Abstract
Breast cancer is the most common malignancy in Korean women, and its incidence continues to increase. The Korean Breast Cancer Society (KBCS) established a nationwide breast cancer database through its online enrollment program in 1996. This study aimed to analyze the clinical characteristics of breast cancer in Korea, and to assess the pattern of changes in breast cancer management in 2018. We analyzed the KBCS and Korea Central Cancer Registry (KCCR) databases in 2018. In 2018, 28,157 patients were newly diagnosed with breast cancer, of whom 4,510 had noninvasive breast cancer and 23,647 had invasive breast cancer. The age-standardized rate of breast cancer in 2018 was 79.0 per 100,000 women (65.6 invasive, 13.4 noninvasive). The median age of female patients diagnosed with breast cancer in 2018 was 52 years, and the incidence of breast cancer was the highest in the 40–49-years age group (9,432 patients, 33.6%). The proportion of patients with stage 0 and stage I breast cancer continued to increase, accounting for 63.8% of cases, and breast-conserving surgery was performed more often than mastectomy (66.2% vs. 33.0%). The most common subtypes of breast cancer were hormone receptor [HR]-positive and human epidermal growth factor receptor-2 (HER2)-negative types (65.9% of cases), while the HR-negative and HER2-positive types accounted for 9.2% of cases. According to the KCCR data, from 2014 to 2018, the 5-year relative survival rate of patients with breast cancer was 93.3%, which was 14.0% higher than that from 1993 to 1995 (79.3%). The clinical characteristics of breast cancer in Korea have been changing, and national databases can improve our understanding of the disease characteristics of Korean women. Therefore, updating the KBCS registry is important for the effective management of breast cancer in Korea.
Keywords: Breast neoplasms, Epidemiology, Korea, Registries, Statistics
INTRODUCTION
Breast cancer was the second most common cancer globally in 2018, but it became the most common malignancy in 2020, according to the International Agency for Research on Cancer (IARC). In 2020, 2,206,771 patients were diagnosed with breast cancer (11.4% of all cancer cases), and the age-standardized incidence rate (ASR) of breast cancer was also the highest at 47.8 [1]. Additionally, breast cancer is the fifth most common cause of death among all cancer types, including lung, colon, liver, and stomach cancer, accounting for 6.9% (6,84,996) of all cancer deaths [1]. According to the 2018 Korea Central Cancer Registry (KCCR) data, breast cancer is the fifth most common cancer in both sexes, with a total of 23,647 cases (9.7%), and is the most common cancer among women (20.5% of all cancer cases in women) [2].
The incidence of cancer and its survival rates markedly vary depending on the nationality, ethnicity, and socioeconomic characteristics of patients, and these factors are particularly important in the treatment of breast cancer. Therefore, statistical research on breast cancer in relation to countries or ethnicities is necessary for a better understanding of the disease biology and for establishing effective public health policies. The Korean Breast Cancer Society (KBCS) has been collecting and analyzing information regarding breast cancer in Korea since 1996, including patients' sex, age, surgical methods, cancer stage, and molecular subtype. This study aimed to describe the characteristics of breast cancer in Korea in 2018, including its incidence, clinicopathological features, stage, and treatment strategies, and compare them with breast cancer trends observed in the past 18 years.
METHODS
Data sources
All patients with newly diagnosed breast cancer in Korea in 2018 were enrolled in this study. The following 3 types of data sources were used: 1) KCCR, 2) KBCS, and 3) global cancer incidence, mortality, and prevalence (GLOBOCAN) databases. The study was approved by the Institutional Review Board of Jeonbuk National University Hospital (approval No. 2021-03-053).
The Korean Ministry of Health and Welfare established a hospital-based nationwide cancer registry called the KCCR. KCCR is a database containing information on cancer incidence, mortality, survival rate, age, and region. The database includes nearly all patients diagnosed with breast cancer in Korea, including both invasive and noninvasive cancer types (International Classification of Disease [ICD], 10th version codes: C50 and D05) [3]. In this study, the incidence of breast cancer, patient's age, and survival rates were analyzed using the KCCR data.
Data regarding treatment, cancer stage, and molecular subtype were evaluated according to the KBCS online breast cancer registry system (https://registry.kbcs.or.kr/ecrf). The KBCS database includes detailed information on patients with breast cancer, including age, body mass index (BMI), occupation, economic status, treatment options, pathological type, stage, and molecular subtype.
Global breast cancer information, including mortality rates, were obtained from the GLOBOCAN database, which was updated in 2020 and can be accessed through the Global Cancer Observatory (http://gco.iarc.fr) [1].
Statistical analyses
In this study, breast cancer refers to both invasive (ICD-10 code: C50) and noninvasive cancers (ICD-10 code: D05) found in women. Those with lobular carcinoma in situ were excluded from the study.
The incidence rate is expressed as the number per 100,000 people using the crude rate (CR) and ASR. CR was defined as the total number of newly diagnosed patients in a year divided by the mid-year population. ASR, which is widely used when referring to the incidence of a disease, is a weighted average of the age-specific rates, where the weights correspond to the proportions of the corresponding age groups of a standard population [4]. In this study, the ASR was standardized using Segi's world standard population [5].
The ASR trend is summarized as the annual percentage change (APC). To monitor the trend over a pre-specified fixed interval and to describe the average APC over a period of multiple years, the average annual percent change (AAPC) was calculated [6]. Furthermore, the Joinpoint model 4.3.1 (National Cancer Institute, Bethesda, USA) was used to analyze the APC and AAPC.
