Abstract
Aims
We compared the clinical outcomes of curved intertrochanteric varus osteotomy (CVO) with bone impaction grafting (BIG) with CVO alone for the treatment of osteonecrosis of the femoral head (ONFH).
Methods
This retrospective comparative study included 81 patients with ONFH; 37 patients (40 hips) underwent CVO with BIG (BIG group) and 44 patients (47 hips) underwent CVO alone (CVO group). Patients in the BIG group were followed-up for a mean of 12.2 years (10.0 to 16.5). Patients in the CVO group were followed-up for a mean of 14.5 years (10.0 to 21.0). Assessment parameters included the Harris Hip Score (HHS), Oxford Hip Score (OHS), Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire (JHEQ), complication rates, and survival rates, with conversion to total hip arthroplasty (THA) and radiological failure as the endpoints.
Results
There were no significant differences in preoperative and postoperative HHS or postoperative OHS and JHEQ between the BIG group and the CVO group. Complication rates were comparable between groups. Ten-year survival rates with conversion to THA and radiological failure as the endpoints were not significantly different between groups. Successful CVO (postoperative coverage ratio of more than one-third) exhibited better ten-year survival rates with radiological failure as the endpoint in the BIG group (91.4%) than in the CVO group (77.7%), but this difference was not significant (p = 0.079).
Conclusion
Long-term outcomes of CVO with BIG were favourable when proper patient selection and accurate surgery are performed. However, this study did not show improvements in treatment results with the concomitant use of BIG.
Cite this article: Bone Joint J 2021;103-B(4):665–671.
Keywords: Osteonecrosis, Femoral head, Curved intertrochanteric varus osteotomy, Bone impaction grafting, Long-term outcomes
Introduction
Osteonecrosis of the femoral head (ONFH) often occurs in young adults and requires early intervention, which makes the treatment choice difficult.1 Total hip arthroplasty (THA) is currently the most widely performed surgical procedure in treating ONFH2,3 but for young patients the possibility of multiple revisions is a concern.4 Although various types of joint-preserving surgery have been performed for ONFH, such procedures have limited indications and difficult surgical techniques.5-8
Curved intertrochanteric varus osteotomy (CVO) can be performed for patients when more than one-third of the weight-bearing area is covered with an intact articular surface as judged from preoperative anteroposterior radiographs of the hip when in maximum abduction.9-11 CVO was developed as a treatment for osteoarthritis secondary to acetabular dysplasia, and several studies have also reported favourable clinical outcomes when used for ONFH.9-11 CVO is a relatively simple surgical procedure that prevents weakening of the gluteus medius and minimus muscles as well as leg length discrepancies which can occur with conventional varus wedge osteotomy.11 Previous studies have shown that favourable outcomes can be achieved when an intact weight bearing cartilage ratio of more than one-third can be achieved postoperatively, but the results were poor for more extensive necrosis where this was not possible.11,12
To further improve treatment outcomes for ONFH, we started performing CVO with bone impaction grafting (BIG) in 2004. BIG can prevent the progression of osteoarthritis by restoring the collapsed spheroid head and remodelling the necrotic area by autologous bone grafting. We hoped that BIG could be applied to a wider range of cases with necrosis that could not be treated with conventional CVO. This study compared the clinical outcomes of CVO with BIG and CVO alone for patients with ONFH at a minimum of ten years follow-up.
Methods
Design
This study was based on a retrospective chart review and was approved by our Institutional Review Board. All patients provided written informed consent to participate. The study included 98 patients who consecutively underwent CVO with BIG (43 patients; BIG group) or CVO alone (55 patients; CVO group) for non-traumatic ONFH between January 1999 and January 2010. There were 17 patients with less than ten years follow-up who were excluded. The BIG group consisted of 37 patients (24 men and 13 women; 40 hips; mean age 37.2 years (18 to 60)) and the CVO group comprised 44 patients (30 men and 14 women; 47 hips; mean age 40.1 years (17 to 66). Patients in the BIG group were followed up for a mean of 12.2 years (10 to 16.5). Those in the CVO group were followed up for a mean of 14.5 years (10 to 21). The stage and type of ONFH were classified as described by the Japanese Investigation Committee (JIC) of the Ministry of Health, Labour, and Welfare (Figure 1 and Table I).13 No significant differences in sex, age, body mass index, or stage and type classification were found between groups; however, there were differences in the follow-up duration (Table II).
