features and peri-implantitis: a cross-sectional study. J Clin Periodontol. 2020;47:392–403. doi: 10.1111/jcpe.13251. [DOI] [PubMed] [Google Scholar]
- 7.Cardaropoli G, Araújo M, Hayacibara R, Sukekava F, Lindhe J. Healing of extraction sockets and surgically produced - augmented and non-augmented - defects in the alveolar ridge. An experimental study in the dog. J Clin Periodontol. 2005;32:435–440. doi: 10.1111/j.1600-051X.2005.00692.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim JH, Koo KT, Capetillo J, Kim JJ, Yoo JM, Ben Amara H, et al. Periodontal and endodontic pathology delays extraction socket healing in a canine model. J Periodontal Implant Sci. 2017;47:143–153. doi: 10.5051/jpis.2017.47.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao L, Xu T, Hu W, Chung KH. Preservation and augmentation of molar extraction sites affected by severe bone defect due to advanced periodontitis: a prospective clinical trial. Clin Implant Dent Relat Res. 2018;20:333–344. doi: 10.1111/cid.12585. [DOI] [PubMed] [Google Scholar]
- 10.Koo TH, Song YW, Cha JK, Jung UW, Kim CS, Lee JS. Histologic analysis following grafting of damaged extraction sockets using deproteinized bovine or porcine bone mineral: a randomized clinical trial. Clin Oral Implants Res. 2020;31:93–102. doi: 10.1111/clr.13557. [DOI] [PubMed] [Google Scholar]
- 11.Kim JJ, Ben Amara H, Schwarz F, Kim HY, Lee JW, Wikesjö UM, et al. Is ridge preservation/augmentation at periodontally compromised extraction sockets safe? A retrospective study. J Clin Periodontol. 2017;44:1051–1058. doi: 10.1111/jcpe.12764. [DOI] [PubMed] [Google Scholar]
- 12.Funato A, Salama MA, Ishikawa T, Garber DA, Salama H. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27:313–323. [PubMed] [Google Scholar]
- 13.Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19:99–104. [PubMed] [Google Scholar]
- 14.Caplanis N, Lozada JL, Kan JY. Extraction defect assessment, classification, and management. J Calif Dent Assoc. 2005;33:853–863. [PubMed] [Google Scholar]
- 15.Smith RB, Tarnow DP. Classification of molar extraction sites for immediate dental implant placement: technical note. Int J Oral Maxillofac Implants. 2013;28:911–916. doi: 10.11607/jomi.2627. [DOI] [PubMed] [Google Scholar]
- 16.Al-Shabeeb MS, Al-Askar M, Al-Rasheed A, Babay N, Javed F, Wang HL, et al. Alveolar bone remodeling around immediate implants placed in accordance with the extraction socket classification: a three-dimensional microcomputed tomography analysis. J Periodontol. 2012;83:981–987. doi: 10.1902/jop.2011.110569. [DOI] [PubMed] [Google Scholar]
- 17.Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9:332–343. [PubMed] [Google Scholar]
- 18.Vignoletti F, de Sanctis M, Berglundh T, Abrahamsson I, Sanz M. Early healing of implants placed into fresh extraction sockets: an experimental study in the beagle dog. II: ridge alterations. J Clin Periodontol. 2009;36:688–697. doi: 10.1111/j.1600-051X.2009.01439.x. [DOI] [PubMed] [Google Scholar]
- 19.Covani U, Ricci M, Bozzolo G, Mangano F, Zini A, Barone A. Analysis of the pattern of the alveolar ridge remodelling following single tooth extraction. Clin Oral Implants Res. 2011;22:820–825. doi: 10.1111/j.1600-0501.2010.02060.x. [DOI] [PubMed] [Google Scholar]
- 20.Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Relationship between the buccal bone plate thickness and the healing of postextraction sockets with/without ridge preservation. Int J Periodontics Restorative Dent. 2014;34:211–217. doi: 10.11607/prd.1885. [DOI] [PubMed] [Google Scholar]
- 21.Spinato S, Galindo-Moreno P, Zaffe D, Bernardello F, Soardi CM. Is socket healing conditioned by buccal plate thickness? A clinical and histologic study 4 months after mineralized human bone allografting. Clin Oral Implants Res. 2014;25:e120–6. doi: 10.1111/clr.12073. [DOI] [PubMed] [Google Scholar]
- 22.Hämmerle CH, Chen ST, Wilson TG., Jr Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19(Suppl):26–28. [PubMed] [Google Scholar]
- 23.Karaca Ç, Er N, Gülşahı A, Köseoğlu OT. Alveolar ridge preservation with a free gingival graft in the anterior maxilla: volumetric evaluation in a randomized clinical trial. Int J Oral Maxillofac Surg. 2015;44:774–780. doi: 10.1016/j.ijom.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Hämmerle CH, Araújo MG, Simion M Osteology Consensus Group 2011. Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res. 2012;23(Suppl 5):80–82. doi: 10.1111/j.1600-0501.2011.02370.x. [DOI] [PubMed] [Google Scholar]
- 25.Sculean A, Stavropoulos A, Bosshardt DD. Self-regenerative capacity of intra-oral bone defects. J Clin Periodontol. 2019;46(Suppl 21):70–81. doi: 10.1111/jcpe.13075. [DOI] [PubMed] [Google Scholar]
- 26.Tonetti MS, Jung RE, Avila-Ortiz G, Blanco J, Cosyn J, Fickl S, et al. Management of the extraction socket and timing of implant placement: Consensus report and clinical recommendations of group 3 of the XV European Workshop in Periodontology. J Clin Periodontol. 2019;46(Suppl 21):183–194. doi: 10.1111/jcpe.13131. [DOI] [PubMed] [Google Scholar]
- 27.Jung RE, Philipp A, Annen BM, Signorelli L, Thoma DS, Hämmerle CH, et al. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol. 2013;40:90–98. doi: 10.1111/jcpe.12027. [DOI] [PubMed] [Google Scholar]
- 28.Chrcanovic BR, Martins MD, Wennerberg A. Immediate placement of implants into infected sites: a systematic review. Clin Implant Dent Relat Res. 2015;17(Suppl 1):e1–e16. doi: 10.1111/cid.12098. [DOI] [PubMed] [Google Scholar]
- 29.Cha JK, Song YW, Park SH, Jung RE, Jung UW, Thoma DS. Alveolar ridge preservation in the posterior maxilla reduces vertical dimensional change: a randomized controlled clinical trial. Clin Oral Implants Res. 2019;30:515–523. doi: 10.1111/clr.13436. [DOI] [PubMed] [Google Scholar]
- 30.Al-Askar M, O'Neill R, Stark PC, Griffin T, Javed F, Al-Hezaimi K. Effect of single and contiguous teeth extractions on alveolar bone remodeling: a study in dogs. Clin Implant Dent Relat Res. 2013;15:569–575. doi: 10.1111/j.1708-8208.2011.00403.x. [DOI] [PubMed] [Google Scholar]