The relative survival rate (RSR) represents the ratio of two groups: the survival of the population of patients with cancer (which is the observed rate) divided by the expected survival of the general population [7]. The expected survival rate is the probability of a population surviving from one year to another, according to age, race, and sex. The relative rate aims to estimate the effect of cancer alone on survival. Statistical significance was set at p < 0.05. The SPSS software (version 20.0; IBM Corp., Armonk, USA) was used to perform all statistical analyses.
RESULTS
Incidence
A total of 28,157 patients were diagnosed with breast cancer in Korea in 2018. Of all cancer cases, invasive breast cancer accounted for 23,647 (84.0%) cases, while noninvasive breast cancer accounted for 4,510 (16%) cases. Of the total study patients, 28,049 (99.6%) were women and 108 (0.4%) were men. Among male patients, 100 (92.6%) and 8 (7.4%) were diagnosed with invasive and noninvasive breast cancers, respectively.
In 2018, the ASR of invasive breast cancer was 65.6 per 100,000 women, whereas that of noninvasive breast cancer was 13.4, 79.0, for all types of breast cancers. The CR of invasive breast cancer was 91.6 per 100,000 women, whereas that of noninvasive breast cancer was 17.5, 109.1, for all types of breast cancers.
In Korea, breast cancer was the most common malignancy in women in 2018, in terms of number and ASR [2]. Breast cancer is the most common cancer in the 35–64-year age group [2]. However, breast cancer is the fourth most common cancer in patients aged ≥ 64 years; meanwhile, it rarely occurs in patients aged < 35 years [2].
Age distribution
The pattern of age distribution is similar to that of previous patterns [8]. The highest frequency of breast cancer was observed in the 40–49-year age group, based on both the KCCR and KBCS datasets. According to the KCCR data, 9,432 (33.6%) patients with breast cancer belonged to the 40–49-year age group. The second most affected age group was the 50–59 years group (8,335, 29.7%) (Table 1). According to the KBCS registry data, the age distribution of patients diagnosed with breast cancer ranged from 18 to 100 years. A similar age distribution pattern was observed in the KCCR dataset.
Table 1. Age-wise distribution of female patients with newly diagnosed breast cancer in 2018 in Korea.
| Age (yr) | KBCS registry data | KCCR data |
|---|---|---|
| < 20 | 6 (< 0.1) | 4 (< 0.1) |
| 20–29 | 101 (0.8) | 205 (0.7) |
| 30–39 | 1.224 (9.8) | 2.425 (8.6) |
| 40–49 | 4.334 (35.2) | 9.432 (33.6) |
| 50–59 | 3.712 (30.2) | 8.335 (29.7) |
| 60–69 | 2.032 (16.5) | 4.845 (17.3) |
| 70–79 | 747 (6.1) | 2.115 (7.5) |
| ≥ 80 | 150 (1.3) | 688 (2.5) |
| Total | 12,306 (100.0) | 28,049 (100.0) |
Values are presented as number (%).
KBCS = Korean Breast Cancer Society; KCCR = Korea Central Cancer Registry.
Surgical treatment and pathological stages
Of the 12,306 patients with breast cancer who were enrolled in the KBCS registry in 2018, 8,143 (66.2%) underwent breast-conserving surgery (BCS), and 4,063 (33.0%) underwent mastectomy. According to the classification established by the American Joint Committee on Cancer and the International Union Against Cancer, 7th edition [9], stage I cancer was the most common (5,312 cases, 43.2%), followed by stage II (3,555 cases, 27.3%), and stage 0 (1,810 cases, 14.7%) (Table 2). Over 198 and 485 patients with stage 0 and stage I breast cancer underwent surgery following neoadjuvant chemotherapy (NACT), respectively.
Table 2. Stage distribution of patients with newly diagnosed breast cancer in 2018 in Korea (KBCS registry data).
| Stage | No. of patients |
|---|---|
| 0 | 1.810 (14.7) |
| I | 5.312 (43.2) |
| II | 3.355 (27.3) |
| III | 821 (6.7) |
| IV | 118 (1.0) |
| Unknown | 890 (7.1) |
| Total | 12.306 (100.0) |
Values are presented as number (%).
KBCS = Korean Breast Cancer Society.
MOLECULAR SUBTYPE PATTERNS
Among the 12,306 patients enrolled in the KBCS registry, 9,096 had estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER2) status. A tumor was defined as hormone receptor (HR) positive if at least one of the hormonal receptors (i.e., ER or PR) was present, and HER2-positivity was reported for tumors that exhibited 3+ or 2+ expression scores on immunohistochemical analysis with amplification on fluorescence in situ hybridization [FISH] or silver-enhanced in situ hybridization (SISH). A total of 608 patients with HER2 status, defined as 2+ without the use of FISH or SISH tests, were excluded from the analysis. A total of 6,226 (68.4%) patients had HR-positive and HER2-negative status, 1,035 (11.4%) had HR-positive and HER2-positive status, 838 (9.2%) had HR-negative and HER2-positive status, and 997 (11.0%) had HR-negative and HER2-negative status (Table 3).
Table 3. Molecular subtypes of newly diagnosed breast cancers in 2018 in Korea (KBCS registry data).
| Molecular subtype | No. of patients |
|---|---|
| HR (+), HER2 (−) | 6.226 (68.4) |
| HR (+), HER2 (+) | 1.035 (11.4) |
| HR (−), HER2 (−) | 838 (9.2) |
| HR (−), HER2 (−) | 997 (11.0) |
| Total | 9.096 (100.0) |
Values are presented as number (%).
KBCS = Korean Breast Cancer Society; HR = hormone receptor; HER2 = human epidermal growth factor receptor-2.