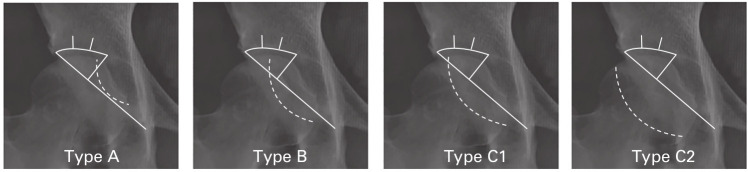
Fig. 1.
The classification of the localization of the necrotic lesion according to the Japanese Investigation Committee of the Ministry of Health, Labour and Welfare.13 Type A necrotic area occupies the medial one-third or less of the weight-bearing area, Type B the medial two-thirds or less, Type C1 more than two-thirds but not extending to the acetabular rim, and Type C2 more than two-thirds and extending to the acetabular rim.
Table I.
Japanese Investigation Committee of the Ministry of Health, Labour and Welfare stage classification.
| Stage 1 | There are no specific findings of osteonecrosis on radiographs. |
| Stage 2 | Demarcating sclerosis is seen without collapse of the femoral head. |
| Stage 3A | Collapse of the femoral head is less than 3 mm. |
| Stage 3B | Collapse of the femoral head is 3 mm or greater. |
| Stage 4 | Osteoarthritic changes are seen. |
Table II.
Patient demographic details.
| Variable | BIG group | CVO group | p-value |
|---|---|---|---|
| Patients, n | 37 | 44 | N/A |
| Hips, n | 40 | 47 | N/A |
| Sex (male/female), n | 24/13 | 30/14 | 0.691* |
| Mean BMI, kg/m2 (SD) | 21.6 (3.4) | 20.9 (3.1) | 0.572† |
| Mean age at surgery, yrs (SD) | 37.2 (8.1) | 40.1 (8.5) | 0.112† |
| Mean follow-up, yrs (SD) | 12.2 (4.3) | 14.5 (4.4) | 0.002† |
| ONFH Stage, n | 0.868‡ | ||
| 1 | 0 | 0 | |
| 2 | 8 | 13 | |
| 3a | 22 | 24 | |
| 3b | 10 | 10 | |
| 4 | 0 | 0 | |
| ONFH Type, n | 0.521‡ | ||
| A | 0 | 0 | |
| B | 6 | 8 | |
| C1 | 25 | 32 | |
| C2 | 9 | 7 |
Fisher's exact test.
Independent-samples t-test.
Chi-squared test.
BIG, bone impaction grafting; BMI, body mass index; CVO, curved intertrochanteric varus osteotomy; N/A, not applicable; ONFH, osteonecrosis of the femoral head.
Surgical indication and technique
CVO was performed for patients when more than one-third of the weight-bearing area was covered with an intact articular surface as judged from preoperative anteroposterior radiographs of the hip in maximum abduction. In general, joint preservation surgery is offered to patients younger than 50 years. For patients 50 years or older, CVO was performed only when the patient strongly desired joint preservation. During the study period, 20 hips (BIG group, nine hips; CVO group, 11 hips) of patients 50 years or older underwent surgery.
We started CVO with BIG for ONFH in 2004. The number of cases was increased gradually due to the increased difficulty of the surgical procedure, the potential for an increased risk of complications and because the outcomes when BIG was used were unknown. From 2007, we started to use BIG for all cases.
The operating technique for CVO has been described previously.6,11 Following completion of the curved osteotomy,for those cases where BIG was performed, a guide pin was passed from the osteotomy to the centre of the necrotic area using fluoroscopy. A 10 mm diameter drill was passed over the guide pin (Figure 2a) and impaction of autogenous bone collected from the iliac bone was performed (Figure 2b). Improvements in the collapsed area of the femoral head were carefully evaluated using fluoroscopy. The procedure was completed by performing artificial bone impaction with a beta-tricalcium phosphate graft (Figure 2c). Subsequently, the CVO correction was completed by orientating the proximal bone fragment into varus and followed by osteosynthesis. The fixation method of a compression hip screw and additional cannulated cancellous screws was the same regardless of whether BIG was performed.Patients were allowed to walk with 10 kg partial weight-bearing using two crutches starting from the first day after surgery. Full weight-bearing was allowed at ten to 12 weeks after surgery. All operations were performed or supervised by one senior surgeon (YH) who also made decisions regarding whether to use BIG.
Fig. 2.