When the distribution of molecular subtypes was analyzed in relation to the stage, different patterns were observed for each stage. The proportions of HR-positive and HER2-negative patients were the highest (70.4%) in the stage I group and lowest (62.0%) in the stage IV group. The proportions of HR-negative and HER2-negative patients were the highest (13.6%) in the stage II group and lowest (5.9%) in the stage 0 group (p < 0.001) (Supplementary Figure 1).
BREAST CANCER TRENDS IN KOREA
Incidence
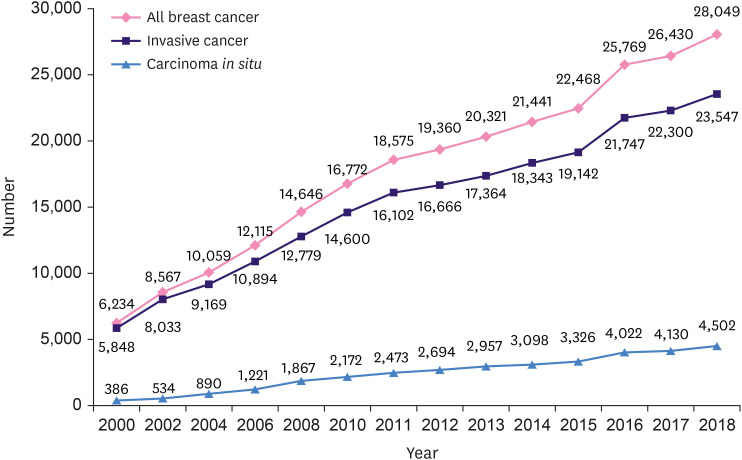
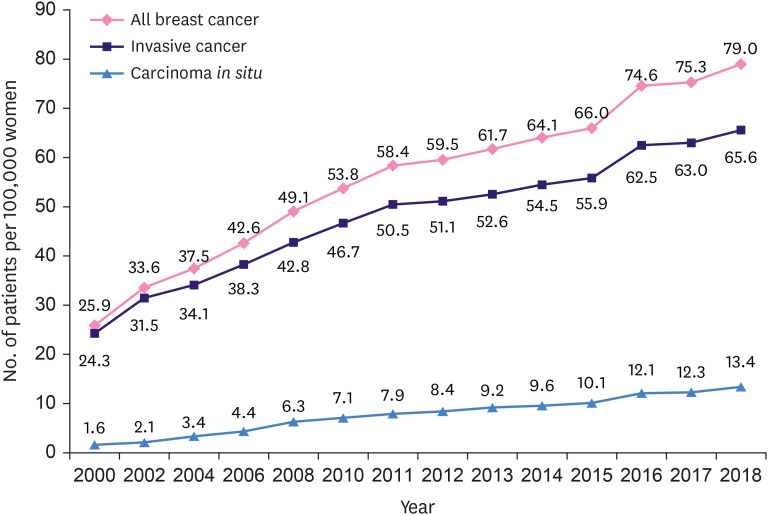
Both the number of newly diagnosed patients and the ASR of breast cancer in Korea are increasing every year. In 2018, 28,049 female patients with newly diagnosed breast cancer were reported, with an increase of 6.1% from 2017 (Figure 1). The number increased by a staggering 350% compared with the 6,234 diagnoses in 2000. The total breast cancer ASR in 2000 was 25.9 (24.3 for invasive breast cancer and 1.6 for noninvasive breast cancer), while it was 79.0, 65.6, and 13.4 for total, invasive, and noninvasive breast cancers, respectively, in 2018. The ASR for invasive and noninvasive breast cancer increased by 2.7 and 8.4 times, respectively (Figure 2).
Figure 1. Number of female patients with newly diagnosed breast cancer in Korea.
Figure 2. Trends in age-standardized incidence rates of breast cancer among female patients from 2000 to 2018 in Korea.
Between 1999 and 2018, the AAPC of breast cancer was 5.7, whereas that of noninvasive breast cancer was 10.7, which was higher than that of invasive breast cancer (Table 4). The AAPCs by age were highest among patients aged ≥ 60 years (7.4%), 5.6% among those aged 45–60 years, and 4.9% among those aged < 45 years.
Table 4. Trends in age-standardized incidence rates of breast cancer in women according to the Joinpoint analysis (1999–2018).
| Factor | AAPC (1999–2018) | Trend 1 | Trend 2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | APC | 95% CI | APC | Period | APC | 95% CI | |||
| Analysis by pathology | |||||||||
| All | 5.7* | 1999–2007 | 7.4* | 6.2–8.6 | 8.6 | 2007–2018 | 4.9* | 4.4–5.4 | |
| Invasive | 5.0* | 1999–2007 | 6.3* | 5.2–7.5 | 7.5 | 2007–2018 | 4.3* | 3.8–4.9 | |
| In situ | 10.7* | 1999–2008 | 18.0* | 15.8–20.2 | 20.2 | 2008–2018 | 7.9* | 7.1–8.7 | |
| Analysis by age (yr) | |||||||||
| < 45 | 4.9* | 1999–2004 | 7.0* | 4.7–9.4 | 9.4 | 2004–2018 | 4.6* | 4.2–5.0 | |
| 45–60 | 5.6* | 1999–2008 | 7.5* | 6.3–8.7 | 8.7 | 2008–2018 | 4.7* | 4.1–5.3 | |
| > 60 | 7.4* | 1999–2008 | 9.6* | 8.1–11.2 | 11.2 | 2008–2018 | 6.3* | 5.5–7.0 | |
AAPC = average annual percentage change (%); APC = annual percent change (%); CI = confidence interval.
*The APC or AAPC is significantly different from 0 (p < 0.05).