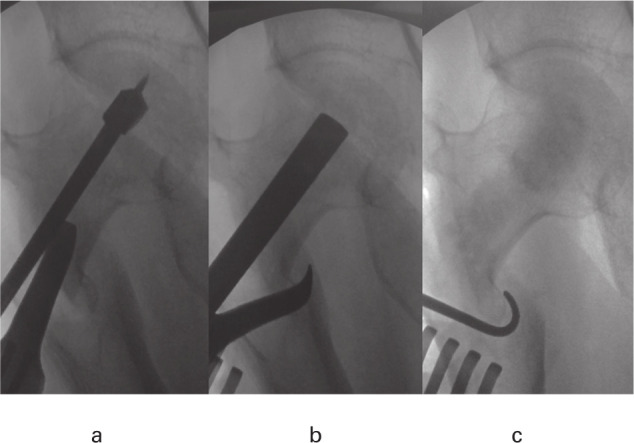
a) An osteotomy guide pin was placed in the centre of the necrotic area during fluoroscopy and a bone hole was drilled over the guide pin. b) Impaction of autogenous bone was performed in the necrotic area and the shape of the femoral head was evaluated to prevent puncture into the joint. c) The procedure was completed by impacting the beta-tricalcium phosphate grating after the autogenous bone.
Measurements
The medical records of patients who underwent THA after CVO were reviewed, and operating time, intraoperative blood loss, and postoperative complications such as infection, pseudarthrosis, nerve palsy, and heterotopic ossification were recorded. Functional outcomes were evaluated using the Harris Hip Score (HHS)14 and range of motion (ROM) before surgery and at the final follow-up. Generally, one senior surgeon (YH) assessed the HHS and ROM annually. Patient-reported outcomes were evaluated post-operatively using the Oxford Hip Score (OHS)15,16 and Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire (JHEQ).17 When the assessment questionnaires were sent to the patients after the last follow-up, the response rate was 89% (33/37) for the BIG group and 73% (32/44) for the CVO group. The cases that were converted to THA during the follow-up period were excluded from the final follow-up results.
Radiological evaluation was performed using an anteroposterior (AP) hip joint image centred on the pubic symphysis in the supine position. The postoperative ratio of the intact articular surface of the femoral head to the weight-bearing area of the acetabulum was calculated according to Sugioka et al’s5 method (Figure 3). We defined successful CVO surgery as a postoperative coverage ratio of more than one-third.9,11 This ratio, along with postoperative progression of osteoarthritis (OA) and postoperative secondary collapse were measured using the AP image of the hip joint after surgery and during follow-up. Radiological progression of OA was defined as narrowing of the minimum joint space in the weight-bearing surface to less than 2 mm without secondary collapse. The minimum width of the joint space was measured in the subchondral sclerotic line of the weight-bearing surface.18 Secondary collapse was defined as subsidence of the articular surface exceeding 2 mm when compared with the postoperative radiograph. This was assessed according to Miyanishi et al’s19 method. Radiological failure was defined as secondary collapse and/or osteoarthritic change. To assess the interobserver reliability of the JIC type, stage classification, and postoperative intact ratio, 30 hips were selected at random and assessed by two surgeons (YO and TO). The interobserver reliability values for the type, stage classification, and postoperative intact ratio were 0.862 (95% confidence interval (CI) 73% to 93%), 0.824 (95% CI 62% to 90%), and 0.802 (95% CI 72% to 93%), respectively.
Fig. 3.
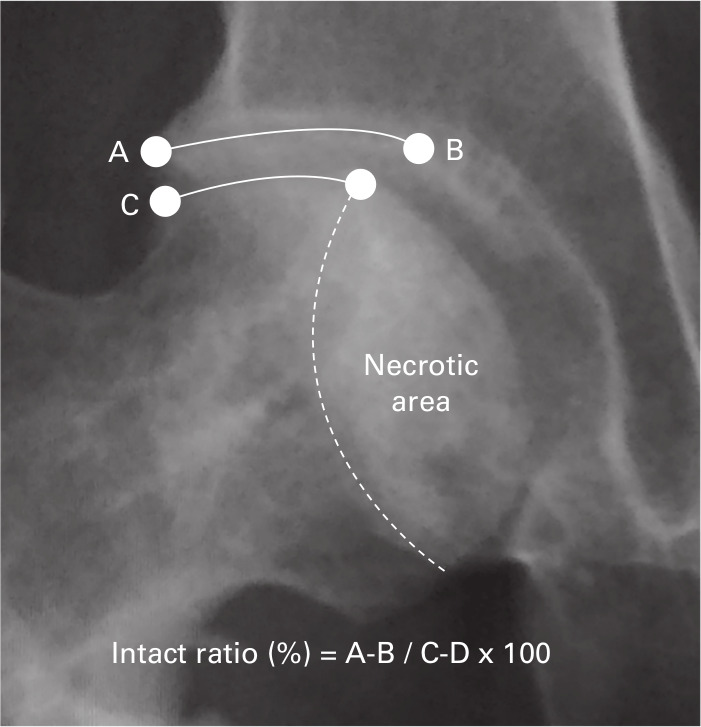
Measurement for the ratio of the intact articular surface of the femoral head to the weight-bearing area of the acetabulum (A to B weight-bearing surface of acetabulum, and C to D intact area by osteotomy)
Statistical analysis
Statistical analyses were performed with SPSS version 21 (IBM, Armonk, New York, USA). Analyses consisted of independent-samples t-test for continuous variables, the Mann-Whitney U test for non-parametric variables, and Fisher’s exact test and chi-squared test for categorical variables. Survival rates were examined using log-rank test and the Kaplan–Meier method with 95% CIs, with conversion to THA and radiological failure as the endpoints. A total of 17 patients who could not participate in follow-up for more than ten years were added to the remaining 81 patients and considered as censored cases during the survival rate analysis. Furthermore, during the subgroup analysis, the survival rate was evaluated according to the type and successful CVO surgeries in each group, with radiological failure as the endpoint. The groups were compared using a log-rank analysis. A p-value < 0.01 was considered statistically significant.
Results
The mean operating times were longer in the BIG group (128.8 minutes (SD 28.1)) than in the CVO group (115.9 minutes (SD 20.0)), but this difference was not significant (p = 0.021, Mann-Whitney U test). Mean intraoperative blood loss was significantly higher in the BIG group (233 g (SD 159)) than in the CVO group (172 g (SD 104; p < 0.001, Mann-Whitney U test). The preoperative mean HHS was slightly lower in the BIG group (72.1 (SD 9.5)) than in the CVO group (74.2 (SD 8.7)), but there was no significant difference between groups. There was no significant difference in the mean postoperative HHS of the BIG group (88.1 (SD 11.1)) and CVO group (86.9 (SD 11.0)). Additionally, the changes in mean HHS preoperatively and at the final follow-up were not significantly different for the BIG group (15.9 (SD 13.4)) and CVO group (12.7 (SD 10.8)). Both preoperative and postoperative mean ROM were not significantly different in the BIG group and CVO group. Patient-reported outcomes indicated that the mean OHS and JHEQ at the final follow-up were not significantly different for the BIG group (40.0 (SD 9.8) and 52.3 (SD 19.2)) and CVO group (38.8 (SD 8.8) and 50.5 (SD 17.1)) (Table III).
Table III.
Clinical evaluations.
| Variable | BIG group | CVO group | p-value |
|---|---|---|---|
| Preoperative HHS (SD) | 72.1 (9.5) | 74.2 (8.7) | 0.071* |
| HHS, last follow-up (SD) | 88.1 (11.1) | 86.9 (11.0) | 0.585* |
| OHS, last follow-up (SD) | 40.0 (9.8) | 38.8 (8.8) | 0.482† |
| JHEQ, last follow-up (SD) | 52.3 (19.2) | 50.5 (17.1) | 0.638† |
| Preoperative ROM (SD) | |||
| Flexion | 113.9 (11.0) | 117.2 (10.4) | 0.182* |
| Extension | 11.9 (5.3) | 12.9 (5.3) | 0.081* |
| Abduction | 28.4 (6.4) | 28.7 (6.5) | 0.868* |
| Adduction | 15.9 (6.7) | 16.8 (6.2) | 0.116* |
| External rotation | 24.3 (11.8) | 28.9 (11.5) | 0.069* |
| Internal rotation | 24.7 (13.7) | 28.7 (11.9) | 0.121* |
| ROM, last follow-up (SD) | |||
| Flexion | 106.3 (19.9) | 100.4 (17.2) | 0.144* |
| Extension | 14.3 (6.2) | 12.7 (6.7) | 0.297* |
| Abduction | 25.6 (7.5) | 20.4 (6.8) | 0.028* |
| Adduction | 18.8 (4.8) | 19.1 (4.3) | 0.877* |
| External rotation | 24.6 (12.3) | 29.5 (14.5) | 0.133* |
| Internal rotation | 23.6 (15.3) | 22.8 (21.4) | 0.859* |
| Complications | 1 | 1 | 1.000‡ |
| Infection | 0 | 0 | 1.000‡ |
| Nerve palsy | 0 | 0 | 1.000‡ |
| Peri‐implant fracture | 1 | 1 | 1.000‡ |
| Conversion to THA | 7 | 6 | 0.561‡ |
Independent-samples t-test.