Age distribution
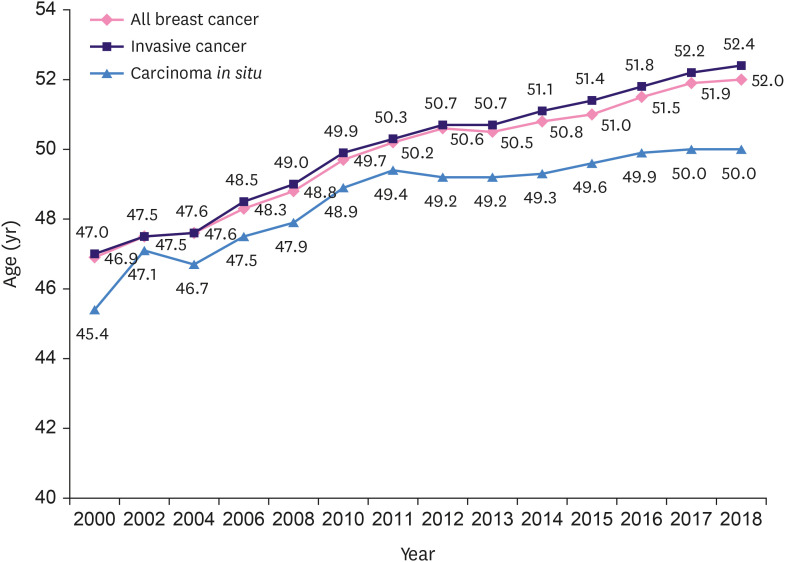
Based on the KCCR data, the median age of women diagnosed with breast cancer in 2018 was 52.0 years. The median age at diagnosis of invasive breast cancer was 52.4 years, whereas that of non-invasive breast cancer was 50.0 years. In 2000, the median age at diagnosis of breast cancer was 46.9 years; it has been increasing steadily ever since, exceeding 50 years for the first time in 2011 (50.2 years) and reaching 52.0 years in 2018 (Figure 3). As shown in Table 4, the median age at diagnosis of breast cancer in Korea is expected to increase continuously as the rate of breast cancer incidence increases rapidly at age ≥ 60 years.
Figure 3. Trends in the median age of women at diagnosis of breast cancer in Korea.
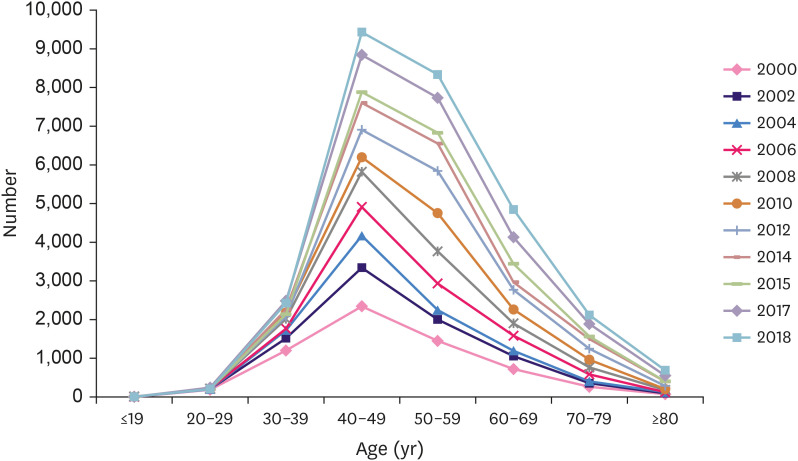
In contrast to the increasing median age, the age distribution pattern was similar to that reported in previous studies. After 2000, the highest incidence was reported in the 40–49-year age group (Figure 4). The graph has remained an inverted V shape since 2000, and the area of the graph is widening.
Figure 4. Trends in the age distribution pattern of female patients with breast cancer diagnosed in 2000–2018 in Korea.
Biological markers and stage distribution
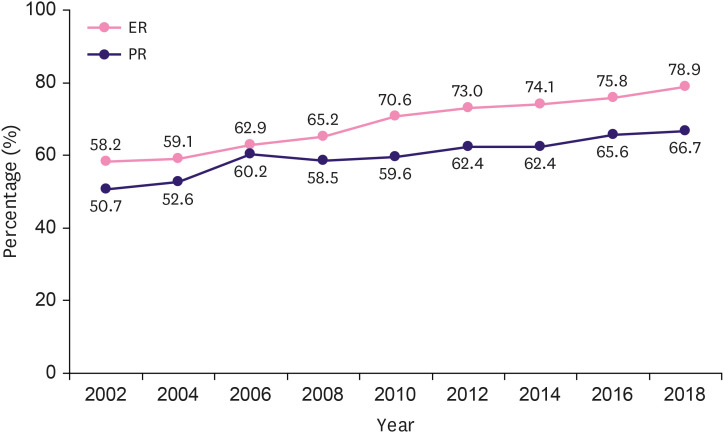
According to the KBCS data from 2002 to 2018, the incidence of HR-positive breast cancer has been increasing. It has increased by more than 1% every year since 2002. This phenomenon occurred in both ER-positive and PR-positive breast cancers; however, the rate of increase in ER-positive breast cancer was higher than that in PR-positive breast cancer. In 2002, 58.2% of patients had ER-positive tumors; in 2018, 78.9% of patients had ER-positive tumors, an increase of approximately 35.6% (p < 0.001). The proportion of patients with PR-positive breast cancer increased by 31.6% from 50.7% to 66.7% during the same period (p < 0.001) (Figure 5).
Figure 5. Changes in the incidence of hormone receptor-positive breast cancer.
ER = estrogen receptor; PR = progesterone receptor.