Mann-Whitney U test.
Fisher's exact test
CVO, curved intertrochanteric varus osteotomy; HHS, Harris Hip Score; JHEQ, Japanese Orthopaedic Association Hip-Disease Evaluation Questionnaire; OHS, Oxford Hip Score; ROM, range of motion; THA, total hip arthroplasty.
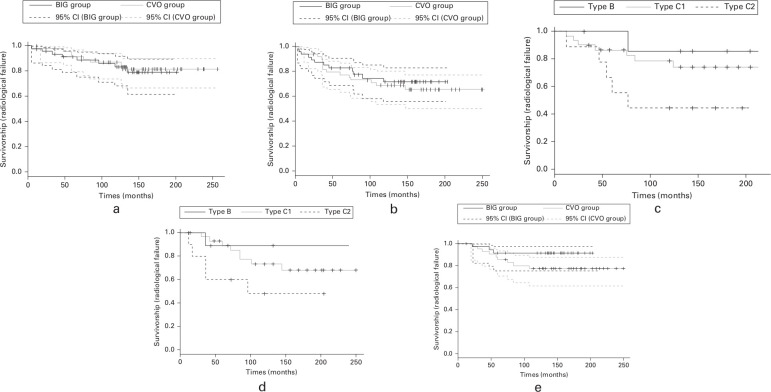
There was one peri-implant fracture case in the BIG group and one peri-implant fracture case in the CVO group. Conversion to THA due to secondary osteoarthritis was performed for seven patients (seven hips) in the BIG group and for six patients (six hips) in the CVO group. The ten-year survival rates using conversion to THA as the endpoint were 83.5% (95% confidence CI 68% to 91%) for the BIG group and 87.3% (95% CI 74% to 94%) for the CVO group (p = 0.758, log-rank test) (Figure 4a). The ten-year survival rates using radiological failure as the endpoint were 71.7% (95% CI 55% to 83%) for the BIG group and 68.8% (95% CI 54% to 80%) for the CVO group (p = 0.644, log-rank test); radiological failure was observed in 12 patients in the BIG group and 13 in the CVO group (Figure 4b). The sub-analysis results of ten-year survival rates of the BIG group, based on type classifications and using radiological failure as the endpoint, showed significant differences in type B (85.7% (95% CI 33% to 98%)), type C1 (78.8% (95% CI 52% to 89%)), and type C2 (44.4% (95% CI 17% to 72%)) (p < 0.001, log-rank test) (Figure 4c). Similarly, in the CVO group, there were significant differences in type B (88.9%), type C1 (73.2%), and type C2 (48.0%) (p < 0.001, log-rank test) (Figure 4d). As defined by the postoperative coverage ratios, there were 30 successful CVO cases in the BIG group and 38 in the CVO group. The ten-year survival rate for these cases using radiological failure as the endpoint was higher for the BIG group (91.4%; 95% CI 76% to 97%) than for the CVO group (77.7%; 95% CI 61% to 87%), but this difference was not significant (p = 0.079, log-rank test) (Figure 4e). A post hoc power analysis was performed to determine the ability of our study to demonstrate a true difference in outcomes from successful CVO surgery between the BIG group and CVO group. The power of this study was 55% and would need 68 patients per group to have 80% power.
Fig. 4.
a) Survival with total hip arthroplasty as the endpoint. The survival rates were similar for the bone impaction grafting (BIG) group (83.5%) and the curved intertrochanteric varus osteotomy (CVO) group (87.3%) at ten years. b) Survival with radiological failure as the endpoint. The survival rate at ten years was not significantly different between the BIG group (71.7%) and the CVO group (68.8%). c) There were significant differences in ten-year survival rates of type B (85.7%), type C1 (78.8%), and type C2 (44.4%) in the BIG group (p < 0.01). d) There were significant differences in ten-year survival rates of type B (88.9%), type C1 (73.2%), and type C2 (48.0%) in the CVO group (p < 0.001). e) The survival rates at ten years were higher in the BIG group (91.4%) than in the CVO group (77.7%), but there were no significant differences between groups (p = 0.079)
Discussion
In the present study, we compared outcomes of surgical treatment for ONFH with either CVO combined with BIG or CVO alone. The clinical outcomes, complication rates, and ten-year survival rates using THA and radiological failure as endpoints were equivalent for the two groups. CVO combined with BIG showed poor outcomes for type C2 ONFH as well as CVO alone. For successful CVO cases, the ten-year survival rate using radiological failure as the endpoint showed a non-significant trend in favour of the additional use of BIG.