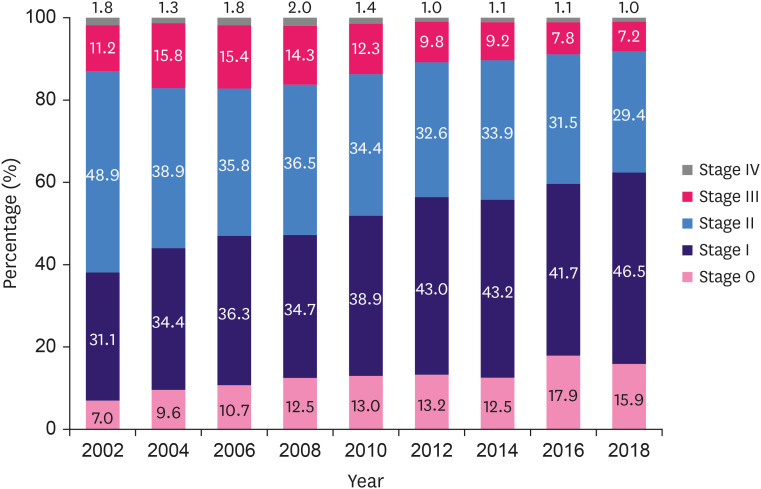
The proportion of patients with stage 0 and stage I breast cancer also continued to increase, from 38.1% in 2002 to 62.4% in 2018, which is an increase of approximately 63.8% (p < 0.001). In particular, the proportion of patients with stage 0 cancer showed the highest increase of 127.1%, from 7.0% in 2002 to 15.9% in 2018 (p < 0.001). The proportion of patients with stage I cancer also increased from 31.1% in 2002 to 46.5% in 2018 (49.5% increase, p < 0.001). By contrast, the proportion of patients with stage II and III breast cancer decreased by 39.9% over the same period, showing a significant difference (p < 0.001) (Figure 6).
Figure 6. Changes in the stage distribution of breast cancer.
Surgical patterns
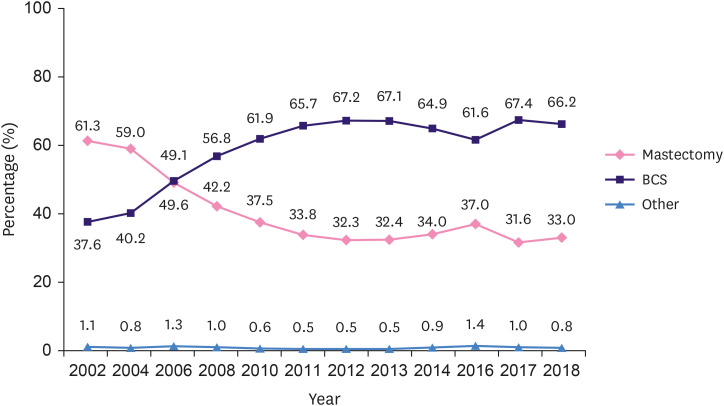
In 2002, the BCS and mastectomy rates were 37.6% and 61.3%, respectively. After that, the proportion of BCS has been gradually increasing, whereas the proportion of mastectomy has been gradually decreasing. In 2012, the BCS rate increased to 67.2% (126% increase, R2 = 0.988, p < 0.001), whereas the mastectomy rate decreased to 32.3% (47.3% decrease; R2 = 0.984, p < 0.001). From 2012 to 2016, the BCS rate decreased slightly to 61.6% (9.1% decrease, R2 = 0.991, p < 0.001), whereas the mastectomy rate slightly increased to 37.0% (14.5%, R2 = 0.984, p < 0.001). In 2018, the BCS and mastectomy rates were 66.2% and 33.0%, respectively. Therefore, the proportion of BCS has gradually increased since 2016 (Figure 7). When analyzing the surgical methods in relation to the invasiveness of cancer, different patterns were observed. Mastectomy was a more common surgical treatment for invasive cancer; it was performed in 28.7% of patients with noninvasive breast cancer and in 34.0% of patients with invasive breast cancer (p < 0.001) (Supplementary Figure 2).
Figure 7. Changes in the surgical management of breast cancer.
BCS = breast-conserving surgery.
Age-related characteristics
Based on the age analysis, 35% of all patients with breast cancer were aged ≥ 55 years (4,312/12,306). The clinical and pathological characteristics in relation to age are presented in Supplementary Table 1. The differences between the < 55-year and > 55-year age groups were also assessed in terms of stage, histological subtype, surgical method, and chemotherapy patterns. There were fewer older patients with stage 0 disease (13.5%) than younger patients. The tumor phenotype could be determined in 9,096 of 12,306 patients, HR-positive and HER2-negative tumors were less frequent in older patients (65.1%), and triple-negative tumors were more common in these patients (12.0%) than in younger patients. Mastectomy was more often performed in older patients (67.8%) than in younger patients, and younger patients were more frequently subjected to NACT (Supplementary Table 1).
Five-year relative survival rate
The 5-year RSR has been increasing according to the KCCR data. The 5-year RSR of female patients with breast cancer diagnosed between 1993 and 1995 was 79.3%, but it has been rising steadily. Consequently, the 5-year RSR of female patients with breast cancer diagnosed in 2014–2018 was 93.3% (Table 5). The 5-year RSRs according to age group were the highest (94.2%) in the 45–60-years age group and lowest (90.9%) in the > 60-year age group. According to the method of classifying local, regional, and distant cancer stages proposed by the Surveillance, Epidemiology, and End Results (SEER) program, the 5-year RSRs of patients diagnosed in 2014–2018 were 98.8%, 92.4%, and 40.3%, respectively. The 5-year RSR of the local and regional stages gradually improved, but the RSR of the distant stage decreased.
Table 5. Five-year relative survival rate of female patients with breast cancer in Korea (1993–2018).
| Factor | Year of diagnosis | ||||||
|---|---|---|---|---|---|---|---|
| 1993–1995 | 1996–2000 | 2001–2005 | 2006–2010 | 2011–2015 | 2014–2018 | ||
| Age group (yr) | |||||||
| < 45 | 80.3 | 85.1 | 89.2 | 91.8 | 93.3 | 93.9 | |
| 45–60 | 80.0 | 83.9 | 90.0 | 92.2 | 93.6 | 94.2 | |
| > 60 | 73.3 | 78.7 | 83.9 | 87.7 | 90.3 | 90.9 | |
| Stage group | |||||||
| Localized | - | - | - | 97.8 | 98.6 | 98.8 | |
| Regional | - | - | - | 89.7 | 91.6 | 92.4 | |
| Distant | - | - | - | 41.1 | 40.7 | 40.3 | |
| Unknown | - | - | - | 88.4 | 84.0 | 84.0 | |
DISCUSSION
The most important observation of this study is that breast cancer incidence is steadily increasing in the Korean population. By contrast, the ASR of other major cancers, such as liver, stomach, colon, and lung cancer, is steadily decreasing in Korea [2]. The increase in female obesity and smoking rates was indicated as the primary cause, but the most important factor is the change in the pattern of reproduction [10]. The mean age at menarche has decreased from 16.64 for women born in 1941 to 12.68 for women born in 1992—a decrease of 0.78 (or 0.81 in a regression) years per decade [11]. In addition, the mean age at onset of menopause has increased. The mean age at menopause in women born in 1929 or earlier and between 1930 and 1934, 1935 and 1939, 1940 and 1944, and 1945 and 1949 were 47.9, 48.1, 48.8, 50.1, and 50.5 years, respectively [12]. Furthermore, the fertility rate has been steadily decreasing and has recently decreased to 0.92 (2018); only 22.1% of the population had their first child in their twenties [10]. The global incidence of invasive breast carcinoma has relatively dropped due to a decrease in the use of post-menopausal hormone replacement therapy (HRT) [13]. In Korea, HRT use decreased from 7.8% in 2000 to 6.3% in 2013; however, the incidence of invasive and noninvasive breast cancers has rapidly increased. Therefore, it is assumed that changes in reproductive patterns have a significant effect on the incidence of breast cancer [14].
Cancer screening has important implications for cancer epidemiology, including the incidence and mortality. In Korea, a steady increase in the screening rate is closely related to an increase in the incidence of early-stage cancers [15,16]. According to the National Health Insurance Service data, 63.8% of eligible women underwent screening in 2018. Considering that socioeconomic status has a profound effect on women's reproductive patterns, lifestyles, and screening rates, the incidence of breast cancer in Korea is expected to increase.
Another important characteristic of Korean patients with breast cancer is that the proportion of breast cancer cases in younger patients is greater than that in patients living in Western countries. The age range at which invasive breast cancer is most frequently diagnosed in the United States is 60–69 years, and the age range with the highest ASR is 70–74 years, which is significantly different from that found in Korea [13]. In Japan, a double peak graph pattern was observed between the ages of 45–49 and 60–64 years, but no significant change was observed in the ASR after the age of 45 years. However, there was a minimal change in the 45–75-year age group, resulting in a plateau graph [17]. The ASR graphs of Japan and Korea are dramatically different, despite the close proximity of the 2 countries. According to the IARC data published in 2020, the ASR of invasive breast cancer in patients aged < 50 years in Korea was 41.4% per 100,000 people, the third highest in the world after Belgium (44.3) and France (42.4) [1].
Since 2000, the ASR of invasive breast cancer in Korea has been the highest between the ages of 45 and 49 years [8]. However, the peak point of the graph is slightly shifting to the right, and the median age has been constantly increasing (from 47.0 years in 2000 to 52.4 years in 2018). As observed in Table 4, the AAPCs were 7.4 in patients aged ≥ 60 years, 5.6 in those aged 45–60 years, and 4.9 in those aged < 40 years. There is a remarkable increase in breast cancer incidence in Korea among the elderly population, and the age group with peak incidence is expected to rise.
The pattern of pathological stages of breast cancer continues to show a favorable trend over time. According to our data, from 2012 (38.1%) to 2018 (62.4%), the number of patients diagnosed with stage 0 and 1 disease has steadily increased. In Korea, the early detection of breast cancer is expected to increase owing to the effective implementation of systematic health checkups [18]. According to the Korean National Cancer Screening Survey, the breast cancer screening rate in Korean women in all age groups is steadily increasing [15].
According to a recent study in the SEER program, the incidence of ER-positive breast cancer has significantly increased in Japanese women [19]. We found a similar trend in the present study. According to a pooled analysis of the Breast Cancer Association Consortium Studies, menarche that occurs before the age of 12 years, nulliparity, old age at first birth, and obesity in elderly women aged < 50 years are associated with the incidence of HR-positive breast cancer, particularly HR-positive and HER2-negative breast cancer. Recent studies have shown that an increase in the incidence of breast cancer in Korean women is associated with an increase in reproductive risk factors [20,21]. In addition, according to recently reported Korean national breast cancer data, an increase in reproductive risk factors is associated with an increase in the incidence of HR-positive breast cancer, particularly HR-positive and HER2-negative breast cancer [22].