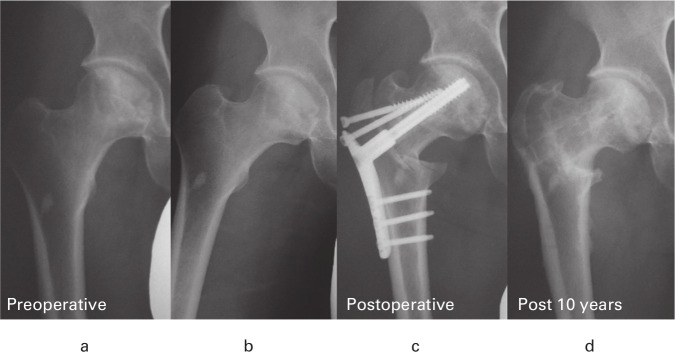
CVO can be performed for patients when more than one-third of the weight-bearing area was covered with an intact articular surface as judged from preoperative AP radiographs of the hip in maximum abduction6,11However, it is difficult to obtain coverage of more than one-third of the weight-bearing area in large necrotic areas, such as type C2; and the treatment results of CVO were poor in our previous reports for these situations.11,12 Therefore, we hypothesised that larger areas of necrosis could be a potential indication for BIG. However, this study demonstrates that the treatment results of BIG with CVO for type C2 lesions were just as poor as those of CVO alone. Therefore, the use of BIG with CVO for type C2 ONFH cannot prevent future OA progression on this evidence. Although the difference was not significant for hips where postoperative coverage was deemed successful, the use of BIG with CVO showed a trend of improvement in the ten-year survival rate with radiological failure as the endpoint. We believe that this resulted from performing CVO and BIG together (Figure 5). Since the number of cases in this study is small, statistical strength is insufficient, but it may be possible to demonstrate any additional effectiveness by conducting the study with an increased number of cases.
Fig. 5.
a) Preoperative anteroposterior (AP) radiograph showing the right hip of a 33-year-old man with type C1 osteonecrosis of the femoral head. b) A preoperative AP radiograph in maximum hip abduction showing coverage of more than one-third of the weight-bearing area with an intact articular surface. c) Postoperative AP radiograph obtained one year after curved intertrochanteric varus osteotomy (CVO) showing restoration of the collapsed spheroid head. d) An AP radiograph showing a lack of osteoarthritic progression and remodelled necrotic area ten years after surgery.
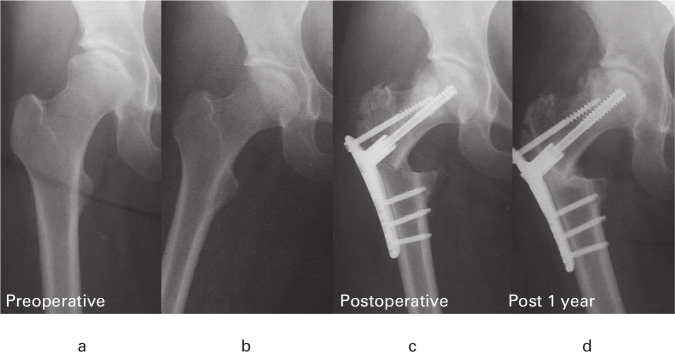
The extent of changes in the necrotic area over time is controversial. It was previously reported that remodelling of the necrotic area was caused by changes in the mechanical environment with CVO.20 It is known that good remodelling of necrotic sites can occur, particularly in young patients.21 However, it is also known that the results of simply transplanting autologous bone to a large necrotic site are poor.22 Chen et al23 reported that the treatment results ofor type C2 were poor when impacting bone allograft combined with fibula grafting compared with those of type B and C1. In this study, it was thought that remodelling of bone could not be expected because early secondary collapse had already occurred in C2 cases with large areas of necrosis (Figure 6).
Fig. 6.
a) Preoperative anteroposterior (AP) radiograph showing the right hip of a 26-year-old woman with type C2 osteonecrosis of the femoral head. b) A preoperative AP radiograph showing a lack of coverage of more than one-third of the weight-bearing area with an intact articular surface in maximum hip abduction. c) Postoperative AP radiograph obtained two weeks after curved intertrochanteric varus osteotomy (CVO). d) The progression of collapse and osteoarthritis six months after CVO.