The sustained increase in the incidence of HR-positive breast cancer is a common phenomenon observed in multiple countries [23]. Although no clear cause has been identified, high incidence of obesity may contribute to an increased risk of breast cancer [24]. HR-positive breast cancer is a subtype with a relatively good prognosis and may contribute to an increase in early breast cancer detection and improved survival rates [25]. Therefore, the significance of precision treatment strategies is higher in premenopausal women than in menopausal women. Insights from gene expression profiling have greatly expanded our understanding of the distinct HR-positive and HER2-negative subtypes of breast cancer and the impact of tumor biology on treatment outcomes. Efforts to develop genomic analysis platforms for clinical use have led to a new era in breast cancer management. In recent years, changes in treatment strategies based on genetic tests have been implemented in breast cancer patients with lymph node metastasis. Data from the SWOG 8814 and several population-based registries strongly indicate that pN1 patients with a recurrence score (RS) of < 18 have excellent oncological outcomes in the absence of chemotherapy. The West German study group PlanB and ADAPT trials provided prospective validation of good outcomes of endocrine therapy alone in patients with RS ≤ 11 and RS ≤ 25, respectively [26]. The recently published SWOG S1007 study, known as the RxPONDER, is a prospective multinational phase 3 clinical trial conducted in women with HR-positive, HER2-negative invasive breast cancer with 1 to 3 positive axillary lymph nodes. In postmenopausal pN1 patients with RS ≤ 25, endocrine therapy alone was shown to achieve results comparable to those of endocrine therapy combined with chemotherapy. However, the 5-year invasive disease-free survival (iDFS) of premenopausal patients in the endocrine therapy and chemotherapy groups was significantly improved, and the absolute difference in iDFS was 5.2%. A small (1.3%) but significant overall survival benefit was also observed in premenopausal patients who underwent to endocrine therapy and chemotherapy. Some chemotherapy benefits in premenopausal women were similar to those related to the age-based difference in chemotherapy observed in the TAILORx trial. This may be due to the indirect effects of chemotherapy on ovarian function [27]. Further research on chemotherapy-induced ovarian function suppression in premenopausal patients is necessary to shed more light on these observations.
In addition, steady changes were observed in the choice of the surgical procedure. The BCS increased from 37.6% in 2002 to 67.2% in 2012. The increase in the incidence of small breast cancer owing to the increased availability of screening programs may be the most important cause, along with the expansion of NACT availability [15]. However, the rate of BCS use has not increased since 2012. By contrast, it has been decreasing, whereas the rate of mastectomy has been increasing. This phenomenon may be due to the increased use of breast magnetic resonance imaging techniques, progress in the field of breast reconstruction, increased availability of genetic counseling, and increased involvement of patients in defining the optimal treatment strategy [28,29]. Unlike this recent trend, the KBCS registry data in 2017 showed an increasing tendency to undergo BCS in patients with breast cancer. The same trend was reported in 2018, with a BCS rate of 66.2% and a mastectomy rate of 33.0%. Interestingly, we analyzed the surgical methods in relation to the invasiveness of cancer, and mastectomy was found to be more commonly performed in patients with invasive breast cancer.
The ratio of mastectomy to BCS varies depending on the country, institution, patient's age, BMI, and socioeconomic status, and future patterns are not easy to predict. In addition, robotic surgery has recently been introduced in breast surgery and is widely used in Korea as well as in other countries. As these changes will influence surgical trends in the future, further research is necessary to assess their effects.
According to the KCCR data, the RSR of breast cancer has been increasing. The 5-year RSR of breast cancer diagnosed in 1993–1995 was 79.3%, but that for breast cancer diagnosed in 2014–2018 was 93.3%. Furthermore, the 5-year RSR was the lowest (90.9%) in the > 60-year age group and highest (94.2%) in the 45–60-year age group. As regards stage 0 cancer at diagnosis, this favorable molecular subtype was less frequent in the >55-year age group. In addition, comorbidities and a high prevalence of obesity may have an impact on breast cancer incidence [30]. There is a possibility that adjuvant therapy was not accurately optimized for older patients (in terms of regimen, dose, and schedule) compared with younger patients.
CONCLUSION
Taken together, our findings indicate that the incidence of breast cancer continues to increase in Korea. It is expected to increase further because of the changes in the reproductive pattern and other factors. As the incidence of HR-positive breast cancer and early-stage breast cancer continues to increase, the survival rate of patients with breast cancer in Korea is expected to increase further. Breast cancer is common in young Korean women, and 57.4% (13.528) of patients were diagnosed at the age of < 55 years, which is greater than that reported in Western countries. Age influences the incidence, surgical patterns, stages, and tumor biology of breast cancer, which has an important effect on disease management. Given that breast cancer is the most prevalent cancer in Korean women, widespread national education on the importance of screening and prevention is of great importance.
ACKNOWLEDGMENTS
We express our gratitude to all the members of the Korean Breast Cancer Society online registry. We also thank the Korean Statistical Information Service and the National Cancer Center for the data available on their websites, which forms the basis for this study.
Footnotes
Conflict of Interest: The authors declare that they have no competing interests.
- Data curation: Lee SB, Kim YS, Kim Z, Kim HY, Kim HJ, Park S, Bae SY, Yoon K, Lee SK, Jung KW, Han J, Youn HJ.
- Formal analysis: Kim YS, Kim Z, Kim HY, Kim HJ, Park S, Bae SY, Yoon K, Lee SK, Jung KW, Han J, Youn HJ.
- Writing - original draft: Kang SY, Lee SB.
- Writing - review & editing: Kang SY, Lee SB.
SUPPLEMENTARY MATERIALS
Age group-specific characteristics
Molecular subtype distribution according to cancer stage.
Surgery method distribution according to invasiveness of breast cancer.