It is unknown whether BIG can effectively prevent crushing. During fluoroscopy, BIG was observed in the centre of a necrotic area. Recent studies have revealed that some necrotic areas are more susceptible to collapse. Kubo et al24 reported that collapse is more likely in cases of large anterior necrosis. Similarly, Hamada et al25 performed a micro-CT analysis and reported that subchondral fractures begin from the anterior part of necrosis. Considering these reports, BIG may be more effective at preventing collapse if it is applied to the anterior necrotic border rather than the centre of necrosis. Recently, navigation has been used so that BIG can be performed in a more accurate position and so that further improvements in clinical outcomes may occur.
There were several limitations to this study. First, this was a retrospective study and the number of cases (40 hips) was small. Increasing the number of patients in the cohorts would increase the statistical power of the relevant findings. Second, we did not evaluate all outcome measures preoperatively and future studies should include both preoperative and postoperative data. Third, we could not evaluate the position of BIG performed in the femoral head and the recovery of spherical shape; a more detailed image analysis could be performed in future studies to evaluate the remodelling effects on the necrotic area. Fourth, the volume of the necrotic area could not be evaluated. Although there was no difference in the preoperative type between the two groups, BIG might have been more frequently used for patients with large necrotic volumes. Therefore, the possibility of differences in the preoperative conditions cannot be excluded. Finally, this research was conducted under the guidance of one experienced senior surgeon and may not be generalizable. Although the surgical procedures for both CVO and BIG are relatively simple, when BIG is used together with CVO, blood loss does increase and therefore careful attention to complications is required until surgical experience is gained.
With the recent progress in THA, the use of osteotomy for ONFH has been decreasing.2,3 However, the Norwegian register reported that the ten-year survival rate for THA for people younger than 20 years was 70%.4 In addition, the Swedish Register reported 15-year survival rates of 78% for those younger than 30 years and 89% for those older than 30 years;26 therefore, the possibility of multiple future revision surgeries should be considered. Favourable clinical outcomes of CVO have been reported mainly in Japan.9-11 This study revealed that CVO combined with BIG can achieve favourable joint preservation in the long term by proper patient selection and accurate surgery.
In conclusion, this study revealed that CVO combined with BIG can result in favourable joint preservation and long-term outcomes for ONFH. However, this study did not show improvements in treatment results with the concomitant use of BIG when compared with CVO alone.
Take home message
- Curved intertrochanteric varus osteotomy (CVO) combined with bone impaction grafting (BIG) could be achieved favourable joint preservation by proper patient selection and accurate surgery compare to CVO alone.
- Long-term outcomes of CVO with BIG and CVO alone were favourable.
- The use of BIG with CVO for type C2 osteonecrosis of the femoral head (ONFH) cannot prevent future osteoarthritis progression.
Author contributions
Y. Osawa: Drafted the manuscript.
T. Seki: Conceptualized and designed the study.
T. Okura: Collected and assembled the data.
Y. Takegami: Conducted the statistical analysis.
N. Ishiguro: Gave final approval on the article.
Y. Hasegawa: Conceptualized and designed the study.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors thank Dr. Taiki Kusano, Dr Shinya Kaneko, Dr. Kazuya Makida and Dr Satoshi Ochiai for their assistance throughout this study.
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
This article was primary edited by J. Hutt and first proof edited by G. Scott.
References
- 1.Osawa Y, Seki T, Takegami Y, Kasai T, Higuchi Y, Ishiguro N. Do femoral head collapse and the contralateral condition affect patient-reported quality of life and referral pain in patients with osteonecrosis of the femoral head? Int Orthop. 2018;42(7):1463–1468. [DOI] [PubMed] [Google Scholar]
- 2.Johnson AJ, Mont MA, Tsao AK, Jones LC. Treatment of femoral head osteonecrosis in the United States: 16-year analysis of the nationwide inpatient sample. Clin Orthop Relat Res. 2014;472(2):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaneko S, Takegami Y, Seki T, et al. . Surgery trends for osteonecrosis of the femoral head: a fifteen-year multi-centre study in Japan. Int Orthop. 2020;44(4):761–769. [DOI] [PubMed] [Google Scholar]