References
- 1.Cancer today: data visualization tools for exploring the global cancer burden in 2020. International Agency for Research on Cancer. [Accessed January 22nd, 2021]. http://gco.iarc.fr/today/home.
- 2.National Cancer Information Center. [Accessed January 22nd, 2021]. https://www.cancer.go.kr.
- 3.International statistical classification of diseases and related health problems (ICD). World Health Organization. [Accessed January 22nd, 2021]. https://www.who.int/standards/classifications/classification-of-diseases.
- 4.Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020;52:335–350. doi: 10.4143/crt.2020.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segi M, Fujisaku S. Cancer mortality for selected sites in 24 countries (1950–1957) Sendai: Department of Public Health, Tohoku University School of Medicine; 1960. [Google Scholar]
- 6.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 7.Henson DE, Ries LA. The relative survival rate. Cancer. 1995;76:1687–1688. doi: 10.1002/1097-0142(19951115)76:10<1687::aid-cncr2820761002>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 8.Kang SY, Kim YS, Kim Z, Kim HY, Kim HJ, Park S, et al. Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer. 2020;23:115–128. doi: 10.4048/jbc.2020.23.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cancer staging system. American College of Surgeons. [Accessed January 22nd, 2021]. https://www.facs.org/quality-programs/cancer/ajcc/cancer-staging.
- 10.Statistics Korea. [Accessed January 22nd, 2021]. http://kostat.go.kr/portal/eng/index.action.
- 11.Sohn K. Improvement in the biological standard of living in 20th century Korea: evidence from age at menarche. Am J Hum Biol. 2017;29:e22882. doi: 10.1002/ajhb.22882. [DOI] [PubMed] [Google Scholar]
- 12.Park CY, Lim JY, Park HY. Age at natural menopause in Koreans: secular trends and influences thereon. Menopause. 2018;25:423–429. doi: 10.1097/GME.0000000000001019. [DOI] [PubMed] [Google Scholar]
- 13.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 14.Park CY, Lim JY, Kim WH, Kim SY, Park HY. Evaluation of menopausal hormone therapy use in Korea (2002−2013): a nationwide cohort study. Maturitas. 2021;146:57–62. doi: 10.1016/j.maturitas.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Suh M, Choi KS, Park B, Lee YY, Jun JK, Lee DH, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004−2013. Cancer Res Treat. 2016;48:1–10. doi: 10.4143/crt.2014.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi KS, Yoon M, Song SH, Suh M, Park B, Jung KW, et al. Effect of mammography screening on stage at breast cancer diagnosis: results from the Korea National Cancer Screening Program. Sci Rep. 2018;8:8882. doi: 10.1038/s41598-018-27152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mizukoshi MM, Hossian SZ, Poulos A. Comparative analysis of breast cancer incidence rates between Australia and Japan: screening target implications. Asian Pac J Cancer Prev. 2020;21:2123–2129. doi: 10.31557/APJCP.2020.21.7.2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016;19:1–7. doi: 10.4048/jbc.2016.19.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamashita H, Iwase H, Toyama T, Takahashi S, Sugiura H, Yoshimoto N, et al. Estrogen receptor-positive breast cancer in Japanese women: trends in incidence, characteristics, and prognosis. Ann Oncol. 2011;22:1318–1325. doi: 10.1093/annonc/mdq596. [DOI] [PubMed] [Google Scholar]
- 20.Yoo KY, Kim Y, Park SK, Kang D. Lifestyle, genetic susceptibility and future trends of breast cancer in Korea. Asian Pac J Cancer Prev. 2006;7:679–682. [PubMed] [Google Scholar]
- 21.Kim Y, Choi JY, Lee KM, Park SK, Ahn SH, Noh DY, et al. Dose-dependent protective effect of breast-feeding against breast cancer among ever-lactated women in Korea. Eur J Cancer Prev. 2007;16:124–129. doi: 10.1097/01.cej.0000228400.07364.52. [DOI] [PubMed] [Google Scholar]
- 22.Jung YS, Na KY, Kim KS, Ahn SH, Lee SJ, Park HK, et al. Nation-wide Korean breast cancer data from 2008 using the breast cancer registration program. J Breast Cancer. 2011;14:229–236. doi: 10.4048/jbc.2011.14.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeSantis CE, Ma J, Goding Sauer A, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017;67:439–448. doi: 10.3322/caac.21412. [DOI] [PubMed] [Google Scholar]
- 24.Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst. 2011;103:250–263. doi: 10.1093/jnci/djq526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kang SY, Kim YS, Kim Z, Kim HY, Lee SK, Jung KW, et al. Basic findings regarding breast cancer in Korea in 2015: data from a breast cancer registry. J Breast Cancer. 2018;21:1–10. doi: 10.4048/jbc.2018.21.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nitz U, Gluz O, Christgen M, Kates RE, Clemens M, Malter W, et al. Reducing chemotherapy use in clinically high-risk, genomically low-risk pN0 and pN1 early breast cancer patients: five-year data from the prospective, randomised phase 3 West German Study Group (WSG) PlanB trial. Breast Cancer Res Treat. 2017;165:573–583. doi: 10.1007/s10549-017-4358-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.RxPONDER clinical trial key findings presented at San Antonio Breast Cancer Symposium. Oncotype IQ. [Accessed January 22nd, 2021]. https://www.oncotypeiq.com/en/announcements/SABCS.
- 28.Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318:918–926. doi: 10.1001/jama.2017.11470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455–1461. doi: 10.1001/jama.2013.278932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul) 2015;30:142–146. doi: 10.3803/EnM.2015.30.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Age group-specific characteristics
Molecular subtype distribution according to cancer stage.
Surgery method distribution according to invasiveness of breast cancer.