- 4.Tsukanaka M, Halvorsen V, Nordsletten L, et al. . Implant survival and radiographic outcome of total hip replacement in patients less than 20 years old. Acta Orthop. 2016;87(5):479–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. indications and long-term results. Clin Orthop Relat Res. 1992;277:111–120. [PubMed] [Google Scholar]
- 6.Sakano S, Hasegawa Y, Torii Y, Kawasaki M, Ishiguro N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2004;86-B(3):359–365. [DOI] [PubMed] [Google Scholar]
- 7.Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999;81-A(2):200–209. [DOI] [PubMed] [Google Scholar]
- 8.Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995;77-A(5):681–694. [DOI] [PubMed] [Google Scholar]
- 9.Zhao G, Yamamoto T, Ikemura S, et al. . Radiological outcome analysis of transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head at a mean follow-up of 12.4 years. J Bone Joint Surg Br. 2010;92-B(6):781–786. [DOI] [PubMed] [Google Scholar]
- 10.Hamanishi M, Yasunaga Y, Yamasaki T, Mori R, Shoji T, Ochi M. The clinical and radiographic results of intertrochanteric curved varus osteotomy for idiopathic osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2014;134(3):305–310. [DOI] [PubMed] [Google Scholar]
- 11.Okura T, Hasegawa Y, Morita D, Osawa Y, Ishiguro N. What factors predict the failure of curved intertrochanteric varus osteotomy for the osteonecrosis of the femoral head? Arch Orthop Trauma Surg. 2016;136(12):1647–1655. [DOI] [PubMed] [Google Scholar]
- 12.Osawa Y, Seki T, Okura T, Takegami Y, Ishiguro N, Hasegawa Y. Curved intertrochanteric varus osteotomy vs total hip arthroplasty for osteonecrosis of the femoral head in patients under 50 years old. J Arthroplasty. 2020;35(6):1600–1605. [DOI] [PubMed] [Google Scholar]
- 13.Sugano N, Kubo T, Takaoka K, et al. . Diagnostic criteria for non-traumatic osteonecrosis of the femoral head. A multicentre study. J Bone Joint Surg Br. 1999;81-B(4):590–595. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 15.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78-B(2):185–190. [PubMed] [Google Scholar]
- 16.Murray DW, Fitzpatrick R, Rogers K, et al. . The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89(8):1010–1014. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto T, Kaneuji A, Hiejima Y, et al. . Japanese orthopaedic association hip disease evaluation questionnaire (JHEQ): a patient-based evaluation tool for hip-joint disease. The Subcommittee on hip disease evaluation of the clinical outcome Committee of the Japanese orthopaedic association. J Orthop Sci. 2012;17(1):25–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B. The relationship of hip joint space to self reported hip pain. A survey of 4.151 subjects of the Copenhagen City heart study: the osteoarthritis substudy. Osteoarthritis Cartilage. 2004;12(9):692–697. [DOI] [PubMed] [Google Scholar]
- 19.Miyanishi K, Noguchi Y, Yamamoto T, et al. . Prediction of the outcome of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000;82-B(4):512–516. [DOI] [PubMed] [Google Scholar]
- 20.Hasegawa Y, Yamaguchi J, Kanoh T, Seki T, Kawabe K. Low signal intensity area by magnetic resonance imaging that disappeared after a curved intertrochanteric varus osteotomy for traumatic osteonecrosis of the femoral head. J Orthop Sci. 2008;13(3):265–268. [DOI] [PubMed] [Google Scholar]
- 21.Atsumi T, Kajiwara T, Hiranuma Y, Tamaoki S, Asakura Y. Posterior rotational osteotomy for nontraumatic osteonecrosis with extensive collapsed lesions in young patients. J Bone Joint Surg Am. 2006;88-A(Suppl 3):42–47. [DOI] [PubMed] [Google Scholar]
- 22.Wang B-L, Sun W, Shi Z-C, et al. . Treatment of nontraumatic osteonecrosis of the femoral head using bone impaction grafting through a femoral neck window. Int Orthop. 2010;34(5):635–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen L, Hong G, Hong Z, et al. . Optimizing indications of impacting bone allograft transplantation in osteonecrosis of the femoral head. Bone Joint J. 2020;102-B(7):838–844. [DOI] [PubMed] [Google Scholar]
- 24.Kubo Y, Motomura G, Ikemura S, et al. . The effect of the anterior boundary of necrotic lesion on the occurrence of collapse in osteonecrosis of the femoral head. Int Orthop. 2018;42(7):1449–1455. [DOI] [PubMed] [Google Scholar]
- 25.Hamada H, Takao M, Sakai T, Sugano N. Subchondral fracture begins from the bone resorption area in osteonecrosis of the femoral head: a micro-computerised tomography study. Int Orthop. 2018;42(7):1479–1484. [DOI] [PubMed] [Google Scholar]
- 26.Mohaddes M, NaucléR E, Kärrholm J, Malchau H, Odin D, Rolfson O. Implant survival and patient-reported outcome following total hip arthroplasty in patients 30 years or younger: a matched cohort study of 1,008 patients in the Swedish hip arthroplasty register. Acta Orthop. 2019;90(3):249–252. [DOI] [PMC free article] [PubMed] [Google Scholar]